Abstract
Background
Adult-onset Still’s disease (AOSD) is a rare systemic autoinflammatory disease which encompasses patients with heterogenous presentation and a wide range of clinical courses. In this study, we aimed to identify potential subgroups of AOSD and reveal risk factors for relapse.
Methods
We included a total of 216 AOSD patients who received treatment in nine hospitals between 2000 and 2019. All patients fulfilled the Yamaguchi classification criteria. We retrospectively collected information about baseline characteristics, laboratory tests, treatment, relapse, and death. We performed latent class analysis and time-to-event analysis for relapse using the Cox proportional hazard model.
Results
The median age at disease onset was 51.6 years. The median follow-up period was 36.8 months. At disease onset, 22.3% of the patients had macrophage activation syndrome. The median white blood cell count was 12,600/μL, and the median serum ferritin level was 7230 ng/mL. Systemic corticosteroids were administered in all but three patients (98.6%) and the median initial dosage of prednisolone was 40mg/day. Ninety-six patients (44.4%) were treated with concomitant immunosuppressants, and 22 (10.2%) were treated with biologics. Latent class analysis revealed that AOSD patients were divided into two subgroups: the typical group (Class 1: 71.8%) and the elderly-onset group (Class 2: 28.2%). During the follow-up period, 13 of 216 patients (6.0%) died (12 infections and one senility), and 76 of 216 patients (35.1%) experienced relapses. Overall and relapse-free survival rates at 5 years were 94.9% and 57.3%, respectively, and those rates were not significantly different between Class 1 and 2 (p=0.30 and p=0.19). Time-to-event analysis suggested higher neutrophil count, lower hemoglobin, and age ≥65 years at disease onset as risk factors for death and age ≥65 years at disease onset as a risk factor for relapse.
Conclusions
AOSD patients were divided into two subgroups: the typical group and the elderly-onset group. Although the survival of patients with AOSD was generally good, the patients often experienced relapses. Age ≥65 years at disease onset was the risk factor for relapse.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13075-021-02708-3.
Keywords: Adult-onset Still’s disease, Macrophage activation syndrome, Latent class analysis, Outcomes, Relapse
Background
Adult-onset Still’s disease (AOSD) is a rare systemic autoinflammatory disease that affects adults with a higher prevalence in women [1–3]. In 1897, George Frederic Still first reported juvenile chronic arthritis with fever and rash as Still’s disease [4], which is now considered systemic juvenile idiopathic arthritis (sJIA). Later, Adult Still’s disease (ASD) was reported by Eric Bywaters as a series of adult patients who had features similar to the children with sJIA with three main symptoms: quotidian fevers, arthritis, and evanescent rash and did not fulfill the criteria for classic rheumatoid arthritis [5]. ASD is now considered a disease concept containing both sJIA patients after becoming adults and AOSD patients.
Clinical manifestations of AOSD include fever, rash, arthralgia, sore throat, elevated liver enzymes, and hyperferritinemia [6–8]. Above all, serum ferritin levels are typically much higher than those in other autoimmune diseases, autoinflammatory diseases, infections or neoplasms, characterized by decreased glycosylated ferritin (<20%) [9, 10]. A five-fold increase of serum ferritin levels compared with the normal value is strongly suggestive of AOSD, and ferritin is also considered a useful marker of disease activity of AOSD [11, 12]. However, AOSD patients do not always present a five-fold increase of serum ferritin levels and other manifestations of AOSD are non-specific. Considering the lack of specific disease markers, patients diagnosed as AOSD could be a heterogeneous population.
Regarding the outcomes of patients with AOSD, the mortality rate has been reported to be 2.6–5.5% [13, 14]. The AOSD patients can have severe complications such as macrophage activation syndrome (MAS), disseminated intravascular coagulation (DIC), thrombotic thrombocytopenic purpura, acute respiratory distress syndrome, and diffuse alveolar hemorrhage [15–22], which can lead to mortality. In terms of relapse, some patients with AOSD experience multiple relapses, while others maintain long-term remission without relapse. In the past, three differential clinical patterns of AOSD have been described: (1) monocyclic pattern, characterized by a single systemic episode; (2) polycyclic pattern, associated with a longer clinical course, alternating with remissions; and (3) chronic pattern, related to persistently active disease with associated polyarthritis [23]. According to the previous review, 30% of AOSD patients develop a monocyclic pattern, 30% a polycyclic pattern, and 40% a chronic pattern on average [1]. However, it is still difficult to predict which clinical pattern the patient will follow, and risk factors for relapse are still unknown.
In this retrospective observational study, we addressed two clinical questions using a large cohort of AOSD patients. First, we aimed to classify the subgroups of AOSD patients, who are considered a heterogenous population. Second, we also aimed to identify the risk factors for relapses by analyzing the clinical features at disease onset.
Patients and methods
Patients
AOSD patients who received treatment in nine Japanese hospitals between April 2000 and March 2019 were the subjects of this retrospective study. Fourteen patients who lacked baseline data were not included. Thirteen patients whose conditions were indistinguishable from other diseases, such as viral infection or malignant lymphoma, were not included. Consequently, a total of 216 AOSD patients who fulfilled the Yamaguchi classification criteria [24] and were 16 years or older at the time of diagnosis were included in the study.
