Abstract
Objectives
Post-COVID-19 symptoms and its features in many recovered patients are almost similar to post-severe acute respiratory syndrome. The study aims to assess the outcome and manifestations during post-COVID follow-up period in recovered patients.
Methods
Ambidirectional longitudinal study was conducted among recovered COVID-19 patients from a tertiary care hospital near Chennai through telephonic interview after discharge. Total admitted patients from June to November 2020 were 3496 and among those 183 died and 12 transferred to other hospitals. Totally 1354 consented for study and the rest were wrong numbers or not willing to participate. Chi-square test and multinominal logistic regression analysis were done.
Results
Majority of, that is, 27.6% and 18.7% were in 21–30 years and >60 years, respectively. Majority were admitted with fever (38.3%), cough (15.3), and body pain (10%). Post-COVID symptoms reported were fatigue (39.7%), stress and anxiety (27.6%), and mood changes (5.8%). Some patients were newly diagnosed with diabetes mellitus (10), hypertension (5), and TB (1) after discharge. Having diabetes mellitus is an independent risk to have neurological and cardio-respiratory symptoms and patients who were discharged with minimal support were to have an independent risk factor of renal symptoms on follow-up than other subjects.
Conclusion
The follow-up symptoms were associated with the patients’ comorbidities, age, severity of illness, and environmental factors.
Keywords: follow-up, anxiety, symptoms, tiredness, mood changes, COVID-19
Introduction
In December 2019, a highly contagious respiratory illness was observed in the Wuhan province of China. This infection has given a serious health crisis across the globe with the severe acute respiratory syndrome caused by the virus and was labeled as coronavirus also known as SARS-CoV-2 virus and later was known to be COVID-19 by World Health Organization (WHO) on 11 February 2020. 1 A rapid spread was observed across the world and has been declared as a global pandemic by WHO on March 11, 2020. 2 On studying the long-term sequelae of COVID-19 disease, it is very difficult in understanding the natural history of disease in spite of predicting its impact on affected individuals. 3 COVID-19 had created a huge impact on individuals across the world physically, mentally, financially, and in all aspects.
Summary Box
• Current understanding of the subject: The knowledge on the post-COVID-19 sequalae is still unclear. Literature shows that the Western population is more affected than the Asian population even after recovery.
• Addition to the literature: Various system-based symptoms are studied and the independent risk factors for the prolonged symptoms are evaluated among South Indian population.
• Implications for public health practice: Encourages more studies on the follow-up of recovered COVID-19 patients to assess various factors influencing the effect in different geographical locations. Helps the public health professionals to have clear plan of action to control and manage further cases of COVID-19.
Millions of people around the world were confirmed to be infected by SARS-CoV-2 and were hospitalized and isolated for further management and thousands of deaths have been recorded, but there is still no proper approach to address the persistent complications of the disease and specialist assessment was required during the follow-up. 4 The clinical spectrum of COVID-19 varies, showing both asymptomatic and symptomatic characteristics, as affected individuals present with mild, moderate, and severe illness. 5 The presenting complaints of the affected individuals mainly depend on the associated comorbidities. The patients on follow-up usually presented with dyspnea, asthenia, myalgia, cough, anosmia, and ageusia and many of the patients had developed further complications even after giving supportive and therapeutic treatment based on their condition. 6
Many of the patients who got infected recovered from their presented symptom and some of them had developed new other symptoms. Subsequently, it is found that most of the recovered patients were presenting with relapsing post-COVID-19 symptoms, especially fatigue, myalgia, anxiety stress, sleep disturbances, and shortness of breath. 7 Some manifestations would be chronic and may last for longer duration requiring long-term monitoring. 8 At this moment, the strategies we deal with the infection are mainly aimed at preventing and reducing the further transmission in the community apart from giving supportive therapeutic care to affected individuals. Thus, this study aims to assess the outcome and manifestations of COVID-19 during their 3 months follow-up period among the recovered patients and to evaluate the factors associated with their clinical manifestations. This follow-up program is a part of follow-up plan instructed by the Tamil Nadu State Government to start follow-up clinic in all the medical colleges and hospitals which was issued by August 2020. 9 Thus, a telemonitored follow-up was initiated by September 2020 and encouraged the patients to follow-up in the hospital.
