Abstract
Background:
Analgesic trade-off preferences, or the relative preference for pain relief vs. risk aversion, shape parents’ decisions to give prescription opioids to their children. These preferences may be influenced by personal experiences and societal factors.
Aim:
To examine whether parental analgesic trade-off preferences and opioid decision-making have shifted toward risk aversion during the opioid crisis in the United States.
Methods:
We conducted a secondary analysis of the preoperative survey data of parents from a single U.S. pediatric hospital whose children aged 5-17 years were to undergo painful surgery in 2013 (Time 1) or 2017/2019 (Time 2). Surveys assessed parents’ analgesic trade-off preference (−12 or risk averse to +12 or pain relief preferent, scores around 0=ambivalent) and their hypothetical decisions to give a prescribed opioid to a child in pain.
Results:
Data from 847 parents were included (Time 1 n=361; Time 2 n=486). Parents at Time 2 were significantly more risk averse compared to Time 1 (adj.β −0.84 [95% CI −1.09, −0.60]). Parents at Time 2 were more than twice as likely to be risk averse or ambivalent (OR 2.17 [95% CI 1.62, 2.91]). There was a significant interaction effect of Time*Preference on parents’ decision to give the opioid (adj.OR 1.09 [95% CI 1.03, 1.16]). At Time 2, parents who were ambivalent or risk averse were less likely than those who preferred to relieve pain to administer the prescribed opioid (OR 0.57 [95% CI 0.37, 0.89]). In contrast, there was no association between preference group and the opioid decision at Time 1.
Conclusion:
Findings suggest that parents of children scheduled for painful surgery at our pediatric hospital have become more analgesic risk averse during the past decade. Parents’ analgesic trade-off preferences may influence their decisions to administer prescribed opioids after surgery, which may contribute to children’s pain outcomes.
Keywords: Parents, opioid analgesics, decision making, children, pain management, opioid epidemic
Introduction
Despite the inherent risks, the use of prescription opioids remains an important strategy to manage severe, acute postoperative pain in children and adolescents.1,2 However, the ongoing opioid crisis may have impacted public sentiment regarding opioid analgesics in ways that affect pediatric pain management. Increasing and alarming rates of prescription opioid-related adverse events, misuse, deaths, and opioid use disorder have elicited widespread attention from healthcare providers, policy makers, and the media.3-5 Indeed, the volume of North American media covering the opioid crisis has exploded over the past few years, from a mere 272 US print articles in 2013 to nearly 3000 in 2017.3,6 The opioid crisis has prompted recent changes in prescribing policies and recommendations in the United States in an attempt to curtail the volume of opioid analgesics available to children, adolescents and adults.7,8 Minimizing prescription opioid exposure is likely to be considered a positive trend; however, the full impact of the opioid crisis on children’s pain outcomes may be mixed and remains unclear.
Since children’s pain is largely managed in the home, it is important to understand the potential influence of societal events on parental beliefs and decisions. We have previously shown how analgesic trade-off preferences, or the relative preference for pain relief (benefit) vs. risk avoidance, shape parents’ decisions to give prescription opioids to their children.9-11 Competing concerns that are reflected in trade-off preferences create decisional dilemmas wherein parents either accept the potential and known risks of a treatment in order to obtain benefit or, rather, forgo the benefits to avoid risky adverse outcomes.12 Parents now make analgesic decisions within the context of the ongoing opioid crisis. In addition to the vast media coverage, personal experiences with or close proximity to individuals who have developed an opioid use disorder or experienced opioid-related overdose may influence parental opioid beliefs and analgesic preferences. This potential reshaping of beliefs and preferences may, in turn, influence pain management decisions for children who are prescribed opioid analgesics following surgery.
The purpose of this study was to examine whether 1) there has been a significant shift toward risk aversion in parental analgesic trade-off preferences from earlier to later in the opioid crisis and 2) this shift would be associated with parents’ hypothetical decisions to give a prescribed opioid to a child in pain.
