Abstract
Introduction:
Although marijuana use has increased since 2012, the perceived risk of adverse outcomes has decreased. This systematic review summarizes articles that examined the association between nonmedical marijuana use (ie, observed smoking, self-report, or urinalysis) and cardiovascular events in observational or experimental studies of adults aged ≥18.
Methods:
We searched Medline, EMBASE, PsycInfo, CINAHL, Cochrane Library Database, and Global Health from January 1, 1970, through August 31, 2018. Of 3916 citations, 16 articles fit the following criteria: (1) included adults aged ≥18; (2) included marijuana/cannabis use that is self-reported smoked, present in diagnostic coding, or indicated through a positive diagnostic test; (3) compared nonuse of cannabis; (4) examined events related to myocardial infarction, angina, acute coronary syndrome, and/or stroke; (5) published in English; and (6) had observational or experimental designs.
Results:
Of the 16 studies, 4 were cohort studies, 8 were case-control studies, 1 was a case-crossover study, 2 were randomized controlled trials, and 1 was a descriptive study. Studies ranged from 10 participants to 118 659 619 hospitalizations. Marijuana use was associated with an increased likelihood of myocardial infarction within 24 hours in 2 studies and stroke in 6 studies. Results of studies suggested an increased risk for angina and acute coronary syndrome, especially among people with a history of a cardiovascular event.
Conclusion:
This review suggests that people who use marijuana may be at increased risk for cardiovascular events. As states expand new laws permitting marijuana use, it will be important to monitor the effect of marijuana use on cardiovascular disease outcomes, perhaps through the inclusion of data on nonmedical marijuana use in diverse national and local surveillance systems.
Keywords: marijuana, cardiovascular events, chronic disease, epidemiology, noncommunicable diseases, substance abuse, heart disease, stroke
Cannabis, also referred to as marijuana, is among the most commonly used nonmedical psychoactive drugs in the United States.1,2 On average, about 8400 people try marijuana for the first time each day. 1 The prevalence of past-month marijuana use increased by 63% among people aged ≥12 from 2002 (6.2%) to 2018 (10.1%).1,3,4 Young adults aged 18-25 are the most frequent consumers of nonmedical marijuana; in 2014, approximately 19.6% of adults aged 18-25 and 8.6% of adults aged ≥26 reported past-month marijuana use.1,3 Although the federal government classifies marijuana as an illegal schedule I drug, at least 33 states and the District of Columbia have legalized marijuana for medical and/or recreational use.5,6 Despite favorable public sentiment for the legalization of marijuana, 7 questions remain about short- and long-term health effects. Marijuana, derived from the cannabis plant, can be ingested orally, vaporized, or smoked in cigarettes, cigars, or pipes. 8 Smoking marijuana is one of the most efficient ways to achieve the desired psychoactive effect.9,10 Perceptions of harm from marijuana use have declined steadily in the United States,1,2,11,12 yet the concentration of the main psychoactive ingredient tetrahydrocannabinol (THC) increased in confiscated samples from 3% in the 1980s to 12% in 2014. 13 This possible increase in potency raises concerns about the health effects of marijuana, particularly for nonmedical use, which may not have the quality control and accompanying supervision of a medically administered dose.
Few large-scale studies have examined the cardiovascular effects of marijuana, yet more than 121 million adults have cardiovascular disease (CVD). 14 When a person smokes and inhales marijuana, multiple mechanisms may affect cardiovascular health, similarly to tobacco smoking, including various histopathological and vascular changes.15 -17 In addition, as with cigarette smoking, marijuana smoking may cause atherosclerotic conditions from tar buildup, 18 although marijuana may cause harm in alternate routes of administration as well. 19 Smoking marijuana has also been associated with a dose-dependent increase in resting heart rate of 20%-100%—an effect lasting up to 3 hours.20 -24 We conducted a systematic review of observational and experimental studies, summarizing existing evidence on marijuana use (vs nonuse) as a potential risk factor for cardiovascular events—myocardial infarction, angina, acute coronary syndrome, and stroke—among adults.
Methods
Data Sources
We conducted a systematic review of the literature using the Preferred Reporting Items of Systematic reviews and Meta-Analyses statement. We accessed Medline, EMBASE, PsycInfo, CINAHL, Cochrane Library Database, and Global Health databases from January 1, 1970, through August 31, 2018, using various combinations of search terms, including “cannabis/or marijuana smoking,” “cannabinoids,” “cardiovascular disease or stroke,” ischemi,* tachycardia, infarction,* and “angina pectoris” (the full search strategy is available from the authors upon request).
