Abstract
Objectives:
During 2010-2018, the Arkansas Department of Health reported 21 genotype-matched cases of tuberculosis (TB) among residents of a rural county in Arkansas with a low incidence of TB and in nearby counties. The Arkansas Department of Health and the Centers for Disease Control and Prevention investigated to determine the extent of TB transmission and provide recommendations for TB control.
Methods:
We reviewed medical and public health records, interviewed patients, and reviewed patients’ social media posts to describe patient characteristics, identify epidemiologic links, and establish likely chains of transmission.
Results:
We identified 21 cases; 11 reported during 2010-2013 and 10 during 2016-2018. All case patients were US-born non-Hispanic Black people. Eighteen case patients had the outbreak genotype, and 3 clinically diagnosed (non–culture-confirmed) case patients had epidemiologic links to patients with the outbreak genotype. Social media reviews revealed epidemiologic links among 10 case patients not previously disclosed during interviews. Eight case patients (38%) had ≥1 health care visit during their infectious period, and 7 patients had estimated infectious periods of >12 months.
Conclusions:
Delayed diagnoses and prolonged infectiousness led to TB transmission in this rural community. TB education and awareness is critical to reducing transmission, morbidity, and mortality, especially in areas where health care providers have limited TB experience. Use of social media can help elucidate people at risk, especially when traditional TB investigation techniques are insufficient.
Keywords: tuberculosis, outbreak response, rural health
Tuberculosis (TB) outbreaks in the United States are frequently associated with congregate settings in urban areas.1,2 However, TB outbreaks also occur in rural, community settings,3,4 where public health resources are often limited and health care providers may have little, if any, experience with TB.
During 2010-2018, the Arkansas Department of Health (ADH) identified 21 cases of TB with a unique genotype not seen elsewhere in the United States: 11 cases during 2010-2013 and 10 cases during 2016-2018. During 2010-2012, ADH initially identified many epidemiologic links among patients and 1 site of potential transmission. However, investigations of cases reported during 2016-2018 did not reveal connections to previous cases for at least 3 patients or clear factors leading to ongoing transmission. In May 2018, ADH and the Centers for Disease Control and Prevention (CDC) conducted a TB outbreak investigation among case patients in a rural county in Arkansas (county A) and in nearby counties to identify likely chains of transmission and provide setting-specific recommendations to stop transmission.
Methods
TB Surveillance and Laboratory Methods
The National Tuberculosis Surveillance System collects data on demographic and clinical characteristics and medical and social risk factors for TB for each newly reported TB case patient in the United States. Since 2009, CDC has offered genotyping of at least 1 isolate for every culture-confirmed TB case in the United States using 2 standard methods: spacer oligonucleotide typing and 24-locus mycobacterial interspersed repetitive units variable-number tandem repeat (MIRU-VNTR). 5 Whole-genome sequencing (WGS) of Mycobacterium tuberculosis isolates is also available by request through CDC, and CDC conducted sequencing for all isolates with the outbreak genotype. CDC performed reference-based WGS alignments and high-quality, single nucleotide polymorphism (SNP) analyses to identify SNP differences between patient isolates.
Case Definitions
We calculated TB rates using case data reported to the National Tuberculosis Surveillance System and population data from the US Census Bureau. 6 We defined an epidemiologic link between cases as (1) a patient with TB naming another patient with TB, (2) two patients who have not directly named each other but who name a shared contact, (3) two patients associated with the same location at the same time (eg, house, building, business), or (4) two patients who are connected through social media. We distinguished between name- and location-based epidemiologic links and social media epidemiologic links. We identified and categorized outbreak cases into 1 of 2 case classifications. We defined a confirmed outbreak case as TB in a person with culture-confirmed disease reported during January 1, 2010–July 1, 2018, in the United States with (1) the outbreak genotype as defined by spacer oligonucleotide typing and MIRU-VNTR and (2) WGS results within 5 SNPs of another outbreak case’s isolate.7,8 We defined a probable outbreak case as TB in a person with culture-negative disease reported during the same period and an epidemiologic link to a person who meets the confirmed outbreak case definition.