Data collection
The presence/absence of the following clinical features at diagnosis was determined: fever, typical rash, atypical rash, arthralgia, myalgia, sore throat, lymphadenopathy, hepatomegaly, splenomegaly, abnormal liver function tests, chest pain, and abdominal pain. We also collected the results of blood examinations at diagnosis, which included white blood cell (WBC) count, neutrophil count, hemoglobin (Hb), platelet count, erythrocyte sedimentation rate (ESR), aspartate aminotransferase (AST), alanine aminotransferase (ALT), lactate dehydrogenase (LDH), C-reactive protein (CRP), and ferritin. In addition, we assessed the presence/absence of AOSD-related specific complications at diagnosis, which included MAS, DIC, renal dysfunction, pleuritis, pericarditis, myocarditis, and interstitial pneumonia. MAS was defined following diagnostic criteria proposed by the Histocyte Society in 1991 and updated in 2004 by Fardet et al. [25–28]. We also calculated the systemic score for AOSD proposed by Pouchot et al. [29]. This score assigns one point to each of 12 manifestations: fever, typical rash, pleuritis, pneumonia, pericarditis, hepatomegaly, or abnormal liver function tests, splenomegaly, lymphadenopathy, leukocytosis > 15,000mm3, sore throat, myalgia, and abnormal pain. Information on the use of systemic corticosteroids, converted to the equivalent prednisolone dose, immunosuppressants, biologics, endotoxin adsorption, and plasma exchange was also collected.
We also assessed the duration of time from diagnosis of AOSD to death and to the first relapse. Relapse was defined as a state in which clinical symptoms were present and treatment was reinforced after remission; remission was defined as the absence of systemic symptoms or laboratory evidence of disease activity for at least three consecutive months, regardless of therapy.
Data were retrospectively acquired from patients’ medical charts and electronic records.
Clinical courses of the patients with AOSD were classified according to the types of monocyclic, polycyclic, or chronic pattern. The classification was based on reviews of case history by the authors according to a previous report [30]. The polycyclic pattern was defined as the existence of a symptom-free period of at least 2 months between 2 relapses. The chronic pattern was defined as the presence of persistent joint symptoms.
Statistical analysis
Comparisons between groups were performed using the Mann-Whitney U test for continuous and ordinal variables and the chi-square test for categorical variables. We used latent class analysis to identify subgroups based on baseline patient/disease characteristics. A multiple-group latent class model [31] with the optimal number of computer-derived subgroups (latent classes) was determined using model selection criteria, consistent Akaike information criteria and Bayesian information criteria values. After the number of classes was chosen, individuals were assigned to the class in which they had the highest posterior probability of membership. The overall survival rates and the relapse-free survival rates were calculated using the Kaplan-Meier method and the survival rates between groups were compared by the log-rank test. To assess the potential risk factors for relapse, time-to-event analysis was performed using the univariate Cox proportional hazard, and multivariate model approach was also conducted with these risk factors included as covariates. P<0.05 was considered statistically significant. Latent class analysis was performed using the PROC LCA (ver 1.3.2) [32], the remaining analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC, USA).
Results
Baseline characteristics
We identified 216 consecutive patients with AOSD. Baseline characteristics of these patients are shown in Table 1. The median age at disease onset was 51.6 years and 75.9% were female. The median WBC count at onset was 12,600/μL and the median neutrophil count was 10677/μL. Serum ferritin and CRP levels at onset were highly elevated (median 7,230ng/mL and 10.8mg/dL).
Table 1.
Baseline characteristics of the patients
| Total (n=216) | Relapse (n=76) | Non-relapse (n=140) | |
|---|---|---|---|
| General characteristics | |||
| Age, median years [IQR] | 51.6 [33.1–68.1] | 50.3 [30.2–65.9] | 47.9 [31.8–69.9] |
| Female, n (%) | 164 (75.9%) | 68 (89.4%) | 59 (65.6%) |
| Follow-up time, median months [IQR] | 36.8 [12.1–88.2] | 80.6 [40.0–135.8] | 18.8 [8–46.8] |
| Proportion of patients with the specific symptom | |||
| Fever, % | 99.5% | 100.0% | 98.9% |
| Rash, % | 90.7% | 97.3% | 87.1% |
| Abnormal liver function tests, % | 81.0% | 85.5% | 76.9% |
| Arthralgia, % | 79.5% | 82.6% | 77.8% |
| Sore throat, % | 63.3% | 56.1% | 67.1% |
| Lymphadenopathy, % | 63.5% | 60.0% | 65.9% |
| Splenomegaly, % | 49.5% | 47.8% | 50.4% |
| Chest pain, % | 1.9% | 1.3% | 2.1% |
| Abdominal pain, % | 1.9% | 1.3% | 2.1% |
| Laboratory tests | |||
| White blood cell count, median /μL [IQR] | 12600 [9400–18100] | 12600 [9190–17975] | 12630 [9575–18100] |
| Neutrophil count, median /μL [IQR] | 10677 [7555–15794] | 10583 [7235–16194] | 10677 [7665–14960] |
| Hemoglobin, median g/dL [IQR] | 11.1 [10.1–12.4] | 10.8 [9.8–11.7] | 11.3 [10.2–12.7] |
| Platelet, median /μL [IQR] | 258 [163–366] | 260 [170–351] | 256 [159–377] |
| Erythrocyte sedimentation rate, median mm/h [IQR] | 76 [41–94] | 80 [40–95] | 75 [44–92] |
| Serum aspartate aminotransferase, median U/L [IQR] | 69 [46–128] | 68 [47–125] | 69 [45–130] |
| Serum alanine aminotransferase, median U/L [IQR] | 52 [30–104] | 50 [25–87] | 53 [31–110] |
| Serum lactate dehydrogenase, median U/L [IQR] | 521 [314–761] | 587 [357–796] | 501 [303–734] |
| Serum C-reactive protein, median mg/dL [IQR] | 10.8 [5.7–16.6] | 11 [5.8–18.6] | 10.8 [5.7–14.8] |
| Serum ferritin, median ng/mL [IQR] | 7230 [2002–22065] | 8536 [1745–29940] | 6190 [2201–18472] |
| Complications | |||
| Macrophage activation syndrome, % | 22.3% | 18.4% | 24.5% |
| Disseminated intravascular coagulation, % | 13.4% | 17.1% | 11.5% |
| Renal dysfunction, % | 3.7% | 3.9% | 3.6% |
| Pleuritis, % | 12.5% | 10.7% | 13.6% |
| Pericarditis, % | 7.4% | 4.0% | 9.3% |
| Myocarditis, % | 0.0% | 0.0% | 0.0% |
| Interstitial pneumonia, % | 2.3% | 2.7% | 2.1% |
IQR interquartile range
Regarding symptoms, most patients had fever (99.5%), rash (90.7%), abnormal liver function tests (81.0%), and arthralgia (79.5%). Other classical symptoms, such as sore throat (63.3%), lymphadenopathy (63.5%), or splenomegaly (49.5%) were also frequently present (Table 1), which was consistent with the previous reports.