Study Selection
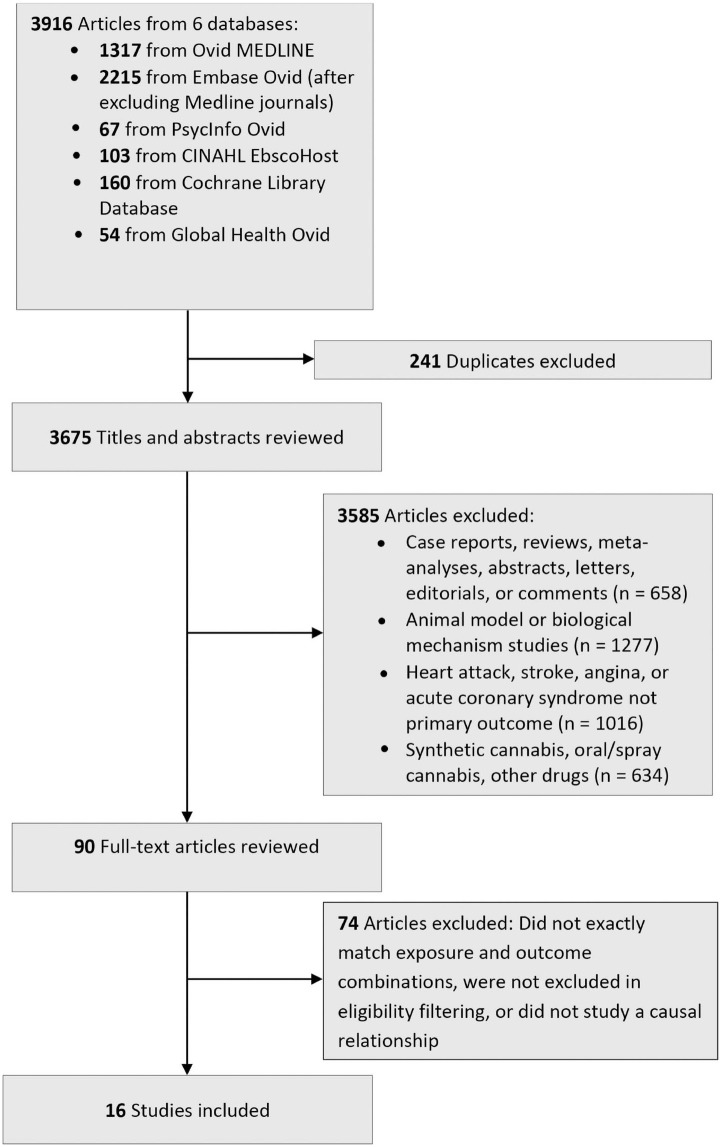
We considered an article eligible for review if it satisfied the following criteria: (1) population: adults aged ≥18; (2) intervention: marijuana/cannabis use that is self-reported smoked, present in diagnostic coding, or indicated through a positive diagnostic test; (3) comparison: nonuse of cannabis; and (4) outcome: events related to myocardial infarction, angina, acute coronary syndrome, and/or stroke. Studies eligible for final review also had to be published in English and have observational or experimental designs. We excluded studies with synthetic, medicinal, and/or clear nonsmoked marijuana use, although studies on clear nonsmoked marijuana use were not discernible in studies that used International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for marijuana abuse and dependence (ICD-9-CM codes 304.30-304.33, 305.20-305.23), and toxicology/urinalysis examinations. 25 We used Endnote version X8.2 (Clarivate Analytics) to collect and sort studies. After deleting duplicates, we excluded articles based on titles, abstract, and keywords that were irrelevant to the study’s exposure and outcome (Figure; full list of exclusion words available from authors upon request). Two authors (P.K.Y. and E.C.O.) reviewed the remaining articles for final inclusion. Two authors (P.K.Y. and E.C.O.) also examined the reference lists of included studies for articles of interest, although none were found.
Figure.
Flow diagram of included and excluded studies in a systematic review evaluating nonmedical marijuana use and cardiovascular events, January 1, 1970, through August 31, 2018.
Data Extraction
Four authors (P.K.Y., E.C.O., R.P., and S.C.K.) abstracted data from studies that met the inclusion criteria and developed a list of data elements for abstraction, including descriptive information about study sample size, type of marijuana exposure, whether a toxicology screen was conducted, and type of cardiovascular event. Two authors (P.K.Y. and E.C.O.) conducted an initial abstraction of the data elements and summarized the findings. Three authors (P.K.Y., E.C.O., and S.C.K.) conducted a secondary review of all data elements.
Three reviewers (P.K.Y., E.C.O., and F.L.) assessed the risk of bias for each study, adapting the US Preventive Services Task Force criteria, 26 assigning a grade for research design (I = randomized controlled trial; II-1 = well-designed controlled trial without randomization; II-2 = well-designed cohort or case-control study; II-3 = time series with or without intervention, uncontrolled experiments; III = descriptive study, case report) and internal validity (good, fair, or poor). “Good” studies metall study design criteria, “fair” studies did not meet all criteria but were not fatally flawed for internal validity, and “poor” studies were fatally flawed for internal validity. The US Preventive Services Task Force does not identify criteria for grading observational studies; however, 3 authors (P.K.Y., E.C.O., and F.L.) reported other types of bias. We did not conduct a meta-analysis because of the limited number of studies that met our inclusion criteria and the diversity of outcomes assessed. This study was deemed exempt from institutional review board review as a systematic review study.
Results
The database search yielded 3916 citations. After removing duplicate articles (n = 241) and articles that did not meet the inclusion criteria (n = 3659), 16 articles remained (Table). Of the 16 articles, 13 included samples from the United States. Sample sizes ranged from 10 participants to 118 659 619 hospitalizations. Thirteen studies included women, 4 were cohort studies, 8 were case-control studies, 1 was a case-crossover study, 2 were randomized controlled trials, and 1 was a descriptive study. In addition, the type of exposure to marijuana varied among the studies. In 2 studies,27,28 patients were directly observed smoking marijuana cigarettes, 3 studies included toxicology screens,29,30,34 5 studies obtained data on marijuana use through self-report,23,32,33,35,37 and 5 studies relied solely on ICD-9-CM diagnosis codes for cannabis dependence and abuse31,36,38 -41 to define marijuana use. Clinical outcomes differed across studies and included angina/acute coronary syndrome (n = 5), myocardial infarction (n = 4), and stroke (n = 10); 2 studies assessed multiple outcomes as a cardiovascular or cerebrovascular “event” or “disease.” Stroke included both hemorrhagic and ischemic strokes, in addition to delayed cerebral ischemia, aneurysmal subarachnoid hemorrhage, and transient ischemic attack.
Table.
