Abstract
Introduction: Perceived control is an individual’s subjective beliefs about the amount of control he or she has over the environment or outcome. Objective: To examine the relationship between perceived control, preventive health behaviors, and mental health effects of undergraduate nursing students during the COVID-19 pandemic. Methods: This cross-sectional correlational study used online self-administered questionnaires. Participants were nursing students attending 3 universities in Tokyo, Japan. Relationships among variables were quantitatively analyzed using linear regressions and a structural equation modeling after adjusting for demographic factors. Results: A total of 557 students participated in the survey. The analysis indicated that higher levels of perceived control were significantly related to higher levels of preventive health behaviors. Although higher preventive health behaviors were related to negative mental health effects, higher levels of perceived health competence translated to improved mental health effects. Perceived control was not directly related to mental health effects but positively related to perceived health competence. Long work hours per week and short hours of sleep per day were associated with lower preventive health behaviors. There were significant differences in the levels of perceived control and preventive health behaviors among students at the 3 universities. Discussion: To improve health behaviors and health competence and subsequently alleviate the mental health effects caused by strictly adhering to recommended health behaviors, students may be supported by the strategies that increase their perceived control. In addition to institutional support, students also require adequate sleep and financial stability to help prevent infections while protecting their mental health.
Keywords: sense of control, health behavior, mental health, nursing, students, COVID-19
Highlights
What do we already know about this topic?
Nursing students’ infection prevention and control measures and the effects they have on their professional and personal mentalities have been studied.
How does your research contribute to the field?
This study’s results aim to present practical information on how best to support healthcare students, who will eventually become industry professionals and leaders, in practicing healthy preventative behaviors against COVID-19 while preventing their academic experiences and professional identities from being interrupted or damaged.
What are your research’s implications toward theory, practice, or policy?
While universities provide students with information sources regarding COVID-19 and safety tactics, and, in turn, students are encouraged to maintain awareness and understanding of social and political issues, so they may effectively prevent infection without increasing their mental burden, nursing faculty monitor and support each student, especially those who are younger, work longer hours, and are only able to get limited hours of sleep.
Introduction
Between December 2019 when its initial cases were first reported in Wuhan, China, and July 2021, the coronavirus disease 2019 (COVID-19) claimed nearly 240 million cases and nearly 5 million confirmed deaths worldwide.1,2 The disease’s devastating impacts have burdened virtually every community in the world, including those of healthcare professionals who have dedicated themselves to treating hordes of patients affected by COVID-19. In the United States, where the number of cases and deaths were the highest in the world, more than 3,600 healthcare workers died during the first year of the pandemic. 3
Overcaution and anxiety, paired with the psychological stress of working on the front lines, have influenced the mindset that prospective healthcare workers, particularly nursing students, have toward their chosen profession. A study conducted in China reported that 9.3% of students in the final year of nursing programs declared their intention to leave the nursing profession after the COVID-19 pandemic. 4 The study found that compared to students who expressed an intention to remain, students who intended to leave exemplified lower professional identity scores. Factors independently related to stronger professional identities were the perceived effectiveness of recommended preventive and control measures (eg, social-distancing, mask-wearing, and quarantining) and higher COVID-19 knowledge. 4
Nursing students’ infection prevention and control measures and the effects they have on their professional and personal mentalities have been studied in the literature. For instance, nursing students who had low levels of preventive health behaviors were more likely to experience anxiety surrounding COVID-19 infection than those with medium or high levels of the same behaviors. 5 Nursing students with positive preventive behaviors during the pandemic were typically older, upperclassmen in their programs, female, and living in urban areas and had strong COVID-19 knowledge, high eHealth literacy, and positive attitudes.6,7 Other contributing factors included high perceived susceptibility (ie, beliefs surrounding the likelihood of getting a disease or condition), 8 high perceived benefits (ie, beliefs surrounding the benefits of various available actions to reduce the disease threat), 8 and low perceived barriers 9 (ie, the potential negative aspects of a particular health action), 8 per the Health Belief Model.
Control beliefs, such as self-efficacy, perceived health competence, and perceived control, have also been found to affect the levels of preventative health behaviors individuals take. Self-efficacy is defined as the perception of control over one’s behavior and ability to achieve one’s goals, and perceived health competence is a measure of one’s sense of competence in the domain of health behavior; both are predictors of preventive health behaviors and positive health outcomes. 10 Meanwhile, perceived control is defined as one’s subjective beliefs surrounding the amount of control one has over their environment or outcome and differs from actual control, which is the objective amount of control an individual has over a given environment or outcome. 11
Several studies have reported perceived control’s associations to enhanced preventive behaviors, perceived general health, and life satisfaction during the COVID-19 pandemic. A lower sense of control was associated with stocking up on food and using a mask for self-protection rather than protecting others, and higher perceived control was associated with responsible behaviors such as coughing into one’s arm to prevent the spread of infection and checking on others during the pandemic with a nationally representative sample in Thailand (N = 1000). 12 Meanwhile, perceived control was able to buffer the psychological effects of regional pandemic severity by moderating the effects of psychological distance across 1,847 participants in 31 provinces of China. 13 Turning their attention to the academic setting, gaining high perceived control over time can help moderate the positive associations between neuroticism and the fear of COVID-19 in university students in Italy (N = 301). 14 Despite the contribution of these studies, the association between perceived control and preventive health behaviors—how preventive behaviors affect nursing students’ mental health and if perceived control buffers the pandemic’s mental consequences—is yet to be reported.