The median systemic score was five points and 38 patients had systemic scores greater than seven points, which was previously reported as a risk factor for death [33]. However, the systemic score did not correlate with death or relapse in our study (p=0.21 and p=0.15, respectively).
With regard to the pre-specified complications, 22.3% of the patients had MAS and 13.4% had DIC. Renal dysfunction and interstitial pneumonitis were rare in our cohort (3.7% and 2.3%, respectively) (Table 1). Patient characteristics according to presence/absence of MAS were summarized in Supplementary Table 1.
As to the patterns of clinical course, 136 patients (62.9%) had a monocyclic pattern, while 76 patients (35.1%) presented a polycyclic pattern. In our cohort, only four patients (1.8%) presented a chronic pattern.
Treatments
The treatment details for the new-onset disease are shown in Table 2. Systemic corticosteroids were administered in all but three patients (98.6%) and the median initial dosage of prednisolone was 40mg/day. Ninety-six patients (44.4%) were treated with concomitant immunosuppressants, and 22 (10.2%) were treated with tocilizumab. Plasma exchange was performed in five patients (2.3%). None of the patients were treated with interleukin-1 inhibitors such as canakinumab and anakinra.
Table 2.
Treatment details
| Treatment at disease onset (n=216) | Treatment after first relapse (n=76) | |
|---|---|---|
| Corticosteroid, n (%) | 213 (98.6%) | 76 (100%) |
| Initial dose of corticosteroid, median mg/day | 40 | 40 |
| Pulse corticosteroid therapy, n (%) | 41 (5.3%) | 6 (7.9%) |
| Increased corticosteroid, n (%) | N/A | 58 (76.3%) |
| Immunosuppressive agents, n (%) | 96 (44.4%) | 38 (50.0%) |
| Cyclosporine | 76 (35.2%) | 23 (30.3%) |
| Methotrexate | 14 (6.5%) | 6 (7.9%) |
| Tacrolimus | 5 (2.3%) | 5 (6.6%) |
| Biological agents, n (%) | 22 (10.2%) | 13 (17.1%) |
| Tocilizumab | 22 (10.2%) | 11 (14.5%) |
| Adalimumab | 0 | 1 (1.3%) |
| Etanercept | 0 | 1 (1.3%) |
| Plasma exchange, n (%) | 5 (2.3%%) | 0 |
N/A not applicable
During the follow-up period, 76 patients (35.1%) experienced relapses, of which 33 (15.2%) had multiple relapses. At the time of the first relapse, 29 of the 76 patients (38.2%) were taking prednisolone with the median of 8mg/day, while the remaining 47 (61.8%) had stopped glucocorticoids prior to the relapse. Fifty-eight of the 76 patients (76.3%) increased the dose of prednisolone to the median of 40mg/day. In addition, immunosuppressants and biologic agents were commenced in 40 and 13 patients, respectively.
Latent class analysis
Model selection criteria suggested that a multiple-group latent class model with two latent classes was preferable (Supplementary Table 2). All item response probabilities in the selected model are provided in Table 3 and additional information that characterizes these subgroups are summarized in Supplementary Table 3. Class 1 (n=155, 71.8%) was associated with a younger age of onset and typical symptoms that are included in the classification criteria, such as skin rash, arthralgia, and hepatosplenomegaly. On the other hand, Class 2 (n=61, 28.2%) was associated with higher serum ferritin levels, an older age of onset, and fewer typical AOSD symptoms. Frequencies of the major complications, MAS and DIC were not significantly different between Class 1 and Class 2 (p=0.50 for MAS and =0.10 for DIC). These data suggest that AOSD patients can be classified into two distinct subgroups, the typical AOSD group (Class 1) and the elderly-onset AOSD group (Class 2).
Table 3.
