Abstract
Background: Congenital insensitivity to pain is a rare autosomal recessive condition characterized by insensitivity to painful stimuli due to absence of sensory and sympathetic post ganglionic neurons in the skin and skeletal system leading to lack of protective sensation and altered joint propioception. This study was performed to assess hand and wrist manifestations of patients with congenital insensitivity to pain in the Maltese Islands. Methods: Records of public and private hospitals were reviewed to identify patients suffering from this condition. A review of notes, patients, and imaging was performed. A Disabilities of the Arm, Shoulder, and Hand score was obtained to assess level of function. Results: Nine patients were identified. Mean age of diagnosis was 8.9 years. Interphalangeal joints were most commonly affected. Multiple spontaneous or posttraumatic fingertip ulceration occurred in 5 patients. Anhidrosis resulted in more protracted ulcers and infections, requiring amputation of distal and middle phalanges due to osteomyelitis. The wrist joint was less commonly involved and showed more complex joint involvement. Conclusion: The hand and wrist are involved in different ways, with fingertip ulceration leading to potential infection and osteomyelitis in the hand, whereas the wrist joint is involved in cases of increased axial loading and load transfer, such as following prolonged use of walking and mobility aids. The latter should be borne in mind during management of lower limb conditions. Hand care and hygiene is important in all patients, especially in cases of anhidrosis due to the increased rate of ulceration and osteomyelitis requiring surgical intervention. Despite the severity of the condition, patients report good overall function.
Keywords: insensitivity to pain, congenital, hereditary sensory and autonomic neuropathy, neuropathic joint, anhidrosis
Introduction
Congenital insensitivity to pain is a rare autosomal recessive sensory autonomic neuropathy characterized by absence to nociceptive stimuli due to a mutation in the SCN9A, SCN11A, or PRDM12 gene responsible for voltage-gated sodium channel function, or a defect in the neurotrophic tyrosine kinase-1 receptor (NTK-1 or NGF) leading to damage or absence of sensory and sympathetic postganglionic neurons in the skin and skeletal system. This leads to lack of protective sensation and altered joint proprioception in the limbs with intact tendon reflexes and relative preservation of vibration sense.
Afferent sensory nerves fail to develop in dorsal root ganglia resulting in inability to feel. Nerve growth factor function and neuropeptide levels are decreased leading to fibroblast rather than osteoblast differentiation and proliferation from pluripotent stromal mesenchymal cells. These changes affect bone metabolism predisposing patients to fractures and delayed bone consolidation.1-3
Various inherited and spontaneous mutations in the SCN9A gene have been identified, and there is variable gene penetrance. This accounts for variations in this condition, with some retained sensation proximally and centrally, and variations in the intensity of dysaesthesia which is symmetrical but may vary between upper and lower limbs.4-7
Anhidrosis is a recognized association and, in combination with congenital insensitivity to pain, is known as hereditary sensory and autonomic neuropathy type IV (HSAN IV). This occurs due to defects in the NTK-1 receptor causing absence of autonomic sympathetic innervation of sweat glands resulting in inability to sweat and inadequate thermoregulation with the risk of developing hyperthermia and hyperpyrexia.
Materials and Methods
The aim of this study was to assess hand and wrist manifestations and function in patients with congenital insensitivity to pain in a population. Patients suffering from this condition in the Maltese Islands were identified from hospital and clinic attendance. These islands have a single health center system with a stable and relatively closed population, allowing identification of the entire cohort of patients diagnosed with this condition in the population. Patients, together with their medical records and imaging were reviewed from birth to date with appropriate consent. The EQ-5D-5L questionnaire was used to assess function, ability to perform daily activities and quality of life.
Results
Nine patients, 5 females and 4 males, were identified. Diagnosis was made by means of clinical and laboratory investigations performed by either a neurologist or a pediatrician depending on patient age at presentation. A sural nerve biopsy was performed in older patients, and genetic studies, which have only been available recently, were performed in the 2 younger patients. Quantitative sweat tests and intradermal histamine tests were performed on all patients to test for anhidrosis. Mean age at diagnosis was 8.9 years (range: 5-16 years).