Summary of included studies evaluating nonmedical marijuana use and cardiovascular events, January 1, 1970, through August 31, 2018
| Study author (year) | Study population/marijuana prevalence | % Female | How exposure assessed | Comparison | Outcome | Effect | Risk bias (design/internal validity) a |
|---|---|---|---|---|---|---|---|
| Aronow and Cassidy (1974) 27 | 10 patients with classic stable exertional angina pectoris and severe coronary artery disease, no history of marijuana use | 0 | Smoked marijuana | Control period to exercise induced angina without exposure to marijuana | Exercise-induced angina | Decreased time to angina by 48% (244.3 ± 16 s for control group vs 129.4 ± 13.6 s after smoking marijuana; P < .001). | I; good |
| Aronow and Cassidy (1975) 28 | 10 patients with classic stable exertional angina pectoris and severe coronary artery disease, no history of marijuana use | 0 | Smoked marijuana | Control period to exercise induced angina without exposure to marijuana | Exercise-induced angina | Decreased time to angina by 50% (243.4 ± 46.6 s for control group vs 124.1 ± 37.7 s after smoking marijuana; t = 24.77; P < .001). | I; fair |
| Barber et al (2013) 29 | Cases: 160 TIA and stroke patients with drug screen Controls: 160 matched patients admitted to internal medicine without cardiovascular issues with drug screens |
37.5 | Urine screen b | No detection of cannabis in urine screen | Ischemic stroke/TIA | Increased univariate odds of stroke/TIA (OR = 2.30; 95% CI, 1.08-5.08); effect not found after adjusting for tobacco use (aOR = 1.59; 95% CI, 0.71-3.70) | II-2; good |
| Behrouz et al (2016) 30 | 108 patients with aSAH; 28 with CB-positive drug screen, 80 with CB-negative drug screen | 53.6 | Urine screen | No detection of cannabis in urine screen | Delayed cerebral ischemia and poor outcome (composite of in-hospital death and modified Rankin score of 4 or 5) | Independent association between cannabis use and increased risk of delayed cerebral ischemia (aOR = 2.68; 95% CI, 1.03-6.99); increased risk of poor outcome (OR = 2.93; 95% CI, 1.07-8.01; P = .04) in univariate model but effect not found in multivariate model. | II-2; good |
| Desai et al (2017) 31 | 2 451 933 weighted hospitalized acute MI patients (35 771 with a history of marijuana use) | 34.0 | ICD-9-CM codes for abuse or dependence b | No ICD-9-CM code reported for abuse or dependence on marijuana | Acute MI | Marijuana use was a significant risk factor for acute MI development when adjusted for age, sex, and race (aOR = 1.079; 95% CI, 1.065-1.093); when adjusted for age, female sex, race, smoking, and cocaine abuse (aOR = 1.041; 95% CI, 1.027-1.054); and when adjusted for age, female sex, race, payer status, smoking, cocaine abuse, amphetamine abuse, and alcohol abuse (aOR = 1.031; 95% CI, 1.018-1.045). | II-2; fair |
| Falkstedt et al (2016) 32 | 49 321 Swedish men in military service (691 past heavy cannabis users) | 0 | Self-reported cannabis use upon military conscription b | Cannabis use in adolescence: never vs 1-10 times, 11-50 times, and >50 times | Ischemic and hemorrhagic strokes | No significant association between all stroke before age 45 and adolescent cannabis use. No significant association between all stroke until age 59 and adolescent cannabis use. Crude association between ischemic stroke before age 60 and adolescent cannabis use >50 times present in crude models (HR = 1.89; 95% CI, 1.09-3.27) adjusted for body mass index, migraine, and history of CVD (HR = 1.85; 95% CI, 1.07-3.22), and adjusted for childhood socioeconomic status and schooling (HR = 1.82; 95% CI, 1.05-3.17), but not significant after adjusting for smoking and alcohol. | II-2; fair |
| Hemachandra et al (2016) 33 | 7455 (1043 past-year cannabis users) | 51 | Self-reported past-year cannabis use and frequency b | No past-year cannabis use | Stroke, mini-stroke, TIA | Past-year cannabis users had increased risk of stroke/TIA compared with participants who had not smoked cannabis in the past year (aIRR = 2.3; 95% CI, 1.1-4.5) after adjusting for socioeconomic status, tobacco, health conditions, and exercise. Using cannabis at least weekly was associated with an increased risk for stroke/TIA (aIRR = 4.7; 95% CI, 2.1-10.7). | II-2; good |
| Jouanjus et al (2014) 34 | 1979 cannabis-related reports; 35 with cardiovascular complications | 14 (5 of 35) | Urine screen, in only 13 of 35 | Not available | 20 acute coronary syndrome; 2 heart rate disorders; 13 extracardiac complications | Increase in proportion of cardiovascular complications due to cannabis use (descriptive only; rose from 1.1% [5 of 468] in 2006 to 3.6% [11 of 309] in 2010). | III; internal validity rating not applicable |
| Lorenz et al (2017) 35 | 558 HIV-positive participants (seroconverters and chronically HIV-positive participants; 101 heavy marijuana users) | 0 | Self-reported marijuana use b | Heavy users (daily or weekly use) vs occasional use or nonuse | Cardiovascular events including MI, ischemic heart disease, angina, cerebrovascular disease, atherosclerosis, heart failure | Cardiovascular events occurred in 19.7% of heavy marijuana users compared with 8.7% of occasional users and nonusers (P = .01). Cardiovascular event rates were also increased among marijuana users who did not smoke cigarettes (P < .001). In logistic regression models adjusted for age, smoking, viral load, and 2 or 3 vs 0 or 1 traditional cardiovascular risk factors, time-updated heavy marijuana use was associated with increased odds of cardiovascular events (aOR = 2.5; 95% CI, 1.2-5.3). | II-2; fair |
