Abstract
For respiratory infections treatment and prevention, we analyze for the first time the possibility of providing a broad range medication based on metallic nanoparticles colloids (NpC) delivery by controlled aerosol inhalation. (i) Based on in-vitro data combined with aerosol deposition characteristics in the respiratory system, we calculate the required effective formulations, dosages and delivery parameters for an aerosol inhalation treatment. The goal is to achieve an effective NpC inhibitory concentration (IC) in the target airway surface liquid (ASL); (ii) We evaluate the clinical safety of such dosages, drawing on information from animal testing data and regulatory limits in the USA for such nanoparticles aerosol inhalation safety. Our analysis indicates a wide range of potentially safe and effective dosages that can be clinically explored, targeting the upper respiratory and bronchial tree system. Similar dosages can also provide antibacterial effectiveness for prophylactic treatment in hospital intensive care units to lower the risk of ventilator-associated pneumonia (VAP).
Our calculations are phenomenological, independent of mechanisms. Nevertheless, we highlight a mechanism of action by which any suitably designed NpC, with nanoparticles sized 2–10 nm and having a large negative zeta-potential, preferentially bind to viruses with predominantly positively-charged spike proteins. These will be ineffective against viruses with predominantly negatively-charged spike proteins. Accordingly, the popular silver metal base for NpC serves just as a construction ingredient, and other metal or metal-oxides which can serve to construct the noted nanoparticle properties would be similarly effective.
We suggest that inhalation delivery of the proposed antiviral formulations could be applied as a first-line intervention while respiratory infections are primarily localized to the upper respiratory system and bronchial tree.
Keywords: Covid-19, Nanomedicine, Pneumonia, VAP, Respiratory infections, Viruses
Introduction
Whether it is the seasonal flu, a sore throat, or early-stage Covid-19 symptoms, presently in the 21st century, there is still no home treatment medication that is easily accessible and available in pharmacies worldwide. The impact of this sorry state of medicine amounted to a global disaster under Covid-19. Moreover, even in the absence of novel epidemics, each year the morbidity and economic cost of respiratory infections are huge. The typical research tendency in novel pharmaceuticals is to develop sophisticated, expensive, patent-protected, highly potent medications for severely ill patients. In contrast, when it comes to public health and pandemic prevention, it may be more impactful to develop a broad-range, mild, cheap, and easily accessible early-stage medications for home treatment, with low risk of side effects and wide availability potential, to prevent deterioration mild patients at home to the severe hospitalized state. From the pitiful present venture point of anti-viral respiratory infections medication, there may be a benefit, humbly and open-mindedly, to revisit some neglected potential options for advancement.
We argue that good candidates for such desired medication can be found in a well-defined formulation of nanoparticle colloids for inhalation delivery. The antibacterial and antiviral potential of nanoparticle colloids)NpC(has been extensively demonstrated in in-vitro and animal testing [1], [2], [3], [4], [5], [6]. Anti-microbial applications of NpC for wound care are approved by the FDA. Unfortunately, a senseless and uncontrolled “alternative medicine” practice of “colloidal silver” ingestion led the pharmacological and academic establishment to widely disregard the potential application of metal-based NpC as antimicrobial agents in contexts other than wound care. In particular, there has been no rigorous analysis of the potential use of inhalation-delivered NpC to prevent or treat respiratory infections.
We substantiate the potential of antimicrobial NpC formulations, delivered by inhalation, to minimize the aggravation of respiratory system infections. We evaluate both (A) viral respiratory infections (including with SARS-CoV-2, the causative agent of COVID-19), and (B) bacterial infections, particularly ventilator-associated pneumonia (VAP) in intensive care unit (ICU) patients. Indeed, the most reliable experience concerning the treatment of respiratory infections has been gained in the context ICU-acquired VAP [7]. There are unique factors to consider for optimal treatment of the lungs. These include aerosol characteristics, breathing patterns, geometrical factors (lung morphology), disease state, pharmacokinetics (including lung clearance and mucus transport). Both the total pulmonary drug dose and the regional deposition distribution of the lung-deposited aerosol are critical factors for the clinical success of an inhalation therapy [8].
The pathogenesis of respiratory infections begins mildly in the nasopharynx or upper bronchial tree portions of the respiratory system [9], [10]. Aggravation occurs once the pathogens and associated inflammation migrate to lower portions of the respiratory system [11]. Greater risk and aggravation of the disease state are associated with an increased microbial load in the upper bronchial tree. Hence, a desirable clinical endpoint for the proposed inhaled NpC treatment is the inhibition of microbial load in the upper sections of the bronchial tree. Such an endpoint implies treatment when most patients are still at home with mild symptoms.
We lay the groundwork for future clinical evaluations of inhaled NpC by determining: (i) the NpC material composition required for effective antiviral activity; (ii) the effective inhibitory concentration (IC) required in target respiratory tissues; (iii) the dosage required for practical inhalation delivery of metal-based NpC antiviral and antibacterial formulations, and (iv) the safe dosage range for clinical evaluation.
Conceptual approach
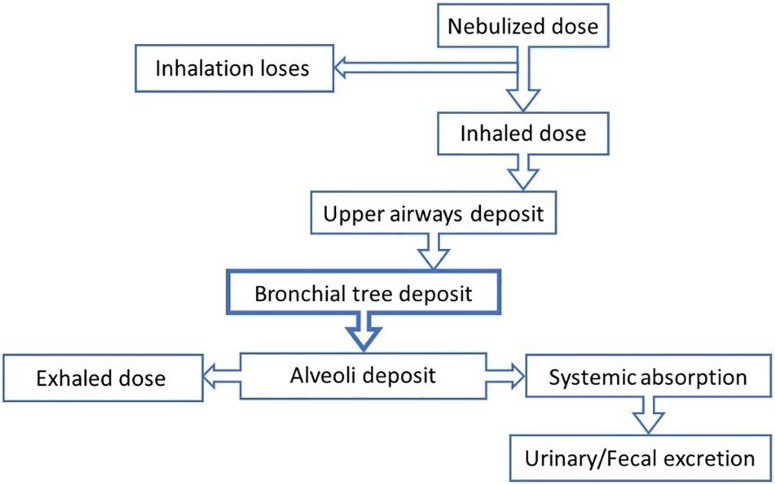
We follow the principles of antibiotics inhalation delivery [7], [12], as illustrated in Fig. 1 . To calculate the dose delivered externally with an aerosol nebulizer, one needs to consider the various losses that occur on route to the target bronchial tree organ and sensitivity to the aerosol properties that determine the deposition fraction.