Subjects and Methods
An ambidirectional follow-up longitudinal study was conducted in a tertiary care hospital near Chennai, Tamil Nadu, India, among 1354 laboratory confirmed cases of COVID-19 who were discharged after their recovery. All the COVID-19 cases were included, irrespective of their age and gender who were admitted in the hospital from June 1, 2020 to November 10, 2020. The baseline details, complaints, and severity of the disease during admission were collected from the case record retrospectively and follow-up details after 3 months of discharge post-recovery prospectively. Individual telephonic interview was conducted from September 2020 to February 2021 with all the discharged patients who were willing to participate in the study to extract the information regarding their mental and physical health status after recovery from COVID-19. A pre-tested, pre-validated, structured questionnaire regarding their baseline sociodemographic details, their complaints, and comorbid conditions during admission, events occurred on their hospital stay, and details on their current status based on systematic symptoms was used after the peer review. The final questionnaire was validated by 2 internal and 2 external validators before using it. The collected data were cross checked by an independent, senior peer from respiratory department to observe for any discrepancies in the data if present. The missing data from the case record were collected during the telephonic interview. This study was conducted after obtaining approval from the Institutional Ethical committee of a Private Medical College and Hospital. Informed consent for telemedicine services 10 was obtained from all the study participants before eliciting the desired information and for those who were less than 18 years of age, assent from their parents or guardians was taken. All the calls were recorded with their permission for further clarifications and to show consent for the study. Universal sampling technique was adopted as all the discharged patients were included in the study.
Severity of the disease considered on admission was based on the guidelines issued by Ministry of Health and Family Welfare from Government of India. 11
Criteria for discharge of COVID-19 patients were based the Revised Discharge Policy for COVID-19 issued by Ministry of Health and Family Welfare from Government of India. 12
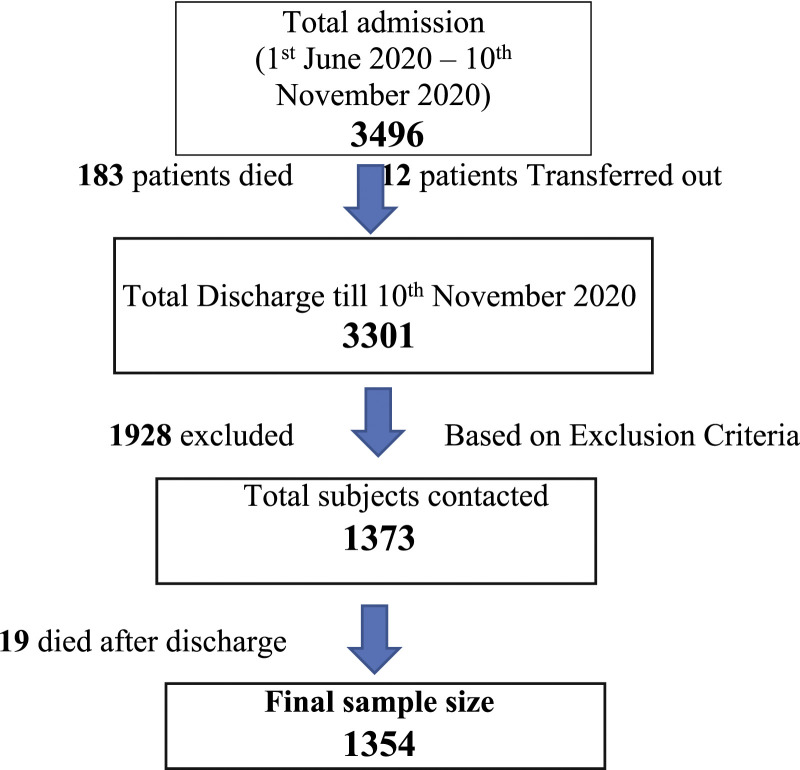
Patients who died during the hospital stay, those who were transferred to other hospitals, those who left the hospital against medical advice, those not willing to participate in the study, those not willing to record the call to show consent for the study, those who cannot be reached after calling 3 times, and those who provided us with wrong numbers to contact were excluded from the study. Those who had symptoms suggestive for physician consultation were asked to visit hospital for a follow-up and complete examination and others with no symptoms were also encouraged to have a follow-up visit to the hospital at least once. Figure 1 represents the procedure involved in the consideration of selecting study participants.
Figure 1.
Flow diagram representing procedure involved in selection of study subjects.
Statistical Analysis
The collected data were entered in MS Excel and analyzed using SPSS version 25. Frequencies and percentages were seen. For univariate analysis, chi-square test (inferential statistics) was used to find the association between independent variables and follow-up symptoms. The multivariate logistic regression technique was used to identify the independent risk factors for system-based symptoms. The P value <.05 was considered significant in this study.