Item response probabilities in latent class analysis
| Class 1 | SE | Class 2 | SE | ||
|---|---|---|---|---|---|
| Estimate | Estimate | ||||
| White blood cell count (/μL) | ≤6,000 | 0.10 | 0.03 | 0.05 | 0.03 |
| 6000–12,000 | 0.42 | 0.05 | 0.29 | 0.09 | |
| 12,000< | 0.48 | 0.05 | 0.67 | 0.10 | |
| Serum ferritin (ng/mL) | ≤500 | 0.10 | 0.03 | 0.04 | 0.04 |
| 500–5000 | 0.40 | 0.05 | 0.22 | 0.07 | |
| 5000< | 0.50 | 0.05 | 0.74 | 0.08 | |
| Serum C-reactive protein (mg/dL) | ≤0.3 | 0.01 | 0.01 | 0.00 | 0.00 |
| 0.3–10 | 0.55 | 0.05 | 0.25 | 0.09 | |
| 10< | 0.44 | 0.05 | 0.75 | 0.09 | |
| Age (years) | ≤50 | 0.64 | 0.08 | 0.15 | 0.07 |
| 50< | 0.36 | 0.08 | 0.85 | 0.07 | |
| Splenomegaly | Presence | 0.61 | 0.08 | 0.24 | 0.08 |
| Hepatomegaly | Presence | 0.40 | 0.07 | 0.13 | 0.06 |
| Sore throat | Presence | 0.68 | 0.05 | 0.53 | 0.08 |
| Arthritis | Presence | 0.82 | 0.04 | 0.75 | 0.07 |
| Pericarditis | Presence | 0.00 | 0.01 | 0.23 | 0.09 |
| Pleuritis | Presence | 0.01 | 0.01 | 0.37 | 0.12 |
| Macrophage activating syndrome | Presence | 0.20 | 0.04 | 0.27 | 0.07 |
| Typical rash | Presence | 0.64 | 0.05 | 0.37 | 0.1 |
SE standard error
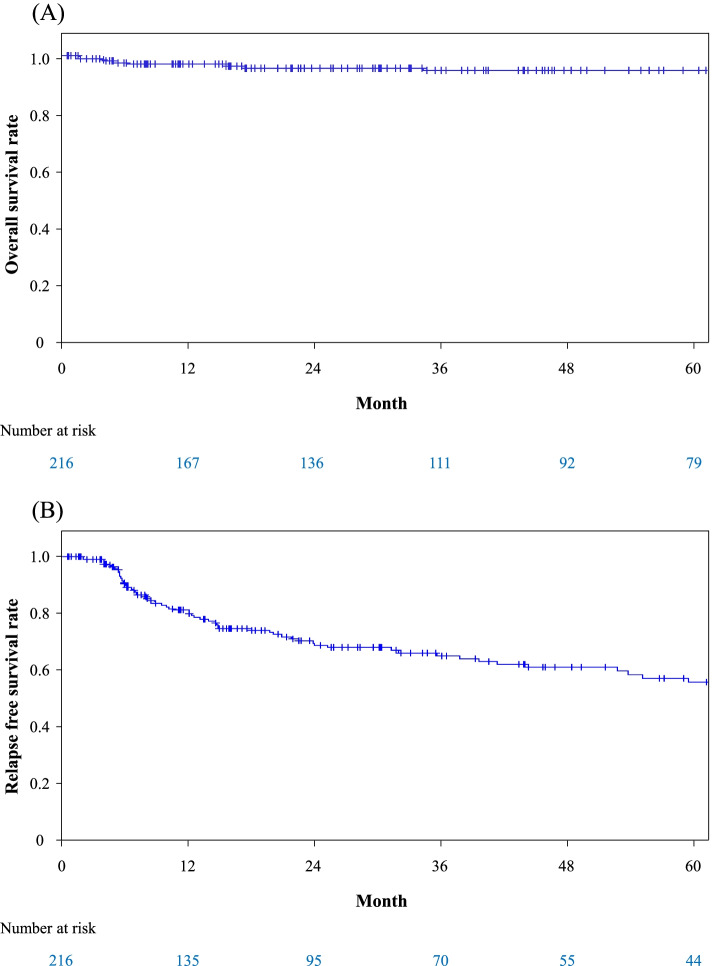
Survival and relapse
During the follow-up period, 13 of 216 patients (6.0%) died (12 infections and one senility). Median age at death was 75.5 years. The overall survival rates at one and 5 years were 97.0% and 94.9%, respectively (Fig. 1A). We assessed Class 1/2 and all items in Tables 1 and 2 as potential risk factors for death. Univariate Cox regression analysis identified a higher neutrophil count, a lower hemoglobin level, and a higher age at disease onset as significant factors for death (p=0.02, 0.02, and p=0.01) (Table 4). In addition, Class 2 showed a tendency to a higher risk for death (p=0.05).
Fig. 1.
Overall and relapse-free survival rates of all patients. A Cumulative survival rate assessed by Kaplan-Meier survival curve is shown. B Cumulative relapse-free survival rate assessed by Kaplan-Meier survival curve is shown
Table 4.
Time to event analysis for death with Cox proportional hazard model
| Parameter | Univariate analysis | |||
|---|---|---|---|---|
| HR | 95%CI | p value | ||
| Neutrophil count, 10^3/μL | 1.07 | 1.01 | 1.13 | 0.02 |
| Hemoglobin, g/dL | 0.69 | 0.50 | 0.95 | 0.02 |
| Age ≤ 65 years old | Ref | |||
| > 65 years old | 45.40 | 5.80 | 355.61 | 0.01 |
HR hazard ratio, 95%CI 95% confidence interval
Seventy-six of 216 patients (35.1%) experienced relapses, of which 33 (15.2%) had multiple relapses. Median time to the first relapse was 12.9 months. The relapse-free survival rates at one and 5 years were 81.6% and 57.3%, respectively (Fig. 1B). In univariate Cox regression analysis of relapse, only a higher age at disease onset was identified as a risk factor (p=0.01) (Table 5)..
Table 5.