To fill this gap, this study examines (1) the relationship between perceived control and preventive health behaviors and (2) the relationship between perceived control and the mental health effects of committing to preventative health behaviors. Additionally, this study identifies factors that encourage preventive health behaviors in students attending undergraduate nursing programs during the COVID-19 pandemic.
Our study focuses on a sample of students in Japan, a country without strict quarantine demands nor lockdowns that completely restrict social activities and, thus, relies heavily on individual behaviors to prevent infection. Regardless of region, personal infection prevention measures remain as crucial as ever in combating COVID-19 in unvaccinated communities as well as breakthrough cases of vaccinated peoples.
In response to its first and second objectives, this study submits the following 2 hypotheses, respectively:
Hypothesis 1 (H1): Nursing students with higher perceived control practice higher levels of preventive health behaviors.
Hypothesis 2 (H2): Higher perceived control buffers the effects that preventive health behaviors have on mental health (ie, higher preventive health behaviors are associated with more adverse mental health effects, but higher perceived control is associated with less adverse mental health effects).
This study’s results aim to present practical information on how best to support healthcare students, who will eventually become industry professionals and leaders, in practicing healthy preventative behaviors against COVID-19 while preventing their academic experiences and professional identities from being interrupted or damaged.
Conceptual Framework and Definitions
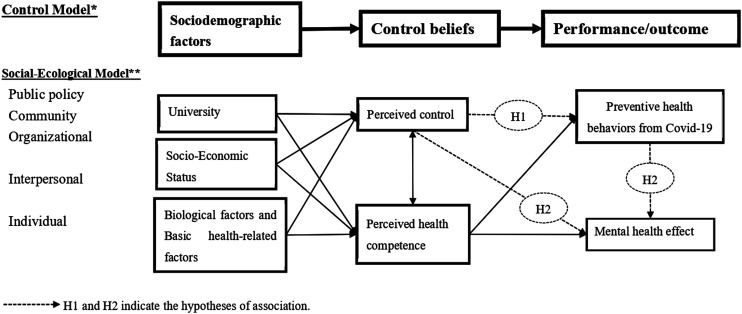
Figure 1 shows this study’s conceptual framework, which utilizes both the control model adapted from Robinson and Lachman 15 and the social-ecological model adapted from the National Institute of Health. 16 This study’s construct is the control model, which suggests that sociodemographic factors affect control beliefs, which, in turn, affect performance and outcome. Meanwhile, social-ecological models emphasize multiple levels of influence, such as public policy, community, organizational, interpersonal, and individual factors, and the idea that behaviors both shape and are shaped by the social environment.
Figure 1.
Conceptual Framework. Source: *Adapted from Robinson, S.A., and Lanchan, M.E. (2017).9. Perceived Control and Behavior Change—A Personalized Approach. In J.W. Reich, and F.J. Infurna (Eds.), Perceived Control Theory, Research and Practice in the First 50 years (pp. 201-227). United States of America: Oxford University Press. **4. Important Theories and Their Key Constructs (Figure 4) In Social and Behavioral Theories, e-Source Behavioral and Social Sciences Research available at https://pdf4pro.com/view/social-and-behavioral-theories-obssr-e-source-5228ab.html https://obssr.od.nih.gov/wp-content/uploads/2016/05/Social-and-Behavorial-Theories.pdf (Retrieved December 15, 2021).
Under this study, sociodemographic factors include the university that the nursing students attend and the students’ socio-economic statuses and biological and basic health-related factors. As shown in Figure 1, these factors inform control beliefs, which include perceived control and perceived health competence, and then these beliefs inform performance and outcome, which are health behaviors, including those that prevent infection by COVID-19, and mental health effects. As denoted on the far-left side of the figure, the social-ecological model dictates that the university falls under public policy, community, and organizational influences; the students’ socio-economic statuses fall under organizational and interpersonal influences; and their biological and basic health-related factors fall under the influence of the individual.
Perceived control is a primary component of social capital, defined as “networks together with shared norms, values and understandings that facilitate co-operation within or among groups.” 17 Individuals who believe they have control over their behavior and additionally possess the ability to contribute to policy decisions regarding their community are capable of achieving positive health outcomes 18 and, cumulatively, improving broader societal and public health outcomes. In this way, perceived control falls under the influence of public policy, community, and organization rather than individual factors while perceived health competence can fall most under the individual’s influence. Both can be affected by all sociodemographic factors.
Preventive health behaviors, especially in Japan, depend on each individual’s performance to prevent infection but can be affected by both control beliefs. That is, perceived control may induce preventative health behaviors, but those who strictly follow social-distancing and stay-home orders may suffer from isolation and/or depression, which this study defines as “mental health effects.”
Methods
Study Design, Setting, and Participants
This cross-sectional correlational study examines undergraduate nursing students attending 3 universities in the Tokyo metropolitan area of Japan. University A is a national institution, and University B and C are private institutions. All nursing students in their first to fourth years (equivalent to freshman through senior year in the U.S.) (N = 1054) were invited to participate in the study and, after consenting, took self-administered questionnaires.
In Japan, most students who pursue higher education do so immediately after graduating from high school, with few who have work experience. While many students do hold part-time jobs for some level of income, the majority rely on their families to pay for their university tuition.
Data Collection
Sampling Procedures
Online questionnaires drafted in Japanese were administered via Google Form. Researchers visited online classrooms through Zoom and, at the end of each session, explained the purpose of the study and the survey procedures. Email invitations and study documents, including descriptions of the study’s purpose, methods, voluntary participation process, and observation of privacy, were also sent to students. By clicking the “Agree” button on the online survey to proceed, participants confirmed that they read, understood, and gave informed consent to participate in the study. Data was collected from November 2020 to February 2021.
