Abstract
A 60-year-old man with out-of-hospital cardiac arrest was transported to our hospital by an emergency medical service. Ventricular fibrillation was finally terminated after the initiation of circulation support by percutaneous cardiopulmonary support device. Although acute myocardial infarction was suspected, emergency coronary angiography could not identify the culprit lesion of myocardial infarction while there were multiple intermediate stenotic lesions. Since re-elevation of troponin I was recorded on the 4th day after admission, coronary angiography was performed again, and diffuse severe stenosis in the right coronary artery and total occlusion in the left circumflex coronary artery that disappeared by the injection of isosorbide dinitrate was detected. Therefore, we reached the diagnosis of acute myocardial infarction due to coronary vasospasm. It is very rare that emergency coronary angiogram reveals coronary vasospasm at the culprit lesion of myocardial infarction. The guideline recommends calcium channel antagonist and long-acting nitrates for vasospastic angina; however, it would be really difficult to make correct diagnosis of coronary vasospasm among the patients with acute myocardial infarction or out-of-hospital cardiac arrest. Repeated measurements of troponin and coronary angiography identified the cause of acute myocardial infarction as coronary vasospasm in the present case.
<Learning objective: Coronary vasospasm may be one of important causes of acute MI and of OHCA, although it is difficult to be diagnosed correctly. We should always take into consideration the possibility of coronary vasospasm as the cause of acute MI or OHCA. Repeated measurements of troponin and coronary angiography were useful for the diagnosis of coronary vasospasm in the present case.>
Keywords: Cardiac arrest, Vasospasm, Myocardial infarction
Introduction
Coronary vasospasm plays an important role in the pathogenesis of rest angina, exertional angina, acute myocardial infarction (MI), and out-of-hospital cardiac arrest (OHCA). We occasionally experience the patients with acute MI in whom emergency coronary angiogram reveals no obstructive coronary stenosis, which is regarded as myocardial infarction with non-obstructive coronary arteries (MINOCA) [1,2]. Furthermore, we occasionally cannot identify the culprit lesion of MI, although the patients have multiple intermediate coronary stenosis. It is very rare that emergency coronary angiogram reveals coronary vasospasm, i.e., coronary occlusion that disappear by nitrates, at the culprit lesion of MI.
Case report
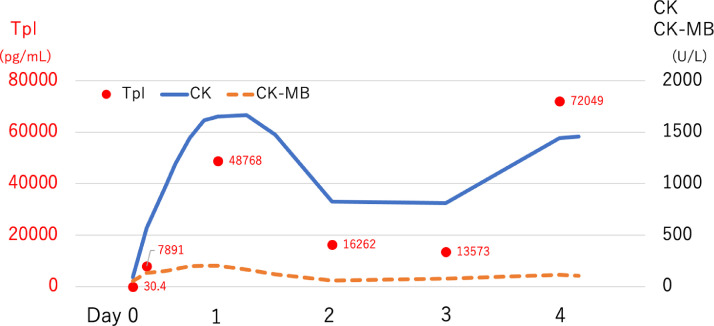
A 60-year-old man was found lying on the platform of railway station and received cardiopulmonary resuscitation with multiple electrical defibrillations for ventricular fibrillation (VF) using automated external defibrillator. He was transported to our hospital by an emergency medical service. He had pulseless electrical activity (PEA) on arrival to our hospital. His heart rhythm changed to VF by the injection of adrenaline, which was not terminated even by multiple electrical defibrillations under mechanical ventilation. VF was finally terminated after the initiation of circulation support by percutaneous cardiopulmonary support device (PCPS). ST elevation in aVR lead and ST depression in inferior and lateral leads were detected on 12-lead electrocardiogram (Fig. 1). The elevation of troponin I was detected. Suspecting acute MI, emergency coronary angiography was performed; however, it could not identify the culprit lesion of MI (Fig. 2A). Having reduced left ventricular ejection fraction (35%), intra-aortic balloon pumping (IABP) was inserted. The diagnosis of acute MI was made according to the time-course in the elevation of troponin I (Fig. 3).
Fig. 1.
Electrocardiogram.
ST-segment elevation in aVR lead and ST-segment depression in leads V4 to V6 were observed on arrival (Day0). There was no significant change in the electrocardiogram thereafter even when re-elevation of troponin was detected on the 4th day (Day4).
Fig. 2.
Coronary angiography.
Emergency coronary angiography on arrival could not identify the culprit lesion of MI, although there were multiple intermediate stenotic lesions (A). Diffuse severe stenosis in right coronary artery and total occlusion (red arrow) in the left circumflex coronary artery were detected on the 4th day when re-elevation of troponin was detected (B), which disappeared by the injection of isosorbide dinitrate (C) (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.).