Time to event analysis for relapse with Cox proportional hazard model
| Parameter | Univariate analysis | |||
|---|---|---|---|---|
| HR | 95%CI | p value | ||
| Age ≤ 65 years old | Ref | |||
| > 65 years old | 4.51 | 1.65 | 12.32 | 0.01 |
HR hazard ratio, 95%CI 95% confidence interval
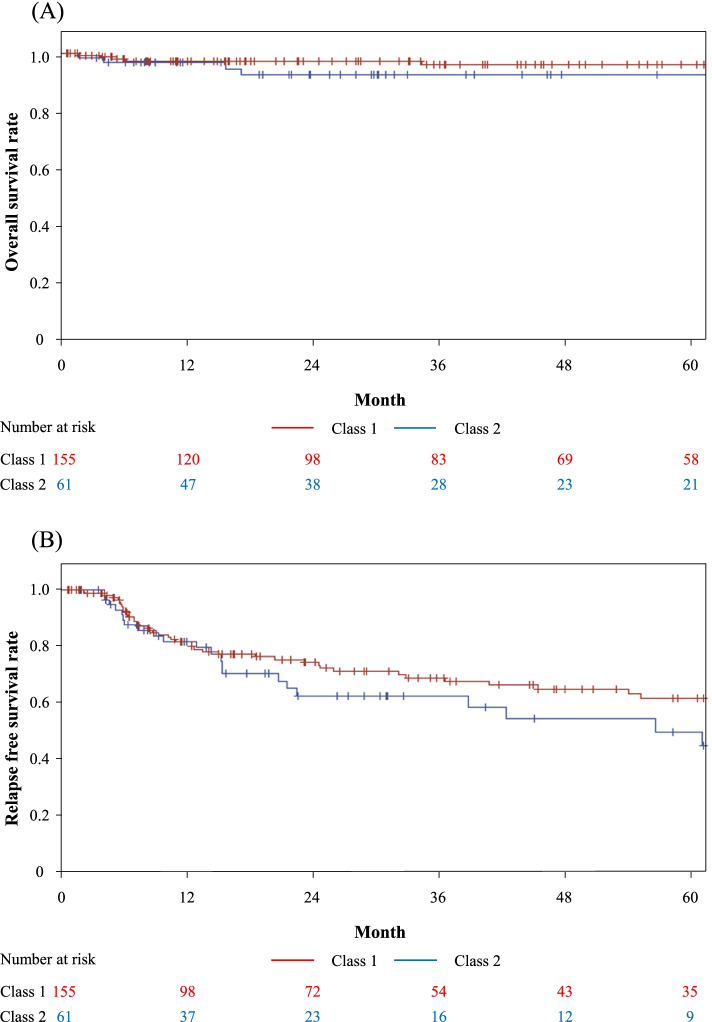
Neither overall survival nor relapse-free survival rates were significantly different between the two classes (p=0.30 and p=0.19) (Fig. 2A, B) although patients in these two classes received similar treatments. Median initial doses of prednisolone were 42.5mg/day and 40mg/day in Class 1 and 2 (p>0.99). Sixty-nine of 155 (44.5%) in Class 1 and 27 of 61 (44.2%) in Class 2 received immunosuppressants (p>0.99), and 14 of 155 (9.0%) in Classes 1 and 8 of 61 (13.1%) in Class 2 received biologics (p=0.37).
Fig. 2.
Overall and relapse-free survival rates according to Class 1 and Class 2. A Cumulative survival rates assessed by Kaplan-Meier survival curve are shown. Red line shows class 1 and blue line shows class 2. B Cumulative relapse-free survival rates assessed by Kaplan-Meier survival curve are shown. Red line shows class 1 and blue line shows class 2
Discussion
AOSD is a rare systemic autoinflammatory disease and its etiology and pathology have not been fully understood yet. Diagnosis of AOSD is made on the basis of a set of non-specific clinical symptoms, and there is no specific laboratory marker for AOSD. Consequently, AOSD patients are heterogeneous populations and predicting their clinical courses in advance is difficult. We addressed these issues with two approaches, latent class analysis and time-to-event analysis using a large cohort of AOSD patients, both of which have not been reported in the literature. In this study, the latent class analysis revealed that AOSD patients were divided into two reasonable populations: the typical AOSD group (Class 1) and the elderly-onset AOSD group (Class 2). Treatment and outcomes were not significantly different between Class 1 and Class 2, indicating that treatment adjustment for each subgroup is not necessary. Thus, this subdivision may not directly help the current practice of AOSD patients. However, focusing on more specific subgroups may lead to attenuation of noise and facilitate finding new biomarkers when combining future studies, such as a genome-wide association study, a gene expression study and proteomics analysis.
The overall survival rate in this study was 94.9% at 5 years, which was comparable with previous reports [34, 35]. The time-to-event analysis with the Cox proportional hazard model expectedly identified age ≧65 years at disease onset as a risk factor for death. In contrast to the good overall survival rate, the long-term relapse-free survival rate was low (57.3% at 5 years). Although small studies in the past suggested that inadequate corticosteroid initiation doses, elevated white blood cell counts, high erythrocyte sedimentation rates, ferritin levels, and high systemic scores as risk factors for relapse of AOSD [6, 7, 36], only age ≧65 years at disease onset was identified as the risk factor for relapse in this study. The reasons for the relapse risk of older age are not known. Different intensity of treatments among ages might be the cause. Older patients in our cohort received similar initial treatments with younger patients; however, there was a possibility of more rapid reduction/withdrawal of prednisolone and immunosuppressants in elder patients considering treatment-related adverse events.
Regarding the classical classification of the disease courses of AOSD patients, 136 patients (62.9%) had a monocyclic pattern, 76 patients (35.1%) had a polycyclic pattern, and 4 patients (1.8%) had a chronic pattern in this study. The remarkable decrease in chronic pattern and increase in monocyclic pattern compared to previous reports [1] were observed in this study. Advances in the treatments of AOSD might be the reason for those changes in addition to differences in the local treatment strategies.
In terms of complications of AOSD, MAS was the most common in this study (22.3%), which was consistent with previous reports from Japan [37]. Wang et al. previously reported that the presence of MAS was the major cause of death in AOSD patients [38]; however, there were no deaths due to MAS in this study. In addition, there was no significant difference in death between AOSD patients with and without MAS in this study. These differences might be caused by the different treatment strategies between the cohorts. In our cohort, tocilizumab was frequently used in refractory cases, especially having MAS. Although there were reports that tocilizumab sometimes induced MAS in AOSD patients [39], among 31 AOSD patients who received tocilizumab in our study, none developed MAS after tocilizumab treatment.
In a previous study using a large US administrative claims database, acute respiratory distress syndrome was present in 12.3% of AOSD patients [40]. In the current study, on the other hand, interstitial pneumonia was observed in 5 patients (2.3%), which was the only pulmonary involvement. Another Japanese group also reported that the proportion of pulmonary involvement in Japanese AOSD patients was 2.5% [37], which was similar to our study. Pulmonary involvement is rare in Japanese patients with AOSD.
Recently, an Italian group published a study of similar concept to identify subgroups of AOSD patients. We used latent class analysis with a larger and Japanese cohort, while they approached using cluster analysis with an Italian population. They divided AOSD patients into four subgroups: cluster 1 with the highest ferritin levels, cluster 2 with the highest CRP levels, cluster 3 with the highest systemic scores, and cluster 4 with the lowest ferritin and CRP levels [41]. Although the reasons for the different results from ours were unknown, the different methods and patient populations might have led to the different results.