Methods
We obtained an exemption from the University of Michigan Health Sciences and Behavioral Sciences Institutional Review Board (IRB-HSBS HUM00189020) to conduct a secondary analysis of de-identified baseline survey data from two previous studies.9,10 Each of these prospective studies included parents whose children were scheduled to undergo a painful ambulatory or short-stay surgical procedure at a tertiary care pediatric hospital in the Midwestern United States, and who were likely to receive a prescription opioid for pain management after discharge. In the first study, parents were recruited and surveyed from January-August 2013 (Time 1). In the second, recruitment occurred between October 2017 and May 2019 (Time 2). Because of sampling and prescribing differences in the two studies, we included only the data from parents whose children were between 5-17 years of age and who underwent orthopedic (e.g., open reduction of fracture), general pediatric surgery (e.g., orchidopexy) or otorhinolaryngology (e.g., tonsillectomy) procedures. We excluded parents who could not speak English, those whose children had a chronic pain diagnosis, who had a procedure unlikely to require prescription opioids, or who could not self-report pain (i.e., developmentally delayed). Our resultant sample, therefore, included 71% of Time 1 study data and 80% of Time 2 study data. We included children aged 5-17 years as this age group is generally old enough to reliably self-report pain but young enough that parents make most of the medication administration decisions.9
For this study, we included only parental baseline survey data which, in both studies, were completed prior to the child’s surgery and before parents had received instruction about the child’s prescriptions and postoperative pain management. In this manner, we hoped to explore the influence of events and experiences external to the child’s scheduled surgical experience.
Outcome measures
Analgesic trade-off preference:
Our primary outcome was measured using a 6-item instrument that assesses the degree to which parents prefer to relieve their child’s pain relative to their preference to avoid analgesic-related risks.9,11 Similar to stated choice methods,13 this scale uses forced choice responses to elicit trade-off preferences. Parents ranked their agreement with each item using a 5-point Likert scale ranging from strongly disagree (−2) to strongly agree (+2) to yield a total score ranging from −12 to +12. Lower scores indicate a preference toward risk aversion, higher scores a preference for pain relief (i.e., analgesic benefit), and scores around zero, ambivalence. We previously reported psychometric data supporting the internal consistency of the preference scale (Cronbach’s alpha 0.763 (95% CI 0.73, 0.80). Further, we have demonstrated that preference scores have predictive validity toward parental hypothetical and real opioid decision-making.9,10
Prescription Opioid Decision:
Our secondary outcome was assessed using the first hypothetical scenario decision exercise from our studies. Parents were given a simple scenario describing a child with a self-reported Faces Pain Score of 7 and no adverse effects since receiving their prescribed postoperative opioid dose 6 hours earlier. Previous studies have reported a treatment threshold of 7/10 for a majority of parents.14 Parents were asked to consider their own child when making the scenario-based decision about whether to give the next dose of the prescribed opioid, a lower dose, an over-the-counter analgesic, or to do nothing. Given our focus here on prescription opioid decision-making, responses were coded as binary (yes/no) to indicate whether parents decided to give the prescribed opioid (any dose) or withhold it.
Covariates
Data regarding parents’ self-reported sex, race, and highest level of education were obtained from their baseline surveys. These variables were dichotomized for the purpose of analyses (i.e., female vs. male, White vs. Non-White, > high school graduate vs. ≤ high school diploma). Parents’ past use of a prescribed opioid to treat their child’s pain, their child’s age and sex were also documented. Finally, parents’ perceived seriousness of habit/addiction, scored from 0 or not at all serious, to 5, extremely serious, was documented from the opioid knowledge and risk perception instruments (i.e., in response to the question., “How serious is the side effect of addiction (i.e., can’t stop taking the drug) when it happens after taking a prescribed narcotic?”), previously shown to have content, face and predictive validity in opioid decision-making.10,15
Statistical Analysis
All analyses were conducted using SPSS version 27 (IBM corporation; Armonk, NY). We used Chi-square and independent, two-sided t-tests to detect differences between the Time 1 and 2 samples. Univariate analyses were used to compare trade-off preference scores between Time 1 and 2 parents. For additional descriptive purposes, we used the overall sample interquartile range data to code parents’ preferences as risk averse (scores from −12 to less than −1), ambivalent (scores −1 to +1), or benefit (i.e., pain relief) preferent (scores from greater than 1 to 12).
