Abstract
Background
Depressive disorders are common in old age, with serious health consequences such as increased morbidity, disability, and mortality. The frailty of elderly people may seriously hamper the efficacy and safety of pharmacotherapy. Therefore, electroconvulsive therapy (ECT) may be an alternative to treatment with antidepressants.
Objectives
To assess the efficacy and safety of ECT compared to simulated ECT or antidepressants in depressed elderly people.
Search methods
We searched the CCDAN Controlled Trials Register on 21/1/2007, MEDLINE 1966‐2006, EMBASE 1980‐2006, Biological abstracts 1985‐2006, CINAHL 1982‐2006, Lilacs from 1982 onwards, Psyclit 1887‐2006, Sigle 1980‐2006. Reference lists of relevant papers were scanned. The Journal of ECT, the International Journal of Geriatric Psychiatry and the American Journal of Geriatric Psychiatry were handsearched.
Selection criteria
Randomised controlled trials of ECT for elderly people (>60 years) with depression, with or without concomitant conditions such as cerebrovascular disease, dementia (including Alzheimer's type and vascular) and Parkinson's disease were included.
Data collection and analysis
Data were independently extracted by at least two review authors. Weighted mean differences (WMD) between groups were calculated for continuous data.
Main results
Randomised evidence was sparse. Only four trials were eligible for inclusion, one comparing the efficacy of real ECT versus simulated ECT, two comparing the efficacy of unilateral versus bilateral ECT and the other comparing the efficacy of ECT once a week with ECT three times weekly. All trials had major methodological shortcomings; reports were mostly lacking essential information to perform a quantitative analysis. Although the findings from one study (35 participants) concluded that real ECT was superior to simulated ECT, these conclusions need to be interpreted cautiously. Only results from one of the trials (29 participants) comparing unilateral versus bilateral ECT could be analysed, and did not show convincing efficacy of unilateral ECT over bilateral ECT, WMD 6.06 (CI ‐5.20 to 17.32). Randomised evidence on the efficacy and safety of ECT in depressed elderly with concomitant dementia, cerebrovascular disorders or Parkinson's disease was lacking completely. Possible side‐effects could not be adequately examined because of the lack of randomised evidence and methodological shortcomings.
Authors' conclusions
None of the objectives of this review could be adequately tested because of the lack of firm, randomised evidence. Given the specific problems in the treatment of depressed elderly, a well designed randomised controlled trial should be conducted in which the efficacy of ECT is compared to one or more antidepressants.
Plain language summary
Electroconvulsive therapy (ECT) for depression in elderly people
Antidepressant drugs often cause side effects in elderly people, which may limit the effectiveness of treatment for depression. ECT can be an important alternative to drug treatment for depressed elderly people. This review involved searching the literature for well‐conducted (randomised) studies that compared ECT to both simulated ECT and to antidepressants. The review found only four studies, all of which had serious problems in their methods. At present, therefore, it is not possible to draw firm conclusions on whether ECT is more effective than antidepressants,.or on the safety or side effects of ECT in elderly people with depression.
Background
The prevalence of depressive disorders in older people in the community is around 12.5%. This includes both major and minor depressive disorders and dysthymic disorder (a chronic form of depression). The prevalence of major depressive disorder in people over the age of sixty is estimated to be around two percent (Beekman 1999). The prevalence of depression in people suffering from dementia, Parkinson's disease and cerebrovascular accidents is higher. The burden of depression both to the individual and to society is huge. Depression in the elderly is accompanied by a high (cardiovascular) mortality (Frasure‐Smith 1993; Penninx 1999) and has a negative effect on well‐being and daily functioning (Ormel 1999).