All patients were Caucasian of native descent. Parents were not affected by the condition and did not have consanguineous marriages. There was no known prior family history of this condition in each case. Seven patients were related: 3 siblings, 2 siblings, and 2 distant cousins. Only 2 were isolated cases. The mean age at the time of the study was 33.7 years (range: 15-58 years).
Growth and mental development was normal, with documented delayed milestones in childhood in 2 cases. In both cases, the delayed milestones affected walking not upper limb function. Symmetrical peripheral anesthesia was present in all limbs in all cases. This varied in intensity proximally with some preservation of central sensation. All patients had normal tendon reflexes, absent corneal reflexes, and some preservation of vibration sense. Manifestations, such as physeal stress fractures leading to subperiosteal haematomas, were not identified in this cohort.
Individuals of working age were gainfully employed except 1, due to family support and personal choice. Lower limb involvement will be briefly mentioned in view of its influence on upper limb manifestations and quality of life. All patients had lower limb manifestations requiring surgical debridement or joint fusion at some stage. Patients remained mobile and independent mobilizing with walking aids if necessary, for stability due to the structural deformities or following surgical intervention. The most common lower limb manifestation was painless infected toe ulcers in 8 cases. Knee involvement occurred in 5 cases. Three of the latter cases required an arthrodesis to improve knee stability and patient mobilization. In view of the high risk of infection in these patients, septic arthritis and osteomyelitis can occur especially in patients who have metalwork inserted for arthrodesis or following trauma. This requires further surgery and long-term antibiotic treatment. In fact, 5 below knee amputations were performed in 4 patients due to osteomyelitis; 3 of which were performed following failed ankle fusions. Amputation stumps healed due to the better quality of soft tissue proximally.
Five patients had spontaneous and traumatic fingertip ulcerations on multiple fingers which were treated initially in the community with dressing changes and antibiotics before having debridements in theater. One of these 5 cases required an amputation of the distal phalanx of the thumb, and 2 of the 5 cases had the anhidrosis variant of this condition with ulceration which was recalcitrant to treatment and development of osteomyelitis requiring phalangeal amputation of multiple fingers. These patients required more prolonged treatment in view of recurrent infections: 1 patient ultimately requiring amputation of phalanges in all fingers and the other patient required sequential more proximal phalangeal amputations and longer courses of antibiotics in order to treat infection and prevent development of further infection until the soft tissues healed (Figure 1). Four patients, 3 females and 1 male, did not develop finger manifestations. Each one of these patients was particularly meticulous about hand hygiene and soft tissue care.
Figure 1.
Radiographs showing hand involvement in cases of anhidrosis with phalangeal amputations in all fingers.
Tissue samples were taken for culture and sensitivity in patients who underwent surgical intervention. A variety of organisms were cultured besides the presence of commensals. The majority, 76%, were strains of Staphylococci and Streptococci, including methicillin-resistant Staphylococcus aureus; Pseudomonas was the next most common organism cultured in 21% of cases. Most of these microbes were resistant to multiple antibiotics.
There was 1 case of flexor tendon sheath infection secondary to delayed presentation of a traumatic wound. This required a number of washout and debridement procedures and resulted in finger stiffness which affected hand function as it involved a central digit.
Soft tissue and carpal changes are not consistent with neuropathic arthropathy as clinic, radiographic changes and intraoperative findings are more destructive and inflammatory in nature with marked bone resorption and bone loss. The disease commences with loss of the proximal carpal row, carpal dislocation, disruption of the distal radioulnar joint and progresses to severe bone loss (Figures 2 and 3). Episodes of acute or chronic inflammatory swelling occur and may be confused with septic arthritis. Inflammatory markers are mildly raised and white cell count is normal. Biopsies are microbiologically negative. Intraoperatively, there are signs of acute and chronic inflammatory changes with marked synovial thickening and florid synovitis. Histology or synovial biopsies show chronically inflamed papillary synovial hyperplasia, and histology of soft tissue and tenosynovium shows fibrosis and chronic inflammatory changes.