Results
Baseline Details of Study Subjects
Among 1354 subjects who participated in the study, 73% were males and 27% were females and majority (27.6%) of them were in the age group of 21–30 years, followed by 51–60 years (18.8%) and >60 years (18.7%). Nearly 9.7% were diagnosed with diabetes mellitus and 6.4% had both diabetes mellitus and hypertension on admission. Majority (98.3%) were admitted in general hospital care, whereas only 1.5% required ICU stay. On admission, 84.9%, 10.4%, and 4.65% were admitted as mild, moderate, and severe cases, respectively. Mostly 77.4% were discharged within 10 days of admission and only .4% stayed more than 1 month in the hospital. Only 3.2% of them required minimal support during discharge. Severity-based baseline details of the study subjects are shown in Table 1. Most commonly reported symptoms on admission were fever (42.2%), followed by dry cough (17.9%) and myalgia (10.6%).
Table 1.
Baseline details of the study subjects based on the severity of disease on admission (N = 1354).
| Characteristics | Severity of disease on admission | |||
|---|---|---|---|---|
| Mild | Moderate | Severe | Total | |
| N = 1150 | N = 141 | N = 63 | N = 1354 | |
| N (%) | N (%) | N (%) | N (%) | |
| Age (years) | ||||
| ≤10 | 3 (.2%) | 1 (.1%) | 1 (.1%) | 5 (.4%) |
| 11–20 | 44 (3.2%) | 6 (.4%) | 1 (.1%) | 51 (3.8%) |
| 21–30 | 329 (24.3%) | 34 (2.5%) | 11 (.8%) | 374 (27.6%) |
| 31–40 | 178 (13.1%) | 24 (1.8%) | 3 (.2%) | 205 (15.1%) |
| 41–50 | 176 (13.0%) | 24 (1.8%) | 12 (.9%) | 212 (15.7%) |
| 51–60 | 205 (15.1%) | 32 (2.4%) | 17 (1.3%) | 254 (18.8%) |
| ≥60 | 215 (15.9%) | 20 (1.5%) | 18 (1.3%) | 253 (18.7%) |
| Sex | ||||
| Male | 842 (62.2%) | 98 (7.25) | 49 (3.6%) | 989 (73.0%) |
| Female | 308 (22.7%) | 43 (3.2%) | 14 (1.0%) | 365 (27.0%) |
| Existed comorbidities | ||||
| Diabetes mellitus (DM) | 116 (8.6%) | 15 (1.1%) | 1 (.1%) | 132 (9.7%) |
| Hypertension (HTN) | 41 (3.0%) | 5 (.4%) | 3 (.2%) | 49 (3.6%) |
| Both (DM + HTN) | 71 (5.2%) | 11 (.8%) | 4 (.3%) | 86 (6.4%) |
| Chronic kidney disease | 4 (.3%) | 1 (.1%) | 2 (.1%) | 7 (.5%) |
| Coronary artery disease | 3 (.2%) | 0 | 0 | 3 (.2%) |
| Chronic obstructive pulmonary disease | 8 (.6%) | 0 | 1 (.1%) | 9 (.7%) |
| Asthma | 5 (.4%) | 1 (.1%) | 1 (.1%) | 7 (.5%) |
| Pulmonary tuberculosis | 1 (.1%) | 0 | 0 | 1 (.1%) |
| Hypothyroidism | 7 (.5%) | 0 | 0 | 7 (.5%) |
| Autoimmune conditions | 2 (.1%) | 0 | 0 | 2 (.1%) |
| None | 892 (65.8%) | 108 (7.9%) | 51 (3.7%) | 1051 (77.6%) |
| Type of care received | ||||
| General hospital admission | 1134 (83.8%) | 139 (10.3%) | 58 (4.3%) | 1331 (98.3%) |
| Hospital admission to home care | 3 (.2%) | 0 | 0 | 3 (.2%) |
| ICU stay | 13 (1.0%) | 2 (.1%) | 5 (.4%) | 20 (1.5%) |
| Duration of hospital stay | ||||
| <10 days | 924 (68.3%) | 98 (7.2%) | 24 (1.8%) | 1046 (77.4%) |
| 11–15 days | 195 (14.4%) | 36 (2.7%) | 19 (1.4%) | 250 (18.5%) |
| 16–30 days | 28 (2.1%) | 6 (.4%) | 16 (1.2%) | 50 (3.7%) |
| >1 Month | 2 (.1%) | 0 | 4 (.3%) | 6 (.4%) |
| Condition on discharge | ||||
| Stable with No support | 1129 (83.4%) | 126 (9.3%) | 53 (3.9%) | 1308 (96.6%) |
| Stable with minimal support | 21 (1.6%) | 12 (.9%) | 10 (.7%) | 43 (3.2%) |
| Wheel chair assisted | 0 | 3 (.2%) | 0 | 3 (.2%) |
ICU, intensive care unit.
