Abstract
Background: Treatment decisions regarding volar base fractures of the middle phalanx depend on whether the proximal interphalangeal (PIP) joint is reduced. Our aim was to study the agreement among hand surgeons in determining whether the PIP joint fractures are subluxated and to study the factors associated with subluxation of these fractures. Methods: In this retrospective chart review, 413 volar base fractures of the middle phalanx were included. Demographic and injury-related factors were gathered from medical records and radiographs. Using a Web-based survey, interobserver agreement was determined among 105 hand surgeons on the assessment of PIP joint subluxation of a series of 26 cases. Using the cohort of 413 fractures, a threshold for percent articular involvement and relative fracture displacement that corresponds with subluxation of the PIP joint was analyzed. Results: We found moderate to substantial agreement between hand surgeons on subluxation (κ = 0.59, P < .0001) and an overall percent agreement of 85%. Percent articular involvement and relative fracture displacement were independently associated with subluxation of the PIP joint (P < .001). Percent articular involvement of 35% had a specificity of 90% and a negative predicting value (NPV) of 92% for joint subluxation. Relative fracture displacement of 35% had a specificity of 92% and an NPV of 94% for joint subluxation. Conclusions: Surgeons generally agree on whether a PIP joint is subluxated. Percent articular involvement and relative fragment displacement are objective measurements that can help characterize joint stability and assist with decision-making.
Keywords: PIP joint, PIP fracture, dorsal subluxation
Introduction
Volar shear fractures of the proximal interphalangeal (PIP) joint with joint subluxation are difficult to treat. 1 General teaching holds that fractures with less than 15% to 20% of articular involvement are considered stable. When the fracture involves 30% to 50% of the articular surface of the middle phalanx, stability is tenuous. Fractures involving greater than 50% of the articular surface are generally unstable.2-4
Operative treatment of the volar base fracture of the middle phalanx is indicated when the joint is considered unstable, subluxated, or stiff. Operative treatment of the PIP joint remains challenging, and postoperative arthritis and subluxation are not uncommon.5-7 However, establishing whether a joint is subluxated is highly subjective. In addition, guidelines vary regarding threshold articular involvement for operative treatment.4,8-10
Our primary aims are to measure interobserver agreement among hand surgeons in determining whether the PIP joint is subluxated and subsequently study the factors associated with subluxation of the PIP joint and to calculate a threshold value of the percent articular involvement and relative fragment displacement associated with subluxation.
Methods
Study Design
This retrospective chart review was approved by our institutional review board. The medical records and radiographs of all adult patients with volar base fracture of the middle phalanx at 2 urban hospitals between January 2002 and December 2015 were reviewed. We started at 2002 because digital images were not available for prior years.
Patients
International Classification of Diseases, Ninth Edition codes (816.03, 816.0, 816.11, and 816.13) within the defined time frame were used to identify all patients with potential volar base fracture of the middle phalanx in our institutional database (n = 12 262). After excluding patients aged <18 years (n = 2102), we excluded all radiological and operation reports without at least one of the following words: “pip,” “volar avulsion,” “volar plate,” “dorsal dislocation,” “middle,” “proximal interphalangeal,” “middle phalanx,” and “P2” with text searching using STATA 13.0 statistical software (StataCorp LP, College Station, Texas; n = 5833). The remaining patients’ radiographs and medical records (n = 4327) were reviewed by MD researchers to confirm the diagnosis of a volar base fracture of the middle phalanx (n = 1004). We excluded patients without available radiographs (n = 556) and patients without a good lateral view on the radiograph (n = 13). Eighteen patients had 2 affected fingers, and 1 patient had 4 affected fingers. We randomly selected 1 finger per patient for analysis using STATA to have all independent cases for analysis, resulting in a cohort of 413 patients with a volar base fracture of the middle phalanx. Demographic and injury-related data were gathered from the electronic medical records.