Fig. 3.
Serial changes in the cardiac enzymes.
Re-elevation of troponin I (TpI) and creatinine kinase (CK) were detected on the 4th day.
He had been treated for hypertension, hypercholesterolemia, hyperuricemia, and heart failure. Precise examinations on heart failure in other hospital reached the diagnosis of old inferior MI 6 months ago. He received percutaneous coronary intervention (PCI) of right coronary artery. He was taking warfarin for paroxysmal atrial fibrillation.
After catheterization, we started his treatment in intensive care unit. On the 4th day after admission, re-elevation of troponin I was recorded (Fig. 3), although there was no significant change in the electrocardiogram (Fig. 1). We performed coronary angiography again and found diffuse severe stenosis in the right coronary artery and total occlusion in the left circumflex coronary artery (Fig. 2B, red arrow). However, those lesions disappeared by the injection of isosorbide dinitrate (Fig. 2C). Therefore, we reached the diagnosis of acute MI due to coronary vasospasm. We started continuous intravenous infusion of glycerin trinitrate. PCPS was removed on the 5th day and IABP was removed on the 7th day. His conditions remained stable without VF recurrence or re-elevation of troponin I thereafter during hospitalization. After discharge, he had no recurrence of VF under the treatment with nitroglycerin.
Discussion
This is a case report of the patient with OHCA and acute MI with unclear culprit lesion but was diagnosed later to have vasospasm as the cause of MI by the detection of troponin re-elevation and repeated coronary angiography during hospitalization.
Although 30-50% of MINOCA patients have been reported positive for coronary vasospasm provocation test with acetylcholine [3,4], it would not always be correct to diagnosis those patients as having acute MI caused by vasospasm. Vasospasm has been reported to cause plaque rupture and formation of thrombi [5], increased thrombin generation [6], and activation of plasminogen activator inhibitor 1 [7]. Thrombin generated by coronary vasospasm promotes the release of adhesion molecules from activated platelets [8]. Therefore, coronary vasospasm causes hyper-coagulation, decreased fibrinolytic activity, and activation of platelets and adhesion molecules, resulting in a thrombophilic state. On the other hand, thrombus is well-known to induce vasoconstriction [9]. Therefore, coronary vasospasm can be both cause and result of coronary thrombosis, which makes it difficult to diagnose correctly the acute MI caused by coronary vasospasm. Vasospasm provocation test in the acute phase of MI may be positive due to the residual thrombus at the culprit lesion; therefore, the positive finding cannot exclude the presence of disrupted plaque at the culprit. However, in the present case, we did not perform provocation test at the first catheterization because we thought one of intermediate stenoses might be the culprit of MI or the elevation of troponin might be secondary to VF; furthermore, it was difficult to perform provocation test in the acute phase of MI patients with PCPS and IABP.
Since the guideline [10] indicates that calcium channel antagonist alone or in combination with long-acting nitrates are useful to reduce the frequency of vasospastic angina, we should always take into consideration the possibility of coronary vasospasm as the cause of acute MI or OHCA. In the present case, oral medications were difficult to use due to severe hypoxic-ischemic encephalopathy; therefore, nitroglycerin transdermal patches alone were used, by which re-elevation of troponin I was prevented thereafter.
According to JCS/JHRS 2019 Guideline on Non-Pharmacotherapy of Cardiac Arrhythmia, the recommendation of implantable cardioverter defibrillator (ICD) for VF due to coronary vasospasm is regarded class IIa when the medical treatment is ineffective and it is regarded class IIb when the medical treatment is effective; however, it is regarded class III in the patients with severe hypoxic-ischemic encephalopathy [11]. Therefore, we decided not in implant ICD in the present case.
In conclusion, coronary vasospasm may be one of important causes of acute MI or OHCA, which is difficult to be diagnosed correctly. Repeated measurements of troponin and coronary angiography identified the cause of acute MI as coronary vasospasm in the present case.
Declaration of Competing Interest
Ueda Y received research grants from Abbott Vascular, Pfizer, Bayer, Daiichi-Sankyo, Astellas, Shionogi, Sanofi, Ono, Nihon Kohden, Amgen Astellas, Actelion, Bristol-Myers Squibb, Medtronic, AstraZeneca, Otsuka, and Novartis, and lecture fees from Daiichi-Sankyo, MSD, Goodman, Sanofi, Mochida, Takeda, Kowa, Teijin, Astellas, Actelion, Bristol-Myers Squibb, AstraZeneca, Boston Scientific, Sumitomo Dainippon Pharma, Eisai, and Amgen Astellas. Koretsune Y received lecture fees from Daiichi Sankyo, Boehringer Ingelheim, Bayer, Bristol-Meyers Squibb, and Pfizer. Abe H received research grants from Daiichi Sankyo and Boehringer Ingelheim.