Figure 2.

Proximal carpal row destruction and carpal dislocation.
Figure 3.

Severe carpal destruction in a case of wrist involvement.
These wrist changes were seen bilaterally in 1 case. Another case had only mild wrist changes that did not progress. Both patients developed clinical signs and radiographic changes following prolonged periods of using crutches and manual wheelchairs following lower limb treatment. Bilateral severe wrist involvement in 1 patient occurred after prolonged use of crutches and wheelchair due to a sequential hindfoot fusion and contralateral knee arthrodesis, both of which required revision due to failure of fusion, and ultimately bilateral below knee amputations. However, 3 other patients who had unilateral lower limb amputations did not develop wrist involvement. All of these 3 patients resumed independent mobilization with the use of prosthetics unlike the former case of bilateral wrist involvement who continued transferring and mobilizing with a wheelchair following bilateral lower limb amputations.
One patient developed an undisplaced insufficiency fracture of the shaft of the ulna with delayed union, which was treated nonoperatively (Figure 4). This fracture occurred when the patient was mobilizing with a wheelchair following a below knee amputation following a failed hindfoot fusion. There was 1 case of avascular necrosis of the humeral head, which was treated nonoperatively and required no further intervention following rehabilitation.
Figure 4.

Healed fracture of the ulnar shaft.
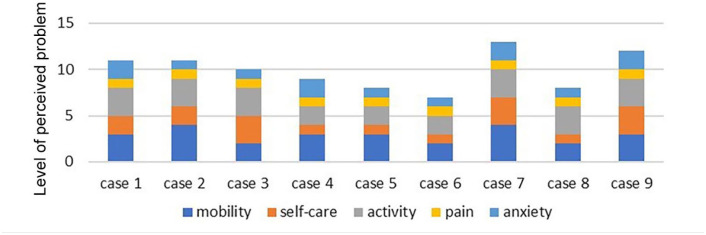
Table 1 shows the site and type of upper and lower limb involvement requiring review and treatment. The most significant lower limb intervention is reported in the table omitting other previous procedures on the limb. Patient recorded outcome measures varied significantly. EQ-5D-5 L reports on the state of mobility, self-care, activity, pain, and anxiety of individuals to evaluate quality of life, besides a visual analog scale (VAS) about patient perception of their general state. The results for each case are shown in a stacked chart (Figure 5). On assessing the individual scores, variations occurred in mobility, self-care, and activity. Worse scores were reported in cases of significant bilateral hand and wrist involvement, and in the case of stiffness of a central digit secondary to a flexor tendon sheath infection. The mean VAS score was 72 (range: 60-80). There was no correlation between quality of life, VAS, and age for this cohort (Figure 6).
Table 1.
Site and Type of Upper and Lower Limb Involvement.
| Case | Age | Gender | Anhidrosis | Upper limb involvement | Lower limb involvement |
|---|---|---|---|---|---|
| 1 | 39 | M | No | Thumb phalangeal amputation | Unilateral below knee amputation Contralateral knee fusion and foot ulcerations |
| 2 | 25 | M | No | None | Unilateral knee and hindfoot fusions Bilateral foot ulcerations |
| 3 | 37 | M | Yes | Phalangeal amputation all fingers Avascular necrosis humeral head |
Unilateral forefoot amputation Bilateral femoral fractures |
| 4 | 43 | F | No | None | Bilateral foot and ankle ulceration Unilateral ankle washout |
| 5 | 58 | F | No | Fingertip ulceration | Bilateral foot ulceration Unilateral subtalar fusion |
| 6 | 18 | F | No | Multiple fingertip ulceration Mild wrist involvement |
Unilateral talar dome osteochondral defect and subtalar fusion |
| 7 | 34 | F | No | Severe bilateral wrist involvement | Bilateral below knee amputation |
| 8 | 34 | F | No | Ulnar shaft fracture | Unilateral below knee amputation Contralateral pantalar fusion, big toe amputation and foot ulceration |
| 9 | 15 | M | Yes | Multiple fingertip ulcerations Flexor tendon sheath infection Multiple phalangeal amputations, including thumb |
Unilateral below knee amputation Contralateral big toe amputation, knee washout and foot ulceration |
Figure 5.