Radiographs
Fragment size, size of the intact joint surface, and fragment displacement were measured on radiographs with a lateral view. Percent articular involvement was then calculated as the percentage of the size of the articular segment of the fracture fragment from the total articular surface. Relative fragment displacement was defined as the percentage of fracture fragment displacement from the total articular surface (Figure 1). 11 All radiographs were assessed on subluxation by 2 MD researchers using the same method as in a previous study on mallet fractures. 12 Disputes were resolved by an attending hand surgeon.
Figure 1.
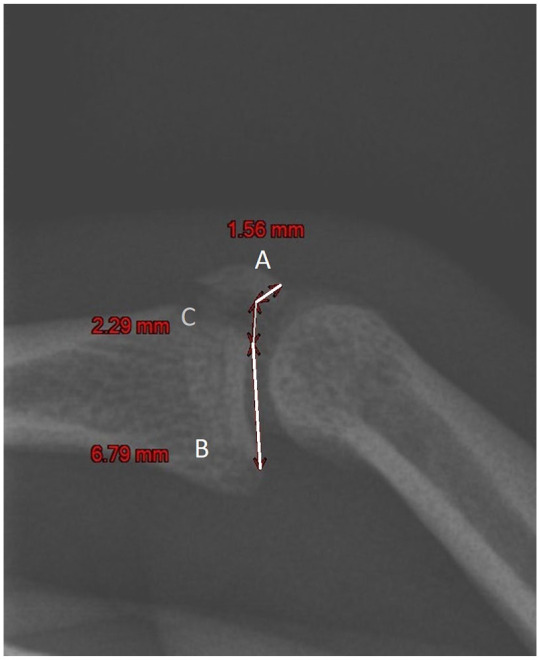
Articular surface involvement (%) is calculated by dividing the fragment size (A) by the total articular surface (A + B). Fragment displacement (%) is calculated by dividing the fragment displacement (C) by the total articular surface (A + B).
Note. In this example, A is 1.56 mm, B is 6.79 mm, and C is 2.29 mm. This results in an articular surface involvement of 19% and fragment displacement of 27%.
Interpretation of Subluxation
For the first study aim, a panel of hand surgeons in the Science of Variation Group (SOVG) were asked to assess several fractured PIP joints on subluxation. The SOVG is a collaborative effort to improve the study of variation interpretation and classification of injuries. This group includes large numbers of fully trained, practicing, and experienced surgeons from all over the world, predominantly the United States and Europe. Through http://www.scienceofvariationgroup.org, many “interobserver reliability” studies were completed.13-18 For these studies, the power increases with the number of observers. 19 We created an online questionnaire using SurveyMonkey (Palo Alto, California) that included radiographs of 26 joint fractures that represented a spectrum of different percentages of articular involvement and relative fragment displacements. We approached only hand surgeons (n = 296). Every hand surgeon in the SOVG was asked to anonymously complete our questionnaire in which the radiographs were shown (lateral views without measurement or patient information) with the question whether the surgeon would classify each joint as subluxated or not.
Statistical Analysis
Cohen’s κ was run and calculated to determine whether there was agreement between hand surgeons in the SOVG on whether 26 PIP joints with volar fracture of the base of the middle phalanx were subluxated. Cohen’s κ is intended to give a quantitative measurement of the magnitude of agreement between observers by calculating the difference between how much agreement is actually present and how much agreement would be expected to be present by chance alone. Bootstrapping (number of resamples of 5000) was used to calculate the P value and 95% confidence interval (CI) for κ values. A value of 0.01 to 0.20 indicates slight agreement; 0.21 to 0.40, fair agreement; 0.41 to 0.60, moderate agreement; 0.61 to 0.80, substantial agreement; and 0.81 to 0.99, almost perfect agreement. 20 The percent agreement, calculated as the number of agreement scores divided by the total number of scores, was also reported as suggested by McHugh 21 for health care studies.
Variables were presented as frequencies and percentages for categorical variables and as mean with SD for continuous variables. In bivariate analysis, Fisher exact test was used for categorical variables and t test for continuous variables. Factors with a value of P <.05 in bivariate analysis were entered into a multivariate logistic regression analysis to assess whether factors were independently associated with subluxation after volar base fracture of the middle phalanx. The area under the receiver operating characteristic curve (ROC) was calculated, and the Hosmer-Lemeshow test was used to assess model fit.