Fig. 1.
Mechanisms by which the dose of an antimicrobial agent inserted into a nebulizer differs from the dose delivered to the target airway location (based on [7]), with a focus on the fraction deposited in the bronchial tree.
Our dose calculation is based on the following results (each one derived in dedicated sections):
-
•
Nanoparticles: The antiviral potency of metal nanoparticles is highly size-dependent, with optimal size being in the range of 3–7 nm. Polymer capping agents (PVP, PVA) reduce the antiviral effectiveness of NpC and better be avoided.
-
•
Inhibitory concentration (IC): The target organ is the airway surface liquid (ASL). For antiviral applications, the nanoparticles minimal microbicidal IC (MMC) is about 10 µg/mL.
-
•
Tissue deposition fraction (TDF): During oral breathing of 5 µm aerosol droplets, NpC deposit onto the pharynx (30%), bronchial tree (30%), and alveoli (25%).
-
•
Inhalation timing losses (ITL): inhalation duration is about a third of the breathing cycle. Thus, using a continuous aerosol source, the aerosol uncontrollably cumulates in the oral cavity during 2/3 of the breathing cycle. Hence, we assume only about 50% of the nebulized substance is actually inhaled.
The required delivery dose is calculated by cumulating the effects of each stage between the aerosolizing nebulizer device and final target tissue deposition and dilution into the local airway liquid. The mass (µg) of nanoparticles deposited to the target organ location (e.g., bronchial tree) is distributed into a liquid volume comprising the tissue airway surface liquid (ASL) plus the deposited solution liquid volume. Equation-(1) delineates the calculation of required NpC aerosolized dose (AD) volume that needs to be put into the nebulizer device to achieve the desired NpC inhibitory concentration (IC) in the target organ location:
| (1) |
where AD (in mL) is a function of the target inhibitory concentration (IC, in µg/mL), mucosal volume (MV, in mL), tissue deposition fraction (TDF), inhalation time losses fraction (ITL), and colloid concentration (CC, in µg/mL).
Results and analysis
Table 1 illustrates examples antiviral formulations delivered by the oral inhalation of aerosol droplets, as calculated from the above Equation-1. Using a typical continuous nebulizer (ITL = 0.5 assumed) with 5 µm droplets size, a nebulized dose of 4 mL is required to effectively deposit the IC of 40 µg/mL in the bronchial tree. Inhaled antibiotics dosages for chronic airway infections are commonly 2–5 mL [13]. Hence, we expect inhalation of nebulized similar size dosage of antiviral solutions to be well-tolerated by home users. For preferential deposition in the alveoli, smaller aerosol droplets of size 3 µm are required (see discussion in section 3.6.2).
Table 1.
Dose calculations for aerosol droplets of various sizes to treat different target tissues.
| Target tissue | Droplet size (µm) | IC In target tissue (µg/mL) | MV Mucosal Volume (mL) | TDF Tissue Deposit Fraction | CC Colloid Concentration (µg/mL) | Inhaled dose (mL) | AD Aerosolized Dose (mL) | |
|---|---|---|---|---|---|---|---|---|
| (i) | Bronchial tree | 5 | 10 | 1 | 0.25 | 50 | 1 | 2 |
| (ii) | Bronchial tree | 5 | 40 | 1 | 0.25 | 120 | 2 | 4 |
| (iii) | Bronchial tree | 3 | 25 | 1 | 0.1 | 120 | 2.75 | 5.5 |
| (iv) | Alveoli | 3 | 10 | 10 | 0.33 | 120 | 2.75 | 5.5 |
As common in the practice of antibiotic inhalation treatments, a target IC inhaled antimicrobial dose should be some significant multiple of the theoretical minimum IC (MIC) and also the minimum bactericidal concentration (MBC). Since the antiviral minimum mucrobicidal concentration (MMC) for NpC is about 10 µg/mL, a recommended treatment target IC may be 40 µg/mL, as illustrated in example (ii) in table-1, for targeting the bronchial tree.
Target IC determination for antiviral applications
Antiviral effect is obtained only by nanoparticle of size < 10 nm (see section 3.2 below). The capping molecule used for the manufacture of nanoparticle affects antiviral potency. The popular PVP cap appears to inhibit antiviral effectiveness significantly. Therefore, in analyzing the published data, we limit our consideration to experiments involving nanoparticles of size < 15 nm and to non-PVP-stabilized NpC. The minimum inhibitory concentration (MIC) is one at which occurs transition from microbial no-growth to growth. The Minimum Microbicidal Concentration (MMC) is the least amount of antibiotic required to kill a microbial organism (e.g., a 50% reduction after 1 h incubation), where always MIC < MMC. In practice, published data is given at a few discrete concentration points, from which the MIC or MMC needs to be deduced somehow by interpolation and often not stated by the authors themselves (see an example below for the TGEV coronavirus). The evidence summarized in Table-2 indicates that an IC of at least 10 µg/mL is desirable at the target respiratory system location. We contend that the optimal size of nanoparticles for antiviral effectiveness is 3–7 nm, not the 10 nm diameter used in all the referenced experiments. Hence, there is potential for better efficacy and lower MIC if an optimal NpC are used.