We next used an ordinary least squares linear regression model to test our first hypothesis; that is the effect of Time on parental trade-off preferences, controlling for the covariates. To test our second hypothesis, we used multivariable logistic regression to regress the scenario-based opioid decision onto a Time*Preference interaction variable, controlling for the parent and child covariates. We followed this analysis with a post-hoc comparison of the relationship between coded preferences (i.e., risk averse or ambivalent vs. benefit/pain relief preferent) and the opioid decision for parents at Time 1 and those at Time 2. Data are described as n (%), mean ± standard deviation, mean difference (MD), β coefficient or Odds Ratio (OR) as appropriate, with 95% confidence intervals (CI). P values <.05 were accepted as significant.
Results
Our analytic sample included 361 parents from Time 1 and 486 parents from Time 2. Table 1 summarizes the characteristics of the parents and their children in the groups. While parental characteristics were similar between groups, their children differed with respect to age, sex, past opioid use, and surgical procedure. Children at Time 2 were significantly more likely to have used opioids in the past than those at Time 1 (see Table 1, row 11). Additionally, parents in the Time 2 sample rated the perceived seriousness of habit/addiction higher compared to those at Time 1 (see Table 1, row 4).
Table 1.
Characteristics of the Study Sample
| 2013 (n = 361) |
2017-2019 (n = 486) |
OR or MD [95% CI], P |
|
|---|---|---|---|
| Parent female | 278 (77.0) | 391 (81.0) | 1.27 [0.91, 1.77], .162 |
| Self-identified race White | 301 (84.6) | 432 (88.9) | 1.46 [0.98, 2.19], .064 |
| Parent > high school graduate | 290 (82.4) | 424 (87.2) | 1.46 [1.00, 2.14], .051 |
| Perceived seriousness addiction† | 4.4 ± 1.4 | 4.6 ± 1.0 | 0.27 [0.11, 0.44], .001 |
| Analgesic trade-off preference§ | |||
| Risk averse | 92 (25.5) | 204 (42.0) | 2.12 [1.57, 2.85], <.001 |
| Ambivalent | 120 (33.2) | 163 (33.5) | 1.01 [0.76, 1.35], .928 |
| Prefer pain relief | 149 (41.3) | 119 (24.5) | 0.46 [0.34, 0.62], <.001 |
| Child age | 9.9 ± 3.6 | 11.3 ± 3.3 | 1.4 [0.9, 1.8], <.001 |
| Child female sex | 162 (44.9) | 172 (35.4) | 0.67 [0.51, 0.89], .005 |
| Child past opioid use | 35 (9.7) | 146 (30.0) | 3.99 [2.68, 5.94], <.001 |
| Child procedure | |||
| Otolaryngology | 136 (37.7) | 61 (12.6) | 0.24 [0.17, 0.33], <.001 |
| Orthopedics | 104 (28.8) | 241 (49.6) | 2.43 [1.82, 3.25], <.001 |
| General surgery | 121 (33.5) | 184 (37.9) | 1.21 [0.91, 1.61], .193 |
Data presented as n (%) or mean ± standard deviations. OR = odds ratio, MD = mean difference, CI = confidence interval. P-values derived from univariate analyses. Percentages calculated based on available data for each variable.
Scale 0 to 5, with 0=not serious, 5=extremely serious.
Scale −12 to +12, with scores < −1 indicating risk aversion, −1 to 1 ambivalence, > 1 preferring pain relief.
Hypothesis 1: Association between Time and Analgesic Trade-off Preferences
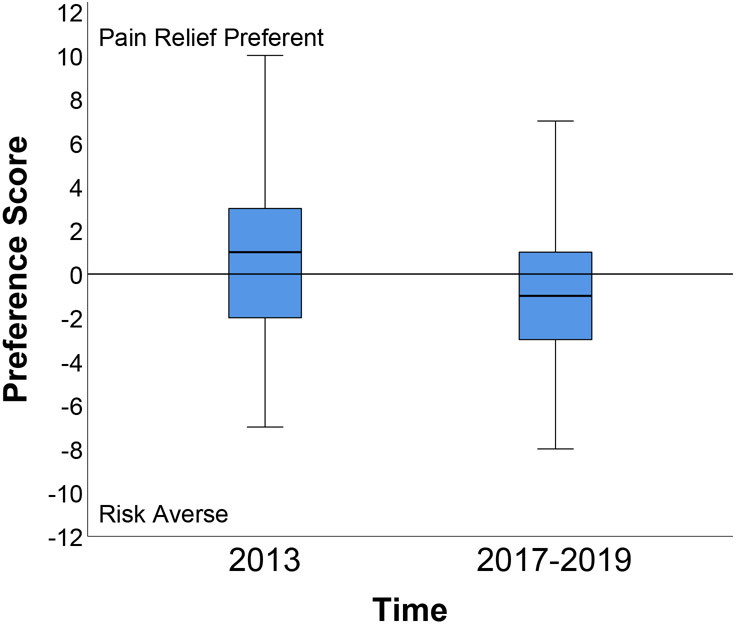
Parents at Time 2 had lower trade-off preference scores (mean −0.8) compared to those at Time 1 (mean 0.8; mean difference −1.6 [95% CI −2.1, −1.1]; see Figure 1). For clarity, parents at Time 2 were more than twice as likely to be risk averse or ambivalent than those at Time 1 (75.5% vs. 58.7%, respectively; OR 2.17 [95% CI 1.62, 2.91]). Linear regression analysis supported the significant effect of Time on analgesic trade-off preferences, supporting our first hypothesis (Table 2).
