Abstract
Background
Studies show smoking and vaping behaviors increase risk of contracting and worse symptoms of COVID-19. This study examines whether past 30-day youth and young adult users of marijuana, e-cigarettes, and cigarettes self-reported changes in their use of these substances due to the COVID-19 pandemic; and cross-sectional associations between perceived stress, nicotine or marijuana dependence, and COVID-19–related changes in use.
Methods
Participants were 709 past 30-day self-reported substance users from the Texas Adolescent Tobacco and Marketing Surveillance study (TATAMS; mean age = 19; 58% female; 38% Hispanic, 35% white). Multiple logistic regression models assessed cross-sectional associations between perceived stress and dependence and increased, decreased, or sustained past 30-day use of marijuana, e-cigarettes, and cigarettes due to COVID-19 (e.g., “Has your marijuana use changed due to the COVID-19 outbreak?”). Covariates included age, race/ethnicity, socio-economic status (SES), dependence (exposure: stress), and stress (exposure: dependence).
Results
Most participants reported sustained (41%, 43%, 49%) or increased (37%, 34%, 25%) use of marijuana, e-cigarettes, and cigarettes due to COVID-19, respectively. Participants who reported symptoms of dependence were significantly more likely than their non-dependent peers to report increasing their marijuana (AOR: 1.66; 95% CI: 1.15–2.39) and e-cigarette (AOR: 2.57; 95% CI: 1.38–4.77) use. Those who reported higher perceived stress were significantly more likely to report increasing their marijuana use (AOR: 1.55; 95% CI: 1.01–2.42).
Conclusions
Most youth and young adults did not decrease their substance use amid a global, respiratory disease pandemic. Health messaging and interventions that address the health effects of smoking and vaping as well as factors like stress and dependence that may be barriers to decreasing use are vital in curbing the COVID-19 pandemic.
Keywords: tobacco, vaping, electronic nicotine delivery systems, marijuana use, cannabis, stress, psychologic, adolescent, young adult
Introduction
The Coronavirus Disease 2019 (COVID-19) pandemic has become pervasive in the lives of youth and young adults in the U.S., a population already facing substantial public health threats. Chiefly among these threats are smoking and vaping, especially marijuana, electronic cigarette (e-cigarette), and cigarette use which are the most common types of substance use by young people, after alcohol. 1 Emerging research supports substance use as an important risk factor for COVID-19 infection. 2 A recent systematic review found tobacco use, specifically cigarette smoking or chewing tobacco, as a cause of more severe symptoms of COVID-19 infection. 3 Evidence of the relationship between e-cigarette use and COVID-19 is limited, although it has been established that e-cigarette use increases the risk of severe lung disease, 4 and emerging studies similarly show e-cigarette use increases risk of contracting COVID-19 and/or experiencing more severe symptoms.5-7 Research has shown that regular marijuana use, much like smoking and vaping, diminishes respiratory health since marijuana may contain damaging toxins and is inhaled via modes similar to tobacco (e.g., vaping marijuana). 8
Given that smoking and vaping behaviors have significant potential to adversely impact COVID-19 outcomes, understanding how youth and young adults have changed their smoking and vaping behaviors due to the COVID-19 pandemic and factors related to these changes is vital. Prior to the COVID-19 pandemic, the U.S. was engulfed in an epidemic of e-cigarette use among youth and young adults, 9 and EVALI (e-cigarette and vaping associated lung injury) cases were emerging across the U.S. 10 However some studies have shown declines in e-cigarette use among youth and young adults since the start of the COVID-19 pandemic, which may be due to a number of factors including greater perceived risk of e-cigarette use and diminished access to e-cigarettes.11-13 Yet, these same studies show that e-cigarette use remains prevalent, and despite declines in use, some youth and young adults have increased their use, too, amid COVID-19.11-13
This study sought to examine the prevalence of self-reported COVID-19–related changes in past 30-day marijuana, e-cigarette, and cigarette use behaviors among a sample of youth and young adult past 30-day users of these substances in Texas. We extend previous research by examining, not only e-cigarette use, but 2 additional smoking behaviors, marijuana use and cigarette use, which are less studied in this context. We also examined changes in use among more recent, regular substance users, past 30-day users, who have greater adverse health-related risks compared to lighter users. 14 We investigated perceived stress and substance-specific dependence as potential correlates of COVID-19–related changes in marijuana, e-cigarette, and cigarette use, controlling for important demographic variables. The COVID-19 pandemic has been cited as a potentially impactful disruption in the e-cigarette epidemic. 15 Both greater stress and dependence are known correlates of substance use; 16 thus, this study sought to examine how these are associated with COVID-19-specific changes in substance use.