Record Reviews
We systematically abstracted patient information from medical and public health records, including demographic information; clinical characteristics; the first date on which a patient had symptoms consistent with TB; dates and reason for health care encounters; periods of incarceration in local jails or state prisons; dates of attendance at school, church, or other potential locations of exposure; and treatment outcomes. Through reviewing health care encounters, we estimated the number of patients with a delayed TB diagnosis, defined as receiving a diagnosis of TB after the patient sought care with signs and symptoms consistent with TB but initially received a non-TB diagnosis. We reinterviewed 5 recent case patients and 3 proxies for a deceased patient to identify possible epidemiologic links to other TB cases and any potential common locations where TB transmission may have occurred.
We reviewed social media content posted by patients to their Facebook profiles with the “public” audience privacy setting that allowed viewing by anyone on the internet to supplement identification of possible epidemiologic links and transmission sites; no content with a “friends only” or more restrictive audience privacy setting was accessed or included in these reviews. If known case patients were found to be Facebook friends, to post on each other’s Facebook “wall,” or to check in virtually on Facebook at the same location, we considered this link a social media epidemiologic link.
We calculated infectious periods using CDC guidelines. 9 For people with symptomatic pulmonary disease, we measured the infectious period as the 3 months before the date of symptom onset or first documented finding consistent with TB; for people who reported no TB symptoms, we measured the infectious period as 1 month before the date of first documented finding consistent with TB. We defined the end of the infectious period as when a patient was placed under airborne infection isolation or when a patient completed 2 weeks of TB therapy with an effective regimen and showed improvement in clinical symptoms and sputum smear results (ie, decrease in the quantity of TB acid-fast bacilli detected on sputum-smear microscopy using the standard scale provided by the American Thoracic Society: no acid-fast bacilli seen, doubtful/repeat test, rare [1+], few [2+], moderate [3+], numerous [4+]). 10 Using estimated infectious periods and clinical indicators of infectiousness, we identified potential sites and periods of transmission that were shared with local health officials to facilitate follow-up with exposed contacts for evaluation and targeted TB education.
The University of Arkansas for the Medical Sciences considered this work to be nonresearch because it was a public health response. CDC determined that this outbreak investigation did not constitute human subjects research and therefore waived institutional review board review.
Results
In line with previous investigations by ADH, we identified 21 cases of TB disease that met the confirmed and probable case definitions among 20 people; 1 person was diagnosed with TB twice. Eleven cases were reported during 2010-2013 and 10 during 2016-2018 (Figure 1). All case patients were US-born non-Hispanic Black people, and all either lived in county A or had personal connections to people who lived in county A (Table). Whole-genome SNP analysis demonstrated that isolates from all culture-confirmed outbreak cases were within 2 SNPs of at least 1 other isolate.
Figure 1.
Tuberculosis (TB) outbreak–associated cases in rural Arkansas, 2010-2018. A confirmed outbreak case was defined as TB in a person with culture-confirmed disease reported during January 1, 2010–July 1, 2018, in the United States with (1) the outbreak genotype defined by spacer oligonucleotide typing and 24-locus mycobacterial interspersed repetitive units variable-number tandem repeat and (2) whole-genome sequencing results within 5 single nucleotide polymorphisms of an isolate of another outbreak case. A probable outbreak case was defined as TB in a person with culture-negative disease reported during the same period and an epidemiologic link to a person meeting the definition of a confirmed outbreak case.
Table.
Demographic and clinical characteristics of tuberculosis outbreak–associated patients (N = 21), rural Arkansas, 2010-2018
| Characteristic | No. (%) of patients |
|---|---|
| Epidemiologic | |
| Confirmed | 18 (86) |
| Probable | 3 (14) |
| Epidemiologic link to county A | 21 (100) |
| Demographic | |
| Female | 13 (62) |
| Median age (IQR), y | 31 (19-38) |
| Patients aged <15 y | 5 (24) |
| US born | 21 (100) |
| Non-Hispanic Black | 21 (100) |
| Social risk | |
| Excess alcohol use | 7 (33) |
| Noninjection drug use | 5 (24) |
| History of homelessness | 1 (5) |
| Diagnosed while incarcerated | 2 (10) |
| Clinical | |
| Previous TB diagnosis | 1 (5) |
| Pulmonary TB | 19 (90) |
| Infectiousness a | |
| Smear positive or cavitary | 12 (57) |
| Smear negative and noncavitary | 7 (33) |
| Extrapulmonary TB only | 2 (10) |
| Median infectious period b in months (IQR) | 12 (6-17) |
| Infectious period b ≥12 mo | 7 (50) |
| HIV-positive | 0 |
| Resistance to any first-line drug | 0 |
| Delayed TB diagnosis | 8 (33) |
| Initial sarcoidosis diagnosis | 2 (29) |
| Completed treatment | 19 (90) |
| Died while being treated | 2 (10) |
Abbreviations: IQR, interquartile range; TB, tuberculosis.