Figure 1.
Parents’ analgesic trade-off preference scores at Time 1 (2013) and Time 2 (2017-2019). Analgesic Trade-off Preference Scores can range from −12 to +12, with scores < −1 indicating risk aversion, −1 to 1 ambivalence, > 1 pain relief preference; data shown represent the group median (horizontal line), interquartile range (box), and range (vertical line).
Table 2.
Effect of Time on Parents’ Analgesic Trade-off Preferences
| Factor (Reference) | Adjusted β [95% CI], P |
|---|---|
| Time 2 (Time 1) | −0.84 [−1.09, −0.60], <.001 |
| Parent female (male) | 0.37 [−0.19, 0.93], .197 |
| Parent race: White (Non-white) | −0.15 [−0.84, 0.54], .671 |
| Parent > high school graduate (≤ high school) | −0.02 [−0.67, 0.64], .960 |
| Child age | −0.01 [−0.07, 0.06], .875 |
| Child female (male) | −0.22 [−0.69, 0.25], .360 |
| Child past opioid use (no) | 0.55 [−0.02, 1.13], .059 |
| Perceived seriousness of addiction | −0.31 [−0.51, −0.12], .002 |
CI=confidence interval; Model summary: r2=0.07, F=8.22 (df8), p<.001
Hypothesis 2: Effect of Preference Shift on Parents’ Opioid Administration Decision
Table 3 depicts the results of the logistic regression model which supported our second hypothesis regarding an interaction effect of time by trade-off preference. A post hoc analysis examined the effect of trade-off preference for parents at Time 1 and for those at Time 2 to clarify the interaction effect on parents’ decision to administer the prescribed opioid. This analysis showed that at Time 2, parents who were coded as risk averse or ambivalent were 43% less likely to give the opioid for the hypothetical scenario compared to those who were pain relief preferent (OR 0.57 [95% CI 0.37, 0.89], p=.013). In contrast, parents at Time 1 exhibited no differences in this decision based on their preference group (OR 0.87 [95% CI 0.57, 1.33], p=.512).
Table 3.
Effect of Time*Trade-off Preference on Parents’ Hypothetical Decisions to Administer a Prescribed Opioid to a Child in Pain
| Factors (Reference) | OR [95% CI], P |
|---|---|
| Time*Trade-off preference | 1.09 [1.03, 1.16], .003 |
| Parent female (male) | 0.93 [0.65, 1.32], .686 |
| Parent race: White (Non-white) | 1.84 [1.21, 2.80], .005 |
| Parent > high school graduate (≤ high school) | 1.71 [1.15, 2.55], .008 |
| Child age | 1.04 [0.99, 1.08], .089 |
| Child female (male) | 1.49 [1.11, 2.00], .008 |
| Child past opioid use (no) | 1.54 [1.07, 2.22], .019 |
OR=odds ratio, CI=Confidence interval. Model summary: Nagelkerke r2=0.065; Chi-square=40.75 (df 7), p<.001; Hosmer Lemeshow=0.718
Discussion
Findings from our secondary analysis suggest that parental analgesic trade-off preferences have recently shifted toward risk aversion in a North American area that has been heavily impacted by the opioid crisis. Specifically, we found that compared to parents of children scheduled for surgery at a single, Midwestern pediatric hospital in 2013, those surveyed more recently were more than twice as likely to be analgesic risk averse or ambivalent (OR 2.17). We also found that this preference shift was associated with parents’ decisions to withhold a prescribed opioid dose for a hypothetical child in pain. Since this later finding was based on parents’ scenario-based decision-making, it remains unclear whether analgesic decision-making in the home has similarly shifted. Yet, our study sheds important light on the potential impact of recent societal events on parents’ analgesic trade-off thinking.