An ROC curve was created to determine a threshold for percent articular involvement and relative fragment displacement that corresponds with subluxation of the PIP joint with a high specificity and negative predicting value (NPV). 22
Patients Characteristics
Of the 413 patients with a volar base fracture of the middle phalanx, 259 (63%) were men, with a mean age of 40 (SD, 15; range, 18-81) years, and the patients were predominantly white (81%). The ring finger was the most affected (33%), and the most common cause was a sports injury (36%). Nine fractures (2.2%) were open, and 81 (20%) fractures were comminuted. The mean time between injury and first visit was a week (Table 1).
Table 1.
Patient Characteristics and Factors Associated With Subluxation of Proximal Interphalangeal Fracture.
| Characteristic | All patients | Subluxated | P value | |
|---|---|---|---|---|
| No | Yes | |||
| (N = 413) | (n = 342) | (n = 71) | ||
| Age, mean (SD), y | 40 (15) | 40 (15) | 39 (14) | .65 |
| Sex, No. (%) | ||||
| Men | 259 (63) | 206 (60) | 53 (75) | .022 |
| Women | 154 (37) | 136 (40) | 18 (25) | |
| Race, No. (%) | .16 | |||
| White | 320 (81) | 265 (82) | 55 (79) | |
| Black | 18 (4.6) | 17 (5.2) | 1 (1.4) | |
| Hispanic | 16 (4.1) | 10 (3.1) | 6 (8.6) | |
| Asian | 12 (3.0) | 9 (2.8) | 3 (4.3) | |
| Other | 29 (7.3) | 24 (7.4) | 5 (7.1) | |
| Smoking, No. (%) a | ||||
| No | 322 (87) | 265 (87) | 57 (88) | >.99 |
| Yes | 49 (13) | 41 (13) | 8 (12) | |
| Diabetes, No. (%) | ||||
| No | 391 (95) | 322 (94) | 69 (97) | .40 |
| Yes | 22 (5.3) | 20 (5.9) | 2 (2.8) | |
| Body mass index, mean (SD), kg/m2 | 27 (5.4) | 27 (5.7) | 27 (4.0) | .73 |
| Affected finger, No. (%) | .57 | |||
| Index | 72 (17) | 58 (17) | 14 (20) | |
| Middle | 89 (22) | 78 (23) | 11 (15) | |
| Ring | 135 (33) | 110 (32) | 25 (35) | |
| Small | 116 (28) | 95 (28) | 21 (30) | |
| Dominant side affected, No. (%) b | >.99 | |||
| No | 137 (52) | 111 (52) | 26 (51) | |
| Yes | 127 (48) | 102 (48) | 25 (49) | |
| Cause of injury, No. (%) c | .36 | |||
| Sports | 123 (36) | 106 (37) | 17 (18) | |
| Fall | 114 (33) | 87 (31) | 27 (44) | |
| Impact | 77 (22) | 66 (23) | 11 (18) | |
| Crush | 21 (6.1) | 17 (6.0) | 4 (6.6) | |
| Sharp | 2 (0.58) | 2 (0.70) | 0 | |
| Other | 9 (2.6) | 7 (2.5) | 2 (3.3) | |
| Open fracture, No. (%) | >.99 | |||
| No | 403 (98) | 333 (98) | 70 (99) | |
| Yes | 9 (2.2) | 8 (2.4) | 1 (1.4) | |
| Comminution, No. (%) | >.99 | |||
| No | 332 (80) | 297 (87) | 35 (49) | |
| Yes | 81 (20) | 45 (13) | 36 (51) | |
| Days between injury and first visit, mean (SD) | 7.0 (25) | 7.1 (27) | 6.5 (16) | .87 |
| Fragment size, mean (SD; min-max), % | 22 (16; 1.5-80) | 19 (13; 1.5-80) | 39 (17; 5.1-72) | <.001 |
| Fragment displacement, mean (SD; min-max), % | 25 (30; 0.67-176) | 16 (14; 0.67-120) | 68 (30; 5.2-176) | <.001 |
Bold values indicate a statistical significance value.
n = 371.
n = 264.
n = 364.