References
- 1.Vincent G.M., Anderson J.L., Marshall HW. Coronary spasm producing coronary thrombosis and myocardial infarction. N Engl J Med. 1983;309:220–223. doi: 10.1056/NEJM198307283090406. [DOI] [PubMed] [Google Scholar]
- 2.Bugiardini R., Bairey Merz C.N. Angina with “normal” coronary arteries: a changing philosophy. JAMA. 2005;293:477–484. doi: 10.1001/jama.293.4.477. [DOI] [PubMed] [Google Scholar]
- 3.Ong P., Athanasiadis A., Hill S., Vogelsberg H., Voehringer M., Sechtem U. Coronary artery spasm as a frequent cause of acute coronary syndrome: the CASPAR (coronary artery spasm in patients with acute coronary syndrome) study. J Am Coll Cardiol. 2008;52:523–527. doi: 10.1016/j.jacc.2008.04.050. [DOI] [PubMed] [Google Scholar]
- 4.Nakayama N., Kaikita K., Fukunaga T., Matsuzawa Y., Sato K., Horio E., Yoshimura H., Mizobe M., Takashio S., Tsujita K., Kojima S., Tayama S., Hokimoto S., Sakamoto T., Nakao K., et al. Clinical features and prognosis of patients with coronary spasm-induced non-ST-segment elevation acute coronary syndrome. J Am Heart Assoc. 2014;3 doi: 10.1161/JAHA.114.000795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin C.S., Penha P.D., Zak F.G., Lin JC. Morphodynamic interpretation of acute coronary thrombosis, with special reference to volcano-like eruption of atheromatous plaque caused by coronary artery spasm. Angiology. 1988;39:535–547. doi: 10.1177/000331978803900607. [DOI] [PubMed] [Google Scholar]
- 6.Oshima S., Yasue H., Ogawa H., Okumura K., Matsuyama K. Fibrinopeptide a is released into the coronary circulation after coronary spasm. Circulation. 1990;82:2222–2225. doi: 10.1161/01.cir.82.6.2222. [DOI] [PubMed] [Google Scholar]
- 7.Misumi I., Ogawa H., Masuda T., Sakamoto T., Okumura K., Yasue H. Increased plasma plasminogen activator inhibitor activity after coronary spasm. Int J Cardiol. 1993;41:21–29. doi: 10.1016/0167-5273(93)90133-2. [DOI] [PubMed] [Google Scholar]
- 8.Kaikita K., Ogawa H., Yasue H., Sakamoto T., Suefuji H., Sumida H., Okumura K. Soluble P-selectin is released into the coronary circulation after coronary spasm. Circulation. 1995;92:1726–1730. doi: 10.1161/01.cir.92.7.1726. [DOI] [PubMed] [Google Scholar]
- 9.Zeiher A.M., Schachinger V., Weitzel S.H., Wollschlager H., Just H. Intracoronary thrombus formation causes focal vasoconstriction of epicardial arteries in patients with coronary artery disease. Circulation. 1991;83:1519–1525. doi: 10.1161/01.cir.83.5.1519. [DOI] [PubMed] [Google Scholar]
- 10.Amsterdam E.A., Wenger N.K., Brindis R.G., Casey D.E., Jr, Ganiats T.G., Holmes D.R., Jr, Jaffe A.S., Jneid H., Kelly R.F., Kontos M.C., Levine G.N., Liebson P.R., Mukherjee D., Peterson E.D., Sabatine M.S., et al. 2014 AHA/ACC guideline for the management of patients with non-st-elevation acute coronary syndromes: a report of the american college of cardiology/american heart association task force on practice guidelines. J Am Coll Cardiol. 2014;64:e139–e228. doi: 10.1016/j.jacc.2014.09.017. Erratum in: J Am Coll Cardiol. 2014;64:2713-4. [DOI] [PubMed] [Google Scholar]
- 11.Nogami A., Kurita T., Abe H., Ando K., Ishikawa T., Imai K., Usui A., Okishige K., Kusano K., Kumagai K., Goya M., Kobayashi Y., Shimizu A., Shimizu W., Shoda M., et al. JCS/JHRS 2019 Guideline on Non-Pharmacotherapy of Cardiac Arrhythmias. Circ J. 2021 doi: 10.1253/circj.CJ-20-0637. In press. [DOI] [PubMed] [Google Scholar]