Importantly, healthcare trade-off preferences are not stable over time, but are complex and dynamic and can shift based on personal experiences, those of friends and family, and information from the media or healthcare providers.16 It remains unclear which of these or other factors may have influenced the observed difference in parental preferences in our samples. While it is unknown whether the media influenced the observed shift toward risk aversion in our recent sample, a large uptick in media attention to the opioid crisis in North America began shortly after 2013 and surged over the next few years.3,6 There were also significant changes in media content from prior to 2013 to 2017, including a higher focus on deaths, overdoses, and addiction among young people (6% vs 19% of articles, respectively) and legitimate (i.e., medically prescribed) opioid users (3% vs. 17%).6 Much of the language used in the Canadian media during this period – which was similarly reflected in US media – was deemed sensational including terminology like “crisis”, “epidemic”, and “hidden killer”.6 Finally, there has been a higher media emphasis on unsafe prescribing practices that began prior to 2013 and that continued through 2017. These and other changes in media foci have created a shifting social construct of the opioid crisis6 that may have contributed to the small but significantly higher perceptions of analgesic-related addiction risk and the preference toward risk aversion observed in our recent sample. It is unclear whether this small shift in risk perceptions is clinically significant, that is, whether it would be enough of a change to influence the decision to administer a prescribed opioid to a child in pain. However, we have previously demonstrated how small, statistically significant changes in risk perceptions altered hypothetical decisions to give a prescribed opioid to a child experiencing significant adverse effects.10 Notably, the ongoing opioid crisis has created a conundrum regarding best pediatric prescribing and pain management practices that remains topical in the US media today.17 The full impact of this crisis on children’s pain outcomes will likely remain unclear in the near future.
Our finding that parents’ trade-off preferences were associated with their baseline hypothetical opioid decision-making is similar to other studies. For instance, parents’ trade-off preferences have been associated with their medication seeking behavior and adherence decisions for a variety of childhood conditions including attention deficit disorders and asthma.12,18,19 Further, we have previously demonstrated an association between parents’ analgesic trade-off preferences and their opioid administration to children after surgery.10 Analgesic decisions may be particularly preference-sensitive since these drugs are typically prescribed and administered “as needed” and alternatives to managing pain are many. However, similar to previous studies,9,20 we found that most parents were not entirely polarized in their risk and benefit preferences, but were somewhat ambivalent about these competing analgesic outcomes (e.g., interquartile range of preference scores were −1 to +1). This is not surprising, since relieving pain and avoiding adverse effects are both important goals of treatment. Notably, a preference toward risk aversion or ambivalence was associated with the decision to withhold the prescribed opioid for parents at Time 2, but not Time 1. This finding may, in part, reflect a stronger influence of what is known as omission bias in our recent sample of parents; that is, risk averse or ambivalent parents may judge the harms of commission (i.e., choosing a treatment that causes harm) worse than that of omission (i.e., forgoing a treatment that may benefit).21 This bias in decision-making has been supported by multiple studies and is particularly germane for individuals making potentially risky decisions for others.22
Our data also show a significant and positive effect of parents’ past use of opioids to treat their child’s pain on their hypothetical decision to give the prescribed opioid to the child in pain. This finding likely reflects an influence of past experience on decision-making. It remains unclear why children in our Time 2 sample were more likely to have received a prescribed opioid previously. However, this sample was older and more likely to be scheduled for orthopedic surgery. These factors may help to explain higher rates of previous opioid prescribing since older children with musculoskeletal disorders may have been treated for pain. Importantly, the effect of Time*Preferences remained significant when controlled for their past opioid use, which was significantly different between the samples at baseline. This may reflect additional influences beyond personal experience.