Based on site of TB disease, sputum smear results, and chest radiography results.
Estimated infectious period for 14 adult pulmonary TB cases; calculated in number of months based on Centers for Disease Control and Prevention guidelines. 6
After reviewing clinical indicators of infectiousness, epidemiologic links to other outbreak cases, and genetic relatedness of patients’ TB isolates, we identified a likely source case diagnosed early in the outbreak period (Figure 2, case 1). This case occurred in a patient who had symptoms of TB disease for 6 months before being diagnosed with pulmonary TB disease at a local hospital. We identified epidemiologic links to 4 other cases and social media connections between 10 more case pairs.
Figure 2.
Social network diagram of confirmed or probable tuberculosis (TB) outbreak–associated cases (N = 21), rural Arkansas, 2010-2018. Social network diagram made using MicrobeTrace version 0.5.3 (Centers for Disease Control and Prevention).
The likely source case for the second wave of the outbreak that started in 2016 (Figure 2, case 14) was a patient who was diagnosed with pulmonary TB at a local hospital after evaluation for persistent pneumonia. This patient was contagious for 10 months before diagnosis, was epidemiologically linked to 2 other cases, and had social media links to 4 more cases. Several other contacts were identified with latent TB infection.
Among the 21 cases, we found epidemiologic links among all but 2 patients; in addition, 10 of the case patients’ home addresses were clustered within 2 neighborhoods.
Delayed Diagnosis
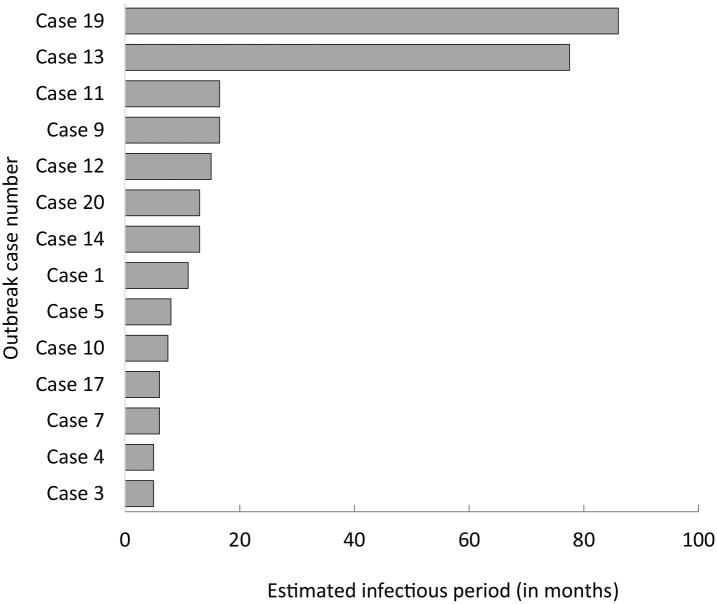
Of 21 outbreak cases, 14 were adult patients with pulmonary TB. All 14 adult patients with pulmonary TB were potentially contagious for at least 4 months, and 7 were contagious for >12 months (Figure 3). Medical record reviews indicated that 8 (38%) patients had a delayed diagnosis, seeking medical care a combined 31 times at local facilities during their infectious periods, several with symptoms consistent with TB, but were diagnosed with other conditions for months or years before their TB diagnoses. Two of these patients were diagnosed with sarcoidosis and treated with corticosteroids. Two patients, including 1 originally diagnosed with sarcoidosis, died during evaluation or treatment for TB; 1 died from sepsis and the other from TB meningitis.