Stacked chart showing EQ-5D-5L for each case.
Figure 6.
Variation of EQ-5D-5L visual analogue score with age.
Discussion
Congenital insensitivity to pain is the term given to a complex systemic condition principally identified by insensitivity to pain. The pathology of this condition is more complex than one would expect solely due to the absence of pain, as would be expected in cases of neuropathic limbs and Charcot joints. This condition has a systemic insidious effect on the skin, skeletal system, and other systems due to absence of the trophic role of nociceptive response as well as other as yet unidentified mechanisms.2,8-11 It can be associated with other features, such as delayed wound and bone healing, stress fractures, joint dislocations, avascular necrosis, anhidrosis, hyperactivity, emotional liability, and intellectual impairment.12,13 Recently, a number of mutations (CLTCL1, SCN11A, NGF, and PRDM12) have been described besides those affecting the SCN9A gene and the NTK-1 receptor, which could account for the associated features mentioned above and for variations in expression of this condition.14-17
Lower limb manifestations are the most common feature, with varying degrees of foot and ankle involvement in all cases due to anesthesia, which leads to atraumatic and traumatic injuries and subsequent chronic ulcers, and to toe amputations in certain cases. These can occur despite meticulous care. The chronicity of these lesions makes osteomyelitis common. This can easily lead to sepsis if undiagnosed or neglected.18,19
Hand and wrist involvement is less common. In the hand, fingertip ulcerations are the most common problem, occurring in 5 of the 9 cases (3 males and 2 females). This was secondary to unidentified accidental injury in certain cases. There was no predilection for specific digits or hands. Despite primary nonoperative care, all patients required debridement procedures to 1 or more fingers in a theater setting for the treatment of infection at some stage. Hand involvement occurred in all the cases of anhidrosis. Patients with the anhidrosis variant (HSAN IV) had more severe ulceration, involvement of multiple digits, and recalcitrant infections ultimately requiring phalangeal amputations in a number of digits, including the thumb of the dominant hand in each case. The cohort is small, and the mechanism by which anhidrosis leads to increased ulceration and amputation in this condition is not fully understood. This series suggests that patients with HSAN IV should undergo early surveillance, patient education, and regular inspection of extremities with advice to seek prompt treatment if they sustain injuries or develop finger ulcerations.20,21
Surveillance and care, including the use of emollients in cases of anhidrosis, is important. Initial treatment should include ulcer debridement in the community or operating room in preference to the empiric use of antibiotics, especially in younger patients in order to delay and decrease the rate of antibiotic resistance and amputation, as patients are prone to developing multiple drug resistance due to chronic ulcers, recurrent infections, and osteomyelitis.
Carpal involvement is uncommon and in this series was associated with prolonged loading of these joints when using crutches and for independent transfer while using a manual wheelchair. This should be borne in mind during treatment of lower limb conditions, especially as these patients have delayed bone healing, therefore knee and ankle arthrodesis have a more protracted course and a higher risk of loosening, metal failure, infection, and multiple operations. A multidisciplinary approach should be used to ensure the best possible care allowing early management and preventing complications. 22 If surgical intervention is necessary, this should be planned and timed appropriately so as to decrease the risk of complications and ensure prompt rehabilitation. Therefore, clinical and radiological wrist assessment should be performed if prolonged use of the upper limbs for axial loading is envisaged for the treatment of lower limb symptoms; primary measures of joint immobilization should be undertaken if there are early signs of wrist joint involvement.