Depression in late life is thought to differ from depression in younger subjects in etiology, presentation, treatment and outcome. Although social, psychological, physical and biological factors interact, depression in the elderly is only partly explained by risk factors like physical health, life events, social support and personality (Beekman 2000). Biological factors may play an important role in the etiology of late‐life depression, and this may be of particular significance in some subgroups of the depressed elderly. It is not clear how these factors interact, but hyperactivity of the hypothalamic‐pituitary‐adrenocortical (HPA) system and an increased production of immune‐mediated cytokines like interleukin‐6 (IL‐6) may be major biological risk factors in the pathogenesis of depression (Holsboer 1995; Maes 1995; Song 1998). Old age is accompanied by increased activity of the HPA‐system independent of the occurrence of depression (Deuschle 1997). Psychosocial stress factors induce even stronger HPA‐system hyperactivity (Holsboer 1996). The high prevalence of depression in the elderly may thus be explained by the effect of psychosocial stress factors on the HPA‐system, which finally lead to depression. Cerebrovascular disorders also are a risk factor of major importance in the pathogenesis of late life depression (Alexopoulos 1997). Lacunar and cortical infarcts occur regularly in elderly people with depression. So‐called white matter hyperintensities appear often on MRI‐scans of depressive elderly people (Alexopoulos 1997). These white matter hyperintensities may have a vascular pathogenesis (Pantoni 1995; Pantoni 1997). Depression in older people with concomitant cerebrovascular disorders is therefore sometimes called 'vascular depression' (Alexopoulos 1997).
There are two major forms of biological treatment for late‐life depression: antidepressants and electroconvulsive therapy (ECT). Various antidepressants are now being marketed, and their efficacy is the topic of two Cochrane systematic reviews (Mottram 2006; Wilson 2001). It is generally acknowledged that older, frail depressed patients are particularly prone to the side effects of antidepressants. Cardio‐vascular side effects of antidepressants occur more often in older than younger patients (Woodhouse 1992). Many of these drugs also have serious anticholinergic side‐effects (Moskowitz 1986), that may seriously affect compliance with treatment. Although approximately 50‐60% of patients are thought to improve clinically as a consequence of antidepressant treatment (Schneider 1995), in subgroups of the depressed elderly, the efficacy of antidepressants may be lower. For example, white matter hyperintensities and lacunar infarcts on MRI‐scan are thought to markedly affect the outcome of treatment with antidepressants (Simpson 1997; Simpson 1998).
ECT involves the application of an electric current to the head with the aim of inducing a controlled tonic clonic convulsion, and is usually carried out at intervals of days. Although the efficacy of ECT has been established in a considerable number of studies, it is still a controversial treatment. The use of ECT is subject to legal restriction in some parts of the world. Some reports suggest that ECT is particularly effective in late‐life depression (Flint 1998), and that it is effective in therapy‐resistant depressive elderly people with extensive white matter hyperintensities (Coffey 1988). Currently there is no evidence to suggest that ECT causes any kind of brain damage, although temporary cognitive impairment is frequently reported (Devanand 1994; Scott 1995). ECT seems to be a safe procedure, even in the elderly with cardiovascular disorders (Rice 1994). ECT is used to treat the depressed elderly more frequently, and its use is declining less rapidly, than in the general population (Glen 1999).
ECT may be safer and more effective than antidepressants in the treatment of late life depression. This greater efficacy may be more pronounced in subgroups of the depressed elderly who suffer from co‐morbid cerebrovascular disorders, dementia and Parkinson's disease. A systematic review to summarise all available high quality evidence on the effectiveness of ECT for depressed elderly people is called for, in order to inform treatment decisions in this population.
Objectives
To perform a systematic review and meta‐analysis on the evidence for the efficacy of ECT in late life depression, and to assess the methodological quality and generalisability of the trials in this area.
The primary objectives of this review were: To test the hypothesis that modified real ECT has a greater and/or more rapid antidepressant effect than simulated (sham) ECT, antidepressant drug treatment or non‐pharmacological interventions in the early phase (the first six weeks) and longer term (six months post treatment) treatment of late life depression.
The secondary objectives of this review were: 1. To determine whether ECT produces a differential response in depressed, elderly patients with concomitant conditions including: a) evidence of cerebrovascular disorders (cortical and lacunar infarcts, and white matter hyperintensities) b) dementia of the Alzheimer's type or vascular dementia c) Parkinson's disease.