Methods
Participants
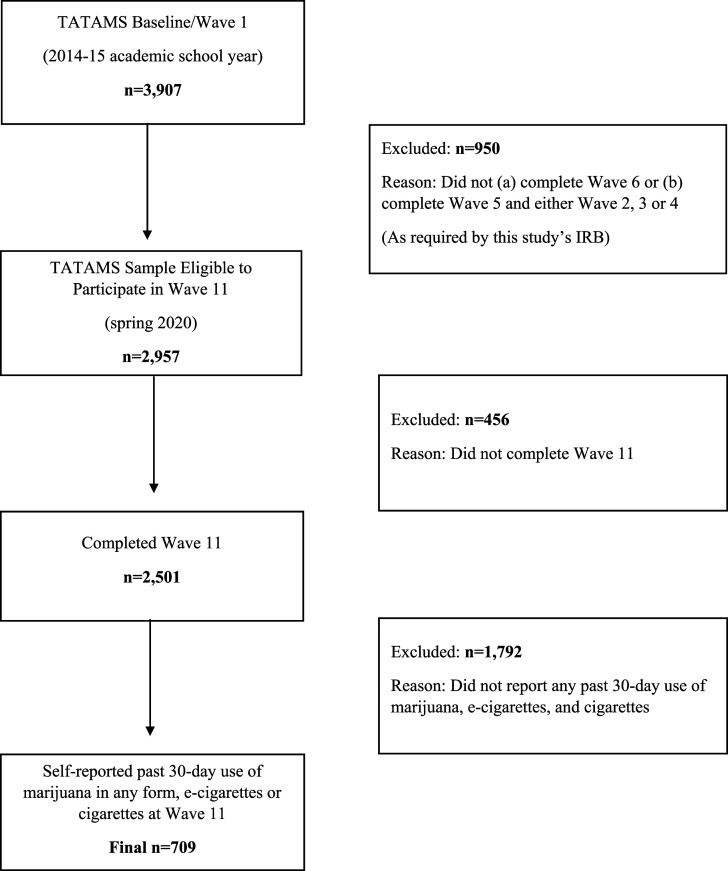
Participants were 709 youth and young adult (ages 16–24) past 30-day marijuana, e-cigarette, and/or cigarette users from the Texas Adolescent Tobacco and Marketing Surveillance study (TATAMS). Data were collected in spring 2020 via an online survey. Participants received a $25 gift card incentive. Detailed information about the TATAMS study has been previously published. 17 A total of 2501 TATAMS participants completed the spring 2020 survey (84% response rate). Past 30-day marijuana (22.8%; n = 570), e-cigarette (10.9%; n = 273), and/or cigarette (4.3%; n = 109) users were included in this study for a total sample size of 709. Substance use categories were not mutually exclusive. Sample selection is detailed in Figure 1.
Figure 1.
Study sample selection.
Measures
Changes in past 30-day marijuana, e-cigarette, and cigarette use behaviors, attributed to COVID-19, were assessed among past 30-day users of each product by asking participants, “Has your [product] use changed due to the COVID-19 outbreak?” Response options were “I use [product] more,” “I use [product] less,” and “My [product] use has not changed.” This question was asked for each separately: marijuana, e-cigarette, and cigarette use. Prior to being asked these questions, participants received this prompt, “Coronavirus (COVID-19) is an infectious disease that was first identified in late 2019. The outbreak of COVID-19 began in Texas in early 2020 and has affected the daily lives of people all over the U.S. and the world. Please answer the next questions about how the outbreak of COVID-19 has affected you.”