Measurements
The questionnaire collected information regarding each participant’s (1) demographics, (2) perceived control and self-efficacy, (3) perceived health competence, and (4) health behaviors.
Demographic questions collected biological data including the participant’s age, gender, ethnic background, height, and weight 19 ; socio-economic data including the participant’s year in the nursing program, marital status, religion, number of live-in family members, work hours per week, and annual family and personal incomes; and basic health-related factors including the participant’s smoking habit, alcohol intake, 20 chronic conditions requiring regular checkup, 21 and hours of sleep per day. 22 In line with previous studies, these variables were considered to reflect a participant’s general health behavior.
Perceived control and self-efficacy 18 were scored on a ten-item, five-point Likert scale (1 = strongly disagree and 5 = strongly agree) adapted from the British general household survey social capital scale. The perceived control and self-efficacy scale covers perceived influence at both the societal and individual levels 17 and consists of 3 domains that evaluate (1) perceived control over community affairs (4 items), (2) perceived influence over political decisions (4 items), and (3) satisfaction with the amount of control one has over their personal life (2 items). A higher score translates to a higher level of self-efficacy, and a sum of the 3 domains, which range from 10 to 50, yields a global score of perceived control and self-efficacy over societal and individual matters. 18 After obtaining permission from Salehi, the original scale was translated into Japanese by the first author then translated back into English by the third author, after which the first, third, and fourth authors finalized the scale after multiple discussions and revisions. This is the first study to date that uses the perceived control and self-efficacy scale with a Japanese population.
Perceived health competence was scored on an eight-item, five-point Likert scale (1 = strongly disagree and 5 = strongly agree) to measure the degree to which an individual feels capable of effectively managing one’s health outcomes. 10 The perceived health competence scale contains both behavioral expectations and outcomes, and scores range from 8 to 40, with higher scores indicating higher health competence. This scale has been previously translated into Japanese, and reliability and validity have been confirmed. 23 Permission to use the scale was obtained from the original developers and translators.
Finally, the health behavior questions consisted of the 2 domains shown in Table 1: Preventive health behaviors containing 17 items, and mental health effects containing 2 items. Note that mental health effects focused specifically on the adverse effects that social-distancing and stay-home orders had on the participant, particularly feelings of stress, depression, or being alienated from society.
Table 1.
Questions regarding health behaviors, N = 557.
| Preventive Health Behaviors | Mean | Median | |
|---|---|---|---|
| 1 | Wear a mask in public | 3.0 | 3 |
| 2 | Self-monitor for respiratory symptoms (eg, cough, runny nose, fever, sore throat, and dyspnea) | 2.8 | 3 |
| 3 | Follow respiratory hygiene recommendations (eg, covering coughs or sneezes by wearing face masks or handkerchief and washing hands often) | 2.9 | 3 |
| 4 | Avoid hand-to-face (especially eyes, mouth, and nose) contact | 2.1 | 2 |
| 5 | Check body temperature regularly | 2.5 | 3 |
| 6 | Wash hands or use hand sanitizer after touching objects and surfaces in public | 2.7 | 3 |
| 7 | Clean and disinfect shared objects and surfaces | 2.1 | 2 |
| 8 | Clean and disinfect packaged products | 1.3 | 1 |
| 9 | Gargle immediately after returning home | 2.6 | 3 |
| 10 | Limit international or domestic travel only to the essential | 2.8 | 3 |
| 11 | Limit usage of public transportation only to the essential | 2.0 | 2 |
| 12 | Avoid crowded, closed, and close-contact settings | 2.6 | 3 |
| 13 | Limit gatherings only to the essential | 2.5 | 3 |
| 14 | Maintain social distance (ie, 2 m) in public areas | 2.0 | 2 |
| 15 | Avoid contact with individuals at high risk for severe illnesses (eg, elders) | 2.5 | 3 |
| 16 | Keep up with the latest information and recommendations from health authorities | 2.4 | 3 |
| 17 | Follow the government’s physical/social-distancing (stay-home) orders/requests | 2.6 | 3 |
| Total | 41.4 | 42 | |
| Mental health effects | Mean | Median | |
| 1 | Have stress and/or symptoms of depression due to following social-distancing (stay-home) orders | 1.8 | 2 |
| 2 | Feel alienated from society | 1.3 | 1 |
| Total | 3.1 | 3 | |
Always, 3; Often, 2; Sometimes, 1; Never, 0.
The first and second authors created the questions using Kamenidou et al.’s 24 questions and the Japanese government’s recommendations for COVID-19 safety protocols 25 as the basis. The authors then approved and confirmed the questions’ validity. For both domains, participants were asked to select one answer on a scale of 0 to 3 (3 = Always, 2 = Often, 1 = Sometimes, and 0 = Never) per question. The total score for preventive health behaviors ranged from 0 to 51, with higher scores indicating higher levels of the behaviors. The total score for mental health effects ranged from 0 to 6, with higher scores indicating more adverse effects.
Sample Size and Power
Researchers calculated sample size with G-Power 3.1 26 and found that 314 participants were necessary for an effect size of 0.2, an alpha level of 0.05 (2 tails), and a power of 0.95 with correlation. With an assumed response rate of 40% and missing data of 20%, at least 1,000 participants were required to be invited.