2. To determine the effect of electrode placement (unilateral versus bilateral forms of ECT) and dosage (both the amount of energy supplied and the frequency of ECT‐application) on the efficacy of ECT in late life depression
3. To examine the immediate and long‐term side effects, and in particular, the cognitive side effects of ECT in the depressed elderly.
Methods
Criteria for considering studies for this review
Types of studies
Randomised and non‐randomised (observational studies, retrospective studies and case series) evidence was obtained. The review and meta‐analysis included randomised controlled trials only. The results of non‐randomised studies were not summarised in this review, and have been summarised separately in a narrative review (van der Wurff 2003).
Types of participants
Patients were included in the review if diagnosed as suffering from major depression by any criteria, including primary depressive illness with psychotic features. Patients with a primary diagnosis of schizophrenia, schizoaffective disorders or bipolar disorders were excluded. The review included depressive patients suffering from concomitant conditions, including dementia of the Alzheimer's type, vascular or multi‐infarct dementia, Parkinson's disease and cerebrovascular disorders.
Trials that included subjects under the age of 60 were excluded, unless data concerning subjects over the age of 60 were analysed separately.
Types of interventions
The intervention of interest was unilateral or bilateral ECT, that is, the electrical induction of cerebral seizure activity after the intravenous induction of a brief general anaesthesia and the pre‐administration of a skeletal muscle relaxant drug. Trials that evaluated the acute phase treatment of depression were included. Trials that examined the effectiveness of maintenance ECT were excluded.
For the primary objectives, trials were included that compared the application of ECT with: 1. "sham‐ECT" or "simulated‐ECT" 2. treatment with antidepressants 3. non‐pharmacological forms of treatment 4. any other form of placebo treatment.
For the secondary objectives, trials were included that compared the application of: 1. ECT applied in groups of depressed elderly with or without concomitant conditions including Parkinson's disease, dementia of the Alzheimer's type, vascular or multi‐infarct dementia and cerebrovascular disorders 2. unilateral versus bilateral ECT 3. ECT applied at different energy levels 4. ECT applied at different frequencies, for example once or twice weekly.
Types of outcome measures
The primary outcome measure to assess antidepressant efficacy was the reduction in symptoms of depressive illness measured as changes in scores from baseline. It was anticipated that reduction in symptoms would be measured on: 1. continuous symptom scales like the Hamilton Rating Scale for Depression (HRDS) (Hamilton 1960), the Montgomery Asberg Depression Rating Scale (MADRS)(Montgomery 1979), the Clinical Global Inventory (CGI) which were then analysed as a continuous variable, or 2. clinical global outcome measures such as "recovered" , "much improved" or "not improved". For trials in which categorical outcome data were available, these were summarised as the number of people who experienced those outcomes in each comparison group and the total number in each group, and were then analysed as a dichotomous variable.
Secondary outcome measures to assess efficacy were if possible determined by: 1. the number of patients in each group who showed significant clinical improvement in the long term (six months post treatment), either measured as a decline in symptoms on continuous scales like the HRDS, MADRS, CGI or dichotomous variables like "recovered", "much improved" or "not‐improved"; 2. the number of drop‐outs 3. cause‐specific and non‐specific mortality 4. suicide 5. functional outcomes like quality of life and cognitive functioning.
The main outcome measures for assessing side effects in controlled trials were: 1. cause specific mortality 2. severe somatic complications like myocardial and cerebral disorders 3. immediate and long‐term cognitive disorders like disorders in attention, orientation and memory measured on the Mini Mental State Examination (MMSE) or any other neuropsychological instruments.
Search methods for identification of studies
The original search was performed in collaboration with John Geddes and others, who were kind enough to share their search results with us. The Geddes' group have conducted a review on the safety and efficacy of ECT for depressive illness, but not specifically in the elderly. Therefore a two‐stage search process was used for our review.
