Residents and staff of long-term care facilities (LTCFs) have been prioritized by the Advisory Committee on Immunization Practices for vaccination in the initial COVID-19 vaccine allocation phase in the US.1 Residents and staff of LTCFs, who live and work in congregate settings, are at increased risk for infection with SARS-CoV-2,2 and residents, given their advanced age and/or underlying chronic medical conditions, are at increased risk for severe outcomes.3
To facilitate vaccination of LTCF residents and staff, the Centers for Disease Control and Prevention (CDC) launched the Pharmacy Partnership for Long-Term Care Program4 in December 2020. This public-private partnership between CDC, CVS Pharmacy, Managed Health Care Associates Inc, and Walgreens provides on-site COVID-19 vaccination of residents and staff members at enrolled LTCFs, including skilled nursing facilities (SNFs), assisted living facilities, and other LTCFs across 54 jurisdictions (49 states, 4 cities, and 1 territory). Pharmacy partners provide comprehensive management of the vaccination process to include scheduling, cold chain management, patient counseling, and administration. This Insights describes estimated rates of early receipt of vaccine among residents and staff during the first month of the program, as recently reported in MMWR.5
For this report, COVID-19 vaccine administration data were restricted to enrolled SNFs with a unique, valid Centers for Medicare & Medicaid Services (CMS) certification number and with an on-site vaccination clinic during the first month of the program (December 18, 2020-January 17, 2021). The number of residents eligible for vaccination was estimated using the mean weekly resident census counts for each facility during December 14, 2020, through January 17, 2021, from the National Healthcare Safety Network; the number of staff members eligible for vaccination was estimated using counts of unique staff members for each facility in July through September 2020 from the CMS Payroll-Based Journal. Inclusion criteria for national vaccination estimates were all CMS-certified SNFs with available denominator data and at least 1 on-site clinic in the first month of the program. Inclusion criteria for jurisdiction-level estimates were those in which more than 50 CMS-certified SNFs had at least 1 on-site clinic in the first month of the program. Data for participating cities were combined with those of their state for jurisdiction-level estimates. This activity was reviewed by CDC and was consistent with applicable federal law and CDC policy.