Perceived stress was assessed via the 10-item Perceived Stress Scale (PSS) 18 which asks, “In the last month, how often have you … been upset because of something that happened unexpectedly, felt that you were unable to control the important things in your life, etc.” Response options were 0 = never, 1 = almost never, 2 = sometimes, 3 = fairly often, and 4 = very often. Scores were summed across the ten items with possible scores ranging 0–40. Participants who scored 0–13 were considered to have “low” stress; 14–26 was considered “moderate” stress, and 27–40 “high” stress, based on validated methods of operationalization. 18
Marijuana dependence was assessed via 9 items from the National Survey on Drug Use and Health 19 based on substance use disorder diagnostic criteria listed in DSM-5. The criteria asked were as follows: spent a great deal of time over a period of a month or more (1) getting, using, or (2) getting over the effects of marijuana, (3) used marijuana more often than intended or was unable to keep set limits on marijuana use, (4) needed to use marijuana more than before to get desired effects or (5) noticed that the same amount of marijuana use had less effect than before, (6) inability to cut down or stop using marijuana every time tried or wanted to, (7) continued to use marijuana even though it was causing problems with emotions, nerves, mental health, or (8) physical problems, and (9) marijuana use reduced or eliminated involvement or participation in important activities. Response options were “yes” and “no.” Participants were considered marijuana dependent if they responded “yes” to 3 or more of the criteria symptoms.
The 10-item Hooked on Nicotine Checklist (HONC) 20 was used to assess dependence on e-cigarettes and cigarettes. Participants were asked “Have you ever tried to quit, but couldn’t,” “Do you smoke (or use e-cigarettes) now because it is really hard to quit?” etc. Response options were “yes” and “no.” The checklist was product-specific such that past 30-day e-cigarette users were asked to answer only about their use of e-cigarettes, and past 30-day cigarette users were asked to answer only about their use of cigarettes. Users of both e-cigarettes and cigarettes answered the HONC twice, once for each product separately. Participants who responded “yes” to one or more items were considered dependent.
Demographic variables included age (ranging 16–24), biological sex (male or female), race/ethnicity (Hispanic or Latino/a, non-Hispanic white, non-Hispanic black or African American, or non-Hispanic other including Asian, American Indian or Alaska Native, and Native Hawaiian or Other Pacific Islander), and socio-economic status (SES). Socio-economic status was assessed by asking “In terms of income, what best describes your family’s standard of living in the home where you live most of the time?” Response options “Just getting by,” “Nearly poor” and “Poor” were considered “low” SES; “Living comfortably” was “middle” SES; and “Very well off” was “high” SES.
Statistical Analyses
Descriptive statistics were computed for the sample, by past 30-day substance use group (Table 1). Multivariable logistic regression models were conducted to examine associations between primary exposures (1) perceived stress and (2) substance-specific dependence (e.g., marijuana dependence for marijuana use changes) and COVID-19–related changes in substance use behaviors (Table 2). The behavioral outcomes were as follows: (1) increasing use (compared to unchanged or decreased use), (2) decreasing use (compared to unchanged or increased use), and (3) unchanged use (compared to increasing or decreasing use). These 3 outcomes were assessed for each of the 3 types of substance use: marijuana, e-cigarettes, and cigarettes (9 separate models). We chose to compare 2 categories (versus 3) (e.g., unchanged use vs decreased + increased use) at one time due to sample size limitations and to achieve more stable estimates. All estimates are adjusted for all other variables in the model: age, sex, race/ethnicity, SES, dependence, and stress. Analyses were conducted using STATA 14.0.
Table 1.
Descriptive Statistics (TATAMS, Wave 11; Spring 2020, n = 2501).