| Mittleman et al (2001) 23 | 3882 (124 marijuana users) | 32 | Self-reported smoked marijuana use | Expected frequency in an average 1-h period, based on usual frequency of marijuana use in the year before MI | Heart attack/MI | Risk of MI elevated from baseline (OR = 4.8; 95% CI, 2.9-9.5) to 60 min after marijuana use. | II-2; fair |
| Moon et al (2018) 36 | 9 561 963 (26 416 cannabis users) | 58.0 | ICD-9-CM codes for abuse or dependence | No ICD-9-CM code reported for abuse or dependence on marijuana or ICD-9-CM code with “in remission” for substance use | Stroke among other irrelevant cardiovascular conditions | Marijuana use was associated with increased odds of stroke in orthopedic hip/knee patients (aOR = 2.62; 95% CI, 1.30-5.25) and spine surgery patients (aOR = 2.65; 95% CI, 1.82-3.87). Zero stroke events in the shoulder arthroplasty marijuana patients. | II-2; fair |
| Reis et al (2017) 37 | 5113 adults from the Coronary Artery Risk Development Study (84% with a history of marijuana use) | 54.5 | Self-report b | No self-reported marijuana use | Strokes, TIAs, CVD | Compared with no marijuana use, cumulative lifetime and recent marijuana use showed no association with stroke or TIAs. Marijuana use was not associated with CVD when stratified by age, gender, race, or family history of CVD. | II-2; good |
| Rumalla et al (2016) 38 | AIS: 478 649 (11 320 cannabis positive); non-AIS: 118 180 969 | AIS: 67.0; non-AIS: 44.3 | ICD-9-CM code for abuse or dependence b | AIS patients without ICD-9-CM code for marijuana use | AIS | AIS incidence was significantly higher for people who use marijuana than for nonusers (RR = 1.13; 95% CI, 1.11-1.15); adjusting for other risk factors, marijuana use increased the likelihood of AIS (aOR = 1.17; 95% CI, 1.15-1.20). | II-2; good |
| Rumalla et al (2016) 39 | aSAH: 94 052 (CB-positive: 2104; CB-negative: 91 948); non-aSAH: 118 565 567 | aSAH: 66.9; non-aSAH: 59.9 | ICD-9-CM code for abuse or dependence b | aSAH patients without ICD-9-CM code for cannabis use | aSAH | aSAH incidence was slightly higher for cannabis users than for nonusers (RR = 1.07; 95% CI, 1.02-1.11); adjusting for other risk factors, cannabis use increased the likelihood of aSAH (aOR = 1.18; 95% CI, 1.12-1.24). | II-2; good |
| Vin-Raviv et al (2017) 40 | 39 836 589 people, 105 957 strokes (387 608 marijuana users, 594 with strokes) | 58 | ICD-9-CM code for abuse or dependence | No ICD-9-CM code reported for abuse or dependence on marijuana | Stroke | Among hospitalized patients, marijuana use was associated with increased odds of stroke (OR = 1.60; 95% CI, 1.44-1.77) compared with nonusers. | II-2; good |
| Westover et al (2007) 41 | 2252 all categories of strokes (hemorrhagic: 937, 28 marijuana users; ischemic: 998, 25 marijuana users) | Not described | ICD-9-CM code for abuse or dependence b | No ICD-9-CM code reported for abuse or dependence on marijuana | Hemorrhagic and ischemic stroke | Among inpatient stroke admissions, cannabis use was associated with ischemic stroke (aOR = 1.76; 95% CI, 1.15-2.71) but not with hemorrhagic stroke (aOR = 1.36; 95% CI, 0.90-2.06). | II-2; good |
Abbreviations: aIRR, adjusted incidence rate ratio; AIS, acute ischemic stroke; aOR, adjusted odds ratio; aSAH, aneurysmal subarachnoid hemorrhage; CB, cannabinoid; CVD, cardiovascular disease; HR, hazard ratio; ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification; MI, myocardial infarction; OR, odds ratio; RR, relative risk; THC, tetrahydrocannabinol; TIA, transient ischemic attack.
Based on US Preventive Services Task Force criteria for research design (I = randomized controlled trial; II-1 = well-designed controlled trial without randomization; II-2 = well-designed cohort, cross-sectional, or case-control study; II-3 = time series with or without intervention, uncontrolled experiments; III = descriptive study, case report) and a separate grade for internal validity (good, fair, or poor). “Good” studies met all study design criteria, “fair” studies did not meet all criteria but were not fatally flawed for internal validity, and “poor” studies were fatally flawed for internal validity. 26
Adjusted for tobacco use in their analyses.
Three articles included only angina/acute coronary syndrome as an outcome. In both studies by Aronow and Cassidy,27,28 time to exercise-induced angina was decreased by nearly 50% after smoking a marijuana cigarette (compared with a control period of nonsmoking). During the 4-year period examined by Jouanjus et al, 34 the proportion of cardiovascular complications associated with cannabis use rose from 1.1% to 3.6%. Complications included 20 reports of patients with cannabis-related acute coronary syndrome, of which 10 required hospitalization and 6 underwent cardiac resuscitation attempts.
Two studies included myocardial infarction as an outcome. In a case-crossover sample of nearly 4000 patients hospitalized for acute myocardial infarction, Mittleman et al 23 showed that cannabis use was associated with a 4.8 (95% CI, 2.4-9.5) times increased risk of myocardial infarction in the first hour after smoking and a 1.7 (95% CI, 0.6-5.1) times increased risk of myocardial infarction in the second hour after smoking, based on an expected frequency used to estimate a univariate relative risk. Using the 2010-2014 National Inpatient Sample (NIS), Desai et al 31 found increased odds of myocardial infarction (adjusted odds ratio [aOR] = 1.03; 95% CI, 1.02-1.05) from nonmedical cannabis after adjusting for demographic characteristics and other substance use.