Results
Interobserver Agreement
There was moderate agreement between the 105 hand surgeons on subluxation in 26 cases, κ = 0.59 (95% CI, 0.44-0.74), P < .001. In 4 (15%) of the 26 cases, about half of the surgeons thought the joint was subluxated and nearly half thought it did not. The percent agreement was 85% (Table 2).
Table 2.
Interobserver Agreement on Subluxation in PIP Joint Fractures Assessed by 105 Hand Surgeons.
| PIP joint case | Subluxated (n) | Not subluxated (n) | Articular involvement, % | Fragment displacement, % |
|---|---|---|---|---|
| 3 | 105 | 0 | 65 | 62 |
| 17 | 105 | 0 | 62 | 64 |
| 19 | 105 | 0 | 67 | 40 |
| 20 | 105 | 0 | 52 | 30 |
| 9 | 105 | 0 | 50 | 75 |
| 12 | 104 | 1 | 32 | 53 |
| 26 | 103 | 2 | 13 | 20 |
| 15 | 96 | 9 | 44 | 48 |
| 24 | 90 | 15 | 40 | 26 |
| 16 | 81 | 24 | 72 | 14 |
| 7 | 78 | 27 | 55 | 81 |
| 18 | 77 | 28 | 32 | 15 |
| 23 | 70 | 35 | 53 | 20 |
| 5 | 63 | 42 | 12 | 9.5 |
| 22 | 60 | 45 | 48 | 52 |
| 4 | 60 | 45 | 42 | 5.9 |
| 25 | 57 | 48 | 54 | 14 |
| 21 | 27 | 78 | 24 | 38 |
| 1 | 19 | 86 | 22 | 2.4 |
| 2 | 11 | 94 | 21 | 21 |
| 10 | 6 | 99 | 9.7 | 17 |
| 13 | 5 | 100 | 22 | 20 |
| 14 | 4 | 101 | 19 | 9.9 |
| 11 | 3 | 102 | 24 | 25 |
| 8 | 2 | 103 | 17 | 4.4 |
| 6 | 1 | 104 | 18 | 16 |
Note. Percent agreement: 85%. κ = 0.59; 95% confidence interval: 0.435-0.740; P < .001. PIP = proximal interphalangeal.
Shading indicates the cases with the lowest interobserver agreement.
In our cohort of 413 patients, significantly more men had a subluxated PIP joint compared with women—29% versus 12%, respectively (P = .022). Furthermore, percent articular involvement and relative fragment displacement (both Ps < .001) were significantly associated with subluxation (Table 2). In multivariate analysis, percent articular involvement (odds ratio [OR], 1.1; 95% CI, 1.04-1.09; P < .001) and relative fragment displacement (OR, 1.1; 95% CI, 1.04-1.08; P < .001) were independently associated with subluxation of the PIP joint after volar base fracture of the middle phalanx, with an area under the ROC of 0.94, and the Hosmer-Lemeshow test had a P value of .81 (Table 3).
Table 3.
Factors Independently Associated With Subluxation of Proximal Interphalangeal Fracture (N = 413).
| Characteristic | Odds ratio | Lower (95% CI) | Upper (95% CI) | P value |
|---|---|---|---|---|
| Male sex | 1.1 | 0.48 | 2.6 | .80 |
| Fragment size, % | 1.1 | 1.04 | 1.09 | <.0001 |
| Fragment displacement, % | 1.1 | 1.04 | 1.08 | <.0001 |
Note. Area under the receiver operating characteristic curve = 0.94. P value for Hosmer-Lemeshow test (goodness-of-fit test) = 0.81. CI = confidence interval.
Bold values indicate a statistical significance value.
Threshold for Percent Articular Involvement and Relative Fragment Displacement Associated With Joint Subluxation
The area under the curve (AUC) for percent articular involvement was 0.82 (95% CI, 0.77-0.88), indicating that it is a reasonable model for predicting subluxation. Percent articular involvement of 35% had a specificity of 90% and an NPV of 92% (Table 4). The AUC for relative fragment displacement was 0.90 (95% CI, 0.86-0.94), with a specificity of 92% for subluxation at a threshold relative fragment size of 35% of the overall distance of the joint surface (NPV, 94%; Table 5).