Patient data in this study consisted of only classical items; however, there are new modalities and biomarkers for evaluating the disease activity of AOSD. FDG-PET/CT was reported as a useful modality for evaluating the disease activity of AOSD [42], though not all facilities in this study have good access to FDG-PET/CT. Regarding biomarkers, elevated interleukin-1β, interleukin-6, and interleukin-18 were associated with a higher risk of MAS [12, 43]. Including those new items may improve the accuracy of the models by latent class analysis and Cox regression analysis in the future.
There were some limitations in this study. First, it was a retrospective study. There was no standardized treatment protocol, and treatments could influence outcomes as confounding factors. However, the multicenter design in this study might reduce treatment bias. Second, due to the small event number of deaths, we were unable to perform a multivariate analysis regarding the mortality risk. Third, our cohort lacked data about interleukin-1 inhibitors-use, though its efficacy for AOSD has already been demonstrated [44, 45]. Interleukin-1 inhibitors have not been approved for AOSD in Japan, while tocilizumab has been approved. Consequently, no patient in this study received interleukin-1 inhibitors.
Conclusions
In this retrospective study, we assessed the large cohort of AOSD patients with the detailed dataset. Latent class analysis identified the two subgroups of AOSD patients: the typical group and the elderly-onset group. However, outcomes were not significantly different between the two groups in terms of overall survival and relapse-free survival. Although the survival of AOSD was generally good, one-third of the patients in our cohort experienced relapses. In this study, only age ≧65 years at disease onset was identified as the risk factor for relapse.
Supplementary Information
Additional file 1: Supplementary Table 1. Patient characteristics according to presence/absence of macrophage activation syndrome. Supplementary Table 2. Selection of the number of classes in latent class analysis. Supplementary Table 3. Patient characteristics according to the latent classes.
Acknowledgements
We thank all staff in our hospitals for the care and management of patients enrolled in this study and for their support in data collection.
Abbreviations
- AOSD
Adult-onset Still’s disease
- sJIA
Systemic juvenile idiopathic arthritis
- ASD
Adult Still’s disease
- MAS
Macrophage activation syndrome
- DIC
Disseminated intravascular coagulation
- WBC
White blood cell count
- Hb
Hemoglobin
- ESR
Erythrocyte sedimentation rate
- AST
Aspartate aminotransferase
- ALT
Alanine aminotransferase
- LDH
Lactate dehydrogenase
- CRP
C-reactive protein
Authors’ contributions
Takahiro S and SF conceived and designed the study. Takahiro S, MH, SK, Yasuhiko K, Kei K, Yoshihisa K, Kazuhiro K, DN, YN, and Takao S collected the data. Takahiro S, SF, YI, Yohei K, and YS analyzed and interpreted the patient data. Takahiro S, SF, KI, and HN were the major contributors in writing the manuscript. The authors read and approved the final manuscript.
Funding
No specific funding was received from any funding bodies in the public, commercial, or not-for-profit sectors to carry out the work described in this article.
Availability of data and materials
Anonymized patient level data can be made available on reasonable request and after approval by a review panel. Requests should be made to shfuruta@gmail.com.
Declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of Chiba University School of Medicine (reference number: 3183). The ethics committee waived the requirement for patient’s written informed consent according to the local regulations for a retrospective observational study. All data were fully anonymized before being analyzed. The data were shared in accordance with the plan approved by the ethics committee, and only the data used in this specific study were provided. The study was performed in accordance with the Declaration of Helsinki.
Consent for publication
This was a retrospective observational study, and consent for publication was waived according to the local regulations for a retrospective observational study.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gerfaud-Valentin M, Jamilloux Y, Iwaz J, Seve P. Adult-onset Still’s disease. Autoimmun Rev. 2014;13:708–722. doi: 10.1016/j.autrev.2014.01.058. [DOI] [PubMed] [Google Scholar]
- 2.Cagatay Y, Gul A, Cagatay A, Kamali S, Karadeniz A, Inanc M, et al. Adult-onset Still’s disease. Int J Clin Pract. 2009;63:1050–1055. doi: 10.1111/j.1742-1241.2007.01393.x. [DOI] [PubMed] [Google Scholar]
- 3.Sampalis JS, Esdaile JM, Medsger TA, Jr, Partridge AJ, Yeadon C, Senecal JL, et al. A controlled study of the long-term prognosis of adult Still’s disease. Am J Med. 1995;98:384–388. doi: 10.1016/s0002-9343(99)80318-0. [DOI] [PubMed] [Google Scholar]
- 4.Still GF. On a form of chronic joint disease in children. Med Chir Trans. 1897;80:47–60.9. [PMC free article] [PubMed] [Google Scholar]
- 5.Bywaters EG. Still’s disease in the adult. Ann Rheum Dis. 1971;30(2):121–133. doi: 10.1136/ard.30.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kong XD, Xu D, Zhang W, Zhao Y, Zeng X, Zhang F. Clinical features and prognosis in adult-onset Still’s disease: a study of 104 cases. Clin Rheumatol. 2010;29:1015–1019. doi: 10.1007/s10067-010-1516-1. [DOI] [PubMed] [Google Scholar]
