Abstract
The extensor indicis proprius muscle (EIPM) is considered a key muscle in the assessment of the level of the neurologic lesion causing any motor or sensory medio-cubital impairment of the hand.
The aim of this study is to illustrate the anatomical peculiarities of the EIPM, the ultrasound (US) anatomy of the inferoposterior part of the forearm, and the technique of US-guided electromyography (EMG) of the EIPM.
The US-guided EMG of the EIPM is technically easy and safe for young practitioners, provided there is a good knowledge of US anatomy of the inferoposterior part of the forearm.
Keywords: residents, electromyography, ultrasound, anatomy, extensor indicis proprius muscle
Introduction
Nowadays, residents and young practitioners still have practical difficulties in electromyographic detection of certain small and deep muscles, such as the extensor indicis proprius muscle (EIPM). They need to acquire some procedural skills for electromyography (EMG) needle placement. For this, the musculoskeletal ultrasound (US) would be of considerable and very precious help. Indeed, it facilitates the identification of these difficult muscles and provides a good knowledge of the forearm ultrasound anatomy [1].
This manuscript aims to illustrate the anatomical peculiarities of the EIPM, the US anatomy of the inferoposterior part of the forearm, and the technique of US-guided EMG of the EIPM. The latter is considered a key muscle in the assessment of the level of a neurologic lesion causing any motor or sensory medial/cubital impairment of the hand [2].
Technical report
A good knowledge of the ultrasound anatomy of the forearm allows locating the EIPM easily to prick it with an EMG needle. First, the practitioner must place the ultrasound probe at the level of the distal part of the posteromedial side of the forearm (Figure 1). The US image should then show all muscles of the posterior compartment of the forearm and, in particular, the EIPM on the extreme medial side as shown in Figure 2. It is then easy and safe to prick the EIPM with the EMG needle. The physician should also know that mobilization of the index is mandatory for the exact US localization of this muscle. Figure 3 shows a schematic and anatomical illustration of this US picture.
Figure 1. Performing the ultrasound of the forearm.
The ultrasound probe is placed at the level of the distal part of the posteromedial side of the forearm, i.e., 4 to 5 cm above the wrist. The electromyography (EMG) needle is then inserted laterally and perpendicular to the medial edge of the forearm.
Note: This individual depicted in this figure was a resident who provided consent for demonstration purposes.
Figure 2. Ultrasound image.
(A) Ultrasound section in the distal part of the forearm without and (B) with delineation of muscle structures. The extensor indicis proprius muscle (EIPM) is located at the deep medial side of the posterior compartment of the forearm. This ultrasound section shows also the electromyography (EMG) needle (arrowheads) in the EIPM.
APL: abductor pollicis longus; ECU: extensor carpi ulnaris; EDB: extensor digitorum brevis; EDC: extensor digitorum communis; EDM: extensor digitorum mini; EIP: extensor indicis proprius; EPL: extensor pollicis longus; R: radius; U: ulna
Note: These images were taken from a voluntary medical resident.
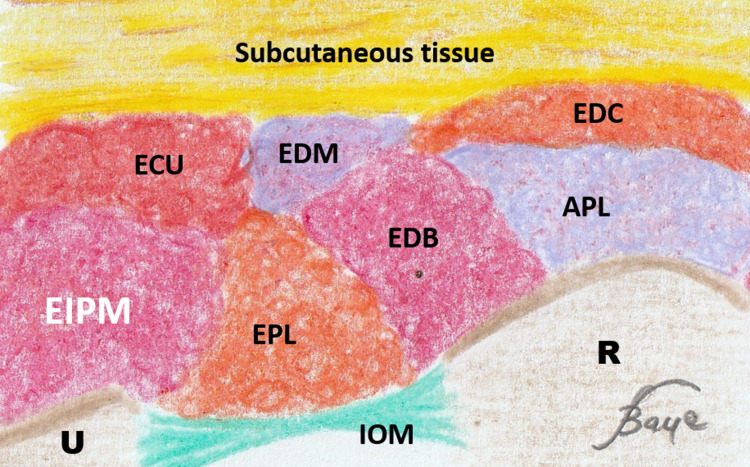
Figure 3. Schematic view.
Schematic and anatomical illustration of the ultrasound section of Figure 2.
APL: abductor pollicis longus; ECU: extensor carpi ulnaris; EDB: extensor digitorum brevis; EDC: extensor digitorum communis; EDM: extensor digitorum mini; EIP: extensor indicis proprius; EPL: extensor pollicis longus; R: radius; U: ulna
Discussion
Anatomy reminder
The EIPM is a thin muscle of the posterior compartment of the forearm. It originates from the distal two-thirds of the posterolateral side of the ulna. Then, it follows a downward path on the medial side of the extensor digitorum longus. At the dorsal side of the carpal bones, the EIPM narrows into a tendon that courses obliquely down to the metacarpal level where it joins the ulnar side of the extensor digitorum tendon. This union forms the extensor apparatus of the index finger [3].