Post-COVID-19 Symptoms Reported
Most commonly reported symptoms by the study subjects were tiredness/fatigue (39.7%), followed by stress and anxiety (27.6%), mood changes (5.8%), and myalgia (5.1%) followed by 17 other symptoms represented in Table 2 in order of their descend among study subjects and the duration of symptoms presented on the day of calling shows that most of the symptoms were present for past 2–3 weeks. It was noted that both males and females reported similar symptoms during the follow-up period. Among the general symptoms, nearly 83.3% reported muscular weakness, 56.5% reported myalgia, and 60.2% reported tiredness and fatigue for past 3 weeks, 2 weeks, and 1 week, respectively. Among the cardio-respiratory symptoms, majority of 71.4% reported palpitations for past 2 weeks and among the abdominal symptoms, majority of 93.5% and 73.1% reported nausea/vomiting and loss of appetite, respectively, for past 2 weeks. In neurological symptoms, 83.3% reported burning and pricking sensation of body for past 3 weeks and 95.7% reported loss of smell for past 2 weeks. The most commonly reported psychological symptoms were mood changes (88.6%) and sleep disturbances (81.6%) for past 2 weeks and last, reduced urine output was the only renal symptom observed only among 4 patients acutely for past 1 week.
Table 2.
Gender-based distribution of post-COVID symptoms as reported by the study subjects in the order of descend (N = 1354).
| S.NO | Post-COVID symptoms | Gender | Total N (%) | |
|---|---|---|---|---|
| Male N (%) | Female N (%) | |||
| 1 | Tiredness/fatigue | 400 (29.5%) | 138 (10.2%) | 538 (39.7%) |
| 2 | Stress and anxiety | 268 (19.8%) | 106 (7.8%) | 374 (27.6%) |
| 3 | Change in mood | 56 (4.1%) | 23 (1.7%) | 79 (5.8%) |
| 4 | Myalgia | 51 (3.8%) | 18 (1.3%) | 69 (5.1%) |
| 5 | Loss of appetite | 36 (2.7%) | 16 (1.2%) | 52 (3.8%) |
| 6 | Sleep disturbances | 42 (3.1%) | 7 (.5%) | 49 (3.6%) |
| 7 | Muscular weakness | 32 (2.4%) | 10 (.7%) | 42 (3.1%) |
| 8 | Constipation | 20 (1.5%) | 15 (1.1%) | 35 (2.6%) |
| 9 | Loss of taste | 29 (2.1%) | 5 (.4%) | 34 (2.5%) |
| 10 | Nausea and vomiting | 19 (1.4%) | 12 (.9%) | 31 (2.3%) |
| 11 | Loss of smell | 18 (1.3%) | 5 (.4%) | 23 (1.7%) |
| 12 | Headache | 18 (1.3%) | 4 (.3%) | 22 (1.6%) |
| 13 | Abdominal discomfort | 13 (1.0%) | 1 (.1%) | 14 (1%) |
| 14 | Breathing difficulty | 12 (.9%) | 2 (.1%) | 14 (1%) |
| 15 | Confusion | 9 (.7%) | 4 (.3%) | 13 (1%) |
| 16 | Numbness | 9 (.7%) | 1 (.1%) | 10 (.7%) |
| 17 | Sore throat | 7 (.5%) | 2 (.1%) | 9 (.7%) |
| 18 | Chest pain | 6 (.4%) | 2 (.1%) | 8 (.6%) |
| 19 | Palpitations | 6 (.4%) | 1 (.1%) | 7 (.5%) |
| 20 | Burning and pricking pain sensation on body | 5 (.4%) | 1 (.1%) | 6 (.4%) |
| 21 | Reduced urine output | 4 (.3%) | 0 | 4 (.3%) |
Newly Diagnosed Comorbidities on Discharge
It was seen that subjects who were admitted with no existing comorbidities were either discharged or developed new comorbidities post-discharge such as diabetes mellitus (10), hypertension (5), and TB (1). Among those who developed new comorbidities, it was observed that 6 (66.6%) females developed diabetes mellitus than 3 (33.3%) males, 4 (80%) females developed hypertension than 1 (20%) male, and only 1 male developed both diabetes mellitus and tuberculosis and these findings were statistically significant (P = .002). It was observed that 60% of those who were newly diagnosed with hypertension reported general symptoms than 45.9% who had no new comorbidities. Similarly, 44.4% of those who were newly diagnosed with diabetes mellitus reported neurological symptoms than 34.4% who had no new comorbidities, though these finding were not statistically significant.