Relation to the mechanism of action
Our core calculations are phenomenological, independent of mechanisms. Yet, an understanding of mechanisms may guide future treatment optimization and alternatives. There are multiple ways for bacteria to interact with silver NpC components (both the nanoparticles and Ag+ ions), as discussed by others [18]. Viruses are simpler. Based on the broad-range effectiveness of silver NpC with diverse capping surface molecules against many different viruses, we argue that the underlying mechanism of action of NpC on viruses must be non-specific, simple, and robust. The prominent material properties that affect the NpC antiviral binding action are the nanoparticle size and surface electric zeta potential, with all remaining aspects of the chemical composition being secondary. Thus, we estimate that silver is not essential in itself other than as a manufacturing basis for nanoparticles with appropriate physical properties. Other NpC with these properties, such as NpC based on metal-oxides (e.g., zinc oxides, titanium oxides) would be effective as well (Iron is not recommended, since iron promotes bacterial biofilm growth).
Antiviral mechanism of action – Nanoparticle size
The importance of nanoparticle size is much greater for antiviral compared with antibacterial properties, and we contend that this is related to the mechanism of action. The antiviral effect arises predominantly from attachment of nanoparticles to the virus. We posit that antiviral effectiveness is limited to nanoparticles of size < 10 nm. This universality arises from the rather uniform geometric scales of respiratory infections viruses (e.g., influenza and coronavirus), all of which have diameters of about 100 nm, the distance between neighboring spike glycoproteins being 10–20 nm, and glycoprotein length of about 15 nm. Thus, based on geometrical limitations alone, for a nanoparticle to interact effectively with a glycoprotein site, its diameter must be around 10 nm or less. Virus functioning becomes disturbed only when the virus is sufficiently covered by attached nanoparticles [19].
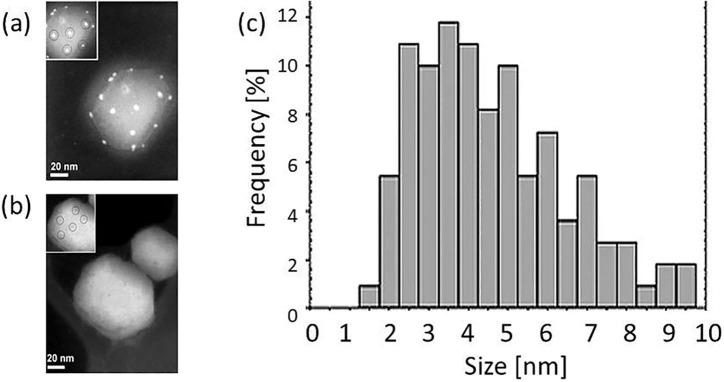
We find supporting evidence for the above argument from experiments and direct imaging of nanoparticles binding to human immunodeficiency virus (HIV) [14], whose size is 120 nm, with ∼ 22 nm spacing between the glycoprotein knobs. Interestingly, the observed sizes of nanoparticles bound to HIV (see Fig. 2 ) are exclusively within 1–10 nm, with peak virus attachment effectiveness for nanoparticle sizes in the range of 3–7 nm. No nanoparticles of diameter greater than 10 nm were observed to interact with the virus, even though about 40% of the overall nanoparticle population in the sample was beyond this size range [14].
Fig. 2.
HIV-1 (a/b) with/without NpC treatment. (c) Size distribution of silver nanoparticles bound to HIV-1 collected from all tested preparations seems to peak at a nanoparticle size of about 4 nm (adapted from [14]).
Consequently, we estimate that experiments in the literature, predominantly performed with larger NpC, have skewed IC values too high, since their effectiveness arises wholly from the margins of the distribution of particles with sizes < 10 nm. The best we can do, with the presently available, is to focus on analyzing published data only from experiments conducted with ∼ 10 nm NpC size. However, there is a need to perform experiments with purposefully produced NpC nanoparticle sizes peak distribution in the range of 3–7 nm.
Antiviral mechanism of action –The electrostatic potential of nanoparticles
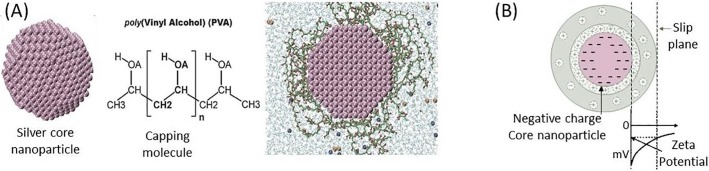
Nanoparticles are composites, having a metal core and an envelope capping material (Fig. 3 ). In a liquid environment, nanoparticles have a surface electric potential, called the zeta potential, the magnitude of which is dependent on solution pH. For a typical silver NpC, the zeta potential is negative.
Fig. 3.
(a) A silver nanocrystal core, the PVA capping, and a full snapshot of an equilibrated PVA-stabilized nanoparticle in aqueous media [21]. (b) The zeta potential of a colloidal nanoparticle is the potential (here negative) at the slip plane surface.
Unlike bacteria, we conjecture that the broad-range antiviral effectiveness of NpC is a consequence of primarily electrostatic interactions. The spike proteins of many human affecting viruses (including influenza and coronaviruses) are positively charged, likely promoting their binding to the predominantly negative surface charge of the host cell receptors (such as ACE2) [20]. Correspondingly, the highly negative surface zeta-potential of the nanoparticles (which is required to keep them in colloidal form) leads the nanoparticles to bind selectively to the spike proteins of viruses and thereby neutralize their receptor binding affinity. Hence, nanoparticles with a zeta potential stronger than − 20 mV or − 30 mV are preferred. The silver as a particular atom is unimportant in itself, other than as a manufacturing method for generating a stable, charged, composite nanoparticle colloid. It follows that any colloid of nanoparticles whose size distribution is predominantly in the 2–10 nm range and that possess a highly negative zeta-potential strength of more than − 20 mV would work as effectively as silver NpC. Correspondingly, viruses whose spike protein binding sites are less positively charged will be less affected by the NpC.