Nine studies included only stroke as an outcome. In a case-control study by Barber et al, 29 cannabis use was associated with an increased risk of ischemic stroke/transient ischemic attack in univariate analyses, although the authors did not find a significant independent association after adjusting for tobacco smoking. A study of 108 patients found that cannabis use increased the risk of delayed cerebral ischemia in patients with aneurysmal subarachnoid hemorrhage, a form of stroke (aOR = 2.68; 95% CI, 1.03-6.99). 34 In a population of 49 321 Swedish men born during 1949-1951, Falkstedt et al 32 found no clear association between cannabis use in young adulthood and stroke. Hemachandra et al 33 found a 2.3 times greater incidence of stroke with past-year cannabis use in a general Australian population (adjusted incidence rate ratio [aIRR] = 2.3; 95% CI, 1.1-4.5), although the effect was relevant only to weekly cannabis users (aIRR = 4.7; 95% CI, 2.1-10.7). In a large population from the NIS, Moon et al 36 found that marijuana use was associated with increased odds of stroke among hip/knee patients (aOR = 2.62; 95% CI, 1.30-5.25) and spinal fusion arthroplasty patients (aOR = 2.65; 95% CI, 1.82-3.87). Using NIS data from 2004-2011, Rumalla et al 38 found an increased likelihood for acute ischemic stroke (aOR = 1.17; 95% CI, 1.15-1.20) among hospitalized patients aged 15-54. In a follow-up study using the same population, Rumalla et al 39 also found cannabis use was an independent predictor of aneurysmal subarachnoid hemorrhage (aOR = 1.18; 95% CI, 1.12-1.24). Using a 2007-2011 NIS population, another study found a greater risk of stroke among hospitalized patients with ICD-9-CM codes for cannabis dependence as compared with those without such codes (aOR = 1.60; 95% CI, 1.44-1.77). 40 Finally, Westover et al 41 used a Texas-wide hospital database with data on 2252 strokes to show an association between cannabis use and ischemic stroke (aOR = 1.76; 95% CI, 1.15-2.71) but not hemorrhagic stroke (aOR = 1.36; 95% CI, 0.90-2.06).
Two articles assessed multiple outcomes as cardiovascular or cerebrovascular “events” or “diseases,” comprising some combination of the primary study outcomes. A study of a multicenter population of HIV-infected men found a strong association between long-term heavy marijuana use and cardiovascular events (aOR = 2.5; 95% CI, 1.3-5.1). 35 A comprehensive follow-up study of the Coronary Artery Risk Development in Young Adults study found no association between marijuana use and CVD incidence among adults aged 43-55. 37
All 16 studies included an assessment of at least 1 CVD risk factor as a covariate (eg, previous angina/myocardial infarction/stroke, hypertension, obesity, diabetes). Among patients who had already had a cardiovascular event, marijuana use decreased the time to angina and was associated with a significant increased risk of myocardial infarction or stroke.23,27,28,30 -33,36,38 -41 Other outcomes after a cardiovascular event included delayed cerebral ischemia, 30 stroke disability, 30 mortality,36,37 and multifocal intracranial stenosis. 30 Outcomes were assessed by the use of electrocardiogram, angiography, computed tomographic scan, magnetic resonance imaging, expert medical record review, magnetic resonance spectroscopy, diagnosis codes, discharge codes, and self-report. In 12 studies,29 -33,35 -41 control variables, including tobacco use, alcohol use, other substance use, and other chronic disease risk factors, were accounted for when reporting the association between marijuana use and the outcome variable. Both studies by Aronow and Cassidy27,28 implemented a control period, whereas other researchers implemented the case-control23,29 -31,36,39 -41 or case crossover 23 study design to reduce confounding.
Risks of Bias
Methods of assessing marijuana use varied across studies, possibly affecting the validity of findings. Because several studies confirmed marijuana use only through diagnostic examinations for THC detection and not the various routes of administration (ie, smoking, vaping, ingestion), the association of cardiovascular events with smoking combustible marijuana could not be assessed with confidence. However, none of the studies suggested a fatal flaw of internal validity; thus, most studies were rated as good or fair quality. First, in both studies by Aronow and Cassidy,27,28 “10 puffs of smoke” was assessed visually by a research assistant. Although the authors estimated this amount was about three-quarters of a marijuana cigarette that contained 18.9 mg of THC, and other vital signs were recorded (eg, heart rate, carboxyhemoglobin, hemoglobin), the consistency of “10 puffs” is uncertain. Moreover, in the 1975 study, 4 of 10 participants had participated in the 1974 study. Seven studies relied on self-reported marijuana use, which may affect the validity of the findings via response bias.23,32 -35,37,41 Patients may be less likely to report the use of an illegal substance or not accurately report consistent use because of social desirability bias. Two studies implemented toxicology screens for marijuana use in all cases and controls,29,30 which does not reflect the route of use (smoked vs nonsmoked) and may not accurately reflect the history of use because of THC’s transience in the body. Three studies used broader disease categories such as “CVD” and “cardiovascular events” as a primary outcome, which may capture more types of diseases or events than our primary outcomes.35 -37 Finally, given the strong association between marijuana use and tobacco use, failure to control for confounding or not assessing outcomes shortly after smoking marijuana could have been a source of bias in 3 studies.23,29,32
Discussion