Post-COVID-19 Symptoms vs Month of Admission vs Duration of Symptoms
It was seen that majority of 55.1% and 33.3% of patients admitted in month of July reported myalgia and sore throat, respectively, which was statistically significant (P = .023 and P = .013). Similarly, majority of 69%, 65.2%, and 46.9% of patients admitted in the month of August reported with muscular weakness, loss of smell, and sleep disturbances, respectively, which was also statistically significant (P = .000, P = .007 and P = .031). Association between the month of admission and duration of symptoms reported showed that 83.3% of subjects who reported muscle weakness for 3 weeks were mostly admitted in the month of August (69%) which was significant (P = .001). Similarly, 42.2% of subjects who reported stress and anxiety for 2 weeks were mostly admitted in the month of July (38%) which was also significant (P = .050).
Association between System-Based Post-Discharge Symptoms vs Existed Comorbidities and Month of Admission of the Participants
It was observed that 12.1% who had diabetes mellitus reported neurological symptoms than 5.4% who did not have diabetes mellitus which was statistically significant (P = .004). Similarly, 51% of those who had hypertension reported general symptoms than 45.7% who did not have hypertension which was statistically significant (P = .027). Nearly 52.3% who had both DM and HTN reported general symptoms than 45.4% who had none which was not statistically significant. On further observing the association between the month of admission and system-based symptoms, it was seen that there was a significant association with general symptoms (P = .014), abdominal symptoms (P = .036), and neurological symptoms (P = .005) which is shown in Table 3.
Table 3.
Association between months of admission and system-based post-discharge symptoms (N = 1354).
| Months of admission 2020 | General symptoms N (%) | Cardio-respiratory symptoms N (%) | Abdominal symptoms N (%) | Psychological symptoms N (%) | Neurological symptoms N (%) | Renal symptoms N (%) |
|---|---|---|---|---|---|---|
| June | 37 (37.8%) | 1 (1%) | 4 (4.1%) | 32 (32.7%) | 4 (4.1%) | 0 |
| July | 236 (44.7%) | 16 (3%) | 64 (12.1%) | 176 (33.3%) | 36 (6.8%) | 3 (.6%) |
| August | 216 (52.9%) | 11 (2.7%) | 43 (10.5%) | 150 (36.8%) | 36 (8.8%) | 1 (.2%) |
| September | 91 (42.5%) | 8 (3.7%) | 16 (7.5%) | 66 (30.8%) | 5 (2.3%) | 0 |
| October | 37 (38.5%) | 0 | 4 (4.2%) | 38 (39.6%) | 1 (1%) | 0 |
| November | 4 (40%) | 1 (10%) | 1 (10%) | 4 (40%) | 0 | 0 |
| P value (<.05) | .014* | .239 | .036* | .565 | .005* | .760 |
Chi-square test (P value <.05 significant)*.
Association between System-Based Post-Discharge Symptoms vs Baseline Details of the Participants
It is seen that nearly 9.8% of participants in the age of 51–60 years reported neurological symptoms compared to 4.9% of them who were in the age of 31–40 years which was statistically significant (P = .050). Similarly, 2.3% of participants who were discharged with minimal support had reported reduced urine output than .3% of participants who were discharged with no support, which was statistically significant (P = .045). It was also observed that 16.7% of subjects who had >1 month of hospital stay reported psychological symptoms compared to 6.1% of them who were discharged in less than 10 days. Similar findings were seen when 16.7% who stayed >1 month reported abdominal symptoms than 9.6% of them who left hospital within 10 days though these findings were statistically not significant. It was observed that both males and females reported general symptoms (M = 47%, F = 42.7%) and psychological symptoms (M = 34.3%, F = 34.8%) equally and these findings were not significant statistically, whereas 12.1% of females reported abdominal symptoms compared to 8.9% of males and this finding was significant (P = .050); 3% males suffered more cardio-respiratory symptoms than 1.9% of females and this was also not significant.