The main function of this muscle is the extension of the index finger by acting at the metacarpophalangeal and interphalangeal joints. In addition, the EIPM may incidentally provoke a weak wrist extension as it crosses this joint.
The main anatomic particularity of the EIPM is that it is the only muscle of the forearm posterior compartment to be innervated by radial nerve branches strictly issued from the C8-T1 roots.
US contribution for performing needle EMG of the EIPM
Two recent studies have shown the significant contribution of musculoskeletal US in teaching residents and young electromyographers to perform needle EMG of the EIPM [1, 4]. Moreover, these studies also showed that trainees have high rates of failure of standard EMG detection of the EIPM.
US also has an important role in detecting EIPM anatomical variants that can be bifidity with a double insertion on the index finger or by giving one tendon to the index and another to the middle finger or thumb. Exceptionally, EIPM can give three slips for the index or one for the index, one for the ring finger, and a third one for the middle [5-6].
Diagnostic value of the extensor indicis proprius muscle
The EIPM electromyographic study is essential for determining the level of non-traumatic nerve damage at the origin of any motor or sensory medial/cubital impairment as in the case of non-traumatic hand amyotrophy.
Moreover, thanks to the fact that it is the only muscle to be innervated strictly by the C8-T1 branches, the EIPM is a key muscle. Thus, the electromyographic study allows distinguishing between a medial/cubital truncal lesion and a proximal C8-T1 root impairment. Indeed, it is the only muscle whose neurogenic impairment leads to the diagnosis of a neurologic lesion at the level of the primary lower trunk instead of a lesion of the anteromedial secondary trunk [7].
In general, the clinical signs of this type of nerve impairment are 1) atrophy of the hand (thenar and hypothenar eminences and interosseous muscles), 2) paraesthesia of the finger(s), and 3) muscle testing revealing the weakness of hand muscles. For example, a patient can have muscle testing at 3 (range: 0 - 5) of the abductor pollicis brevis and the EIPM [8].
Conclusions
Thanks to its anatomical peculiarities, the EIPM is a key muscle in determining the level of the neurologic lesion that causes motor or sensory medial/cubital impairment of the hand. Ultrasound guidance greatly facilitates the electromyographic exploration of the EIPM (a thin and deep muscle), particularly for trainees and young practitioners who have to be familiar with the anatomy of the inferoposterior part of the forearm.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.The accuracy of needle electrode placement by trainees in selected forearm muscles using verification by neuromuscular ultrasound. Jin TG, D'Andrea D, Ajroud-Driss S, Franz CK. J Electromyogr Kinesiol. 2021;60:102573. doi: 10.1016/j.jelekin.2021.102573. [DOI] [PubMed] [Google Scholar]
- 2.Gragossian A, Varacallo M. StatPearls (Internet) Treasure Island (FL): StatPearls Publishing; 2021. Radial Nerve Injury. [PubMed] [Google Scholar]
- 3.Moore KL, Dalley AF, Agur AMR. Clinically Oriented Anatomy, 7th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2013. Upper Limb; pp. 746–779. [Google Scholar]
- 4.Resident accuracy of electromyography needle electrode placement using ultrasound verification. Karvelas K, Ziegler C, Rho ME. PM R. 2016;8:748–753. doi: 10.1016/j.pmrj.2015.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The prevalence of the extensor indicis tendon and its variants: a systematic review and meta-analysis. Yammine K. Surg Radiol Anat. 2015;37:247–254. doi: 10.1007/s00276-014-1352-0. [DOI] [PubMed] [Google Scholar]
- 6.Extensor indicis proprius muscle and its variants together with the extensor digitorum brevis manus muscle: a common classification. Clinical significance in hand and reconstructive surgery. Georgiev GP, Tubbs RS, Iliev A, Kotov G, Landzhov B. Surg Radiol Anat. 2018;40:271–280. doi: 10.1007/s00276-018-1981-9. [DOI] [PubMed] [Google Scholar]
- 7.Cael C. Burlington: Jones & Bartlett Learning; 2020. Functional Anatomy: Musculoskeletal Anatomy, Kinesiology, and Palpation for Manual Therapists (Enhanced Edition) [Google Scholar]
- 8.Correlation of electrodiagnostic findings in C8 radiculopathies with radiographic data: a retrospective chart review. Tahmasbi Sohi M, Nortman S, Brega K, Forster JE, Guzzetti JR. Am J Phys Med Rehabil. 2021;100:721–724. doi: 10.1097/PHM.0000000000001722. [DOI] [PubMed] [Google Scholar]