| Past 30-day any substance use (n = 709; 28.35%) | Past 30-day marijuana use (n = 570; 22.80%) | Past 30-day e-cigarette use (n = 273; 10.92%) | Past 30-day cigarette use (n = 109; 4.36%) | |
|---|---|---|---|---|
| Mean Age (range: 16–24) | 19.93 (1.44) | 19.92 (1.45) | 19.82 (1.41) | 20.33 (1.30) |
| Sex | ||||
| Male | 305 (43.02%) | 234 (41.05%) | 132 (48.35%) | 54 (49.54%) |
| Female | 404 (56.98%) | 336 (58.95%) | 141 (51.65%) | 55 (50.46%) |
| Race/Ethnicity | ||||
| Hispanic/Latino | 270 (38.08%) | 227 (39.75%) | 75 (27.47%) | 43 (39.45%) |
| Non-Hispanic white | 251 (35.40%) | 177 (31.00%) | 145 (53.11%) | 40 (36.70%) |
| Non-Hispanic black | 93 (13.12%) | 86 (15.06%) | 11 (4.03%) | 6 (5.50%) |
| Non-Hispanic other a | 95 (13.40%) | 81 (14.19%) | 42 (15.38%) | 20 (18.35%) |
| SES b | ||||
| Low | 198 (27.93%) | 167 (29.30%) | 60 (21.98%) | 36 (33.03%) |
| Middle | 439 (61.92%) | 348 (61.05%) | 176 (64.47%) | 61 (55.96%) |
| High | 72 (10.16%) | 55 (9.65%) | 37 (13.55%) | 12 (11.01%) |
| Perceived stress c | ||||
| Low | 175 (24.68%) | 133 (23.33%) | 77 (28.21%) | 15 (13.76%) |
| Moderate | 441 (62.20%) | 357 (62.63%) | 159 (58.24%) | 74 (67.89%) |
| High | 91 (12.83%) | 78 (13.68%) | 35 (12.82%) | 20 (18.35%) |
| Substance-specific dependence d | ||||
| No | 356 (50.21%) | 375 (65.79%) | 87 (31.87%) | 37 (33.94%) |
| Yes | 352 (49.65%) | 193 (33.86%) | 186 (68.13%) | 72 (66.06%) |
| Marijuana use changes e | ||||
| Unchanged | 233 (40.88%) | |||
| Increased | 212 (37.19%) | |||
| Decreased | 124 (21.75%) | |||
| E-cigarette use changes f | ||||
| Unchanged | 116 (42.49%) | |||
| Increased | 93 (34.07%) | |||
| Decreased | 62 (22.71%) | |||
| Cigarette use changes g | ||||
| Unchanged | 54 (49.54%) | |||
| Increased | 27 (24.77%) | |||
| Decreased | 28 (25.69%) | |||
aOther race/ethnicity includes Asian, American Indian or Alaska Native, and Native Hawaiian or Other Pacific Islander.
b“In terms of income, what best describes your family’s standard of living in the home where you live most of the time?” Response options: “Just getting by,” “Nearly poor” and “Poor” = “low” SES; “Living comfortably” = “middle” SES; and “Very well off” = “high” SES.
c10-item Perceived Stress Scale (PSS): “In the last month, how often have you … been upset because of something that happened unexpectedly, felt that you were unable to control the important things in your life, etc.” Response options: 0 = never, 1 = almost never, 2 = sometimes, 3 = fairly often, and 4 = very often. Scores summed across 10 items with possible scores ranging 0–40. Score 0–13 = “low” stress; 14–26 = “moderate” stress; 27–40 = “high” stress.
dMarijuana dependence assessed via 9 items from the National Survey on Drug Use and Health with those endorsing 3 or more items considered dependent. Cigarette and e-cigarette dependence were assessed, separately, via the 10-item Hooked on Nicotine Checklist (HONC): “Have you ever tried to quit, but couldn’t,” “Do you smoke (or use e-cigarettes) now because it is really hard to quit?” etc. Not dependent= “no” to 10 items; dependent = “yes” to at least one item.
e“Has your marijuana use changed due to the COVID-19 outbreak? Response options: “I use marijuana more,” “I use marijuana less” and “My marijuana use has not changed.”
f“Has your e-cigarette use changed due to the COVID-19 outbreak? Response options: “I use e-cigarettes more,” “I use e-cigarettes less” and “My e-cigarette use has not changed.”
g“Has your cigarette use changed due to the COVID-19 outbreak? Response options: “I use cigarettes more,” “I use cigarettes less” and “My cigarette use has not changed.”
Table 2.
Stress, Dependence, and COVID-19–related Changes in Marijuana, E-cigarette and Cigarette Use Behaviors among Past 30-day Users (TATAMS, Wave 11; Spring 2020).