During December 18, 2020-January 17, 2021, among 12 702 CMS-certified SNFs enrolled in the Pharmacy Partnership for Long-Term Care Program, 11 460 (90.2%) had at least 1 on-site vaccination clinic through the program. A total of 713 909 residents and 582 104 staff members received at least a first dose of COVID-19 vaccine; administration of second doses was not analyzed. Among 11 376 (99.3%) facilities with available resident census data, the median estimated percentage of residents vaccinated per facility was 77.8% (IQR, 61.3%−93.1%), and among 11 134 (97.2%) facilities with available payroll data, the median estimated percentage of staff vaccinated was 37.5% (IQR, 23.2%−56.8%). Among 40 states that met inclusion criteria for jurisdiction-level estimates, the median percentage of residents vaccinated per facility by state ranged from 65.7% to more than 100% and of staff members, from 19.4% to 67.4% (Figure).
Figure.
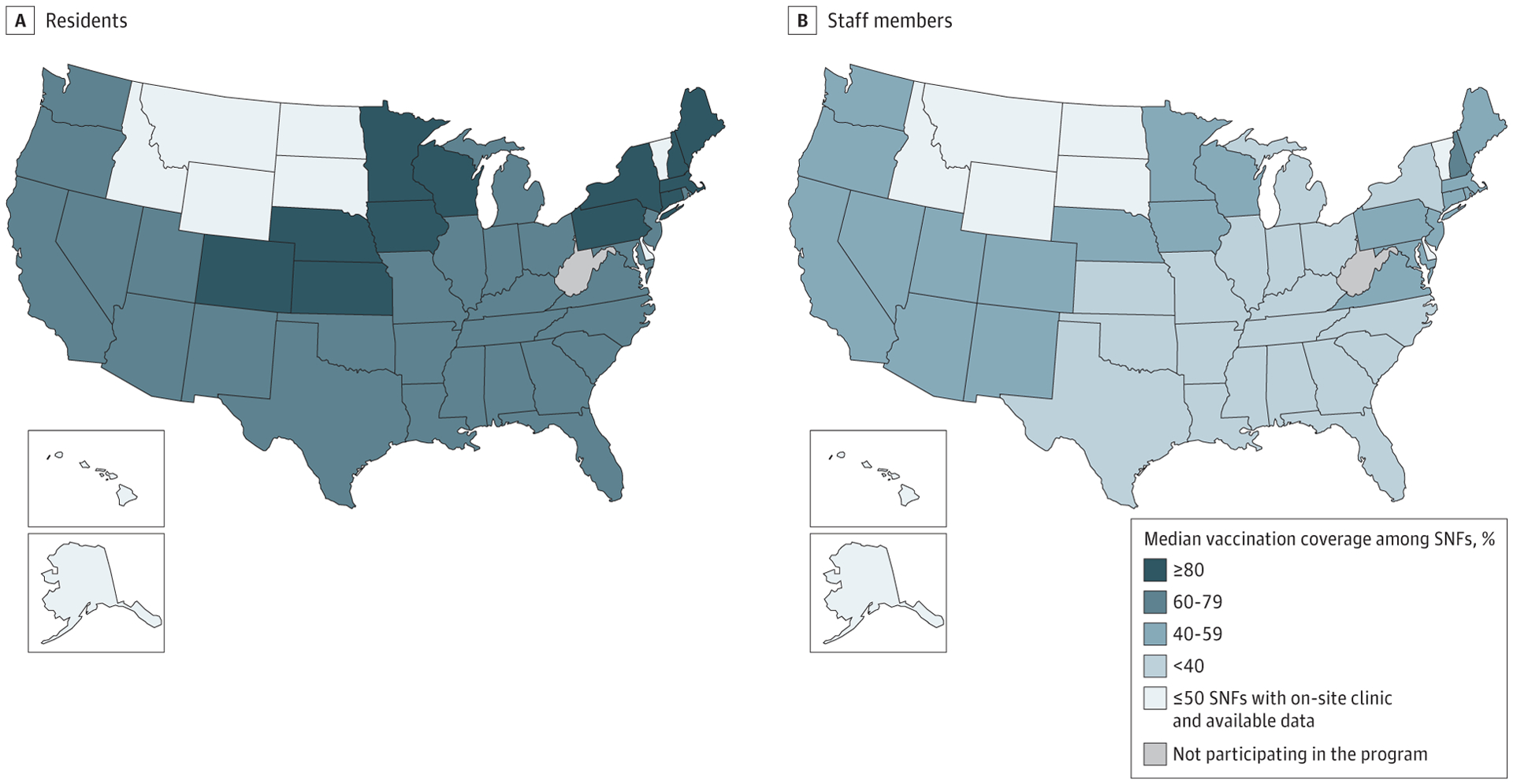
Estimated Median Percentage of Residents and Staff Members at SNFs Enrolled in the Pharmacy Partnership for Long-Term Care Program Who Received at Least 1 Dose of COVID-19 Vaccine, by Jurisdiction—United States, December 18, 2020-January 17, 2021
Includes skilled nursing facilities (SNFs) with at least 1 on-site clinic conducted through the Pharmacy Partnership for Long-Term Care Program, December 18, 2020-January 17, 2021. Only jurisdictions with >50 CMS-certified SNFs with a vaccination clinic conducted during the first month of the program and available denominator data (n = 40 states) are shown. The number of residents eligible for vaccination was estimated using the mean of National Healthcare Safety Network weekly resident census counts for each facility during December 14, 2020-January 17, 2021 (11 376 facilities). The number of staff members eligible for vaccination was estimated using CMS Payroll-Based Journal counts of unique staff members for each facility during July-September 2020 (11 134 facilities). Estimates reflect staff members vaccinated through the Pharmacy Partnership for Long-Term Care Program; additional staff members might have been vaccinated through other programs.