Wrist manifestations are rare, and arthrodesis can be considered. However, bone healing is delayed or poor in this complex condition, and bone resorption leads to nonunion and failure of fixation, and there is an increased risk of infection leading to failure of fusion and requiring revision procedures.
The functional score used in this study to report quality of life shows that despite lower limb involvement in all cases and upper limb involvement in most cases, the outcome and quality-of-life scores are better than expected. This could be due to the early age of presentation, allowing patients to adapt, modify their activities to improve and maintain function, develop an awareness of the condition, and seek advice when appropriate, therefore retaining reasonable overall function. Other factors which promote adaption are the gradual progression of anatomical changes and slow development of neuropathic joints. This allows patients to develop coping skills due to their young age and the painless nature of the condition, allowing them to continue to be independent. The VAS score shows that these patients report reasonable quality of life possibly due to an awareness of their condition and its potential complications. Cases of unilateral lower limb amputations report better quality-of-life scores, suggesting that this procedure is a reliable treatment option in these patients partly due to the shorted rehabilitation period. The quality-of-life assessment also shows that carpal destruction, central digit stiffness secondary to tendon sheath infection, and multiple phalangeal amputations affect upper limb function more significantly as it affects the various types of grip and causes weakness. Therefore, patients can compensate for mild hand manifestations but struggle with certain combinations of hand and wrist involvement.
Conclusion
Congenital insensitivity to pain is a complex condition and involves much more than insensitivity to pain. The systemic effects create unusual patterns of joint destruction, soft tissue manifestations, and diminished bone and soft tissue healing, with increased susceptibility to infection. Upper limb manifestations are less common than lower limb manifestations in this condition. The hand and wrist are involved in different ways, with fingertip ulceration leading to infection and osteomyelitis in the hand, whereas the wrist joint is involved in cases of increased axial loading and load transfer, with bone loss, dislocation, and the risk of infection. Hand care and hygiene is important in all patients, especially in cases of the anhidrosis variant of this condition. Early intervention in cases of digital ulceration by debridement and soft tissue cover may prevent amputation. Joint fusion requires greater mechanical bone and structural stability, bone contact, vascularity, and longer duration of protection than normal joints.
Acknowledgments
Orthopaedic Department, Mater Dei Hospital, Malta.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: Human rights were respected and there is no identifiable information. This article does not involve animal subjects.
Statement of Informed Consent: Informed consent was obtained prior to review of all patients included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Michelle Spiteri  https://orcid.org/0000-0002-5782-0507
https://orcid.org/0000-0002-5782-0507
References
- 1. Derwin KA, Glover RA, Wojtys EM. Nociceptive role of substance-P in the knee joint of a patient with congenital insensitivity to pain. J Pediatr Orthop. 1994;14(2):258-262. [DOI] [PubMed] [Google Scholar]
- 2. Hill EL, Elde R. Distribution of CGRP-, VIP-, DβH-, SP-, and NPY-immunoreactive nerves in the periosteum of the rat. Cell Tiss Res. 1991;264(3):469-480. [DOI] [PubMed] [Google Scholar]
- 3. Melamed I, Levy J, Parvari R, et al. A novel lymphocyte signalling defect: trk A mutation in the syndrome of congenital insensitivity to pain and anhidrosis (CIPA). J Clin Immunol. 2004;24(4):441-448. [DOI] [PubMed] [Google Scholar]