| Marijuana use (n = 570) | E-cigarette use (n = 273) | Cigarette use (n = 109) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Unchanged a | Decreased b | Increased c | Unchanged a | Decreased b | Increased c | Unchanged a | Decreased b | Increased c | |
| AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI)< | AOR (95% CI) | AOR (95% CI) | |
| Stress (ref: low) d | |||||||||
| Moderate to high | .76 (.51–1.15) | .82 (.51–1.33) | 1.55* (1.01–2.42) | .87 (.49–1.53) | .86 (.45–1.65) | 1.37 (.73–2.56) | .49 (.14–1.72) | 1.11 (.26–4.65) | 2.36 (.47–11.88) |
| Dependence e | .54** (.37–.79) | 1.13 (.74–1.74) | 1.66** (1.15–2.39) | .43** (.25–.75) | 1.11 (.59–2.07) | 2.57** (1.38–4.77) | .43 (.17–1.10) | 1.44 (.51–4.04) | 2.31 (.73–7.29) |
| Age (16–24) | 1.00 (.88–1.12) | .96 (.84–1.11) | 1.02 (.90–1.15) | 1.03 (.85–1.24) | .81 (.66–1.00) | 1.08 (.89–1.32) | .98 (.70–1.37) | .95 (.65–1.38) | 1.05 (.71–1.56) |
| Female sex (ref: Male) | .95 (.66–1.35) | 1.02 (.67–1.55) | 1.03 (.71–1.48) | .86 (.51–1.44) | .96 (.53–1.74) | 1.24 (.72–2.13) | .41 (.18–.94) | 1.38 (.55–3.46) | 2.50 (.94–6.61) |
| Race/ethnicity (ref: white) | |||||||||
| Hispanic/Latino | 1.04 (.62–1.73) | .86 (.46–1.58) | 1.07 (.62–1.83) | 2.36 (.61–9.17) | .84 (.16–4.39) | .38 (.07–2.01) | .73 (.11–4.84) | 2.44 (.39–14.90) | .46 (.43–5.04) |
| Non-Hispanic black | .73 (.48–1.11) | .97 (.59–1.57) | 1.42 (.92–2.19) | 1.49 (.82–2.69) | 1.21 (.62–2.36) | .60 (.32–1.12) | 1.57 (.53–4.61) | .59 (.16–2.07) | .95 (.28–3.17) |
| Non-Hispanic other | .59 (.34–1.02) | .69 (.35–1.33) | 2.16** (1.27–3.66) | 1.05 (.47–2.33) | .69 (.26–1.80) | 1.20 (.55–2.67) | .49 (.15–1.59) | 1.12 (.33–3.82) | 2.27 (.62–8.32) |
| SES (ref: High) | |||||||||
| Middle | 1.07 (.59–1.95) | 2.18 (.94–5.03) | .56 (.31–1.02) | 1.92 (.86–4.30) | .77 (.34–1.77) | .66 (.30–1.44) | 2.83 (.65–12.31) | .29 (.06–1.31) | .89 (.18–4.35) |
| Low | .95 (.49–1.84) | 1.95 (.79–4.79) | .70 (.36–1.34) | 1.58 (.62–3.97) | .95 (.36–2.49) | .82 (.33–2.03) | 3.55 (.67–18.57) | .63 (.12–3.23) | .27 (.04–1.76) |
aAmong past 30-day users, participant selected “My [substance] use has not changed.” Unchanged use is compared to increased or decreased use.
bAmong past 30-day users, participant selected “I use [substance] less.” Decreased use is compared to unchanged or increased use.
cAmong past 30-day users, participant selected “I use [substance] more.” Increased use is compared to unchanged or decreased use.
d10-item Perceived Stress Scale (PSS): “In the last month, how often have you … been upset because of something that happened unexpectedly, felt that you were unable to control the important things in your life, etc.” Response options: 0 = never, 1 = almost never, 2 = sometimes, 3 = fairly often, and 4 = very often. Scores summed across 10 items with possible scores ranging 0–40. Score 0–13 = “low” stress; 14–26 = “moderate” stress; 27–40 = “high” stress.
eMarijuana dependence assessed via 9 items from the National Survey on Drug Use and Health with those endorsing 3 or more items considered dependent. Cigarette and e-cigarette dependence were assessed, separately, via the 10-item Hooked on Nicotine Checklist (HONC): “Have you ever tried to quit, but couldn’t,” “Do you smoke (or use e-cigarettes) now because it is really hard to quit?” etc. Not dependent = “no” to 10 items; dependent = “yes” to at least one item.
Boldface indicates statistical significance (* P ≤ .05 **P ≤ .01).
AOR, adjusted odds ratio: Adjusted for all other variables in the model; 95% CI, 95% confidence interval; SES, socio-economic status.
Results
Participants were 16–24 years of age (mean age: 19.9, SD: 1.44); 56.9% female; 38.1% Hispanic, 35.4% non-Hispanic white, 13.1% non-Hispanic black, and 13.4% other race/ethnicity.