Generally, the chemistry of solutions is such that the zeta potential becomes more negative with increasing pH. Changing pH may even cross the zeta potential between negative and positive values. In humans, normal pH values of the bronchial tree mucus are in the range 6.9–9.0 [22]. Therefore, NpC should preferably have a pH of around 7–7.5 in order that their zeta potential not overly degrade in the mucosal environment.
Coronavirus evidence
Transmissible gastroenteritis virus (TGEV), a porcine coronavirus, causes very high mortality in piglets. Fig. 4 presents the results of testing the effect of NpC on coronavirus TGEV [17]. With nanoparticles of non-optimal size 10–20 nm, tested for 1 h incubation, there is a significant inhibitory (>50% reduction) effect at a 12.5 µg/mL concentration and what seems like near static (no growth) at a 3 µg/mL concentration. Hence we would conclude from this experiment the values of MIC = 3 µg/mL , and MMC = 12 µg/mL.
Fig. 4.
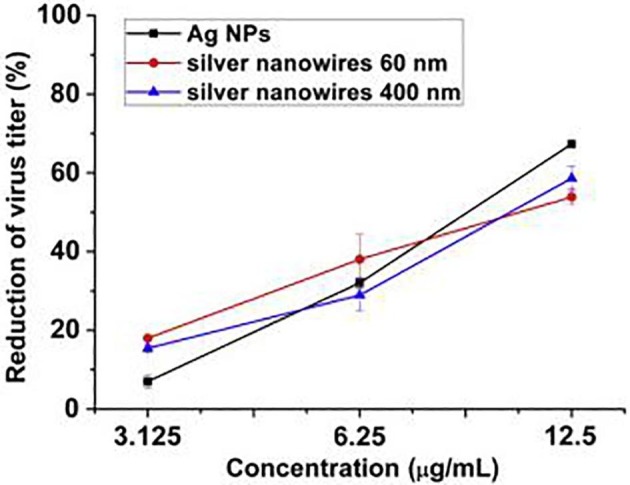
The coronavirus TGEV (MOI 0.5) was incubated with the indicated concentrations of silver-based nanoparticles (AgNP) at 37 °C for 1 h in DMEM. The AgNP were of size < 20 nm (adapted from [17]).
Material properties
Distinguishing ionic vs nanoparticle colloids
It is essential to distinguish between ionic solution (recognized by clear water-like color) and nanoparticle colloids (identified by a visibly yellow-brownish color). Ionic silver solution consists of positively charged silver ions dissolved in water, whereas silver NpC consists of negatively charged nano-sized chunks of elemental silver, size 1–100 nm. Both ionic silver and silver NpC manifest antibacterial properties. In contrast, regarding antiviral properties, it has been argued that colloidal particles are significantly more potent than ionic silver [23].
Significance of selected stabilization coating of the nanoparticles
Prior testing results suggest that the capping agent material can affect antiviral effectiveness. For example, it appears that PVP-capped NpC had practically no antiviral effect on the coronavirus TGEV, whereas a non-PVP NpC exhibited strong antiviral effectiveness [17]. A similar result was obtained for HIV, where a ten-fold greater concentration was needed for a PVP-coated NpC sample to achieve the same antiviral effect as a non-PVP NpC [13]. Overall, it appears that a thinner capping layer may have a less deleterious effect on antiviral potency.
Anti-bacterial applications
For bacterial infections, the literature suggests the presence of a poorly differentiated mixed effect arising from both silver ions and nanoparticles [18]. A major problem in deriving clear numerical conclusions from the published literature is that the IC, commonly stated in weight fraction units (µg/mL), does not take into account the sensitivity to nanoparticle size. For the same weight fraction (µg/mL) the number density (N/mL) of smaller nanoparticles is higher than larger nanoparticles. Since higher number density (number of nanoparticles per volume) increases the probability of nanoparticle–pathogen interactions, we expect smaller nanoparticles to exhibit greater antimicrobial effectiveness for same weight fraction (µg/mL) than larger nanoparticles (as has been manifested experimentally [24]). Confusion arises from published studies using different-sized nanoparticles from one another while expressing the results in weight fraction µg/mL. The variance in the reported outcomes between publications is an artifact of the different nanoparticle sizes used in the various protocols, obscuring the consistency of NpC effects. Considering the antibacterial properties of silver NpC (e.g., on Pseudomonas aeruginosa) [24], the typical IC values (∼7 µg/mL) of small nanoparticles (∼7 nm) are similar to those of the typical antiviral IC, according to our analysis.
Dose calculation
Antimicrobial drugs exhibit concentration-dependent efficacy. Therefore, ensuring an appropriate concentration in the relevant body fluid is essential. For inhaled antimicrobials, the applicable body fluid for drug concentration purposes is the airway surface liquid (ASL) [12], also referred to as epithelial lining fluid (ELF). The delivered dose is deposited on and diluted by the ASL. We argue that dosage planning, correction, and controlled verification can be achieved by examining the trachea or primary bronchi (G1). Deposition models indicate that the trachea and G1 bronchi can serve as lower/upper bounds for all of the concentration estimators for all first 10 generations of the bronchial tree (see Fig. 5 ). Therefore, BAL sampling of tracheal & G1 bronchi NpC concentration is a well-defined and measurable verification method of target IC in the whole bronchial tree organ.
Fig. 5.