- 4. Sawal HA, Harripaul R, Mikailov A, et al. Biallelic truncating SCN9A mutation identified in four families with congenital insensitivity to pain in Pakistan. Clin Genet. 2016;90(6):563-565. [DOI] [PubMed] [Google Scholar]
- 5. Drenth J, Waxman S. Mutations in sodium-channel gene SCN9A cause a spectrum of human genetic pain disorders. J Clin Invest. 2007;117(12):3603-3609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kurban M, Wajid M, Shimomura Y, et al. A nonsense mutation in the SCN9A gene in congenital insensitivity to pain. Dermatology. 2010;221(2):179-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bar-On E, Weigl D, Parvari R, et al. Congenital insensitivity to pain. Orthopaedic manifestations. J Bone Joint Surg Br. 2002;84(2):252-257. [DOI] [PubMed] [Google Scholar]
- 8. Swanson AG, Buchan GC, Alvord EC., Jr. Anatomic changes in congenital insensitivity to pain. Arch Neurol. 1965;12:12-18. [DOI] [PubMed] [Google Scholar]
- 9. Langer J, Goebel HH, Veit S. Eccrine sweat glands are not innervatedin hereditary sensory neuropathy type IV. An electron-microscopic study. Acta Neuropathol. 1981;54:199-202. [DOI] [PubMed] [Google Scholar]
- 10. Nolano M, Crisci C, Santoro L, et al. Absent innervation of skin and sweat glands in congenital insensitivity to pain with anhydrosis. Clin Neurophysiol. 2000;111:1596-1601. [DOI] [PubMed] [Google Scholar]
- 11. Zhang Y, Haga N. Skeletal complications in congenital insensitivity to pain with anhydrosis: a case series of 14 patients and review of articles published in Japanese. Orthop Sci. 2014;19(5):827-831. [DOI] [PubMed] [Google Scholar]
- 12. Axelrod FB, Gold-von Simson G. Hereditary sensory and autonomic neuropathies: types II, III and IV. Orphanet J Rare Dis. 2007;2:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Schulman H, Tsodikow V, Einhorn M, et al. Congenital insensitivity to pain with anhidrosis (CIPA): the spectrum of radiological findings. Pediatr Radiol. 2001;31(10):701-705. [DOI] [PubMed] [Google Scholar]
- 14. Indo Y, Tsuruta M, Hayashida Y, et al. Mutations in the TRKA/NGF receptor gene in patients with congenital insensitivity to pain with anhidrosis. Nat Genet. 1996;13(4):485-488. [DOI] [PubMed] [Google Scholar]
- 15. Indo Y, Mardy S, Tsurate M, et al. Structure and organization of the human TRK A gene encoding a high affinity receptor for nerve growth factor. Jpn J Hum Genet. 1997;42(2):343-351. [DOI] [PubMed] [Google Scholar]
- 16. Lin YP, Su YN, Wend WC, et al. Novel neurotrophic tyrosine kinase receptor type I gene mutation associated with congenital insensitivity to pain with anhidrosis. J Child Neurol. 2010;25(12):1548-1551. [DOI] [PubMed] [Google Scholar]
- 17. Daneshjou K, Jafarieh H, Raaeskarami S-R. Congenital insensitivity to pain and anhydrosis (CIPA) syndrome; A report of 4 cases. Iran J Pediatr. 2012;22(3):412-416. [PMC free article] [PubMed] [Google Scholar]
- 18. Freeman R. Autonomic peripheral neuropathy. Lancet. 2005;365:1259-1270. [DOI] [PubMed] [Google Scholar]
- 19. van den Bosch GE, Baartmans MG, Vos P, et al. Pain insensitivity syndrome misinterpreted as inflicted burns. Pediatrics. 2014;133(5):e1381-e1137. [DOI] [PubMed] [Google Scholar]
- 20. Perez-Lopez LM, Cabrera-Gonzalez M, Gutierrez-de la, Iglesia D, et al. Update review and clinical presentation in congenital insensitivity to pain and anhidrosis. Case Rep Pediatr. 2015;2015:589852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rosemberg S, Nagahashi Marie SK, Kliemann S. Congenital insensitivity to pain with anhidrosis (hereditary sensory and autonomic neuropathy type IV). Pediatr Neurol. 1994;11(1):50-56. [DOI] [PubMed] [Google Scholar]
- 22. Nabiyev V, Kara A, Aksoy MC. Multidisciplinary assessment of congenital insensitivity to pain syndrome. Childs Nerv Syst. 2016;32(9):1741-1744. [DOI] [PubMed] [Google Scholar]