Table 4.
Receiver Operating Characteristic Curve Analysis for Different Thresholds of Articular Involvement for Subluxation.
| Threshold, % | Sensitivity | Specificity |
|---|---|---|
| 0 | 100 | 0 |
| 5 | 100 | 4.7 |
| 10 | 99 | 26 |
| 15 | 92 | 44 |
| 20 | 81 | 66 |
| 25 | 73 | 78 |
| 30 | 66 | 85 |
| 35* | 64 | 90 |
| 40 | 48 | 93 |
| 45 | 40 | 96 |
| 50 | 30 | 96 |
| 55 | 19 | 97 |
| 60 | 12 | 98 |
| 65 | 7.9 | 99 |
| 70 | 2.7 | 100 |
Note. Negative predicting value of 92%.
The best clinically relevant threshold for articular involvement of subluxation with a high specificity.
Table 5.
Receiver Operating Characteristic Curve Analysis for Different Thresholds of Fracture Displacement.
| Threshold, % | Sensitivity | Specificity |
|---|---|---|
| 0 | 100 | 0 |
| 5 | 100 | 13 |
| 10 | 97 | 43 |
| 15 | 92 | 62 |
| 20 | 88 | 76 |
| 25 | 82 | 84 |
| 30 | 74 | 87 |
| 35* | 73 | 92 |
| 40 | 70 | 93 |
| 45 | 64 | 95 |
| 50 | 62 | 96 |
| 55 | 55 | 97 |
| 60 | 49 | 97 |
| 65 | 42 | 99 |
| 70 | 40 | 99 |
| 75 | 38 | 99 |
| 80 | 34 | 99 |
Note. Negative predicting value of 95%.
The best clinically relevant threshold for Fracture displacement with a high specificity.
Discussion
We found that in a review of 26 sample cases among 105 surgeons, there was a moderate to substantial agreement among hand surgeons on whether a PIP joint fracture-dislocation was subluxated. On this basis, we performed a retrospective image review and found that in a volar fracture of the middle phalangeal base, 35% articular involvement had a specificity of 90% and an NPV of 92% for subluxation and a specificity of 92% and an NPV of 95% for 35% relative fragment displacement. We found no other demographic or injury-related factors associated with subluxation.
This study has some limitations. First, as with any retrospective study, we were dependent on coding accuracy and available imaging to establish our cohort. However, the large sample size helps mitigate this problem. Second, radiographs in isolation are not necessarily sufficient to determine joint instability; however, the goal of the study was to understand to what degree quantitative measurements on radiographs can assist in determining instability. Two MD researchers evaluated radiographs with methods used in a previous study on mallet fractures. 12 Disputes regarding joints that were subluxated were resolved by an attending hand surgeon. Third, measuring articular involvement on radiographs might lead to an underestimation of actual articular involvement as noted by Donovan et al. 23 However, these fractures are more frequently assessed with similar standard radiographs, which makes our study generalizable to usual practice. Finally, 105 hand surgeons (response rate of 35%) completed the questionnaire because many SOVG members listed in the database are not active participants and participate on a voluntary basis. In addition, e-mails in the list are not updated frequently, so the participation rate is not similar to the true response rate as this is not a survey that “surveys” the observers but rather tests the variability of a specific factor of interest. However, the response rate is comparable with other studies including the SOVG. 24
We found moderate interobserver agreement when 105 hand surgeons assessed 26 radiographs of only volar middle phalangeal base fractures on subluxation. This is in line with Janssen et al who studied the most reliable and useful middle phalanx base fracture characteristics for surgical decision-making. Ninety-nine hand surgeons evaluated 21 intra-articular fractures on lateral radiographs. They reported a substantial interobserver agreement (κ = 0.72) among surgeons in classifying subluxation. There was also a substantial agreement (κ = 0.67) on percent articular involvement. No differences were found in the agreement on subluxation and proposed treatment between experienced (>10 years of experience) and less experienced surgeons (<10 years of experience) and other surgeon demographics. 24
Overall, we found that surgeons tend to agree as to which middle phalanx base fractures are subluxated. In distinction, many other radiographic evaluations through the SOVG do not have similar concordance. Van Leeuwen et al reported a fair agreement (κ = 0.36) among hand surgeons who evaluated the diagnosis of Kienböck disease on radiograph. 18 In a study about treatment of small finger metacarpal neck fractures, 250 surgeons assessed 20 radiographs either without or with measurements of angulation. Both groups had fair agreement, that is, κ of 0.22 versus 0.24, respectively. 25 When surgeons were asked to distinguish mild Madelung deformity from normal on radiograph, interobserver agreement was low (κ = 0.12). 26 Mellema et al 27 found a slight overall interobserver agreement (κ < 0.20) in surgeons classifying simple proximal humeral fracture. Mallee et al 28 found low agreement (κ = 0.15) between observers for the recognition of scaphoid fracture on 6-week radiographs.