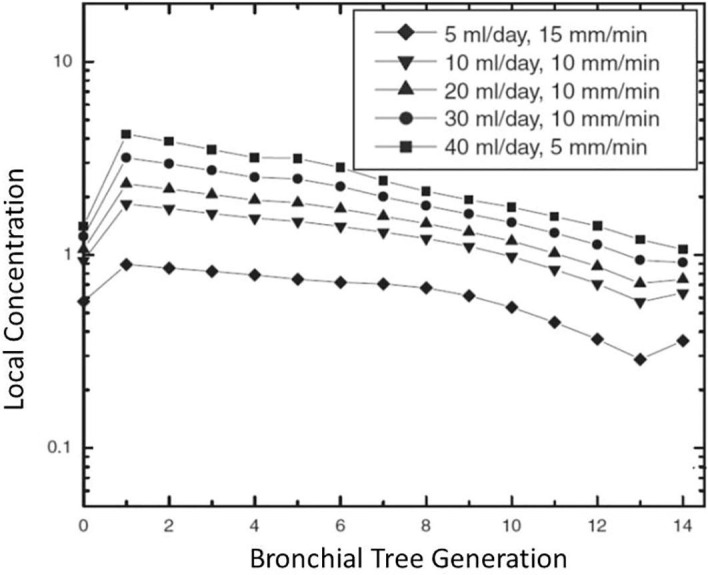
Local concentration of inhaled aerosol in different generations of the bronchial tree, where the trachea is generation 0. Adapted from [12].
Theoretically, to calculate the dose that needs to be deposited to achieve the target IC requires knowing the volume of the ASL. Unlike the predictability of blood volume, the ASL volume may have significant inter-personal variability. Such variability may result from individual disease states (e.g., pneumonia, healthy) or lifestyles (e.g., smoking). The ASL concentration of an individual patient can be verified by bronchoalveolar lavage (BAL) sampling.
Concentration in airway surface liquid (ASL)
A dose calculation yields a range of possibilities rather than a fixed number. In clinical practice with antibiotics, the indicated dosage for achieving a significant inhibitory concentration (IC) is a substantial multiple of the MIC within wide clinician-determined margins limited by the bounds of safety. It is common for antibiotics inhalation to target IC that can be ten times (10x) the MIC. Similar considerations apply to our nanoparticles dose calculation.
The bronchial tree’s first 10 generations surface area is about 1 m2 (10,000 cm2). The ASL layer thickness ranges from about 6 µm in the trachea to 3 µm in the 10th generation of the bronchial tree [12], amounting to a combined mucosal volume in the top half of the bronchial tree to be about 1 mL in a healthy adult. The surface area of the alveoli is about 100 m2, with mucosal thickness of about 0.07 µm, resulting in a total ASL volume of 7–10 mL. Therefore, the more realistic target treatment is disinfection of the upper bronchial tree at early stages before the infection spreads deep into the lungs. The disease state significantly affects antimicrobial inhalation delivery. Increased mucus production dilutes the drug concentration in the ASL, compared with healthy adults. Fortunately, for inhalation of NpC formulations, our theoretically computed MIC or MMC are more than 40 times smaller than the estimated safety limit (see section 3.7 below).
Deposition fraction in target tissue
The deposition fraction factor depends on the:
-
i.
Target tissue location: extra-thoracic, trachea-bronchial (TB) tree, or pulmonary (alveoli)
-
ii.
Mode of inhalation: nasal or oral
-
iii.
Size of the aerosol droplets.
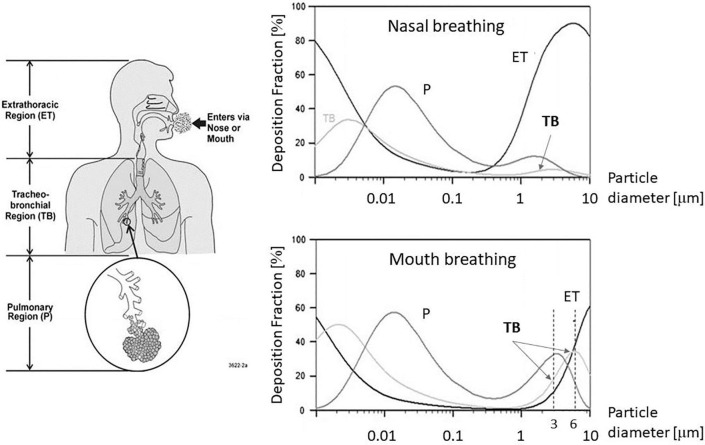
There is a significant difference in tracheal-bronchial (TB) tree deposition between nasal and oral breathing (Fig. 6 ). Peak nasal breathing TB deposition is only about 10%, whereas oral breathing TB deposition is about 30%. Hence, we recommend oral inhalation.
Fig. 6.
Deposition fractions in primary respiratory system structures when breathing at rest. Adapted from [25].
Depending on aerosol droplet size, the deposition fraction is different in each tissue region. As illustrated in Fig. 6: (a) the peak bronchial tree deposition fraction (of about 30%) is obtained with aerosol droplets of diameter ∼ 6 μm, whereas (b) peak alveoli deposition (of about 30%) is with aerosol droplets of diameter ∼ 3 μm. For 5 µm droplets, typical in mass-produced devices presently on the market, the bronchial tree deposition fraction is ∼ 25% and the alveoli deposition fraction is also ∼ 25%.
Inhalation timing losses
Inhalation represents only about a third of the duration of a complete breathing cycle. Consequently, when aerosols are delivered continuously, during 2/3 of the time the aerosol is cumulated in a cloud within the oral cavity until the next inhalation begins. Hence, we postulate a lower-bound working assumption that only about 50% of the aerosolized dose is considered to have been effectively inhaled. This would be common for home users utilizing standard commercial medicament aerosol devices available in pharmacies. By contrast, using a breath-actuated nebulizer would correspondingly lower wastage of silver NcP colloid, changing the associated dosage instructions.
Lung clearance
The lungs have innate mechanisms to remove deposited particles. Thus, we need to examine whether the nanoparticles reside long enough in respiratory system surface tissue to fulfill their antiviral potential. For indicative reference, we consider the behavior of inhaled antibiotics (tested in ventilated ICU patients) [26], [27]. We note that inhalation-deposited antibiotics reside for an effective peak duration of about 2–3 h in the lungs. The NpC experimental data we analyzed were commonly for 1 h treatments (e.g., for the coronavirus presented in Fig. 4). Hence, experience with inhaled antibiotics suggests that also the inhaled NpC will be retained in lung surface tissue for long enough to exhibit antiviral potency.