The prevalence of past 30-day (current) marijuana use was 22.8%, 10.9% for e-cigarettes, and 4.3% for cigarettes. Of current marijuana users (n = 570), 40.8% of participants reported not changing their marijuana use due to the COVID-19 pandemic; 37.1% reported increasing their marijuana use; and 21.5% decreased their use. Similarly, current e-cigarette users (n = 273) reported unchanged (42.4%), increased (34.0%), and decreased (22.7%) e-cigarette use. Current cigarette users (n = 109) reported unchanged (49.5%), increased (24.7%), and decreased (25.6%) cigarette use.
Controlling for demographic characteristics and perceived stress, participants presenting with symptoms of substance-specific dependence were significantly more likely to report increasing use of marijuana (AOR: 1.66; 95% CI: 1.15–2.39) and e-cigarettes (AOR: 2.57; 95% CI: 1.38–4.77) due to the COVID-19 pandemic (compared to not changing or decreasing use), and significantly less likely to report unchanged marijuana (AOR: .54; 95% CI: .37–.79) and e-cigarette use (AOR: .43; 95% CI: .25–.75) (compared to increasing or decreasing use). Controlling for demographic characteristics and marijuana dependence, higher perceived stress was significantly associated with using marijuana more due to the COVID-19 pandemic (AOR: 1.55; 95% CI: 1.01–2.42). Youth and young adults who reported “other” race/ethnicity, compared to non-Hispanic white, were significantly more likely to report using marijuana more due to the COVID-19 pandemic (AOR: 2.16; 95% CI: 1.27–3.66).
Discussion
This study extends previous research examining COVID-19–related changes in smoking and vaping behaviors and factors associated with these changes among young people.11,21-23 We found that most (∼75%) youth and young adult current users of marijuana, e-cigarettes, and cigarettes reported either sustained or increased use due to COVID-19. This is consistent with studies of adult 23 and college student 21 cigarette and e-cigarette users, and studies of youth 24 and young adult 22 marijuana users. To our knowledge, this is the first study to report on past 30-day marijuana, e-cigarette, and cigarette behavior changes among youth, building on research by Gaiha et al. (2020) 11 that examined similar changes among youth and young adult lifetime e-cigarette users. Gaiha et al. (2020) 11 reported 56% of e-cigarette ever users changed their use since COVID-19, with the majority of changes being quitting e-cigarette use or reducing the amount of nicotine used. Fewer increased their nicotine use and increased their marijuana use. 11 This study’s greater prevalence of increased and sustained use, compared to decreased use may be due to our sample being more recent, regular users (past 30-day users compared to ever users). Our examination of current, popular substance use behaviors among young people amid the COVID-19 pandemic is key since this population is in an important transitional life stage where substance use behaviors are adopted and solidified. 25
In this study, substance-specific dependence especially emerged as an important factor associated with sustained and increased use of marijuana and e-cigarettes. This finding is consistent with Sokolovsky et al. (2021) 21 and Gaiha et al. (2020) 11 who both reported significant relationships between nicotine dependence and continuing or increasing nicotine use. Notably, “other” race/ethnicity, which includes multi-racial/ethnic, Asians, American Indians or Alaska Natives, and Native Hawaiians or Pacific Islanders, compared to white race/ethnicity was significantly associated with increasing marijuana use due to COVID-19. This highlights an important health disparity since young people belonging to these populations, like American Indians, historically have higher rates of marijuana and other drug use compared to their peers, 26 and crises like COVID-19 may exacerbate these disparities. More research is needed to investigate relationships between stress, dependence, and other potential influencing factors, like race/ethnicity and cultural factors, and substance use changes related to socio-economic crises, or other emerging public health events.
These findings have implications for public health messaging and intervention. Studies have shown that smoking and vaping increase risk of contracting COVID-19 and more severe symptoms,5,6 yet the majority of users (74–78%) in this study sustained or increased their use due to COVID-19. These findings suggest a need for greater, more effective health messaging about the effects of smoking and vaping on the risk of contracting COVID-19 and the severity of symptoms that result, as well as on lung and respiratory health in general, especially via media outlets like social media that have a large young audience. A recent study reported that e-cigarette users believed their use may be protective against COVID-19, for example, believing that heat from e-cigarettes kills COVID-19. 27 Misinformation like this is easily and widely spread on social media and other online media. 7 Additional support for e-cigarette and marijuana cessation services and prevention may be required, as well, given the findings specific to dependence here, and stress management should be incorporated into marijuana cessation efforts given that higher stress, when controlling for dependence, was significantly associated with increased marijuana use in this study. Another study showed that adult past 6-month cigarette smokers reporting higher perceived stress, were more likely to report increased cigarette smoking since hearing about COVID-19. 28 The present study did not find a statistically significant association between stress and changes in cigarette use which may be due to our younger sample, who use cigarettes less compared to adults, 29 and less compared to e-cigarettes and marijuana. Additionally, most (>70%) of our sample reported moderate to high stress compared to low stress which is common in these age groups, and thus, stress may be less impactful on substance use behaviors in youth and young adults. Finally, findings support the need for health messages and programs to be culturally tailored to address health disparities related to race/ethnicity since “other” race/ethnicity was the only socio-demographic factor that was significantly associated with increasing marijuana use in this study.