Figure 3.
Estimated infectious period for tuberculosis outbreak–associated adult patients (n = 14) with pulmonary tuberculosis disease, rural Arkansas, 2010-2018.
Exposures in Health Care Facilities
In 2 health care facilities frequented by several patients during their infectious periods, we calculated 34 inpatient days during infectious periods in 1 hospital and 81 inpatient days during infectious periods in the other facility. We identified a previously unknown epidemiologic link between 2 patients with an overlapping hospitalization of 4 days in nearby rooms during one of the patient’s infectious periods. The patient with active disease had cavitary pulmonary disease and was not in airborne isolation at the time. Although none of the health care facilities reported any new TB infections among hospital staff members, the underlying diagnoses of several contagious patients were previously unknown to health care facility staff members because of delayed or missed diagnosis of TB disease.
Perceived Stigma and Contact Disclosure
We identified 12 epidemiologic links via social media reviews during the investigation that had not been previously noted among patients (Figure 2). Nurses at the local health unit communicated that patients were hesitant to name contacts and often reported few, if any, contacts outside the household. On reinterview, some patients conveyed that stigma in the community was a main reason that they were not initially forthcoming with naming contacts and that education in the community in general helps to address stigma and elicit more contacts during this ongoing investigation.
Discussion
Through our investigation, we identified an outbreak of TB in a rural setting with evidence of 2 periods of recent and ongoing transmission. Our findings suggest that delays in diagnosis, specifically for 2 patients, created opportunities for transmission within the community. Whole-genome SNP analysis results were consistent with epidemiologic data, suggesting recent and ongoing transmission among cases. 11 This outbreak occurred in a county in Arkansas that had reported only 1 case of TB in the 5 years before 2010 (unpublished data, Arkansas Department of Health, 2005-2009), when the first outbreak-associated case was reported. During 2010-2018, the average rate of TB per 100 000 population in Arkansas was 2.6 cases, consistent with the national rate, 11 and the average rate of TB in county A was 17 cases, which was 6.5 times higher than the state TB rate.
This TB outbreak occurred in a rural, impoverished community, 12 underscoring the need for sustained resources to conduct rapid case finding, provide treatment, evaluate contacts, and educate community members and health practitioners about TB disease. Other states have also encountered TB outbreaks in rural communities in recent years. In 2011, Mississippi public health authorities detected a cluster of 9 genotype-matched cases of TB associated with close community contact after 2 hurricane seasons caused displacement in the affected area. 3 Public health authorities in Mississippi also noted delayed diagnosis in patients who presented to hospitals with symptoms of TB. An outbreak in rural Georgia in 1996 identified both delayed diagnosis and delayed disclosure of contacts as issues encountered in outbreak response, requiring intensive community outreach. 4 In both examples, all but 1 patient was born in the United States. Social- or community-based transmission was the most likely source, illustrating the diverse settings and challenges associated with TB outbreaks.
In this outbreak investigation, social media reviews of publicly available information played a key role in uncovering previously unidentified social- and community-based epidemiologic links among patients. Social media is a relatively new and constantly evolving tool that can be used to better understand social connections among patients and potential sites of transmission. Although substantial literature has examined the use of social media in communication, literature exploring the use of social media in outbreak investigations is scarce. We found 1 study in Virginia that used social media to connect patients from 2 TB clusters that occurred several years apart. 13 In addition, an outbreak investigation team in Canada asked patients or their guardians to review social media posts for possible contacts, a strategy that could promote trust by engaging the patient when using social media for enhanced investigations. 14
The use of social media as a resource in outbreak investigations highlights an area for continued research. More investigation is needed to discover the best strategies and practices to use it effectively and ethically. Social media networks strengthen the epidemiologic links between cases, especially when patients are hesitant to name contacts or potential source cases. Knowing that cases are linked can save valuable time and resources from trying to identify missed cases or additional sites of transmission not yet identified. Using social media can also help identify additional people who may be at risk of exposure to TB infection. Investigators should weigh the public health benefit of better understanding social connections between patients in an outbreak with the potential harms of uncovering personal information that was not volunteered by the patient. Utmost care should be practiced to preserve the patient’s privacy and dignity while using social media searches to supplement an understanding of transmission to stop outbreaks.