Reproduced from MMWR.5
Even though the program achieved moderately high vaccination coverage among residents, the lower coverage among staff members is concerning because this population is at occupational risk for exposure to SARS-CoV-2. Low coverage among staff members working in LTCFs has also been described for influenza vaccination. During the 2017–2018 influenza season, vaccination coverage among LTCF staff was lower than that among other health care workers, with rates of 67.4% for long-term care settings vs 91.9% for hospitals, 75.1% for ambulatory care, and 74.9% for other clinical settings.6 Survey data suggest that vaccine hesitancy among this population could be associated with skepticism about influenza vaccine effectiveness and perceived low risk of virus transmission.7 Although efforts are ongoing to promote confidence in COVID-19 vaccination among health care workers, challenges persist. A November 2020 survey found that only 45% of respondents who worked in LTCFs were willing to receive a COVID-19 vaccine immediately once available, and an additional 24% would consider it in the future; the most common reason for hesitancy was concern about adverse effects.8 High staff turnover, staff members working in multiple facilities, and limited resources for staff outreach and education might also be barriers to vaccination.9
The findings in this report are subject to limitations. First, the percentage of staff members vaccinated could have been underestimated because some might received vaccination elsewhere, or vaccination might have been intentionally staggered. Second, the number of residents and staff eligible for vaccination at each facility was estimated using secondary data sources and not captured in real time at each clinic. Variation in facility occupancy, resident and staff turnover, and other variability could affect the accuracy of these denominator estimates. Third, these estimates evaluated only the first month of the program among CMS-certified SNFs; vaccination coverage might have increased with subsequent clinics and may not be generalizable to all other LTCFs in the program (eg, assisted living facilities). Fourth, no qualitative data were collected to assess motivators for vaccination or to characterize possible vaccine hesitancy suggested by the low percentage of staff members vaccinated. Fifth, data on adherence with second vaccine dose administration is not reported, and it is unknown whether rates will be comparable with those for initial dose administration.
Use of focused communication to increase COVID-19 vaccine confidence among LTCF staff members10 might help improve vaccination acceptance and coverage. Staff members serve as a trusted source of information for patients and residents and, particularly in LTCF settings where residents and staff might be vaccinated simultaneously, increasing vaccine confidence among staff members might have additional benefits for promoting vaccination among residents. Strategies to address structural barriers, such as scheduling around shift work or provision of paid sick leave for possible postvaccination adverse effects, should also be encouraged. Because coverage varied among jurisdictions, lessons learned from jurisdictions or individual facilities with high coverage might provide insight into strategies that could be applied more broadly. Further studies should explore differential vaccination coverage by characteristics including geographic location, sociodemographic factors, and facility size, as well as characterize barriers to vaccination of persons working in LTCFs. Continued development and implementation of focused communication and outreach strategies are needed to improve vaccination coverage among this priority population.
Footnotes
Conflict of Interest Disclosures: None reported.
Additional Contributions: We thank collaborators from the CDC COVID-19 Response Team; CDC Division of Healthcare Quality Promotion, CMS; American Health Care Association; and participating pharmacies, health departments, and long-term care facilities.
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of CDC.
REFERENCES
- 1.Dooling K, McClung N, Chamberland M, et al. The Advisory Committee on Immunization Practices’ interim recommendation for allocating initial supplies of COVID-19 vaccine—United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(49):1857–1859. doi: 10.15585/mmwr.mm6949e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Medicare & Medicaid Services. COVID-19 nursing home data. January 31, 2021. Accessed February 17, 2021. https://data.cms.gov/stories/s/COVID-19-Nursing-Home-Data/bkwz-xpvg
- 3.CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69 (12):343–346. doi: 10.15585/mmwr.mm6912e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Understanding the Pharmacy Partnership for Long-Term Care Program. Updated January 7, 2021. https://www.cdc.gov/vaccines/covid-19/long-term-care/pharmacy-partnerships.html
- 5.Gharpure R, Guo A, Bishnoi CK, et al. Early COVID-19 first-dose vaccination coverage among residents and staff members of skilled nursing facilities participating in the Pharmacy Partnership for Long-Term Care Program—United States, December 2020-January 2021. MMWR Morb Mortal Wkly Rep. 2021;70(5):178–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Black CL, Yue X, Ball SW, et al. Influenza vaccination coverage among health care personnel—United States, 2017–18 influenza season. MMWR Morb Mortal Wkly Rep. 2018;67(38):1050–1054. doi: 10.15585/mmwr.mm6738a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daugherty JD, Blake SC, Grosholz JM, et al. Influenza vaccination rates and beliefs about vaccination among nursing home employees. Am J Infect Control. 2015;43(2):100–106. [DOI] [PubMed] [Google Scholar]
- 8.Unroe KT, Evans R, Weaver L, et al. Willingness of long-term care staff to receive a COVID-19 vaccine: a single state survey. J Am Geriatr Soc. Published online December 28, 2020. [DOI] [PubMed] [Google Scholar]
- 9.Jaklevic MC. Nursing homes’next test—vaccinating workers against COVID-19. JAMA. 2020;324(19):1928–1930. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Long-Term Care Facility Toolkit: preparing for COVID-19 vaccination at your facility. December 23, 2020. https://www.cdc.gov/vaccines/covid-19/toolkits/long-term-care/index.html [Google Scholar]