Limitations
Data were collected via self-report. We asked participants whether their substance use had increased, decreased, or remained the same, and we did not assess the degree of change. However, participants did attribute self-reported changes to the COVID-19 pandemic which is an important distinction of our study that allowed us to discount other potential reasons for changes in substance use. In addition, data for this study were collected early in the COVID-19 pandemic. COVID-19 was declared a pandemic on March 11, 2020 by the World Health Organization, and data for this study were collected in April through June 2020. Study findings are reflective of youth and young adults’ behavioral responses early in the pandemic, and future research is needed to examine changes in substance use behavior in later stages of the COVID-19 pandemic. This study is cross-sectional, so the temporal relationship between stress and dependence and changes in substance use was not assessed. However, since we asked participants to report how their substance use had changed due to COVID-19, and the onset of COVID-19 was so recent at the time of data collection, we felt that examining stress and dependence at this same time (i.e., cross-sectionally) was appropriate. Future research should examine changes in stress, dependence, and substance use from before to early and later in the pandemic, as well as interrelationships among these.
Conclusions
Youth and young adult current substance users in this study attributed changes in their use to COVID-19, and dependence and stress were significant factors associated with increased and/or unchanged e-cigarette and/or marijuana use amid the pandemic. As substance use in young people continues to rise, 1 and COVID-19 variants emerge, 30 as well other potential respiratory infections (e.g., EVALI; e-cigarette and vaping associated lung injury), 10 health messaging and interventions that address the health effects of substance use and factors that may be barriers to decreasing or stopping use are vital.
Footnotes
Author Contributions: All authors contributed to the conceptualization and study design. MBH, SLC and AS oversaw data collection. SC conducted the statistical analysis and wrote the first draft of the manuscript. All authors contributed to the interpretation of results and conclusions made. All authors contributed to and approved the final manuscript.
Declaration of Conflicting Interests: Authors SLC, DSM, EJM and MBH are consultants in litigation involving the vaping industry. Other authors have no conflicts of interest to disclose.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by grant number R01-CA239097 from the National Cancer Institute.
ORCID iD
Stephanie L. Clendennen https://orcid.org/0000-0002-3890-9733
References
- 1.Schulenberg J, Johnston L, O’Malley P, Bachman J, Miech R, Patrick M. Monitoring the Future National Survey Results on Drug Use, 1975-2019: Volume II, College Students and Adults Ages 19-60; 2020. [Google Scholar]
- 2.Wang QQ, Kaelber DC, Xu R, Volkow ND. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol Psychiatr. 2021;26(1):30-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta AK, Nethan ST, Mehrotra R. Tobacco use as a well-recognized cause of severe COVID-19 manifestations. Respir Med. 2020;176:106233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhatta DN, Glantz SA. Association of e-cigarette use with respiratory disease among adults: A longitudinal analysis. Am J Prev Med. 2020;58(2):182-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaur G, Lungarella G, Rahman I. SARS-CoV-2 COVID-19 susceptibility and lung inflammatory storm by smoking and vaping. J Inflamm. 2020;17(1):21-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simons D, Shahab L, Brown J, Perski O. The association of smoking status with SARS‐CoV‐2 infection, hospitalization and mortality from COVID‐19: A living rapid evidence review with Bayesian meta‐analyses (version 7). Addiction. 2020;116(6):1319-1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Soule EK, Kheradmand F, Eissenberg T. Health practitioners should caution about misinformation and association of adverse effects of electronic cigarette use and COVID-19. Preventive Medicine Reports. 2020;20:101255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;370(23):2219-2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Surgeon General’s Advisory on E-cigarette Use Among Youth. Centers for Disease Control and Prevention website. Updated March 4, 2021. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/surgeon-general-advisory/index.html. Accessed November 12, 2021 [Google Scholar]