Limitations
Our findings are limited by several methodologic and sample weaknesses. First, all data were collected at a single, large tertiary care academic pediatric hospital in a Midwestern state with one of the highest opioid-involved death rates in the nation.23 Additionally, parents in both studies were largely White and well-educated, which may have introduced a selection bias. We and others have demonstrated racial differences in opioid prescribing, knowledge and experiences which may have impacted our findings.24 The ability to generalize our findings to other settings and populations is thus, limited. Next, our study focused on analgesic trade-off preferences and risk perception and did not examine the influence of parental or child anxiety, or catastrophizing, all known to influence analgesic use in pediatric settings. Additionally, our hypothetical scenario focused the parent only on pain intensity rather than the child’s functional status which is also likely to factor into their decisions. Our study samples at Time 1 and 2 were entirely independent, leaving us unable to assess changes in analgesic trade-off preferences or decision-making at the individual level. Further, as noted above, parents in our 2013 sample may have been influenced by the already shifting media landscape which may have dampened our findings. Finally, though strong evidence indicates high correlations between hypothetical and actual healthcare decision-making,25 whether the observed shift in parents’ hypothetical decisions translates into a similar shift in real, post-operative opioid use remains unknown. Indeed, their children’s surgical procedure (which was different between groups), their course of treatment, pain experience and outcomes may further shape and influence parents’ preferences and decisions throughout the postoperative recovery period.
Conclusions
Despite its limitations, this study provides important insight into the instability of parents’ analgesic trade-off preferences and prescription analgesic decision-making. Our data suggest that parents of children scheduled for painful surgery in North American areas heavily impacted by the opioid crisis have become more analgesic risk averse. Given the known associations between medication preferences and usage, these findings may have clinical implications for pain management of children after surgery. Risk-avoidant or ambivalent parents may be hesitant to give a drug they believe is risky. While the need to balance the risks and benefits of analgesic medications remains important, healthcare providers can help parents better understand the safe and effective use of opioid analgesics when prescribed in order to lessen their decisional dilemmas. Helping parents to recognize and mitigate opioid-related risks while effectively managing their children’s pain may lead to optimal analgesic decisions and pain outcomes for their children following surgery.
Acknowledgements
This work was supported in part by the National Institute on Drug Abuse (R01DA044245, PI Voepel-Lewis). Ms. Lenko is also funded by Predoctoral Fellowship Training Grant (T32 NR016914. Program Director: Titler) Complexity: Innovations in Promoting Health and Safety. 7/1/2017 – 6/30/2022.
Footnotes
Conflict of Interest
The authors have no conflicts of interest to disclose.
Data availability:
Data sharing not applicable to this article as no new datasets were generated for these secondary analyses.
References
- 1.Kelley-Quon LI, Kirkpatrick MG, Ricca RL, et al. Guidelines for Opioid Prescribing in Children and Adolescents After Surgery: An Expert Panel Opinion. JAMA Surg. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cravero JP, Agarwal R, Berde C, et al. The Society for Pediatric Anesthesia recommendations for the use of opioids in children during the perioperative period. Paediatr Anaesth. 2019;29(6):547–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McGinty EE, Stone EM, Kennedy-Hendricks A, Sanders K, Beacham A, Barry CL. U.S. news media coverage of solutions to the opioid crisis, 2013–2017. Prev Med. 2019;126:105771. [DOI] [PubMed] [Google Scholar]
- 4.Harris PA. The Opioid Epidemic: AMA's response. Am Fam Physician. 2016;93(12):975. [PubMed] [Google Scholar]
- 5.Paulozzi LJ, Jones CM, Mack KA, Rudd RA. Vital signs: overdoses of prescription opioid pain relievers---United States, 1999--2008. Morb Mortal Wkly Rep. 2011;60(43):1487–1492. [PubMed] [Google Scholar]
- 6.Webster F, Rice K, Sud A. A critical content analysis of media reporting on opioids: The social construction of an epidemic. Soc Sci Med. 2020;244:112642. [DOI] [PubMed] [Google Scholar]