Clinical safety
Clinical safety evaluations are performed in the context of an estimated treatment dose and schedule. To be specific, we analyze the example outlined in table-1(ii): 2 mL of NpC with a concentration of 120 μg are inhaled (i.e., a dose of 240 μg per treatment), taken two times per day, which amounts to a daily deposition of about 480 μg , taken over five days (similar to an antibiotics regimen).
The human body has mechanisms for the disposal of silver. The natural median daily intake of silver from food and drinks has been reported to be up to 80 μg/day [28]. Therefore, our above scenario of a recommended treatment regimen (deposition of about 480 μg) is a significant increase over normal daily dietary intake for a short acute treatment duration of a few days. When addressing safety or toxicity, the professional guidelines distinguish between acute exposure of < 14 days and prolonged (repeated dose) or chronic exposure of more than 14 days. Only acute (<14 days) exposure is relevant in our context, but we shall discuss both.
USA occupational guidelines and exposure limits for airborne silver dust are all defined on a mass basis. The Occupational Safety and Health Administration (OSHA) in the USA adopted a threshold-limit value time-weighted average (TLV-TWA) chronic exposure over a 40-hr week of 100 μg/m3 (0.1 μg/L) of metallic silver dust. Under a regular breathing rate of 6–8 L/min, the resulting silver nanoparticle inhalation of 36–42 μg/h is considered a safe work environment. It amounts to daily, 8 h, inhaling ∼ 300 μg of silver nanoparticles on a prolonged routine basis. Thus, the treatment regimen stipulated here, of 240 μg dose given two times per day, is close to the safety bounds for acceptable chronic intake in the work environment in the USA.
However, chronic work environment exposure is not the appropriate context for acute drug toxicity evaluation. We should focus on the assessment of short-term inhalation. It has been shown that even after 90 days of continuous inhalation exposure to high doses of silver nanoparticles (total of 1,143 μg/day of silver – about three times (3x) our realistic treatment regimen example – the accumulated tissue levels recover to normal within about 12 weeks from the end of treatment (Fig. 7 ). This provides a firm indication of the safety and tolerance of short-term silver NpC inhalation exposure in that it does not lead to any lasting accumulation in body tissues.
Fig. 7.
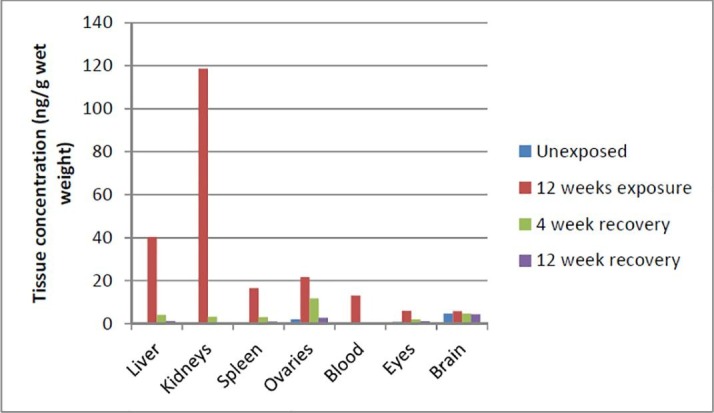
Tissue silver concentrations in female rats exposed to high levels of AgNP (381 μg/m3 silver nanoparticles of ∼ 15 nm diameter, for 6 h/day, which amounts to an inhalation dosage of 1,143 μg/day of silver) in a 90-day inhalation study, followed by a 12-week recovery period. Adapted from [29], [30].
A test closest to our envisioned treatment protocol was performed on rats for 10 days, 4 h/day, at a concentration of 3,300 μg/m3 (3.3 μg/L) using an aerosol of 5 nm silver nanoparticles, resulting in minimal pulmonary toxicity or inflammation [31]. Human breathing at an average rate of 6 L/min translates to a daily inhaled dosage of silver nanoparticle aerosol of 4,700 μg/day. This study indicates that, for acute short-term treatment of < 10 days, even an inhalation intake of 4,000 μg/day, which is about 10 times our realistic treatment regimen example, would induce no adverse reaction or a lasting residue.
Discussion
Though marred by the charlatan claims of unprofessional “alternative medicine” products, there is well-established scientific research on the antibacterial and antiviral properties of silver NpC. However, the potential applications for respiratory infections treatment have never been adequately explored. The surveyed literature indicates that silver nanoparticles colloids (NpC) of diameter 3–7 nm can be highly effective in suppressing many viral pathogens at an inhibitory concentration (IC) of 10 µg/mL (Table 2 ). For a treatment via inhalation delivery of silver NpC (Table 1), inhalation of 1 mL of NpC at a concentration of 120 μg can achieve a significant IC of 40 μg (i.e., 4x of MMC) in the bronchial tree airway surface liquid (ASL). With common market continuous nebulizers, one would need to nebulize a dose of 240 μg (because of 50% inhalation time losses). A twice daily treatment protocol corresponds to a total daily deposition of 240 μg. The available safety information indicates that such doses and regimens are well within the safe range and enable the safe delivery of even ten times (10x) the IC noted in Table 1. We estimate that these formulations can effectively prevent and treat any early-stage respiratory viral infection, including infection with SARS-CoV-2.
Table 2.
Inhibitory concentration (IC) for non-PVP stabilized nanoparticle colloids (NpC) with diameter ≤ 10 nm.
| Virus | NpC diameter distribution peak (nm) | MMC (µg/mL) | Reference |
|---|---|---|---|
| Influenza A H3N2 | 9.5 | <12.5 | [15] |
| Monkeypox (MPV) | 10 | <12.5 | [16] |
| Coronavirus TGEV 1 | 10 | ∼10 | [17] |
TGEV, transmissible gastroenteritis virus.