Multinominal Regression Analysis for Independent Risk Factors of Follow-up Symptoms
Under multinominal regression with system-based symptoms and age, condition on discharge, months of admission, having pre-existing diabetes mellitus, and pre-existing hypertension which were significant previously, we observed that those with diabetes mellitus had independent risk of getting cardio-respiratory symptoms (P = .05, AOR = 2.29, CI = 1.97–5.40) and neurological symptoms (P = .00, AOR = 2.64, CI = 1.46–4.77) on follow-up. Similarly, those who were discharged with support had independent risk of getting renal symptoms such as reduced urine output (P = .01, AOR=6.26, CI = 1.47–26.64) on follow-up. These findings are shown in Table 4.
Table 4.
Multi-nominal logistic regression analysis parameters with system-based post-discharge symptoms (N = 1354).
| Parameters | General symptoms | Cardio-respiratory symptoms | Abdominal symptoms | Psychological symptoms | Neurological symptoms | Renal symptoms | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AOR (CI) | P value | AOR (CI) | P value | AOR (CI) | P value | AOR (CI) | P value | AOR (CI) | P value | AOR (CI) | P value | |
| Age (years) | ||||||||||||
| >60 | .91 | .54 | .98 | .98 | .75 | .28 | .81 | .19 | .52 | .07 | .52 | .96 |
| - < 60R | (.69–1.21) | (.41–2.33) | (.44–1.26) | (.60–1.10) | (.26–1.05) | (.37–4.08) | ||||||
| Condition on discharge | ||||||||||||
| With support | .97 | .92 | 1.23 | .83 | 1.46 | .53 | .98 | .96 | .61 | .37 | 6.26 | .01* |
| With No supportR | (.53–1.75) | (.16–9.34) | (.44–4.81) | (.53–1.84) | (.21–1.80) | (1.47–26.64) | ||||||
| Month of admission | ||||||||||||
| June–August | 1.21 | .08 | .94 | .86 | .83 | .32 | 1.13 | .30 | .90 | .67 | 1.52 | .23 |
| September–NovemberR | (.97–1.51) | (.47–1.85) | (.57–1.20) | (.89–1.42) | (.57–1.43) | (.70–3.33) | ||||||
| Diabetes mellitus | ||||||||||||
| Yes | .77 | .16 | 2.29 | .05* | .89 | .74 | 1.02 | .88 | 2.64 | .00* | .79 | .99 |
| NoR | (.53–1.11) | (1.97–5.40) | (.46–1.72) | (.70–1.50) | (1.46–4.77) | (.38–1.61) | ||||||
| Hypertension | ||||||||||||
| Yes | 1.21 | .50 | .85 | .87 | 1.6 | .24 | .77 | .43 | 1.22 | .73 | 1.58 | .48 |
| NoR | (.68–2.15) | (.11–6.42) | (.71–3.76 | (.41–1.46) | (.37–4.08) | (.43–5.80) | ||||||
AOR, adjusted odds ratio; CI, confidence interval. *P value <.05 is significant.
Discussion
To our knowledge, there are no studies conducted so far in India regarding the COVID-19 follow-up in detail, and this study is one which was conducted with large number of recovered patients and thus the results are compared with that of the global data available.
Gender-Based Differences Observed on Follow-up
It was seen that 73% males reported follow-up symptoms compared to only 27% of females and the males developed more cardio-respiratory and neurological symptoms compared to females. These findings were similar to other studies13-16 conducted globally in China, USA, South Korea, and Italy that males suffered more with the disease than females. Jordan et al. 17 on analyzing global aggregate data have reported that males suffer severe form of disease and death compared to females. This contrast finding may mostly be due to the genetic factors of male and also due to the behavioral risk factors like smoking and alcohol being most common lifestyle among males compared to females.
Severity of Symptoms Observed on Follow-up
It is observed that only 39.7% of the subjects in this study showed the highest reported symptoms on follow-up which was very minimal as compared to the studies conducted in Western countries where nearly 2/3rd of the people had symptoms by 2 months in a study conducted in France by Schneider et al. 18 and study done by Yvonne et al. 19 among the Netherlands and Belgium population stated that only .7% of the respondents were asymptomatic, 79 days after the infection. Similarly, an UK-based study 20 showed that 74% of their subjects continued to have at least one symptom during follow-up and it was stated that their overall health-related quality of life was reduced. A study conducted by Liang et al. 21 in China showed that 91% of their subjects returned to work at 3 months after discharge. This finding shows that the Asian population was less affected with sequalae of COVID-19 than their Western counterpart, though a complete opinion about this remains limited.