Ninety percent of fractures that were not subluxated had a percent articular involvement less than 35%. Also, 92% of fractures with a percent articular involvement of 35% or lower were not subluxated. This is consistent with prior thinking. In 1982, Eaton and Dray 9 concluded that volar base fractures of the middle phalanx involving more than 40% of the articular surface were classified as unstable because they are more prone to recurrent dorsal subluxation, creating a relationship between articular fracture involvement and dorsal instability. In 1998, Kiefhaber and Stern 4 suggested guidelines for the treatment of PIP fracture-dislocations: (1) restoration of joint congruency by eliminating subluxation, followed by reestablishing joint stability, and (2) early motion. Volar base fractures were divided into 3 groups: articular involvement of less than 30% was categorized as stable, articular involvement of 30% to 50% as tenuous, and articular involvement of greater than 50% as unstable.
In addition, we found relative fragment displacement as a useful objective measure associated with subluxation, independent from the size of the articular fragment. Ninety-two percent of stable fractures had relative fragment displacement of less than 35% of the total articular length. Only 5% of fractures with a relative fragment displacement of less than 35% of the total articular length were unstable. A similar association between articular involvement and fragment displacement with subluxation has been observed in distal interphalangeal (DIP) joint fracture-dislocations. Moradi et al found 39% articular involvement to be the threshold for subluxation in DIP fracture-dislocations, which is relatively close to our findings in PIP fracture-dislocations. We found a greater variance of both percent articular involvement and relative fragment displacement in the PIP joint fractures compared with data from the DIP joint reported by Moradi et al. 11
In conclusion, hand surgeons generally agree on whether a PIP joint is subluxated after a volar base of middle phalanx fracture. When subluxation is not clear, percent articular involvement and relative fragment displacement are objective measurements that can help characterize joint stability and assist with decision-making. We found that when about one-third of the articular surface is involved in fracture on a lateral radiograph, there is a reasonable likelihood that the PIP joint is unstable. This guideline may help with surgical decision-making in the treatment of these injuries.