A. Firstly, we used the search results of Geddes et al. The search strategy was as follows: 1. An updating search of the Cochrane Controlled Trials Register and the Cochrane Collaboration Depression Anxiety and Neurosis Controlled Trials Register was carried out on 12/1/2007 using the search terms Diagnosis Depress or Dysthymi or "Adjustment Disorder*" or "Mood Disorder*" or "Affective Disorder" or "Affective Symptoms" and Age Group Aged and Intervention "Electroconvulsive Therapy" In addition CCDANCTR‐References were searched on 12/1/2007 with Keyword Depress* or Dysthymi* or "Adjustment Disorder*" or "Mood Disorder*" or "Affective Disorder*" or "Affective Symptoms" And Free‐text Elder or Geriatri or Senil or Older or "Old Age" or "Late Life" or "Aged, 80‐And‐Over" And Free‐text Electr or ECT
2. In addition a number of other electronic databases were searched using the CCDAN search strategy: Biological abstracts 1985‐2006 CINAHL 1982‐2006 EMBASE 1980‐2006 Lilacs from 1982 onwards MEDLINE 1966‐2006 PsycLIT 1887‐2006 Sigle 1980‐2006 2 We searched reference lists of the handbooks on ECT by Abrams and Fink and the latest APA Guidelines. 3. We handsearched the Journal of ECT/Convulsive Therapy. More than 3000 references resulted from this process, of which John Geddes' group selected just under 600 studies initially satisfying their inclusion criteria. These references were held on Reference Manager Version 9 and this database was shared with us. One of us (FvdW) searched this database for references in which elderly or aged were used as keywords or appeared in the abstract.
B. Due to the difficulty in locating trials in older people, additional electronic and hand searches were done by the authors (FvdW and MS). In this additional searching, the target was to locate randomised and non‐randomised (observational studies, retrospective studies, case series, case reports) evidence on ECT in depressed elderly. 1. The CCDAN and CCTR was searched using "electroconvuls*" or "electro‐convuls*" or "electroshock*" or "electro‐shock*" or "convuls*" or "ECT" and senil* or geriatr* or older or elder* or late‐life or later‐life or "late* life" as search terms. 2. The following databases were additionally searched using the CCDAN Controlled Trials Register search strategy in combination with search terms on elderly, dementia, cerebrovascular disorders and Parkinson's disease, case reports, case series, retrospective studies: Biological abstracts 1985‐2006 Cinahl 1982‐2006 EMBase 1980‐2006 Lilacs from 1982 onwards Medline 1966‐2006 Psyclit 1887‐2006 Sigle 1980‐2006 2. We searched reference lists of the chapter on "Electroconvulsive Therapy in late‐life depression" by Harold Sackeim in the handbook on Clinical Geriatric Psychopharmacology by Carl Salzman (Salzman 1992) and the chapter Electroconvulsive Therapy in the handbook on Late‐life depression by Roose and Sackeim (Roose 2004). 3. We handsearched the International Journal of Geriatric Psychiatry and the American Journal of Geriatric Psychiatry. 4. Additional searching of references cited in all included and excluded trials was carried out to identify any missing studies on the basis of the title. 5. C.H. Kellner, expert in the field, was asked whether he was aware of any additional eligible studies.
Through this process, more than 400 citations potentially fulfilling the inclusion criteria for the review were selected. The title, abstracts or full copy of these references were assessed independently by the first two reviewers for inclusion into the review. Following assessment of the references, 191 references that included ECT and depression (with or without dementia, cerebrovascular disorders or Parkinson's disease) in the elderly remained. Of these 191 references, the abstracts or full copy were assessed independently by FvdW and MS. An inter‐rater agreement (kappa) of 0.96 was obtained for inclusion into the review.