To set the scale of potential benefits, we flash out the remarkable results of an Influenza H3N2 in-vivo experiment done on mice (one of the very few in vivo animal experiments in the NpC literature), comparing the effectiveness of intranasal administration of NpC to that of Tamiflu (Oseltamivir) [15]. Tamiflu is claimed to reduce the number of patients with severe flu complications, such as pneumonia (by 44%) or hospitalization (by 63%). As shown in Fig. 8 below, it appears that potentially NpC can be as effective as Tamiflu. A NpC flu treatment, if effective as in the mice model, could cost < 1/10 of Tamiflu, with lower side effects risk, be available essentially OTC (as market availability of NpC already is) and be manufactured locally in any country. However, no investment in clinical human trials was ever done to investigate the possibility. We can only speculate that this is due to conventional pharma companies' lack of financial incentives to make the required investment in development and regulatory procedures. One of the main goals of this paper is to motivate, guide, and advocate for future investment in the clinical and regulatory development of NpC treatment formulations.
Fig. 8.
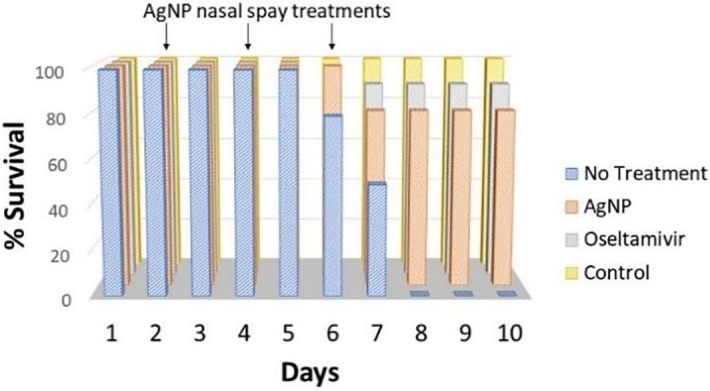
In-vivo intranasal NpC administration protected mice from H3N2 infection. Adapted from [15].
For bacterial infections, particularly in the context of preventing ICU-acquired VAP, the same formulations are expected to be applicable. An additional risk-reduction benefit of silver NpC inhalation treatment for ventilated patients is the possibility of suppression of biofilm formation inside the endotracheal or tracheostomy tube.
Funding
This research received no external funding.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Yamor Technologies promotes a drug development program based on the framework presented in this article.
Acknowledgments
Acknowledgements
We thank Alex Singer for editorial assistance in the manuscript’s preparation.
Consent statement/Ethical approval
Not required.
References
- 1.Aderibigbe B.A. Metal-based nanoparticles for the treatment of infectious diseases. Molecules [Internet]. 2017;22(8):1370. doi: 10.3390/molecules22081370. http://www.mdpi.com/1420-3049/22/8/1370 Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nakamura S., Sato M., Sato Y., et al. Synthesis and application of silver nanoparticles (Ag NPs) for the prevention of infection in healthcare workers. Int J Mol Sci [Internet] 2019;20(15):3620. doi: 10.3390/ijms20153620. https://www.mdpi.com/1422-0067/20/15/3620 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Siadati S.A., Afzali M., Sayadi M. Could silver nano-particles control the 2019-nCoV virus?; An urgent glance to the past. Chem Rev Lett [Internet] 2020;3(1):9–11. http://www.chemrevlett.com/article_105425.html Available from: [Google Scholar]
- 4.Galdiero S., Falanga A., Vitiello M., Cantisani M., Marra V., Galdiero M. Silver nanoparticles as potential antiviral agents. Molecules [Internet] 2011;16(10):8894–8918. doi: 10.3390/molecules16108894. http://www.mdpi.com/1420-3049/16/10/8894 Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Balavandy S.K., Shameli K., Biak D.R.B.A., Abidin Z.Z. Stirring time effect of silver nanoparticles prepared in glutathione mediated by green method. Chem Cent J. 2014;8(1):11. doi: 10.1186/1752-153X-8-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haggag E., Elshamy A., Rabeh M., et al. Antiviral potential of green synthesized silver nanoparticles of Lampranthus coccineus and Malephora lutea. Int J Nanomed [Internet] 2019;14:6217–6229. doi: 10.2147/IJN.S214171. https://www.dovepress.com/antiviral-potential-of-green-synthesized-silver-nanoparticles-of-lampr-peer-reviewed-article-IJN Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rouby J.J., Bouhemad B., Monsel A., Brisson H., Arbelot C., Lu Q. Aerosolized antibiotics for ventilator-associated pneumonia: Lessons from experimental studies. Anesthesiology. 2012;117(6):1364–1380. doi: 10.1097/ALN.0b013e3182755d7a. [DOI] [PubMed] [Google Scholar]
- 8.Darquenne C., Fleming J.S., Katz I., et al. Bridging the gap between science and clinical efficacy: Physiology, imaging, and modeling of aerosols in the lung. J Aerosol Med Pulm Drug Deliv. 2016;29(2):107–126. doi: 10.1089/jamp.2015.1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Behrens G., Stoll M. Pathogenesis and immunology [Internet] Flying Publisher; Paris, France: 2006. pp. 92–109. [cited 2020 Nov 30]. Available from: [Google Scholar]
- 10.Garland J.S. Ventilator-associated pneumonia in neonates: An update. Neoreviews [Internet] 2014;15(6):e225–e235. https://neoreviews.aappublications.org/content/15/6/e225 Available from. [Google Scholar]
- 11.Manjarrez-Zavala EM, Patricia D, Horacio L, Ocadiz-Delgado R, Cabello-Gutierrez C. Pathogenesis of viral respiratory infection [Internet]. In: Respiratory Disease and Infection - A New Insight. Mahboub BH (Ed.), InTech (2013) [cited 2020 Nov 30]. Available from: http://dx.doi.org/10.5772/54287.