Delayed diagnosis of TB, even in patients with cavitary disease, led to prolonged infectious periods and poor outcomes among patients in this outbreak. These delays could have been the result of a lack of health care provider awareness about TB. In the 5 years preceding this outbreak in the most highly affected county, only 1 case of TB had been reported. Recent evidence suggests that delayed diagnosis of TB is a nationwide problem; patients are increasingly diagnosed with advanced TB disease, likely attributable in part to the decreasing incidence of TB, which leads to decreasing awareness of TB among health care providers. 15 In a population-based study from California in 2015, up to 33% of TB cases were among people who had made at least 1 visit to an emergency department or had a hospitalization related to a respiratory diagnosis, encounters that could have represented a missed TB diagnosis. The proportion of missed diagnoses increased with decreasing incidence of TB in the reporting institution. 16
When patients present with symptoms of TB, they may often be treated initially for community-acquired pneumonia instead of TB because of an overlap in symptoms. 17 Although community-acquired pneumonia is more common than TB, health care providers should consider TB when patients do not respond to antibiotic therapy or have other symptoms consistent with TB, such as weight loss, night sweats, cough >3 weeks, or hemoptysis, especially when transmission is occurring in the community. Health care providers should also carefully consider use of fluoroquinolone monotherapy as initial therapy for presumptive diagnoses of community-acquired pneumonia, especially in patients at high risk for TB, because TB symptoms will often temporarily improve during fluoroquinolone treatment, thereby further delaying correct diagnosis. Use of fluoroquinolone monotherapy in patients who have TB can also inadvertently lead to acquisition of fluoroquinolone-resistant TB. 18
Delayed TB diagnosis is a risk factor for TB transmission; therefore, timely evaluation, diagnosis, and treatment of active TB is critical to reducing transmission and TB-associated morbidity and mortality. 19 Public health departments can assist health care providers by alerting them when they detect evidence of transmission in their communities or suspect an outbreak. If health care providers are aware that TB is circulating, they may be more likely to include it in their differential diagnosis along with pneumonia, bronchitis, and other respiratory infections when evaluating patients with symptoms of TB than if they are not aware that TB is present in the community.
TB and pulmonary sarcoidosis can have similar clinical presentations with nonspecific symptoms. The reported incidence of sarcoidosis in the United States is estimated to be about 6 cases per 100 000 population, 20 whereas the incidence of TB is 2.8 cases per 100 000 population. 21 Current clinical practice guidelines recommend excluding other granulomatous diseases, including TB, during diagnostic evaluations for sarcoidosis. 20 Because of the nonspecific clinical presentation and the lack of diagnostic tests that are 100% sensitive, medical providers should consider sarcoidosis and TB in their differential diagnoses of granulomatous and respiratory diseases to perform diagnostic evaluations in appropriate circumstances, such as patients diagnosed with community-acquired pneumonia with persistent symptoms and signs despite appropriate antibiotic therapy.
During our investigation, stigma and lack of community awareness were reasons people cited for their initial hesitancy to disclose contacts to public health workers. This finding is also common in rural settings. 22 A study of patients with TB and health care workers in several counties in Georgia, Tennessee, and North Carolina found that the fear of stigma was an important factor in the nondisclosure of contacts and was most noted among residents of rural communities, 23 consistent with our findings in the rural Arkansas population. In addition, study participants reported that they trusted their local health department staff members and information that was communicated to them by their physicians and reported that mass media and word of mouth was the best way to disseminate information about TB to the communities while reducing stigma associated with restricting information to only those affected. 23 A framework developed for addressing the rising number of cases of HIV/AIDS among African American people in rural Alabama found that the primary barriers to successful interventions were stigma, fear, and denial. 24 When TB outbreaks occur in rural areas, outreach and communication should focus on reducing stigma by using culturally appropriate and community-tailored interventions. Culturally appropriate communication on TB transmission, diagnosis, and treatment should be prioritized to improve community-wide understanding of the disease and enhance contact-tracing efforts in rural communities that are experiencing outbreaks.