Analysis
Analysis was conducted using SPSS version 27 (IBM, 2020) and AMOS version 26 (IBM, 2019). Distributions of all data were checked, and the Shapiro–Wilk test was used to test the normality of the perceived control and self-efficacy, perceived health competence, and health behavior (ie, preventative health behaviors and mental health effect) scales. Although all the scales were not normally distributed (P < 0.001), the Q-Q plot did not indicate a great deviation from normality. Both parametric and non-parametric methods were applied, and linear regression rather than logistic regression was found to have better statistical power and model fit. Therefore, researchers used the parametric method, and residuals were checked using linear regression.
Cronbach’s alpha was used to test the reliability of the 3 scales. Missing data inputs were not substituted by any value but were treated as missing.
Participant characteristics among the 3 universities were compared using a chi-square test for nominal variables such as gender and students’ personal incomes of less than 1 million yen (approximately 9,000 US dollars [USD]). The Kruskal–Wallis test was used for ordinal variables such as work hours per week, and analysis of variance (ANOVA) was used for continuous variables such as age, body mass index, and hours of sleep per day.
Factors associated with each scale were analyzed using ANOVA among the 3 universities, t-tests between 2 opposing answers (eg, gender, have or do not have religious affiliations, live alone or with somebody, single or married/partnered, smoker or non-smoker, have or do not have at least one chronic disease), and Pearson’s correlation coefficients among ordinal and interval variables (eg, age, school year, sleep hours, frequency of alcohol intake, work hours per week, family and personal incomes, and body mass index). Factors associated with the scales were selected from the above-mentioned bivariate analyses (P < 0.05) and entered into each linear regression. The normality of residuals was confirmed by the Durbin-Watson ratio (between 1.5 and 2.5). 27 Multicollinearity was checked via the variance inflation factor (<5.0), and model fit was checked via adjusted R2 (variance accounts for).
Finally, structural equation modeling was used to analyze the association among variables based on these bivariate analyses and linear regressions. Model fit was checked via a chi-square test (P > 0.05) and comparative fit index (>0.97).28,29 AMOS automatically estimated mean and intercepts for missing values. 30
Ethical Considerations
This study was conducted with approval from the institutional review board of the 3 universities (approval no. M2020-166 at Tokyo Medical and Dental University). Researchers explained to participants that participation was voluntary, their answers would not affect or be used against them or their grades, and they were not required to answer all of the demographic questions, though questions for the perceived control and self-efficacy, perceived health competence, and health behavior scales were mandatory. Additionally, the survey was conducted anonymously and did not collect identifiers such as names or students’ school identification numbers. To thank participants for their time, 500-yen (4.50-USD) Amazon gift cards were sent to every participant who completed the survey and provided their email addresses. These email addresses were collected through a separate Google Form that was not connected to the survey form.
Results
Participants’ Characteristics
A total of 557 students participated in the survey, with an overall response rate of 52.8%. Though some demographic data was missing, all participants’ data was used for analysis.
Table 2 summarizes the participants’ characteristics. All participants were of Japanese ethnicity and ranged in age from 18 to 36 years old (average 20.4±1.7). The majority was female (96.1%) and identified as having no religious affiliations (80.1%). Compared to those attending Universities B and C, more students attending University A lived alone (χ2 = 15.6, P < 0.001), worked longer hours (H = 14.0, P = 0.001), and had lower body mass indexes (F = 5.1, P = 0.006). There were no differences in age (F = 1.4, P = 0.257), hours of sleep per day (F = 0.940, P = 0.589), personal income (χ2 = 2.6, P = 0.272), or alcohol intake (H = 1.3, P = 0.522) among participants from the 3 universities.
Table 2.
Participants’ basic information, N = 557.
| University, n (%) | A | 174 (31.2) |
| B | 171 (30.7) | |
| C | 212 (38.1) | |
| School year, n (%) | 1 (freshman) | 140 (25.1) |
| 2 (sophomore) | 153 (27.5) | |
| 3 (junior) | 129 (23.2) | |
| 4 (senior) | 135 (24.2) | |
| Gender, n (%) | Male | 10 (1.8) |
| Female | 535 (96.1) | |
| Missing | 12 (2.2) | |
| Age (n = 542) | Mean ± SD | 20.4 ± 1.7 |
| Religion, n (%) | Buddhism | 73 (13.1) |
| Shintoism | 5 (0.9) | |
| Christianity | 13 (2.3) | |
| None | 446 (80.1) | |
| Missing | 20 (3.6) | |
| Marital status, n (%) | Single | 523 (93.9) |
| Married | 2 (0.4) | |
| Partnered | 16 (2.9) | |
| Missing | 16 (2.9) | |
| Live with, n (%) | Alone | 93 (16.7) |
| Parent(S) | 428 (76.8) | |
| Others | 28 (5.0) | |
| Missing | 8 (1.4) | |
| Work hours per week, n (%) | None | 222 (39.9) |
| <5 | 54 (9.7) | |
| 5∼<10 | 112 (20.1) | |
| 10∼<20 | 140 (25.1) | |
| 20∼<40 | 20 (3.6) | |
| Missing | 9 (1.6) | |
| Students’ income, n (%) | <1 million | 508 (91.2) |