Symptoms Reported on Follow-up
The most common symptoms reported in this study were tiredness (39.7%), stress and anxiety (27.6%), mood changes (5.8%), and myalgia (5.1%). Although a significant number expressed that their mood changes depended on their sleep level and 3.6% had disturbed sleep, it was observed that fatigue or tiredness was the most common symptom which was reported all around the world as a major component of post-COVID-19 sequelae. Arnold et al. 20 in his study in UK reported 39% had fatigue and 24% had insomnia. In a study conducted by Carfi 7 in Italy, it was reported 53.1% had fatigue and 27.3% had joint pain which was similar to our results. Similar findings were also reported by Liang et al. 21 that 60% of their subjects suffered fatigue. On looking into psychological aspect, a majority of them suffered stress and anxiety in our study and these findings were similar by the report given by Gopal A et al. 22 that anxiety, stress, and depressive symptoms increased during the lockdown among adults in India. Another report by Balachander et al. 23 stated that the recovered patients might suffer anxiety, stress, and depression for an extended period as they may fear re-infection and might also have the fear of infecting others.
Factors Influencing the Symptoms Reported
This study reported that increased age, having diabetes mellitus and hypertension, being admitted in months of June to August, and being discharged with support showed significant association with having some or few system-based post-COVID symptoms. The study done in France 18 reported that subjects with age between 40 and 60 years had significant prolonged symptoms. The striking finding in this study was having significant association with more cases which were admitted in the months of June to August had more symptoms than those admitted in September to November. This can be due to the changing environmental conditions over the year as stated by the report given by Sammadar et al. 24 that the weather impacts with the varied transmission dynamics as it is hight in presence of cold/or dry air. Advanced management of the disease with better facilities in later months than former could also impact this finding significantly.
Limitations and Strengths
The results cannot be generalized as it is a single-center study which involved only a particular category of subjects with almost similar sociodemographic and environmental background. The study was not able to observe a clear post-COVID-19 sequalae, as most of the subjects suffered only mild form of the disease. Information and recall bias are unavoidable as the period of time involved with symptoms was being observed and that may vary invariably. The association tables were not shown as they were lengthy and also due to the word count constraints. The major strength of this study would be that 1354 of the recovered patients were traced and contacted over a phone call as this study will be an epitome to express the ignition of telehealth in India that it is possible to achieve in our country too like our Western counterparts. The findings of this study can also be useful to promote the usefulness of vaccinations and prevention of further transmission. For the future studies on the follow-up symptoms, we recommend the researchers to formulate a Likert scale (ordinal data) to attain more accurate results as it will be difficult to quantify the symptoms.
Conclusion
The COVID-19 pandemic has affected the whole world in one way or the other and the prevailing chronic symptoms of the disease after the recovery are one of it. Existing health conditions and the severity of the disease will have major impact in the post-COVID-19 sequalae. It is notable that increasing age and presence of comorbid conditions such as diabetes mellitus and hypertension are risk factors for having persistent symptoms during the follow-up period. Thus, more follow-up studies must come up to understand the complete picture of the disease and also to observe its major determinants across the world.