Data collection and analysis
Selection of studies The first review author identified the studies. The first two review authors independently assessed the relevance of each trial, blind to the decisions made by one another. Each trial was assessed against pre‐set criteria. In cases of disagreement, decisions were reached by consensus through open discussion. Based on the title of the publication and its abstract, and if necessary the complete article, irrelevant citations were excluded. Potential studies for inclusion (randomised and non‐randomised) were obtained in hard copy. Reasons for exclusion or inclusion were recorded. Review authors were not blinded for authorship of trials, journals and institutions from which articles came. The four review authors judged the relevance of the included trials independently. FvdW has a special interest in the topic of depression in the elderly with concomitant cerebrovascular disorders or dementia. MS has a special interest in ECT in late life depression. AB and WH are acknowledged experts in the field of late‐life depression. The latter two review authors were not involved in the search and identification phase. They were active in the selection process of included trials and in the editorial phase of the review.
Data collection Data were extracted from studies using a preset form. Data were entered into Review Manager software. Where data were missing, the principal investigator of the study was contacted for more information.
Methodological qualities of included studies We assessed the methodological quality of each trial according to the guidelines in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2005). Concealment of allocation was the main quality criterion for included studies. The adequacy of allocation concealment was rated as adequate (A), unclear (B) or inadequate (C) (for example an open list of random numbers, the use of alphabet or date of birth) or not used (D). Other major aspects on which the methodological quality were assessed included the blinding of participants and assessors; the adequacy of outcome assessment (intention to treat analysis (ITT)), and the adequacy of follow‐up assessments. Only trials in category A or B were included in the review.
Data and statistical analysis We hoped we would be able to find enough studies to be able to analyse data as described in the Cochrane Handbook. Categorical data would be transformed into dichotomous outcomes as described earlier. Relative risks, odds ratios and 95% confidence intervals would be calculated for the individual studies and pooled using the fixed effect model of Peto. The random effects method would then be used as a test for the robustness of the findings from the fixed effect analysis. We hoped to present data as 'the Number Needed to Treat" (NNT). In case continuous data were normally distributed, they would be analysed by calculating the weighted mean difference or the standardised mean difference depending on whether the same or different scales had been used for measuring outcome.
Sensitivity analysis When possible, we wished to investigate the effect of including or excluding studies with methodological shortcomings.
Subgroup analysis We hypothesised that clinical factors, such as the presence of co‐morbid cerebrovascular disorders would influence the outcome of trials. Therefore, our intention was to perform subgroup analyses to investigate whether there were differences in response between:
a) depressed elderly people with or without cerebrovascular disorders (cortical and lacunar infarcts, and white matter hyperintensities) b) depressed elderly people with or without dementia of the Alzheimer's type or vascular dementia c) depressed elderly people with or without Parkinson's disease.
Assessment of heterogeneity If a meta‐analysis was possible, the random effects model would be used to test the robustness of the findings from the fixed effect analysis. Statistical heterogeneity would be assessed through use of I‐squared test.
Publication bias It was planned to examine publication bias through the use of funnel plots.
Results
Description of studies
For substantive descriptions of studies please see "Characteristics of Included and Excluded Studies" tables. 1. General remarks Randomised evidence on ECT in elderly people was sparse. In the original version of the review, we were only able to select three trials that studied one of the primary or secondary objectives of this review (Fraser 1980. Kellner 1992, O'Leary 1994). The updating search identified one new trial for inclusion (Stoppe 2006). Only one controlled trial was found that investigated one of the primary objectives of this review, that is, the efficacy of real ECT to simulated ECT (O'Leary 1994). No controlled trials could be found that examined any of the other primary objectives of this review, for example the efficacy of ECT compared to antidepressants. Three RCTs investigated one of the secondary objectives of the review, two of which compared the efficacy of unilateral versus bilateral ECT (Fraser 1980, Stoppe 2006) and the third comparing the efficacy of ECT once a week with ECT three times weekly (Kellner 1992). Randomised evidence on the efficacy and safety of ECT in depressed elderly with concomitant dementia, cerebrovascular disorders or Parkinson's disease is lacking completely. One RCT that may meet the inclusion criteria for the review considering long term treatment (6 months) is awaiting further assessment (Kellner 2006). It reports on maintenance ECT versus pharmacotherapy with lithium and nortriptyline after a successful course of ECT. To date no separate analysis has been done in the elderly (> 60 years) in this study. Although randomised evidence is sparse and the four included trials had several methodological problems, we decided to present the reader with an overview of the different methodological aspects of the studies. In one comparison a quantitative analysis on the data was performed (the effectiveness of unilateral versus bilateral ECT). In case this quantitative analysis was not possible, the major results were summarised as reported by the investigators for each study.