Acknowledgments
Science of Variation Group (collaborative authorship): J. Abrams, L. Adolfsson, N.M. Akabudike, C. Bainbridge G.W. Balfour, H.B. Bamberger, C.J.R. Barreto, M. Baskies, A. Bauer, T. Baxamusa, R. de Bedout, P. Benhaim, J.W. Brubacher, M. Calcagni, K.J. Chepla, J. Choueka, G. DeSilva, J.F. Di Giovanni, R.W. Draeger, S. Duncan, H. Durchholz, K. Elzinga, J. M. Erickson, P.J. Evans, S. Farr, C.H. Fernandes, C.H. Fernandes, G. Fierro, T.J. Fischer, W.E. Floyd III, Fricker, R.S. Gilbert, A.Y. Giuffrida, T. Gosens, M.W. Grafe, L.C. Grandizio, T.G. Guitton, P. Hahn, J. Hall, W.C. Hammert, P.F.W. Hannemann, B.F. Hearon, S.L. Henry, N.A. Hoekzema, E.P. Hofmeister, B. Hyatt, E.F. Ibrahim, A.M. Ilyas, P. Jebson, J.W. Johnson, C.M. Jones, S.G. Kaar, D.M. Kalainov, F.T.D. Kaplan, V. Kashyap Gajendran, N.H. Kazmers, S.A. Kennedy, H.L. Kimball, G. Kohut, L.B. Lane, L. Lattanza, K.E. Lee, J.A. McAuliffe, I. McGraw, D.M. McKee, C. Metzger, B. Miller, S. Mitchell, C.L. Moreno-Serrano, P. Muhl, M. Nakashian, M. Nancollas, J.F. Nappi, F. O’Brien, J.A. Ortiz Jr, P.W. Owens, B. Palmer, B.A. Palmer, M.J. Palmer, M. Patel, J.M. Patiño, G. Pianka, G.M. Pess, D. Polatsch, T. Rebele, M.J. Richard, M. Richardson, M. Rizzo, C. Rodner, V. Ruggiero, J. Sandoval, M. Sanmartin-Fernandez, N.W.L. Schep, A. Shafritz, J.D. Tavakolian, G. Veríssimo de Miranda, A.J.H. Vochteloo, E.T. Walbeehm, G.P. Watchmaker, B.W.D. Wills, M. Wilson, J. Wint, M.M. Wood, E.E. Zaidenberg, D. Zeltser
Footnotes
Ethical Approval: This study was approved by our institutional review board. The institutional review board of our institution approved this study under protocol #2009P001019/MGH.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all individual participants included in the study.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Each author certifies that he has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements) or financial remunerations that might pose a conflict of interest in connection with the submitted article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Statement of the Location Where the Work Was Performed: The work was performed at the Hand and Upper Extremity Service, Department of Orthopedic Surgery, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA.
ORCID iD: Neal C. Chen  https://orcid.org/0000-0001-7527-1110
https://orcid.org/0000-0001-7527-1110
References
- 1. Kamnerdnakta S, Huetteman HE, Chung KC. Complications of proximal interphalangeal joint injuries: prevention and treatment. Hand Clin. 2018;34(2):267-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shah CM, Sommerkamp TG. Fracture dislocation of the finger joints. J Hand Surg Am. 2014;39(4):792-802. [DOI] [PubMed] [Google Scholar]
- 3. Calfee RP, Sommerkamp TG. Fracture-dislocation about the finger joints. J Hand Surg Am. 2009;34(6):1140-1147. [DOI] [PubMed] [Google Scholar]
- 4. Kiefhaber TR, Stern PJ. Fracture dislocations of the proximal interphalangeal joint. J Hand Surg Am. 1998;23(3):368-380. [DOI] [PubMed] [Google Scholar]
- 5. Deitch MA, Kiefhaber TR, Comisar BR, et al. Dorsal fracture dislocations of the proximal interphalangeal joint: surgical complications and long-term results. J Hand Surg Am. 1999;24(5):914-923. [DOI] [PubMed] [Google Scholar]
- 6. Waris E, Mattila S, Sillat T, et al. Extension block pinning for unstable proximal interphalangeal joint dorsal fracture dislocations. J Hand Surg Am. 2016;41(2):196-202. [DOI] [PubMed] [Google Scholar]
- 7. Eaton RG, Malerich MM. Volar plate arthroplasty of the proximal interphalangeal joint: a review of ten years’ experience. J Hand Surg Am. 1980;5(3):260-268. [DOI] [PubMed] [Google Scholar]
- 8. Wheeless CR. Dorsal Fracture Dislocations of the PIP Joint. 2012. http://www.wheelessonline.com/ortho/dorsal_fracture_dislocations_of_the_pip_joint. Accessed December 4, 2019.