Limitations
This study had several limitations. First, few contacts were named or had confirmed TB testing during contact investigations during 2016-2018, thereby limiting the extent of contact tracing. Second, although social media links suggested a common social network among people in this outbreak, they did not prove in-person interactions as definitive evidence of transmission. Third, reinterviews were possible with only 5 people because of the availability of case patients, and interviews by proxy had to be conducted for 1 decedent, limiting the availability of follow-up data. Despite these limitations, our findings from medical record abstractions, interviews with patients, results of the whole-genome SNP analysis, and social media searches all provided strong evidence of ongoing community transmission fueled by delayed diagnoses of TB disease.
Conclusion
This TB outbreak in a rural area in Arkansas with a low incidence of TB illustrates some of the challenges of TB elimination in the United States, including delayed diagnosis, perceived stigma among patients, and prolonged infectious periods leading to disease transmission and morbidity and mortality. Continued targeted education of health care providers, public health officials, and communities is needed to reduce delayed diagnosis, transmission of disease, and morbidity and mortality among people with TB. Use of social media can be an important adjunct to traditional field-based TB investigations, especially in settings in which stigma surrounding TB diagnosis and mistrust of the health care system create challenges in identifying contacts.
Acknowledgments
The authors acknowledge Dirk Haselow, MD, PhD; Courtney Radcliff; J. Gary Wheeler, MD, MS; Naveen Patil, MD; and Gail Grant for their support.
Footnotes
Disclaimer: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the Arkansas Department of Health.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Arkansas Department of Health and CDC.
ORCID iD: Sarah M. Labuda, MD, MPH  https://orcid.org/0000-0002-3312-681X
https://orcid.org/0000-0002-3312-681X
References
- 1. Mindra G, Wortham JM, Haddad MB, Powell KM. Tuberculosis outbreaks in the United States, 2009-2015. Public Health Rep. 2017;132(2):157-163. doi: 10.1177/0033354916688270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Powell KM, VanderEnde DS, Holland DP, et al. Outbreak of drug-resistant Mycobacterium tuberculosis among homeless people in Atlanta, Georgia, 2008-2015. Public Health Rep. 2017;132(2):231-240. doi: 10.1177/0033354917694008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bloss E, Newbill K, Peto H, et al. Challenges and opportunities in a tuberculosis outbreak investigation in southern Mississippi, 2005-2007. South Med J. 2011;104(11):731-735. doi: 10.1097/SMJ.0b0.3e318232679e [DOI] [PubMed] [Google Scholar]
- 4. Bock NN, Mallory JP, Mobley N, DeVoe B, Taylor BB. Outbreak of tuberculosis associated with a floating card game in the rural South: lessons for tuberculosis contact investigations. Clin Infect Dis. 1998;27(5):1221-1226. doi: 10.1086/514986 [DOI] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention. Overview of the CDC tuberculosis genotyping program. 2012. Accessed October 22, 2020. https://www.cdc.gov/tb/programs/genotyping/chap1/intro_3_overview.htm
- 6. US Census Bureau. American Community Survey (ACS) demographic and housing estimates. 2010-2019. Accessed November 22, 2019. https://data.census.gov/cedsci/table?q=arkansaspopulationbycounty&tid=ACSDP5Y2019.DP05&hidePreview=false
- 7. Meehan CJ, Goig GA, Kohl TA, et al. Whole genome sequencing of Mycobacterium tuberculosis: current standards and open issues. Nat Rev Microbiol. 2019;17(9):533-545. doi: 10.1038/s41579-019-0214-5 [DOI] [PubMed] [Google Scholar]
- 8. Walker TM, Ip CLC, Harrell RH, et al. Whole-genome sequencing to delineate Mycobacterium tuberculosis outbreaks: a retrospective observational study. Lancet Infect Dis. 2013;13(2):137-146. doi: 10.1016/S1473-3099(12)70277-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. National Tuberculosis Controllers Association, Centers for Disease Control and Prevention. Guidelines for the investigation of contacts of persons with infectious tuberculosis. Recommendations from the National Tuberculosis Controllers Association and CDC. MMWR Recomm Rep. 2005;54(RR-15):1-47. [PubMed] [Google Scholar]