Acknowledgments
The authors would like to thank the management of the Medical College and Hospital, Chennai in supporting the study for the prompt completion. The authors also acknowledge the efforts taken by the postgraduates and house surgeons who worked in this study. Lastly, all the study participants who co-operated in this study are also remembered.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article
ORCID iD
G Shiny Chrism Queen Nesan https://orcid.org/0000-0002-1668-3307
References
- 1.WHO . Coronavirus Disease (COVID-19) - Events as They Happen. Geneva, Switzerland: Who.int.; 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. Accessed February 22, 2021. [Google Scholar]
- 2.Boseley S. WHO declares coronavirus pandemic. The Guardian. 2020. https://www.theguardian.com/world/2020/mar/11/who-declares-coronavirus-pandemic. Accessed February 22, 2021. [Google Scholar]
- 3.Weerahandi H, Hochman KA, Simon E, et al. Post-discharge health status and symptoms in patients with severe COVID-19. J Gen Intern Med. 2021;36:738-745. doi: 10.1007/s11606-020-06338-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greenhalgh T, Knight M, A’Court C, et al. Management of post-acute covid-19 in primary care. BMJ. 2020:m3026. [DOI] [PubMed] [Google Scholar]
- 5.Kebede T, Kumar D, Sharma PK. Symptoms, transmission, prevention and treatment of pandemic corona virus: a review. Coronaviruses. 2021;2:151-158. doi: 10.2174/2666796701999200713191436. [DOI] [Google Scholar]
- 6.Rosales-Castillo A, García de los Ríos C, Mediavilla García JD. Persistent symptoms after acute COVID-19 infection: importance of follow-up. Med Clínica. 2021;156(1):35-36. doi: 10.1016/j.medcle.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carfì A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. J Am Med Assoc. 2020;324(6):603. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kamal M, Abo Omirah M, Hussein A, Saeed H. Assessment and characterisation of post‐COVID‐19 manifestations. Int J Clin Pract. 2020;75. doi: 10.1111/ijcp.13746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Hindu . Coronavirus | major medical college hospitals in Tamil Nadu will have follow-up clinics. The Hindu. 2020. https://www.thehindu.com/news/national/tamil-nadu/coronavirus-major-medical-college-hospitals-in-tamil-nadu-will-have-follow-up-clinics/article32398291.ece. Accessed February 23, 2021. [Google Scholar]
- 10.HHS . Obtaining Informed Consent | Telehealth. Washington, DC: United States Department of Health and Human Services; 2020. https://telehealth.hhs.gov/providers/preparing-patients-for-telehealth/obtaining-informed-consent/. Accessed February 23, 2021. [Google Scholar]
- 11.Mohfw.gov.in . 2020. https://www.mohfw.gov.in/pdf/UpdatedClinicalManagementProtocolforCOVID19dated03072020.pdf. Accessed February 23, 2021.
- 12.Mohfw.gov.in . 2021. https://www.mohfw.gov.in/pdf/ReviseddischargePolicyforCOVID19.pdf. Accessed February 23, 2021.
- 13.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708-1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Faure E, Kipnis E, Bortolotti P, Salik J. Clinical characteristics of Covid-19 in New York City. N Engl J Med. 2020;29(1):2016-2017. [Google Scholar]. [Google Scholar]
- 15.Shim E, Tariq A, Choi W, Lee Y, Chowell G. Transmission potential and severity of COVID-19 in South Korea. Int J Infect Dis. 2020;93:339-344. doi: 10.1016/j.ijid.2020.03.031. [PMC free article] [PubMed] [CrossRef] [Google Scholar]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. J Am Med Assoc. 2020;323:1775-1776. [PubMed] [Google Scholar]. [DOI] [PubMed] [Google Scholar]
- 17.Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ. 2020;368(March):m1198. doi: 10.1136/bmj.m1198. [PubMed] [CrossRef] [Google Scholar]. [DOI] [PubMed] [Google Scholar]
- 18.Carvalho-Schneider C, Laurent E, Lemaignen A, et al. Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin Microbiol Infect. 2021;27(2):258-263. doi: 10.1016/j.cmi.2020.09.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goërtz YMJ, Van Herck M, Delbressine JM, et al. Persistent symptoms 3 months after a SARS-CoV-2 infection: the post-COVID-19 syndrome? ERJ Open Research. 2020;6(4):00542-02020. doi: 10.1183/23120541.00542-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arnold DT, Hamilton FW, Milne A, et al. Patient outcomes after hospitalisation with COVID-19 and implications for follow-up: results from a prospective UK cohort. Thorax. 2020;76:399-401. doi: 10.1136/thoraxjnl-2020-216086. thoraxjnl-2020-216086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liang L, Yang B, Jiang N, et al. Three-month follow-up study of survivors of coronavirus disease 2019 after discharge. J Kor Med Sci. 2020;35(47). doi: 10.3346/jkms.2020.35.e418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gopal A, Sharma AJ, Subramanyam MA. Dynamics of psychological responses to COVID-19 in India: a longitudinal study. PLoS One. 2020;15(10):e0240650. doi: 10.1371/journal.pone.0240650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Balachandar V, Mahalaxmi I, Subramaniam M, et al. Follow-up studies in COVID-19 recovered patients - is it mandatory?. Sci Total Environ. 2020;729:139021. doi: 10.1016/j.scitotenv.2020.139021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Samaddar A, Gadepalli R, Nag VL, Misra S. The enigma of Low COVID-19 fatality rate in India. Front Genet. 2020;11. doi: 10.3389/fgene.2020.00854. [DOI] [PMC free article] [PubMed] [Google Scholar]