Our review identified 16 studies that examined the association between marijuana use and cardiovascular events. Thirteen studies showed a significant relationship between marijuana use and cardiovascular events, which points to a potential temporal association between marijuana use and cardiovascular outcomes, including decreased time to angina, acute coronary syndrome, myocardial infarction within 24 hours, and onset of ischemic stroke. Likewise, in a systematic review of 34 case reports on 64 patients, Hackam 42 found that in about 80% of cases, a stroke or transient ischemic attack occurred within 24 hours of marijuana use. However, some studies suggest that the temporal risk associated with marijuana use may be short-lived. For example, 1 study showed that the relative risk for myocardial infarction in the second hour after use was no longer significant (aOR = 1.7; 95% CI, 0.6-5.1). 23 Another study found that partial or total reversal of cerebrovascular damage occurred in some patients after they refrained from marijuana use. 34 Another review found reason to believe that marijuana may be associated with CVD, 43 which, although distinct from the cardiovascular events our study focused on, is the underlying disease causing the outcome. More recently, Ravi et al 44 did not find sufficient evidence for an association between marijuana use and cardiovascular outcomes in their systematic review, although that review used 1 article on myocardial infarction and 4 articles on stroke. Our review included 4 articles on myocardial infarction and 10 articles on stroke. Also, little is known about how marijuana dose and strength (ie, potency or percentage of THC) affect the risk of cardiovascular events. In 2 studies, more regular use of marijuana (weekly or more) increased the risk or odds of cardiovascular events, including stroke/transient ischemic attack,33,35 whereas another study that measured occasional or nonchronic marijuana use showed decreased or no risk of a cardiovascular event. 37 Another study identified dose-dependent cardiovascular effects among daily marijuana users. 45 Finally, mode of marijuana use may be associated with various mechanisms linked to cardiovascular events, such as tar buildup from smoking15 -19 or possible lung injury from vaping THC in electronic cigarette pods. 46
As more states consider legalizing recreational or medicinal marijuana use and the drug becomes more readily available, the full scope of population-wide cardiovascular consequences, including death, has yet to be determined. Several studies that explored the association between marijuana use and death had mixed results. In a study of surveillance data, researchers found a 25.6% mortality rate for marijuana-related cardiovascular complications. 34 In a prospective cohort study of marijuana use and death after myocardial infarction, a death risk gradient was found among people who used marijuana more frequently (ie, any use, <weekly use, and weekly use compared with nonuse) when examined during a nearly 4-year follow-up period, 47 although the association between marijuana use and death among myocardial infarction survivors in an 18-year follow-up was not significant. Similarly, risk of circulatory disease death was not associated with current marijuana use relative to nonuse among men (aOR = 1.22; 95% CI, 0.80-1.87) and women (aOR = 0.96; 95% CI, 0.46-2.02) in a cohort of Kaiser Permanente enrollees followed during a 10-year period.48,49
Limitations
Our findings must be interpreted with caution because of several limitations. First, a causal association between marijuana use and myocardial infarction or stroke cannot be proven by currently available data.29,42 Inherent differences, such as behavioral risk factors that are independent of marijuana use, may be present between people who use marijuana and people who do not use marijuana. Moreover, standardized tools that assess exposure (eg, chemical potency) and route of administration (eg, vaping, ingesting, topical application) may be needed to determine differences between outcomes. Second, because studies included in our review used small convenience samples, were cross-sectional, or used a retrospective review of hospital or surveillance data, study findings may not be generalizable beyond these samples. Although randomized controlled trials or other experimental studies with more direct control of the exposures and outcomes may be ideal study designs to test the effects of use on cardiovascular events, intentional exposure of people to marijuana in the research setting may be deemed unethical. Thus, we included observational, cohort, and case-crossover studies and identified when confounders were controlled.
Third, although our review suggests an association between marijuana use and risk for cardiovascular events, the underlying biological mechanisms could not be determined from the current findings. Finally, although 9 studies in this review adjusted their analyses to account for tobacco use, this adjustment may not itself account for the duration and effects of tobacco use history on patient outcomes. Subsequently, some risk of an interactive effect between marijuana and tobacco use may be present that is not fully explained by these adjusted studies.
Conclusions
Findings from our review suggest that people who use nonmedical marijuana, as indicated by observation, self-report, or urinalysis, may be at acute risk for myocardial infarction and stroke, particularly people who have had previous cardiovascular events. Especially with the increase in the prevalence of marijuana use with the expansion of state marijuana laws, 50 marijuana use may have widespread implications for public health as individual and environmental exposure to marijuana increases. Heightened awareness of these potential associations among primary care providers, cardiologists, and emergency care providers may aid in the inclusion of marijuana use in standardized triage intake forms, including the systematic collection of data on recent nonmedical drug use in medical history, especially for patients presenting with cardiac-related problems. It will also be important for the public health community to monitor the effect of marijuana use on CVD risk factors and outcomes, perhaps through the inclusion of nonmedical marijuana use in diverse national and local surveillance systems, and the eventual inclusion of nonmedical drugs such as marijuana in electronic health record data systems. Finally, further research will be needed on estimating the association among frequency, THC concentration, and duration of exposure to marijuana and cardiovascular outcomes.
Acknowledgments
The authors appreciate the staff of the Stephen J. Thacker Library at the Centers for Disease Control and Prevention (CDC) for their support, especially librarian Joanna Taliano for conducting the electronic search for this article.
Footnotes
Disclaimer: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Oak Ridge Institute for Science and Education (ORISE) or the Centers for Disease Control and Prevention (CDC).
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported in part by an appointment to the Research Participation Program at CDC administered by ORISE through an interagency agreement between the US Department of Energy and CDC. The authors report no other financial disclosures. No study sponsor had any role in the study design, data collection, analysis, or interpretation of data; the writing of the article; or the decision to submit the article for publication.