| (Yen per year) | 1∼<2 million | 15 (2.7) |
| 4∼<5 million | 1 (0.2) | |
| Missing | 33 (5.9) | |
| Family income, n (%) | <2 million | 20 (3.6) |
| 2∼<3 million | 14 (2.5) | |
| 3∼<4 million | 13 (2.3) | |
| 4∼<5 million | 13 (2.3) | |
| 5∼<6 million | 20 (3.6) | |
| 6 million∼ | 183 (32.9) | |
| Missing | 294 (52.8) | |
| Have chronic disease, n (%) | Yes: at least one | 43 (7.7) |
| Hours of sleep/day | Mean ± SD | 6.7 ±1.2 |
| Body mass index (n = 475) | Mean ± SD | 20.1 ±2.5 |
| Smoke, n (%) | Yes | 14 (2.5) |
| Alcohol intake, n (%) | No | 245 (44.0) |
| Less than once/week | 236 (42.4) | |
| Once/week | 40 (7.2) | |
| 2–3 times/week | 30 (5.4) | |
| 4–5 times/week | 5 (0.9) | |
| Every day | 1 (0.2) | |
| Perceived control (total) | Mean ± SD (median) | 31.4 ± 5.0 (31) |
| Domain 1: Community | Mean ± SD (median) | 12.3 ± 3.2 (12) |
| Domain 2: Political | Mean ± SD (median) | 13.1 ± 2.3 (13) |
| Domain 3: Personal | Mean ± SD (median) | 6.0 ± 1.6 (6) |
| Perceived health competence | Mean ± SD (median) | 28.0 ± 5.6 (28) |
Table 1 summarizes the mean and median score of each item for the health behavior questions. Regarding preventative health behaviors, “wear a mask in public” had the highest score, with 99.1% of participants reporting they always did so; additionally, 93.5% reported that they always “follow respiratory hygiene recommendations.” In comparison, “clean and disinfect shared objects and surfaces,” “clean and disinfect packaged products,” “limit usage of public transportation only to the essential,” and “maintain social distance in public areas” all scored lower. Regarding mental health effects, 68.5% of participants stated they always or often “have stress and/or symptoms of depression due to following social-distancing (stay-home) orders” and 43.0% stated they always or often “feel alienated from society.”
Reliability of Scores
Cronbach’s alpha of the total score of the perceived control and self-efficacy scale was 0.706, perceived health competence scale was 0.832, preventive health behavior scale was 0.814, and mental health effect scale was 0.709. All meet or exceed acceptable levels.
Relationship Between Perceived Control and Preventive Health Behaviors
Table 3 shows factors related to preventive health behaviors in linear regression. After perceived health competence and other factors were adjusted, higher perceived control was significantly associated with higher preventive health behavior scores (β = 0.175, P < 0.001). Adjusted R2 indicated that perceived control accounted for 2.9% of variance. The Durbin–Watson ratio (1.922) indicated that the residuals of this model were normally distributed. Since age and school year were highly correlated (r = 0.668, P < 0.001), age was selected for the analysis.
Table 3.
Relationship between perceived control and preventative health behaviors.
| β | B (95% CI) | P value | VIF | |
| Perceived control | 0.175 | 0.195 (0.102 to 0.288) | <0.001 | 1.123 |
| University B | 0.199 | 2.455 (1.300 to 3.610) | <0.001 | 1.414 |
| University C | 0.181 | 2.118 (1.016 to 3.219) | <0.001 | 1.429 |
| Age | 0.037 | 0.123 (−0.182 to 0.428) | 0.428 | 1.318 |
| Perceived health competence | 0.162 | 0.163 (0.079 to 0.246) | <0.001 | 1.108 |
| Drink alcohol | −0.038 | −0.245 (−0.781 to 0.291) | 0.370 | 1.139 |
| Students’ income >1 million yen/year | −0.116 | −3.900 (−6.647 to −1.153) | 0.005 | 1.065 |
| Work hours (part-time)/week | −0.196 | −0.834 (−1.201 to −0.468) | <0.001 | 1.197 |
| Sleep hours | 0.112 | 0.538 (0.152 to 0.924) | 0.006 | 1.045 |
Linear regression: Adjusted R2 = 0.167 (perceived control accounted for 0.029).
Durbin–Watson ratio = 1.922.
CI: confidence interval; VIF: variance inflation factor.
Relationship Between Perceived Control and Mental Health Effects
In the linear regression, higher preventive health behaviors were associated with higher mental health effects (ie, more adverse mental condition) (β = −0.182, P < 0.001, adjusted R2 = 0.013), and higher perceived health competence were associated with lower mental health effects (ie, less adverse mental condition) (β = −0.255, P < 0.001, adjusted R2 = 0.051). After perceived health competence and preventive health behaviors were adjusted, perceived control was not significantly associated with mental health effects (β = −0.055, P = 0.190, adjusted R2 = 0.005); however, perceived control was significantly and negatively related to mental health effects (β = −0.104, P = 0.015) when perceived health competence was excluded from the model. Perceived control was not significantly related to mental health effects (β = −0.080, P = 0.061) when preventive health behaviors were also excluded from the model.
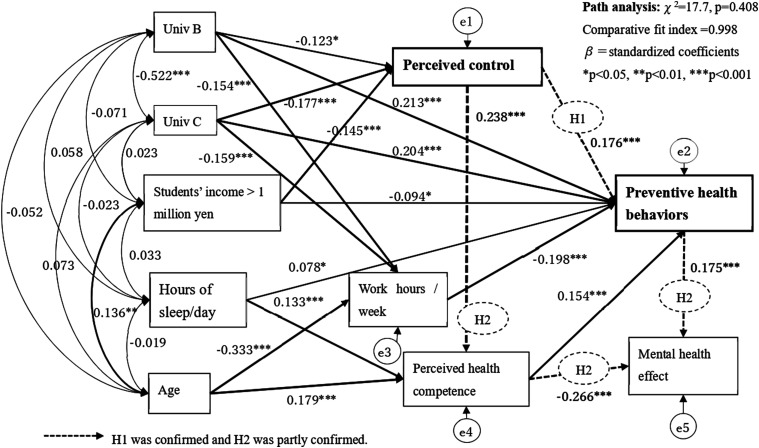
Factors Related to Preventive Health Behaviors
Figure 2 summarizes the association among variables under structural equation modeling. The model fit was robust (χ2 = 17.7, P = 0.408; comparative fit index = 0.998). Higher perceived control was significantly related to higher preventive health behaviors (β = 0.176, P < 0.001), which were significantly associated with higher mental health effects (β = 0.175, P < 0.001). However, perceived control was also positively related to perceived health competence (β = 0.238, P < 0.001), which connected to both higher preventive health behaviors (β = 0.154, P < 0.001) and lower mental health effects (β = −0.266, P < 0.001).