All other identified studies consisted of non‐randomised evidence, including observational studies, retrospective studies, case reports and case series. As stated earlier, the findings have been summarised separately in a narrative review (van der Wurff 2003).
2. Excluded studies We excluded 187 studies. One study was an open trial without a control group. Thirty‐five were prospective, mostly naturalistic follow‐up studies, but without randomisation or control conditions. Thirty‐six were excluded because they were retrospective studies and fifty‐one because they concerned case‐reports. Another 64 studies were excluded, either because they were reviews or because they did not fulfil our inclusion criteria (for example they examined the effectiveness of maintenance ECT, or the effectiveness of ECT on the motor symptoms of Parkinson's disease without concomitant depressive disorder, or considered epidemiological aspects of ECT in the elderly).
3. Included studies For the primary objective, only one RCT meeting our inclusion criteria was found (O'Leary 1994). Some remarks need to be made concerning this study. This study was a post‐hoc analysis of data in elderly people who participated in the Nottingham trial on ECT (Gregory 1985). The Nottingham trial is an RCT in which the efficacy of ECT (unilateral and bilateral) was compared with simulated ECT in 69 patients, but not specifically the elderly. The presentation of the data in the O'Leary study was sparse, mean scores in the treatment conditions and/or standard deviations for the different comparisons the investigators performed were not available. Therefore we were not able to calculate a standardised mean difference, necessary to perform a quantitative analyses. We contacted the principal investigator in an attempt to obtain the relevant data to be able to perform a quantitative analysis. Because of the post‐hoc nature of the report and all the other methodological limitations, which we will describe, the results of this study need to be interpreted with caution. But because of the lack of randomised evidence for the primary objective of this review, we decided to include this study in the review and to provide the reader with its major results. There are a large number of non‐randomised studies on the primary and secondary objectives of our review, which are summarised separately in a narrative review (van der Wurff 2003)
For the secondary objectives we found three RCTs meeting our inclusion criteria. Fraser 1980 compared the efficacy of unilateral versus bilateral ECT. Stoppe 2006 compared fixed high‐dose unilateral ECT versus bilateral ECT for efficacy and effects on cognition. Kellner 1992 performed a randomised trial on the dosage of ECT comparing the efficacy of ECT weekly with ECT three times weekly. In only one of these studies could data be extracted for inclusion (Fraser 1980). In the study by Stoppe 2006, continuous data were only presented in graphs, and presentation of dichotomous data was limited to numbers of participants who were in remission at the end of the study, excluding partial response or no response. In addition, there was a marked difference in pre‐ECT MADRS scores between the compared groups of RUL ECT versus BL ECT. We have attempted to contact the trialists to obtain continuous data, but have not yet received a response. Data in the study by Kellner 1992 were sparse. Means and standard deviations were not reported. We contacted the principal investigator, who informed us that the necessary information to perform a quantitative analysis was not available. Again, because of the lack of randomised evidence, we decided to include these trials in the review, but our results need to be interpreted with caution because of the methodological problems that we will describe hereafter.
a. Length of included trials The Nottingham trial, from which O'Leary 1994 re‐analysed the data, took place between August 1981 and February 1983. The subgroup analysis of elderly participants was done more than 10 years after the study. In the Nottingham trial participants were followed for up to 6 months. Fraser 1980 and Kellner 1992 did not specify the length of the trial and no relevant follow‐up took place. Stoppe 2006 did not specify length of treatment and the time frame of measurements, but reports that 28 from the original 39 participants had a follow‐up 1 month after the last ECT session.
b. Participants of included trials All of the studies included participants of 60 years and older. Both sexes were included.