- 12.Hasan M.A., Lange C.F. Estimating in vivo airway surface liquid concentration in trials of inhaled antibiotics. J. Aerosol Med. 2007;20(3):282–293. doi: 10.1089/jam.2007.0603. [DOI] [PubMed] [Google Scholar]
- 13.Ringshausen F.C., Chalmers J.D., Pletz M.W. Anti-infectives and the Lung. European Respiratory Society; 2017. pp. 57–79. [DOI] [Google Scholar]
- 14.Elechiguerra J.L., Burt J.L., Morones J.R., et al. Interaction of silver nanoparticles with HIV-1. J. Nanobiotechnology [Internet]. 2005;3(1):6. doi: 10.1186/1477-3155-3-6. http://jnanobiotechnology.biomedcentral.com/articles/10.1186/1477-3155-3-6 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xiang D, Zheng C, Zheng Y, et al. Inhibition of A/Human/Hubei/3/2005 (H3N2) influenza virus infection by silver nanoparticles in vitro and in vivo. Int. J. Nanomedicine [Internet]. 8(1), 4103 (2013). Available from: http://dx.doi.org/10.2147/IJN.S53622. [DOI] [PMC free article] [PubMed]
- 16.Rogers J.V., Parkinson C.V., Choi Y.W., Speshock J.L., Hussain S.M. A preliminary assessment of silver nanoparticle inhibition of Monkeypox virus plaque formation. Nanoscale Res Lett. 2008;3(4):129–133. [Google Scholar]
- 17.Lv X., Wang P., Bai R.u., Cong Y., Suo S., Ren X., et al. Inhibitory effect of silver nanomaterials on transmissible virus-induced host cell infections. Biomaterials. 2014;35(13):4195–4203. doi: 10.1016/j.biomaterials.2014.01.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dakal T.C., Kumar A., Majumdar R.S., Yadav V. Mechanistic basis of antimicrobial actions of silver nanoparticles. Front Microbiol. 2016;7:1831. doi: 10.3389/fmicb.2016.01831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morris D., Ansar M., Speshock J., et al. Antiviral and immunomodulatory activity of silver nanoparticles in experimental rsv infection. Viruses [Internet] 2019;11(8) doi: 10.3390/v11080732. https://pubmed.ncbi.nlm.nih.gov/31398832/ Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prabakaran P., Xiao X., Dimitrov D.S. A model of the ACE2 structure and function as a SARS-CoV receptor. Biochem Biophys Res Commun. 2004;314(1):235–241. doi: 10.1016/j.bbrc.2003.12.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kyrychenko A., Pasko D.A., Kalugin O.N. Poly(vinyl alcohol) as a water protecting agent for silver nanoparticles: The role of polymer size and structure. Phys Chem Chem Phys. 2017;19(13):8742–8756. doi: 10.1039/c6cp05562a. [DOI] [PubMed] [Google Scholar]
- 22.Clary-Meinesz C., Mouroux J., Cosson J., Huitorel P., Blaive B. Influence of external pH on ciliary beat frequency in human bronchi and bronchioles. Eur Respir J. 1998;11(2):330–333. doi: 10.1183/09031936.98.11020330. [DOI] [PubMed] [Google Scholar]
- 23.Lara H.H., Ayala-Nuñez N.V., Ixtepan-Turrent L., Rodriguez-Padilla C. Mode of antiviral action of silver nanoparticles against HIV-1. J Nanobiotechnol [Internet] 2010;8(1):1. doi: 10.1186/1477-3155-8-1. http://jnanobiotechnology.biomedcentral.com/articles/10.1186/1477-3155-8-1 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Martínez-Castañón G.A., Niño-Martínez N., Martínez-Gutierrez F., Martínez-Mendoza J.R., Ruiz F. Synthesis and antibacterial activity of silver nanoparticles with different sizes. J Nanoparticle Res [Internet] 2008;10(8):1343–1348. https://link.springer.com/article/10.1007/s11051-008-9428-6 Available from: [Google Scholar]
- 25.Cheng Y.S. Mechanisms of pharmaceutical aerosol deposition in the respiratory tract. AAPS PharmSciTech [Internet] 2014;15(3):630–640. doi: 10.1208/s12249-014-0092-0. https://link.springer.com/article/10.1208/s12249-014-0092-0 Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dhanani J., Fraser J.F., Chan H.K., Rello J., Cohen J., Roberts J.A. Fundamentals of aerosol therapy in critical care. Crit Care. 2016;20(1):1–16. doi: 10.1186/s13054-016-1448-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lu Q., Girardi C., Zhang M., Bouhemad B., Louchahi K., Petitjean O., et al. Nebulized and intravenous colistin in experimental pneumonia caused by Pseudomonas aeruginosa. Intensive Care Med. 2010;36(7):1147–1155. doi: 10.1007/s00134-010-1879-4. [DOI] [PubMed] [Google Scholar]
- 28.WHO. Silver in drinking-water: Background document for development of WHO Guidelines for Drinking-water Quality [Internet]. Geneva. Available from: https://www.who.int/water_sanitation_health/dwq/chemicals/silver.pdf.
- 29.Fewtrell L. Silver: Water disinfection and toxicity [Internet]. Available from: https://www.who.int/water_sanitation_health/dwq/chemicals/Silver_water_disinfection_toxicity_2014V2.pdf.
- 30.Song K.S., Sung J.H., Ji J.H., Lee J.H., Lee J.S., Ryu H.R., et al. Recovery from silver-nanoparticle-exposure-induced lung inflammation and lung function changes in Sprague Dawley rats. Nanotoxicology. 2013;7(2):169–180. doi: 10.3109/17435390.2011.648223. [DOI] [PubMed] [Google Scholar]
- 31.Stebounova L.V., Adamcakova-Dodd A., Kim J.S., Park H., O'Shaughnessy P.T., Grassian V.H., et al. Nanosilver induces minimal lung toxicity or inflammation in a subacute murine inhalation model. Part Fibre Toxicol. 2011;8(1) doi: 10.1186/1743-8977-8-5. [DOI] [PMC free article] [PubMed] [Google Scholar]