- 10. American Thoracic Society. Diagnostic standards and classification of tuberculosis. Am Rev Respir Dis. 1990;142(3):725-735. doi: 10.1164/ajrccm/142.3.725 [DOI] [PubMed] [Google Scholar]
- 11. Centers for Disease Control and Prevention. Table 1: tuberculosis cases, case rates per 100,000 population, deaths, and death rates per 100,000 population, and percent change: United States, 1953-2018. Accessed November 1, 2019. https://www.cdc.gov/tb/statistics/reports/2018/table1.htm
- 12. US Census Bureau. Selected economic characteristics: American Community Survey, 2010-2019. Accessed November 22, 2019. https://data.census.gov/cedsci/table?g=0400000US05&tid=ACSDP5Y2019.DP03
- 13. Thomas TA, Heysell SK, Houpt ER, Moore JL, Keller SJ. Outbreak of pyrazinamide-monoresistant tuberculosis identified using genotype cluster and social media analysis. Int J Tuberc Lung Dis. 2014;18(5):552-558. doi: 10.5588/ijtld.13.0663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gournis E, Shane A, Shane E, Arthur A, Berger L. Exploring gaps in surveillance of a small measles outbreak in Toronto, Canada. Can Commun Dis Rep. 2016;42(7):146-148. doi: 10.14745/ccdr.v42i07a02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wallace RM, Kammerer JS, Iademarco MF, Althomsons SP, Winston CA, Navin TR. Increasing proportions of advanced pulmonary tuberculosis reported in the United States: are delays in diagnosis on the rise? Am J Respir Crit Care Med. 2009;180(10):1016-1022. doi: 10.1164/rccm.200901-0059OC [DOI] [PubMed] [Google Scholar]
- 16. Miller AC, Polgreen LA, Cavanaugh JE, Hornick DB, Polgreen PM. Missed opportunities to diagnose tuberculosis are common among hospitalized patients and patients seen in emergency departments. Open Forum Infect Dis. 2015;2(4):ofv171. doi: 10.1093/ofid/ofv171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Shen G-H, Tsao TC-Y, Kao S-J, et al. Does empirical treatment of community-acquired pneumonia with fluoroquinolones delay tuberculosis treatment and result in fluoroquinolone resistance in Mycobacterium tuberculosis? Controversies and solutions. Int J Antimicrob Agents. 2012;39(3):201-205. doi: 10.1016/j.ijantimicag.2011.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kim H, Mok JH, Kang B, et al. Trend of multidrug and fluoroquinolone resistance in Mycobacterium tuberculosis isolates from 2010 to 2014 in Korea: a multicenter study. Korean J Intern Med. 2019;34(2):344-352. doi: 10.3904/kjim.2018.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Golub JE, Bur S, Cronin WA, et al. Delayed tuberculosis diagnosis and tuberculosis transmission. Int J Tuberc Lung Dis. 2006;10(1):24-30. [PubMed] [Google Scholar]
- 20. Statement on Sarcoidosis. Joint statement of the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) adopted by the ATS Board of Directors and by the ERS Executive Committee, February 1999. Am J Respir Crit Care Med. 1999;160(2):736-755. doi: 10.1164/ajrccm.160.2.ats4-99 [DOI] [PubMed] [Google Scholar]
- 21. Stewart RJ, Tsang CA, Pratt RH, Price SF, Langer AJ. Tuberculosis—United States, 2017. MMWR Morb Mortal Wkly Rep. 2018;67(11):317-323. doi: 10.15585/mmwr.mm6711a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Courtwright A, Turner AN. Tuberculosis and stigmatization: pathways and interventions. Public Health Rep. 2010;125(suppl 4):34-42. doi: 10.1177/00333549101250S407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Royce RA, Colson PW, Woodsong C, et al. Tuberculosis knowledge, awareness, and stigma among African-Americans in three Southeastern counties in the USA: a qualitative study of community perspectives. J Racial Ethn Health Disparities. 2017;4(1):47-58. doi: 10.1007/s40615-015-0200-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Foster PH. Use of stigma, fear, and denial in development of a framework for prevention of HIV/AIDS in rural African American communities. Fam Community Health. 2007;30(4):318-327. doi: 10.1097/01.FCH.0000290544.48576.01 [DOI] [PubMed] [Google Scholar]