Figure 2.
Factors Related to Perceived Control and Preventative Health Behaviors in Japanese Nursing Students under the COVID-19 Pandemic.
Factors related to higher perceived control were attendance at University A compared to Universities B (β = −0.123, P = 0.012) and C (β = −0.177, P < 0.001) and lower personal incomes (β = −0.145, P < 0.001). Factors related to higher preventive health behaviors were attendance at Universities B (β = 0.213, P < 0.001) and C (β = 0.204, P < 0.001) compared to University A, lower personal incomes (β = −0.094, P = 0.020), longer hours of sleep per day (β = 0.078, P = 0.047), and shorter work hours per week (β = −0.198, P < 0.001).
Results showed that students attending University A had much longer work hours per week compared to those attending Universities B and C. Additionally, older age was related to higher personal incomes but shorter work hours and higher perceived health competence. There was no significant association between personal income, work hours, and sleep hours.
Discussion
This study found that higher levels of perceived control are associated with higher levels of preventative health behaviors among undergraduate nursing students and also that those behaviors do affect mental health. Although perceived control was not directly related to mental health effects, it was related to perceived health competence, which was associated with lower mental health effects (ie, improved mental conditions).
Factors related to higher perceived control were attendance at University A and lower personal incomes. Factors related to higher preventative health behaviors included higher perceived health competence, longer hours of sleep per day, lower personal income, shorter work hours, and attendance at Universities B and C.
H1: Nursing Students With Higher Perceived Control Practice Higher Levels of Preventive Health Behaviors
As shown in Figure 2 (see H1), results confirmed that perceived control is positively related to preventive health behaviors. This study used a control scale related to social capital, including 3 domains of control over community, political affairs, and satisfaction with one’s personal life, but any item related to control over health affairs was not included. Since preventing infection is closely intertwined with government policies and strategies, students who are aware of those policies or are politically active may have higher preventive behaviors. Although previous studies have shown that Japanese people have lower levels of perceived control than people in any other countries,31,32 this study found that students’ perceived control was comparable with that of Salehi et al.’s 18 participants of young Iranian women.
H2: Higher Perceived Control Buffers the Effects That Preventive Health Behaviors Have on Mental Health
The second hypothesis was partially confirmed. Although higher perceived control related to lower mental health effects, perceived health competence had even stronger associations to mental health. That is, perceived control was significantly related to higher perceived health competence, which, in turn, was associated with lower mental effects. This is illustrated in Figure 2’s path of H2.
While higher levels of preventive health behaviors may lead to feeling depressed or isolated, adjusted R2 indicated that the value was not so high (1.3%), meaning students with higher perceived control may have higher preventive health behaviors but the perceived control may act to buffer adverse mental health effects. As such, this study agrees with previous works 13 : Enhancing perceived control may be a promising way to improve individuals’ mental health during the COVID-19 pandemic. 33
Other Factors Related to Preventive Health Behaviors
Students who work longer hours and have higher personal income reported lower preventive health behaviors because they likely have difficulty maintaining strict social distances and limiting their use of public transportation. Longer hours of sleep per day were associated with both higher preventive health behaviors and better health competence, which agreed to the study reported that nursing students who slept well had better health behaviors. 22 Since no association was found between hours of sleep and work, work hours were not found to prevent students from sleeping.
Preventive health behaviors were significantly different among students attending the 3 universities, which is in line with results that the variations between universities are caused by differences in strategies, frequencies of educational campaigns, and efforts to increase students’ awareness of COVID-19. 7 This study found that, though students attending University A had higher perceived control, they worked longer hours and practiced lower levels of preventive health behaviors. Even after work hours and other factors were adjusted, the university of attendance had the highest effect on preventive behaviors (β > 0.2). All of University B’s students are required to stay in their dormitories during the first year of school and receive thorough information on self-care, health, and daily living throughout the school year. These students also received strict instructions regarding infection prevention during the pandemic. These strict instructions, however, could lead to high preventive health behaviors but low self-control.
Other factors such as religion, living situation, and marital status did not influence preventive health behaviors. Since the university plays a decisive role in students’ preventive behaviors, conducting effective education campaigns and offering financial support are critical in preventing the spread of infection while protecting students’ mental health.
Older age was also associated with higher preventive health behaviors, which aligns with previous studies.6,7,34 In this study, age was not directly related to health behaviors; however, senior students had higher perceived health competence and fewer hours of part-time work, which lead to higher preventive health behaviors. Since coursework intensifies as nursing programs progress, senior students are likely to concentrate on their studies rather than paid work.
Gender and chronic disease were not related to perceived control or preventative health behaviors since the proportions of male students and students with chronic conditions were too small (1.8% and 7.7%, respectively) to detect any differences in the study.