- 7.Kim YJ, Koo BS, Kim YG, Lee CK, Yoo B. Clinical features and prognosis in 82 patients with adult-onset Still’s disease. Clin Exp Rheumatol. 2014;32:28–33. [PubMed] [Google Scholar]
- 8.Cozzi A, Papagrigoraki A, Biasi D, Colato C, Girolomoni G. Cutaneous manifestations of adult-onset Still's disease: a case report and review of literature. Clin Rheumatol. 2016;35:1377–1382. doi: 10.1007/s10067-014-2614-2. [DOI] [PubMed] [Google Scholar]
- 9.Pay S, Turkcapar N, Kalyoncu M, Simsek I, Beyan E, Ertenli I, et al. A multicenter study of patients with adult-onset Still’s disease compared with systemic juvenile idiopathic arthritis. Clin Rheumatol. 2006;25:639–644. doi: 10.1007/s10067-005-0138-5. [DOI] [PubMed] [Google Scholar]
- 10.Fautrel B, Le Moel G, Saint-Marcoux B, Taupin P, Vignes S, Rozenberg S, et al. Diagnostic value of ferritin and glycosylated ferritin in adult onset Still’s disease. J Rheumatol. 2001;28:322–329. [PubMed] [Google Scholar]
- 11.Rosário C, Zandman-Goddard G, Meyron-Holtz EG, D’Cruz DP, Shoenfeld Y. The hyperferritinemic syndrome: macrophage activation syndrome, Still’s disease, septic shock and catastrophic antiphospholipid syndrome. BMC Med. 2013;11:185. doi: 10.1186/1741-7015-11-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jamilloux Y, Gerfaud-Valentin M, Martinon F, Belot A, Henry T, Seve P. Pathogenesis of adult-onset Still’s disease: new insights from the juvenile counterpart. Immunol Res. 2015;61:53–62. doi: 10.1007/s12026-014-8561-9. [DOI] [PubMed] [Google Scholar]
- 13.Mehta BY, Ibrahim S, Briggs W, Efthimiou P. Racial/Ethnic variations in morbidity and mortality in Adult Onset Still’s Disease: an analysis of national dataset. Semin Arthritis Rheum. 2019;49:469–473. doi: 10.1016/j.semarthrit.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 14.Sakata N, Shimizu S, Hirano F, Fushimi K. Epidemiological study of adult-onset Still’s disease using a Japanese administrative database. Rheumatol Int. 2016;36:1399–1405. doi: 10.1007/s00296-016-3546-8. [DOI] [PubMed] [Google Scholar]
- 15.Efthimiou P, Kadavath S, Mehta B. Life-threatening complications of adult-onset Still’s disease. Clin Rheumatol. 2014;33:305–314. doi: 10.1007/s10067-014-2487-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arlet JB, Le TH, Marinho A, Amoura Z, Wechsler B, Papo T, et al. Reactive haemophagocytic syndrome in adult-onset Still’s disease: a report of six patients and a review of the literature. Ann Rheum Dis. 2006;65:1596–1601. doi: 10.1136/ard.2005.046904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ramos-Casals M, Brito-Zerón P, López-Guillermo A, Khamashta MA, Bosch X. Adult haemophagocytic syndrome. Lancet. 2014;383:1503–1516. doi: 10.1016/S0140-6736(13)61048-X. [DOI] [PubMed] [Google Scholar]
- 18.Kumakura S, Murakawa Y. Clinical characteristics and treatment outcomes of autoimmune-associated hemophagocytic syndrome in adults. Arthritis Rheum. 2014;66:2297–2307. doi: 10.1002/art.38672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Perez MG, Rodwig FR., Jr Chronic relapsing thrombotic thrombocytopenic purpura in adult onset Still’s disease. South Med J. 2003;96:46–49. doi: 10.1097/01.SMJ.0000047763.56451.F0. [DOI] [PubMed] [Google Scholar]
- 20.Gopal M, Cohn CD, McEntire MR, Alperin JB. Thrombotic thrombocytopenic purpura and adult onset Still’s disease. Am J Med Sci. 2009;337:373–376. doi: 10.1097/MAJ.0b013e318191436e. [DOI] [PubMed] [Google Scholar]
- 21.Zheng XL, Kaufman RM, Goodnough LT, Sadler JE. Effect of plasma exchange on plasma ADAMTS13 metalloprotease activity, inhibitor level, and clinical outcome in patients with idiopathic and nonidiopathic thrombotic thrombocytopenic purpura. Blood. 2004;103:4043–4049. doi: 10.1182/blood-2003-11-4035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheema GS, Quismorio FP., Jr Pulmonary involvement in adult-onset Still’s disease. Curr Opin Pulm Med. 1999;5:305–309. doi: 10.1097/00063198-199909000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Cush JJ, Medsger TA, Jr, Christy WC, Herbert DC, Cooperstein LA. Adult-onset Still’s disease. Clinical course and outcome. Arthr Rheum. 1987;30:186–194. doi: 10.1002/art.1780300209. [DOI] [PubMed] [Google Scholar]
- 24.Yamaguchi M, Ohta A, Tsunematsu T, Kasukawa R, Mizushima Y, Kashiwagi H, et al. Preliminary criteria for classification of adult Still's disease. J Rheumatol. 1992;19:424–430. [PubMed] [Google Scholar]
- 25.Filipovich AH. Hemophagocytic lymphohistiocytosis (HLH) and related disorders. Hematol Am Soc Hematol Educ Program. 2009:127–31. https://ashpublications.org/hematology/article/2009/1/127/19872/Hemophagocytic-lymphohistiocytosis-HLH-and-related. [DOI] [PubMed]
- 26.Henter JI, Elinder G, Ost A. Diagnostic guidelines for hemophagocytic lymphohistiocytosis. The FHL Study Group of the Histiocyte Society. Semin Oncol. 1991;18:29–33. [PubMed] [Google Scholar]
- 27.Henter JI, Horne A, Arico M, Egeler RM, Filipovich AH, Imashuku S, et al. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48:124–131. doi: 10.1002/pbc.21039. [DOI] [PubMed] [Google Scholar]
- 28.Fardet L, Galicier L, Lambotte O, Marzac C, Aumont C, Chahwan D, et al. Development and validation of the HScore, a score for the diagnosis of reactive hemophagocytic syndrome. Arthritis Rheum. 2014;66:2613–2620. doi: 10.1002/art.38690. [DOI] [PubMed] [Google Scholar]