- 9. Eaton RG, Dray GJ. Dislocations and ligament injuries in the digits. In: Green DP, ed. Operative Hand Surgery. 3rd ed. New York, NY: Churchill Livingstone; 1982:637-668. [Google Scholar]
- 10. Weinzweig N, Gozalez MH. Metacarpal and phalangeal fractures. In: Weinzweig J, ed. Plastic Surgery Secrets. 2nd ed. Philadelphia, PA: Mosby Elsevier; 2010:794-801. [Google Scholar]
- 11. Moradi A, Braun Y, Oflazoglu K, et al. Factors associated with subluxation in mallet fracture. J Hand Surg Eur Vol. 2017;42:176-181. [DOI] [PubMed] [Google Scholar]
- 12. Oflazoglu K, Moradi A, Braun Y, et al. Mallet fractures of the thumb compared with mallet fractures of the fingers. Hand (N Y). 2017;12(3):277-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bruinsma WE, Guitton TG, Warner JJ, et al. Interobserver reliability of classification and characterization of proximal humeral fractures: a comparison of two and three-dimensional CT. J Bone Joint Surg Am. 2013;95(17):1600-1604. [DOI] [PubMed] [Google Scholar]
- 14. Buijze GA, Wijffels MM, Guitton TG, et al. Interobserver reliability of computed tomography to diagnose scaphoid waist fracture union. J Hand Surg Am. 2012;37(2):250-254. [DOI] [PubMed] [Google Scholar]
- 15. Buijze GA, Guitton TG, van Dijk CN, et al. Training improves interobserver reliability for the diagnosis of scaphoid fracture displacement. Clin Orthop Relat Res. 2012;470(7):2029-2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Doornberg JN, Guitton TG, Ring D. Diagnosis of elbow fracture patterns on radiographs: interobserver reliability and diagnostic accuracy. Clin Orthop Relat Res. 2013;471(4):1373-1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gradl G, Neuhaus V, Fuchsberger T, et al. Radiographic diagnosis of scapholunate dissociation among intra-articular fractures of the distal radius: interobserver reliability. J Hand Surg Am. 2013;38(9):1685-1690. [DOI] [PubMed] [Google Scholar]
- 18. van Leeuwen WF, Janssen SJ, Guitton TG, et al. Interobserver agreement in diagnosing early-stage Kienbock disease on radiographs and magnetic resonance imaging. Hand (N Y). 2017;12(6):573-578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Walter SD, Eliasziw M, Donner A. Sample size and optimal designs for reliability studies. Stat Med. 1998;17(1):101-110. [DOI] [PubMed] [Google Scholar]
- 20. Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37(5):360-363. [PubMed] [Google Scholar]
- 21. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22(3):276-282. [PMC free article] [PubMed] [Google Scholar]
- 22. Metz CE. Basic principles of ROC analysis. Semin Nucl Med. 1978;8(4):283-298. [DOI] [PubMed] [Google Scholar]
- 23. Donovan DS, Podolnick JD, Reizner W, et al. Accuracy and reliability of radiographic estimation of volar lip fragment size in pip dorsal fracture-dislocations. Hand (N Y). 2019;14:797-802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Janssen SJ, Molleman J, Guitton TG, et al. What middle phalanx base fracture characteristics are most reliable and useful for surgical decision-making? Clin Orthop Relat Res. 2015;473(12):3943-3950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tosti R, Ilyas AM, Mellema JJ, et al. Interobserver variability in the treatment of little finger metacarpal neck fractures. J Hand Surg Am. 2014;39(9):1722-1727. [DOI] [PubMed] [Google Scholar]
- 26. Farr S, Guitton TG, Ring D. How reliable is the radiographic diagnosis of mild Madelung deformity. J Wrist Surg. 2018;7(3):227-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mellema JJ, Kuntz MT, Guitton TG, et al. The effect of two factors on interobserver reliability for proximal humeral fractures. J Am Acad Orthop Surg. 2017;25(1):69-76. [DOI] [PubMed] [Google Scholar]
- 28. Mallee WH, Mellema JJ, Guitton TG, et al. 6-week radiographs unsuitable for diagnosis of suspected scaphoid fractures. Arch Orthop Trauma Surg. 2016;136(6):771-778. [DOI] [PMC free article] [PubMed] [Google Scholar]