Conclusions
This study is the first to find that higher perceived control is associated with higher levels of preventative health behaviors among nursing students. Although perceived control was not directly related to mental health effects, it informed perceived health competence, which mitigated mental health effects caused by the preventative health behaviors of Japanese nursing students during the COVID-19 pandemic. Factors that influenced preventive health behaviors were perceived health competence, hours of sleep per day, personal income, work hours, and the university of attendance.
Practical Implications
This study suggests that students who are younger with low perceived control, low health competence, longer hours of work, and shorter hours of sleep per day may practice lower levels of preventive health behaviors and suffer higher mental health effects under the pandemic. Behavioral interventions to support such students should focus on instilling control beliefs as well as skills and preventative behaviors. 15 Since perceived control improves as uncertainty decreases, public communication regarding the pandemic is important. 13 Universities are recommended to provide students with information sources regarding COVID-19 and safety tactics, and, in turn, students are encouraged to maintain awareness and understanding of social and political issues so they may effectively prevent infection without increasing their mental burden.
Furthermore, developing effective interventions that take sociodemographic factors, personality traits, and beliefs into account can help promote control beliefs and related outcomes. 15 Nursing faculty may be able to monitor and support each student, especially those who are younger, work longer hours, and are only able to get limited hours of sleep. In this sense, governmental and/or university-funded financial support is essential in helping students to work less and reduce their chances of being exposed. It is also necessary to investigate if this type of support can enhance students’ perceived control and preventative health behaviors.
Limitations and Future Studies
Since this study investigated nursing students attending programs in an urban area, the result may not wholly represent students living in rural areas or attending vocational nursing schools. This study may also have participation bias since students who strictly practice preventative health behaviors may have participated more than those who do not. And, since the study collected data through self-administered questionnaires, the accuracy of student responses is unverified, and there were some missing demographic data inputs.
Finally, the students’ university of attendance was the only variable under the influence of public policy, community, and organizational factors. A nationwide survey that includes not only university-level but also prefecture- and city-level variables, as well as international comparisons, is necessary. Because this is a cross-sectional study, causal relationships among the variables could not be proven. In an intervention study, educational programs that could enhance perceived control and evaluate its effects on preventive health behaviors must be developed.
Footnotes
Author contributions: Akiko Kondo: Conceptualization, methodology, formal analysis, investigation, data curation, writing—original draft, visualization, and Funding acquisition. Renaguli Abuliezi: Methodology, investigation, and data curation. Kazuko Naruse: Conceptualization, methodology, investigation, and data curation. Tomomi Oki: Investigation and data curation. Kosuke Niitsu: Methodology. Mabel C Ezeonwu: Conceptualization and writing—review and English editing. All authors critically reviewed and approved the final manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: This work was supported by the scientific research fund, Japan Society for the Promotion of Science (19K10794). The founder had no involvement in any of the study processes and submission of the article for publication.
ORCID iD
Akiko Kondo https://orcid.org/0000-0003-2817-9623
References
- 1.World Health Organization . WHO Coronavirus (COVID-19) Dashboard. WHO; 2021. https://covid19.who.int/. https://covid19.who.int/. Accessed October 16, 2021. [Google Scholar]
- 2.World Health Organization . WHO Coronavirus (COVID-19) Dashboard. WHO; 2021. https://covid19.who.int/. https://covid19.who.int/. Accessed July 27, 2021. [Google Scholar]
- 3.Spencer J, Jewett C. Twelve Months of Trauma: More than 3,600 US Health Workers Died in Covid’s First Year. Kaiser Health News; 2021. https://www.theguardian.com/us-news/2021/apr/08/us-health-workers-deaths-covid-lost-on-the-frontline. Accessed May 1st, 2021. [Google Scholar]
- 4.Nie S, Sun C, Wang L, Wang X. The professional identity of nursing students and their intention to leave the nursing profession during the coronavirus disease (COVID-19) pandemic. J Nurs Res. 2021;29(2):e139. [DOI] [PubMed] [Google Scholar]
- 5.Sun Y, Wang D, Han Z, Gao J, Zhu S, Zhang H. Disease prevention knowledge, anxiety, and professional identity during COVID-19 pandemic in nursing students in Zhengzhou, China. J Korean Acad Nurs. 2020;50(4):533-540. [DOI] [PubMed] [Google Scholar]
- 6.Yuan T, Liu H, Li XD, Liu HR. Factors affecting infection control behaviors to prevent COVID-19: An online survey of nursing students in Anhui, China in March and April 2020. Med Sci Monint. 2020;26:e925877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Albaqawi HM, Alquwez N, Balay-Odao E, Bajet JB, Alabdulaziz H, Alsolami F, et al. Nursing students' perceptions, knowledge, and preventive behaviors toward COVID-19: A multi-university study. Front Public Health. 2020;8:573390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Glanz K, Rimer BK, Viswanath K. Health Behavior and Health Education: Theory, Research, and Practice. JOSSEY-BASS A Wiley Imprint; 2008. [Google Scholar]