- 10.E-cigarette Use Associated Lung Injury . Centers for Disease Control and Prevention website. Updated March 4, 2021. https://www.cdc.gov/mmwr/ecigarette_lung_injury.htmlr. Accessed July 15, 2021 [Google Scholar]
- 11.Gaiha SM, Lempert LK, Halpern-Felsher B. Underage youth and young adult e-cigarette use and access before and during the coronavirus disease 2019 pandemic. JAMA network open. 2020;3(12):e2027572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choi BM, Abraham I. The decline in e-cigarette use among youth in the United States—an encouraging trend but an ongoing public health challenge. JAMA Network Open. 2021;4(6):e2112464. [DOI] [PubMed] [Google Scholar]
- 13.Wang TW, Gentzke AS, Neff LJ, et al. Characteristics of e-cigarette use behaviors among US youth, 2020. JAMA Network Open. 2021;4(6):e2111336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schulte MT, Hser Y-I. Substance use and associated health conditions throughout the lifespan. Publ Health Rev. 2013;35(2):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stokes AC. Declines in electronic cigarette use among US youth in the era of COVID-19—a critical opportunity to stop youth vaping in its tracks. JAMA Network Open. 2020;3(12):e2028221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.U.S. Department of Health and Human Services . Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2012. [Google Scholar]
- 17.Pérez A, Harrell MB, Malkani RI, et al. Texas adolescent tobacco and marketing surveillance system’s design. Tobacco Regul Sci. 2017;3(2):151-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385-396. [PubMed] [Google Scholar]
- 19.National Survey on Drug Use and Health (NSDUH) . Substance Abuse and Mental Health Services Administration website. https://www.samhsa.gov/data/data-we-collect/nsduh-national-survey-drug-use-and-health. https://www.samhsa.gov/data/data-we-collect/nsduh-national-survey-drug-use-and-health. Accessed July 15, 2021. [PubMed] [Google Scholar]
- 20.DiFranza JR, Savageau JA, Fletcher K, et al. Measuring the loss of autonomy over nicotine use in adolescents: The DANDY (development and assessment of nicotine dependence in youths) study. Arch Pediatr Adolesc Med. 2002;156(4):397-403. [DOI] [PubMed] [Google Scholar]
- 21.Sokolovsky AW, Hertel AW, Micalizzi L, White HR, Hayes KL, Jackson KM. Preliminary impact of the COVID-19 pandemic on smoking and vaping in college students. Addict Behav. 2021;115:106783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Graupensperger S, Fleming CB, Jaffe AE, Rhew IC, Patrick ME, Lee CM. Changes in young adults’ alcohol and marijuana use, norms, and motives from before to during the COVID-19 pandemic. J Adolesc Health. 2021;68(4):658-665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.White AM, Li D, Snell LM, et al. Perceptions of tobacco product-specific COVID-19 risk and changes in tobacco use behaviors among smokers, E-cigarette users, and dual users. Nicotine Tobacco Res. 2021;23(9):1617-1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dumas TM, Ellis W, Litt DM. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J Adolesc Health. 2020;67(3):354-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ling PM, Glantz SA. Why and how the tobacco industry sells cigarettes to young adults: Evidence from industry documents. Am J Publ Health. 2002;92(6):908-916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Swaim RC, Stanley LR. Substance use among American Indian youths on reservations compared with a national sample of US adolescents. JAMA Network Open. 2018;1(1):e180382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Soule EK, Mayne S, Snipes W, Guy MC, Breland A, Fagan P. Impacts of COVID-19 on electronic cigarette purchasing, use and related behaviors. Int J Environ Res Publ Health. 2020;17(18):6762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kalkhoran SM, Levy DE, Rigotti NA. Smoking and E-cigarette use among US adults during the COVID-19 pandemic. Am J Prev Med 2021;00499-2. doi: 10.1016/j.amepre.2021.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cornelius ME, Wang TW, Jamal A, Loretan CG, Neff LJ. Tobacco product use among adults—United States, 2019. Morb Mortal Weekly Rep. 2020;69(46):1736-1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Variants of the Virus . Centers for Disease Control and Prevention website. Updated June 28, 2021. https://www.cdc.gov/coronavirus/2019-ncov/variants/variant.html. Accessed July 15, 2021 [Google Scholar]