In the Nottingham trial a standardised psychiatric history was taken and all patients were assessed using the MRC and Feighner criteria for major depressive illness and the Present State Examination (PSE). Fraser 1980 operationalised diagnosis according to the Feighner criteria (Feighner 1972). Kellner 1992 used DSM‐III criteria to diagnose depressive illness. Only one of the studies (Stoppe 2006) used a structured clinical interview to establish diagnosis (Cambridge Examination of for Mental Disorders of the Elderly, DSM‐IV criteria).
The participants in the Nottingham trial were, for the most part, referred for ECT treatment. Fraser 1980 provided no information on preliminary treatment of the participants. The participants in the study by Kellner 1992 were referred for ECT. Stoppe 2006 indicates that patients were especially referred for ECT. More specific information on earlier treatment with antidepressants prior to the episode in which the patients participated in the studies was missing in all the included studies. In addition, no information was provided on the treatment of participants' possible earlier depressive episodes. Information on the mean number of admissions was also lacking in all the studies.
As adequate information on somatic and psychiatric co‐morbidity and history is important in the treatment of depressed elderly people, the lack of data about physical disease and psychiatric co‐morbidity is a serious limitation. Only Fraser 1980 mention that "mild or moderate senile dementia did not by itself exclude a patient from ECT".
c. Setting of included trials Participants in the studies were inpatients as well as outpatients. d. Study size of included trials O'Leary 1994 analysed data on 35 patients aged 60 and over from the Nottingham trial (Gregory 1985), in which 69 patients originally participated. Twelve of the elderly participants were withdrawn from the Nottingham trial before completing the six study treatments. Three of these non‐completers were withdrawn because they improved before the six study treatments were finished, eight of them because they failed to improve, and one because of physical illness. A separate analysis on the completers and non‐completers was performed, but not an intention‐to‐treat analysis. Some serious doubt is necessary, therefore, on the value of the results they describe. In the Nottingham trial, seven elderly patients completed treatment with simulated ECT, eight patients completed treatment with unilateral and eight with bilateral ECT.
Fraser 1980 initially included 33 patients. Four of them dropped out of the study, two of them died, and two left treatment "against advice". The authors did not include these drop‐outs in their analyses. Kellner 1992 included only 15 patients. It seems that all of them completed treatment. Stoppe 2006 included 39 patients for randomisation. No information was provided on the number of eligible participants before inclusion.
e. Interventions of included trials In the O'Leary 1994 analysis (based on re‐examination of data on elderly patients in the Nottingham trial) participants were randomised to receive simulated ECT, unilateral ECT or bilateral ECT. Treatment was twice weekly. Six study treatments were given. An Ectron Duopulse Mark IV machine, waveform 1, was used, delivering energy in units of Joules rather than charge, which made it impossible to quantify the amount of electrical stimulation administered. Bilateral treatment was applied using the bitemporal position and unilateral ECT was administered using the Lancaster position, applied to the right tempero‐parietal position (Lancaster 1958). Anaesthesia consisted of methohexital 70 mg with suxamethonium bromide 50 mg as a muscle relaxant. Patients in the simulated group received the whole ECT procedure, but no shock. Adequacy of seizures was determined by means of the cuff method but details were not reported. The use of low‐dose benzodiazepines was allowed during the study.
Fraser 1980 randomised participants to receive either unilateral or bilateral ECT. They used an Elektron Duopuls Mark 4 machine, delivering 30 to 120 Joules in a unidirectional "chopped" sine waveform, making it impossible to quantify the amount of electrical stimulation administered. Patients were anaesthetised with thiopentone 150‐250 mg, and the muscle relaxant was suxamethonium 25‐40 mg, doses depending on body weight. The electrode placement was according to the method by Stromgren 1973. No information is provided on the adequacy of seizure induction or the parameters by which this was established. All psychotropic medication was stopped 24 hours before treatment. The number of treatments ranged from 4‐11, twice weekly.