- 7.Toce MS, Michelson K, Hudgins J, Burns MM, Monuteaux MC, Bourgeois FT. Association of State-Level Opioid-Reduction Policies with Pediatric Opioid Poisoning. JAMA Pediatrics. 2020;174(10):961–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Groenewald CB. Opioid-prescribing Patterns for Pediatric Patients in the United States. Clin J Pain. 2019;35(6):515–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Voepel-Lewis T, Zikmund-Fisher BJ, Smith EL, Zyzanski S, Tait AR. Parents' preferences strongly influence their decisions to withhold prescribed opioids when faced with analgesic trade-off dilemmas for children: A prospective observational study. Int J Nurs Stud. 2015;52(8):1343–1353. [DOI] [PubMed] [Google Scholar]
- 10.Voepel-Lewis T, Malviya S, Grant JA, et al. Effect of a brief scenario-tailored educational program on parents' risk knowledge, perceptions, and decisions to administer prescribed opioids: a randomized controlled trial. Pain. 2021;162(3):976–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Voepel-Lewis T, Zikmund-Fisher BJ, Boyd CJ, et al. Effect of a Scenario-tailored Opioid Messaging Program on Parents' Risk Perceptions and Opioid Decision-making. Clin J Pain. 2018;34(6):497–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ross M, Nguyen V, Bridges JFP, et al. Caregivers' Priorities and Observed Outcomes of Attention-Deficit Hyperactivity Disorder Medication for Their Children. J Dev Behav Pediatr. 2018;39(2):93–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnson F, Hauber A, Poulos C. A Brief Introduction to the Use of Stated-Choice Methods to Measure Preferences for Treatment Benefits and Risks. RTI International; September 2009. 2009. RR-0009–0909. [Google Scholar]
- 14.Demyttenaere S, Finley GA, Johnston CC, McGrath PJ. Pain treatment thresholds in children after major surgery. Clin J Pain. 2001;17(2):173–177. [DOI] [PubMed] [Google Scholar]
- 15.Voepel-Lewis T, Zikmund-Fisher BJ, Smith EL, Redman RW, Zyzanski S, Tait AR. Parents' analgesic trade-off dilemmas: How analgesic knowledge influences their decisions to give opioids. Clin J Pain. 2016;32(3):187–195. [DOI] [PubMed] [Google Scholar]
- 16.Street RL Jr., Elwyn G, Epstein RM. Patient preferences and healthcare outcomes: An ecological perspective. Expert Rev Pharmacoecon Outcomes Res. 2012;12(2):167–180. [DOI] [PubMed] [Google Scholar]
- 17.Klass P New Guidelines Cover Opioid Use After Children’s Surgery. The New York Times. 2020. [Google Scholar]
- 18.Waschbusch DA, Cunningham CE, Pelham WE Jr, et al. A discrete choice conjoint experiment to evaluate parent preferences for treatment of young, medication naïve children with ADHD. J Clin Child Adolesc Psychol. 2011;40(4):546–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Conn KM, Halterman JS, Fisher SG, Yoos HL, Chin NP, Szilagyi PG. Parental beliefs about medications and medication adherence among urban children with asthma. Ambul Pediatr. 2005;5(5):306–310. [DOI] [PubMed] [Google Scholar]
- 20.Brown KF, Kroll JS, Hudson MJ, et al. Factors underlying parental decisions about combination childhood vaccinations including MMR: a systematic review. Vaccine. 2010;28(26):4235–4248. [DOI] [PubMed] [Google Scholar]
- 21.Blumenthal-Barby JS, Krieger H. Cognitive biases and heuristics in medical decision making: a critical review using a systematic search strategy. Med Decis Making. 2015;35(4):539–557. [DOI] [PubMed] [Google Scholar]
- 22.Zikmund-Fisher BJ, Sarr B, Fagerlin A, Ubel PA. A matter of perspective: Choosing for others differs from choosing for yourself in making treatment decisions. J Gen Intern Med. 2006;21(6):618–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wilson N, Kariisa M, Seth P, Smith Ht, Davis NL. Drug and Opioid-Involved Overdose Deaths - United States, 2017-2018. Morb Mortal Wkly Rep. 2020;69(11):290–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Olshansky E, Zender R, Kain ZN, Rosales A, Guadarrama J, Fortier MA. Hispanic parents' experiences of the process of caring for a child undergoing routine surgery: a focus on pain and pain management. J Spec Pediatr Nurs. 2015;20(3):165–177. [DOI] [PubMed] [Google Scholar]
- 25.Robinson MD, Clore GL. Simulation, scenarios, and emotional appraisal: Testing the convergence of real and imagined reactions to emotional stimuli. Pers Soc Psychol. 2001;27(11):1520–1532. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no new datasets were generated for these secondary analyses.