ORCID iD: Peter K. Yang, MPH  https://orcid.org/0000-0001-9379-6981
https://orcid.org/0000-0001-9379-6981
References
- 1. Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results From the 2018 National Survey on Drug Use and Health. Substance Abuse and Mental Health Services Administration; 2019. NSDUH Series H-54, HHS Publication No. PEP19 5068. [Google Scholar]
- 2. Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME. Monitoring the Future National Survey Results on Drug Use, 1975-2018: Overview, Key Findings on Adolescent Drug Use. University of Michigan; 2017. [Google Scholar]
- 3. Azofeifa A, Mattson ME, Schauer G, McAfee T, Grant A, Lyerla R. National estimates of marijuana use and related indicators—National Survey on Drug Use and Health, United States, 2002-2014. MMWR Surveill Summ. 2016;65(11):1-28. doi: 10.15585/mmwr.ss6511a1 [DOI] [PubMed] [Google Scholar]
- 4. Hasin DS, Saha TD, Kerridge BT, et al. Prevalence of marijuana use disorders in the United States between 2001-2002 and 2012-2013. JAMA Psychiatry. 2015;72(12):1235-1242. doi: 10.1001/jamapsychiatry.2015.1858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. US Drug Enforcement Administration. Drug scheduling. Accessed September 21, 2015. http://www.justice.gov/dea/druginfo/ds.shtml [PubMed]
- 6. National Conference of State Legislatures. State medical marijuana laws. 2018. Accessed November 12, 2018. http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx
- 7. Salas-Wright CP, Vaughn MG, Todic J, Córdova D, Perron BE. Trends in the disapproval and use of marijuana among adolescents and young adults in the United States: 2002-2013. Am J Drug Alcohol Abuse. 2015;41(5):392-404. doi: 10.3109/00952990.2015.1049493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gloss D. An overview of products and bias in research. Neurotherapeutics. 2015;12(4):731-734. doi: 10.1007/s13311-015-0370-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hall W, Degenhardt L. Adverse health effects of non-medical cannabis use. Lancet. 2009;374(9698):1383-1391. doi: 10.1016/S0140-6736(09)61037-0 [DOI] [PubMed] [Google Scholar]
- 10. Pacula RL, Jacobson M, Maksabedian EJ. In the weeds: a baseline view of cannabis use among legalizing states and their neighbours. Addiction. 2016;111(6):973-980. doi: 10.1111/add.13282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Volkow ND, Baler RD, Compton WM, Weiss SRB. Adverse health effects of marijuana use. N Engl J Med. 2014;370(23):2219-2227. doi: 10.1056/NEJMra1402309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pacek LR, Mauro PM, Martins SS. Perceived risk of regular cannabis use in the United States from 2002 to 2012: differences by sex, age, and race/ethnicity. Drug Alcohol Depend. 2015;149:232-244. doi: 10.1016/j.drugalcdep.2015.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. ElSohly MA. Quarterly Report: Potency Monitoring Project Report 104—December 16, 2008, Through March 15, 2009. University of Mississippi, National Center for Natural Products Research; 2009. [Google Scholar]
- 14. Benjamin EJ, Muntner P, Alonso A, et al. Heart disease and stroke statistics—2019 update: a report from the American Heart Association. Circulation. 2019;139(10):e56-e528. doi: 10.1161/CIR.0000000000000659 [DOI] [PubMed] [Google Scholar]
- 15. Gong H, Jr, Fligiel S, Tashkin DP, Barbers RG. Tracheobronchial changes in habitual, heavy smokers of marijuana with and without tobacco. Am Rev Respir Dis. 1987;136(1):142-149. doi: 10.1164/ajrccm/136.1.142 [DOI] [PubMed] [Google Scholar]
- 16. Tomar RS, Beaumont J, Hsieh JCY. Evidence on the Carcinogenicity of Marijuana Smoke. California Environmental Protection Agency, Office of Environmental Health Hazard Assessment, Reproductive and Cancer Hazard Assessment Branch; 2009. [Google Scholar]
- 17. Goyal H, Awad HH, Ghali JK. Role of cannabis in cardiovascular disorders. J Thorac Dis. 2017;9(7):2079-2092. doi: 10.21037/jtd.2017.06.104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Moir D, Rickert WS, Levasseur G, et al. A comparison of mainstream and sidestream marijuana and tobacco cigarette smoke produced under two machine smoking conditions. Chem Res Toxicol. 2008;21(2):494-502. doi: 10.1021/tx700275p [DOI] [PubMed] [Google Scholar]
- 19. Jones RT. Cardiovascular system effects of marijuana. J Clin Pharmacol. 2002;42(Suppl 1):58S-63S. doi: 10.1002/j.1552-4604.2002.tb06004.x [DOI] [PubMed] [Google Scholar]
- 20. Hollister LE. Health aspects of cannabis. Pharmacol Rev. 1986;38(1):1-20. [PubMed] [Google Scholar]
- 21. National Institute on Drug Abuse. Drug facts—marijuana drugfacts. Accessed September 21, 2015. http://www.drugabuse.gov/publications/drugfacts/marijuana
- 22. Beaconsfield P, Ginsburg J, Rainsbury R. Marihuana smoking: cardiovascular effects in man and possible mechanisms. N Engl J Med. 1972;287(5):209-212. doi: 10.1056/NEJM197208032870501 [DOI] [PubMed] [Google Scholar]
- 23. Mittleman MA, Lewis RA, Maclure M, Sherwood JB, Muller JE. Triggering myocardial infarction by marijuana. Circulation. 2001;103(23):2805-2809. doi: 10.1161/01.CIR.103.23.2805 [DOI] [PubMed] [Google Scholar]
- 24. Wu TC, Tashkin DP, Djahed B, Rose JE. Pulmonary hazards of smoking marijuana as compared with tobacco. N Engl J Med. 1988;318(6):347-351. doi: 10.1056/NEJM198802113180603 [DOI] [PubMed] [Google Scholar]
- 25. Centers for Disease Control and Prevention. International Classification of Diseases, 9th Revision, Clinical Modification. Accessed December 6, 2020. https://www.cdc.gov/nchs/icd/icd9cm.htm
- 26. Harris RP, Helfand M, Woolf SH, et al. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20(3 suppl):21-35. doi: 10.1016/s0749-3797(01)00261-6 [DOI] [PubMed] [Google Scholar]