- 9.Tsai FJ, Hu YJ, Chen CY, Tseng CC, Yeh GL, Cheng JF. Using the health belief model to explore nursing students' relationships between COVID-19 knowledge, health beliefs, cues to action, self-efficacy, and behavioral intention. Medicine. 2021;100(11):e25210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith MS, Wallston KA, Smith CA. The development and validation of the perceived health competence scale. Health Educ Res. 1995;10(1):51-64. [DOI] [PubMed] [Google Scholar]
- 11.Villarreal B, Heckhausen J. Control striving and Control perception in a life span developmental framework. In: Reich JW, Infurna FJ, eds. Perceived control Theory, Research and Practice in the First 50 years: United States of America: Oxford University Press; 2017:253-279. [Google Scholar]
- 12.Goodwin R, Wiwattanapantuwong J, Tuicomepee A, Suttiwan P, Watakakosol R, Ben-Ezra M. Anxiety, perceived control and pandemic behaviour in Thailand during COVID-19: Results from a national survey. J Psychiatr Res. 2021;135:212-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zheng L, Miao M, Gan Y. Perceived control buffers the effects of the COVID‐19 pandemic on general health and life satisfaction: The mediating role of psychological distance. Appl Psychol Health Well-Being. 2020;12(4):1095-1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Caci B, Miceli S, Scrima F, Cardaci M. Neuroticism and Fear of COVID-19. The interplay between boredom, fantasy engagement, and perceived control over time. Front Psychol. 2020;11:574393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Robinson SA, Lachman ME. Perceived control and behavior change -A personalized approach. In: Reich JW, Infurna FJ, eds. Perceived control Theory, Research and Practice in the First 50 years. United States of America: Oxford University Press; 2017:201-227. [Google Scholar]
- 16.e-Source Behavioral & Social Sciences Research . Social and Behavioral Theories. e-Source Behavioral & Social Sciences Research; 2012. https://obssr.od.nih.gov/wp-content/uploads/2016/05/Social-and-Behavioral-Theories.pdf. Accessed May 3rd, 2021. [Google Scholar]
- 17.Foxton F, Jones R. Social Capital Indicators Review. In: Pisani E, Franceschetti G, Secco L, Christoforou A, eds. Office for National Statistics. Springer; 2017:UK2011. [Google Scholar]
- 18.Salehi A, Harris N, Coyne E, Sebar B. Perceived control and self-efficacy, subjective well-being and lifestyle behaviours in young Iranian women. J Health Psychol. 2016;21(7):1415-1425. [DOI] [PubMed] [Google Scholar]
- 19.Baer HJ, Glynn RJ, Hu FB, Hankinson SE, Willett WC, Colditz GA, et al. Risk factors for mortality in the nurses' health study: a competing risks analysis. Am J Epidemiol. 2011;173(3):319-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Okamoto S. A study on consciousness of health among nursing students. Jpn J Nurs Res. 2006;16(1):75-82. (in Japanese). [Google Scholar]
- 21.Murray CJL. The state of US health, 1990-2010. J Am Med Assoc. 2013;310(6):591-608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fujita C. Research on nursing students' health behavior, mental status and lifestyle. J Jpn Nurs Assoc. 2016;46:99-102. (in Japanese). [Google Scholar]
- 23.Togari T, Ikezaki S, Yamazaki Y, Ito M, Zenko A, Taguchi R. The development of perceived health competence scale (PHCS) Japanese version. Jpn J Health Hum Ecol. 2004;70(5):184-195. [Google Scholar]
- 24.Kamenidou IE, Stavrianea A, Liava C. Achieving a Covid-19 free country: Citizens preventive measures and communication pathways. Int J Environ Res Publ Health. 2020;17(13):4633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ministry of Health Labour and Welfare . Novel Coronavirus (COVID-19). Ministry of Health Labour and Welfare; 2021. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000164708_00079.html. Accessed May 3rd, 2021. [Google Scholar]
- 26.Heinrich Heine University of Dusseldorf . G*Power: Statistical Power Analyses for Windows and Mac. Heinrich Heine University of Dusseldorf; 2020. http://www.gpower.hhu.de/en.html. [Google Scholar]
- 27.Karadimitriou SM, Marshall E. Stats tutor: Outliers, Durbin-Watson and interactions for regression in SPSS. SPSS; 2021. https://www.sheffield.ac.uk/polopoly_fs/1.531431!/file/MASHRegression_Further_SPSS.pdf. Accessed May 3rd, 2021. [Google Scholar]
- 28.Schermelleh-Engel K, Moosbrugger H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Psychol Methods Res. 2003;18(2):23-74. [Google Scholar]
- 29.Wuensch KL. Conducting a Path Analysis With SPSS/AMOS. SPSS; 2017. http://core.ecu.edu/psyc/wuenschk/MV/SEM/Path-SPSS-AMOS.pdf. [Google Scholar]
- 30.Amos TM . Estimation With Missing Values Application. Amos TM; 2021. http://www.spss.com.hk/amos/missing_values_application.htm. Accessed June 27, 2021. [Google Scholar]
- 31.Hornsey MJ, Greenaway KH, Harris EA, Bain PG. Exploring cultural differences in the extent to which people perceive and desire control. Pers Soc Psychol Bull. 2019;45(1):81-92. [DOI] [PubMed] [Google Scholar]
- 32.Kondo A, Eckhardt AL, Abuliezi R, Oki T, Otaki A. A pilot study on perceived control and health related quality of life in patients with acute coronary syndrome in Japan and the United States. J Jpn Soc Int Nurs. 2021;4(2):35-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li JB, Yang A, Dou K, Cheung RYM. Self-control moderates the association between perceived severity of coronavirus disease 2019 (COVID-19) and mental health problems among the Chinese public. Int J Environ Res Publ Health. 2020;17(13):4820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Somma A, Gialdi G, Frau C, Barranca M, Fossati A. COVID-19 pandemic preventive behaviors and causal beliefs among Italian community dwelling adults. J Health Psychol. 2020;1359105320962243. [DOI] [PubMed] [Google Scholar]