- 29.Pouchot J, Sampalis JS, Beaudet F, Carette S, Décary F, Salusinsky-Sternbach M, et al. Adult Still’s disease: manifestations, disease course, and outcome in 62 patients. Medicine (Baltimore) 1991;70:118–136. [PubMed] [Google Scholar]
- 30.Colina M, Zucchini W, Ciancio G, Orzincolo C, Trotta F, Govoni M. The evolution of adult-onset Still disease: an observational and comparative study in a cohort of 76 Italian patients. Semin Arthritis Rheum. 2011;41:279–285. doi: 10.1016/j.semarthrit.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 31.Collins LM, Lanza ST. Latent class and latent transition analysis: with applications in the social, behavioral, and health sciences. Hoboken: Wiley; 2009. [Google Scholar]
- 32.Lanza ST, Collins LM, Lemmon DR, Schafer JL. PROC LCA: a SAS procedure for latent class analysis. Struct Equ Model Multidiscip J. 2007;14:671–694. doi: 10.1080/10705510701575602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ruscitti P, Cipriani P, Masedu F, Iacono D, Ciccia F, Liakouli V, et al. Adult-onset Still’s disease: evaluation of prognostic tools and validation of the systemic score by analysis of 100 cases from three centers. BMC Med. 2016;14:194. doi: 10.1186/s12916-016-0738-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bae CB, Jung JY, Kim HA, Suh CH. Reactive hemophagocytic syndrome in adult-onset Still disease: clinical features, predictive factors, and prognosis in 21 patients. Medicine (Baltimore) 2015;94:e451. doi: 10.1097/MD.0000000000000451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ruscitti P, Iacono D, Ciccia F, Emmi G, Cipriani P, Grembiale RD, et al. Macrophage activation syndrome in patients affected by adult-onset still disease: analysis of survival rates and predictive factors in the Gruppo Italiano di Ricerca in Reumatologia Clinica e Sperimentale Cohort. J Rheumatol. 2018;45:864–872. doi: 10.3899/jrheum.170955. [DOI] [PubMed] [Google Scholar]
- 36.Kim HA, Sung JM, Suh CH. Therapeutic responses and prognosis in adult-onset Still’s disease. Rheumatol Int. 2012;32:1291–1298. doi: 10.1007/s00296-011-1801-6. [DOI] [PubMed] [Google Scholar]
- 37.Asanuma YF, Mimura T, Tsuboi H, Noma H, Miyoshi F, Yamamoto K, et al. Nationwide epidemiological survey of 169 patients with adult Still’s disease in Japan. Mod Rheumatol. 2015;25:393–400. doi: 10.3109/14397595.2014.974881. [DOI] [PubMed] [Google Scholar]
- 38.Wang R, Li T, Ye S, Tan W, Zhao C, Li Y, et al. Macrophage activation syndrome associated with adult-onset Still’s disease: a multicenter retrospective analysis. Clin Rheumatol. 2020;39:2379–2386. doi: 10.1007/s10067-020-04949-0. [DOI] [PubMed] [Google Scholar]
- 39.Lee YH. Tocilizumab in patients with adult-onset Still’s disease refractory to glucocorticoid treatment. Ann Rheum Dis. 2019;78:e133. doi: 10.1136/annrheumdis-2018-214635. [DOI] [PubMed] [Google Scholar]
- 40.Lenert A, Oh G, Ombrello MJ, Kim S. Clinical characteristics and comorbidities in adult-onset Still’s disease using a large US administrative claims database. Rheumatology (Oxford) 2020;59:1725–1733. doi: 10.1093/rheumatology/kez622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Berardicurti O, Conforti A, Iacono D, Pantano I, Caso F, Emmi G, et al. Dissecting the clinical heterogeneity of adult-onset Still’s disease, results from a multi-dimensional characterisation and stratification. Rheumatology (Oxford). 2021;keaa904. 10.1093/rheumatology/keaa904 Online ahead of print. [DOI] [PubMed]
- 42.Yamashita H, Kubota K, Takahashi Y, Minamimoto R, Morooka M, Kaneko H, et al. Clinical value of (1)(8)F-fluoro-dexoxyglucose positron emission tomography/computed tomography in patients with adult-onset Still’s disease: a seven-case series and review of the literature. Mod Rheumatol. 2014;24:645–650. doi: 10.3109/14397595.2013.850998. [DOI] [PubMed] [Google Scholar]
- 43.Maria AT, Le Quellec A, Jorgensen C, Touitou I, Rivière S, Guilpain P. Adult onset Still's disease (AOSD) in the era of biologic therapies: dichotomous view for cytokine and clinical expressions. Autoimmun Rev. 2014;13:1149–1159. doi: 10.1016/j.autrev.2014.08.032. [DOI] [PubMed] [Google Scholar]
- 44.Kedor C, Listing J, Zernicke J, Weiss A, Behrens F, Blank N, et al. Canakinumab for Treatment of Adult-Onset Still’s Disease to Achieve Reduction of Arthritic Manifestation (CONSIDER): phase II, randomised, double-blind, placebo-controlled, multicentre, investigator-initiated trial. Ann Rheum Dis. 2020;79:1090–1097. doi: 10.1136/annrheumdis-2020-217155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Giampietro C, Ridene M, Lequerre T, Costedoat Chalumeau N, Amoura Z, Sellam J, et al. Anakinra in adult-onset Still’s disease: long-term treatment in patients resistant to conventional therapy. Arthritis Care Res. 2013;65:822–826. doi: 10.1002/acr.21901. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary Table 1. Patient characteristics according to presence/absence of macrophage activation syndrome. Supplementary Table 2. Selection of the number of classes in latent class analysis. Supplementary Table 3. Patient characteristics according to the latent classes.
Data Availability Statement
Anonymized patient level data can be made available on reasonable request and after approval by a review panel. Requests should be made to shfuruta@gmail.com.