- 27. Aronow WS, Cassidy J. Effect of marihuana and placebo-marihuana smoking on angina pectoris. N Engl J Med. 1974;291(2):65-67. doi: 10.1056/NEJM197407112910203 [DOI] [PubMed] [Google Scholar]
- 28. Aronow WS, Cassidy J. Effect of smoking marihuana and of a high-nicotine cigarette on angina pectoris. Clin Pharmacol Ther. 1975;17(5):549-554. doi: 10.1002/cpt1975175549 [DOI] [PubMed] [Google Scholar]
- 29. Barber PA, Pridmore HM, Krishnamurthy V, et al. Cannabis, ischemic stroke, and transient ischemic attack: a case-control study. Stroke. 2013;44(8):2327-2329. doi: 10.1161/STROKEAHA.113.001562 [DOI] [PubMed] [Google Scholar]
- 30. Behrouz R, Birnbaum L, Grandhi R, et al. Cannabis use and outcomes in patients with aneurysmal subarachnoid hemorrhage. Stroke. 2016;47(5):1371-1373. doi: 10.1161/STROKEAHA.116.013099 [DOI] [PubMed] [Google Scholar]
- 31. Desai R, Patel U, Sharma S, et al. Recreational marijuana use and acute myocardial infarction: insights from Nationwide Inpatient Sample in the United States. Cureus. 2017;9(11):e1816. doi: 10.7759/cureus.1816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Falkstedt D, Wolff V, Allebeck P, Hemmingsson T, Danielsson A-K. Cannabis, tobacco, alcohol use, and the risk of early stroke: a population-based cohort study of 45 000 Swedish men. Stroke. 2017;48(2):265-270. doi: 10.1161/STROKEAHA.116.015565 [DOI] [PubMed] [Google Scholar]
- 33. Hemachandra D, McKetin R, Cherbuin N, Anstey KJ. Heavy cannabis users at elevated risk of stroke: evidence from a general population survey. Aust N Z J Public Health. 2016;40(3):226-230. doi: 10.1111/1753-6405.12477 [DOI] [PubMed] [Google Scholar]
- 34. Jouanjus E, Lapeyre-Mestre M, Micallef J. French Association of the Regional Abuse and Dependence Monitoring Centres (CEIP-A) Working Group on Cannabis Complications. Cannabis use: signal of increasing risk of serious cardiovascular disorders. J Am Heart Assoc. 2014;3(2):e000638. doi: 10.1161/JAHA.113.000638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lorenz DR, Dutta A, Mukerji SS, Holman A, Uno H, Gabuzda D. Marijuana use impacts midlife cardiovascular events in HIV-infected men. Clin Infect Dis. 2017;65(4):626-635. doi: 10.1093/cid/cix391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Moon AS, Smith W, Mullen S, et al. Marijuana use and mortality following orthopedic surgical procedures. Subst Abus. 2019;40(3):378-382. doi: 10.1080/08897077.2018.1449054 [DOI] [PubMed] [Google Scholar]
- 37. Reis JP, Auer R, Bancks MP, et al. Cumulative lifetime marijuana use and incident cardiovascular disease in middle age: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Am J Public Health. 2017;107(4):601-606. doi: 10.2105/AJPH.2017.303654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Rumalla K, Reddy AY, Mittal MK. Recreational marijuana use and acute ischemic stroke: a population-based analysis of hospitalized patients in the United States. J Neurol Sci. 2016;364:191-196. doi: 10.1016/j.jns.2016.01.066 [DOI] [PubMed] [Google Scholar]
- 39. Rumalla K, Reddy AY, Mittal MK. Association of recreational marijuana use with aneurysmal subarachnoid hemorrhage. J Stroke Cerebrovasc Dis. 2016;25(2):452-460. doi: 10.1016/j.jstrokecerebrovasdis.2015.10.019 [DOI] [PubMed] [Google Scholar]
- 40. Vin-Raviv N, Akinyemiju T, Meng Q, Sakhuja S, Hayward R. Marijuana use and inpatient outcomes among hospitalized patients: analysis of the Nationwide Inpatient Sample database. Cancer Med. 2017;6(1):320-329. doi: 10.1002/cam4.968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Westover AN, McBride S, Haley RW. Stroke in young adults who abuse amphetamines or cocaine: a population-based study of hospitalized patients. Arch Gen Psychiatry. 2007;64(4):495-502. doi: 10.1001/archpsyc.64.4.495 [DOI] [PubMed] [Google Scholar]
- 42. Hackam DG. Cannabis and stroke: systematic appraisal of case reports. Stroke. 2015;46(3):852-856. doi: 10.1161/STROKEAHA.115.008680 [DOI] [PubMed] [Google Scholar]
- 43. Franz CA, Frishman WH. Marijuana use and cardiovascular disease. Cardiol Rev. 2016;24(4):158-162. doi: 10.1097/CRD.0000000000000103 [DOI] [PubMed] [Google Scholar]
- 44. Ravi D, Ghasemiesfe M, Korenstein D, Cascino T, Keyhani S. Associations between marijuana use and cardiovascular risk factors and outcomes: a systematic review. Ann Intern Med. 2018;168(3):187-194. doi: 10.7326/M17-1548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ramesh D, Haney M, Cooper ZD. Marijuana’s dose-dependent effects in daily marijuana smokers. Exp Clin Psychopharmacol. 2013;21(4):287-293. doi: 10.1037/a0033661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Perrine CG, Pickens CM, Boehmer TK, et al. Characteristics of a multistate outbreak of lung injury associated with e-cigarette use, or vaping—United States, 2019. MMWR Morb Mortal Wkly Rep. 2019;68(39):860-864. doi: 10.15585/mmwr.mm6839e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mukamal KJ, Maclure M, Muller JE, Mittleman MA. An exploratory prospective study of marijuana use and mortality following acute myocardial infarction. Am Heart J. 2008;155(3):465-470. doi: 10.1016/j.ahj.2007.10.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Sidney S. Cardiovascular consequences of marijuana use. J Clin Pharmacol. 2002;42(S1):64S-70S. doi: 10.1002/j.1552-4604.2002.tb06005.x [DOI] [PubMed] [Google Scholar]
- 49. Sidney S, Beck JE, Tekawa IS, Quesenberry CP, Friedman GD. Marijuana use and mortality. Am J Public Health. 1997;87(4):585-590. doi: 10.2105/AJPH.87.4.585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Cerdá M, Wall M, Feng T, et al. Association of state recreational marijuana laws with adolescent marijuana use. JAMA Pediatr. 2017;171(2):142-149. doi:10.1001/jamapedi atrics.2016.3624 [DOI] [PMC free article] [PubMed] [Google Scholar]