Kellner 1992 randomised between two treatment groups. Group 1 underwent ECT once a week for 3 weeks. Group 2 underwent three‐times‐weekly ECT for 3 weeks. Slow‐responders in group 1 were switched to three‐times weekly treatment after treatment 3. Slow‐responders in group 2 after nine treatments were given ongoing three‐times‐weekly ECT until clinically well. Bilateral electrode placement was used for all participants. A MECTA SR2 ECT device was used, delivering a brief‐pulse, square‐wave stimulus. Anaesthesia consisted of methohexital (1 mg/kg) and succinylcholine (0.75 mg/kg). Dose titration was not performed. Stimulus dosing was adjusted to produce a motor seizure >20 s. Motor seizures lasting <15 s were considered missed. Those patients were re‐stimulated at higher‐energy settings within 30‐60s. No information is provided on the adequacy of seizure induction and the parameters by which this was established. Information on the use of psychotropic medication is lacking.
Stoppe 2006 randomised participants to receive either unilateral or bilateral ECT. They used a SpECTrum 5000Q (Mecta corp). A maximum charge of 1152 mC could be delivered. Patients were randomised to BL ECT modified fixed dose (2.5 times age) or RUL ECT at a modified fixed dose (7 times age formula). Seizures < 25 seconds EEG monitoring were considered as missing. Anaesthesia and relaxation was provided with etomidate (0.2‐0.3 mg/ kg) and succinylcholine chlorhydrate (0.5 mg/kg).
f. Outcomes In all studies improvement was measured on internationally validated instruments like the Hamilton Depression Rating scale (HRDS or HAM‐D) (Hamilton 1960) and the Montgomery Asberg Depression Rating Scale (MADRS) (Montgomery 1979). These were all continuous outcome measures. Only the study by Stoppe 2006 used pre‐defined criteria for responders or non‐responders; remission was defined as a drop of >10 points, response as a reduction of at least 50% on the MADRS scores. In the other studies no dichotomous data could be generated.
Primary outcomes Primary outcome measures in the Nottingham trial (O'Leary 1994) were scores on continuous outcome scales, the MADRS and HRDS. Study patients were assessed after every two treatments and within two days of the last ECT. Raters were blinded to the treatment group. No information is provided on how this blinding was achieved.
In Fraser 1980 scores on the HAM‐D were the primary outcome. Participants were assessed before treatment, within 24 hours of the fifth treatment and 3 weeks after the last. Fraser 1980 also made comparisons between patients with 'good' and 'moderate' outcomes. However, information on this point is so scarce, that the review authors have serious doubts on the interpretation of these data. A rater who was blind to the patient's treatment condition measured the depressive symptoms. No information was provided on how this blinding was achieved.
Kellner 1992 measured the primary outcome by means of the HAM‐D, the Beck Depression Inventory (BDI), the Clinical Global Improvement Scale (CGI), and the Brief Psychiatric Rating Scale (BPRS), all of them being continuous outcome scales. A researcher who was blind to the patient's treatment rated the depression scales. No information was provided on how this blinding was achieved.
Stoppe 2006 measured outcome by the continuous scores of the MADRS during (4th, 8th, 12th, 16th session), before and after the last ECT session. In addition, response and remission were compared dichotomously. No specific information was given on the way in which blinding of measurements was carried out.
Secondary outcomes In the Nottingham trial (O'Leary 1994) no information on cognitive or other side effects was collected. Fraser 1980 examined cognitive side effects by applying the Wechsler memory scale before treatment, not less than 24 hours after the fifth treatment and 3 weeks after the last treatment. The principal investigator also administered a "simple ad hoc questionnaire" at the moment the second Hamilton test was applied, intended to score potential side effects such as headache and nausea. Kellner 1992 examined cognitive side effects by applying the Mini‐Mental Status Examination (MMSE) at baseline, weekly on non‐ECT days, and 1 week after the last ECT. Thereby, the Wechsler memory Scale‐Revised (WMS‐R) was administered at baseline and 1 week after the last ECT treatment. Stoppe 2006 examined cognitive side effects with the MMSE during (4th, 8th, 12th, 16th session) before and after the last ECT session. A neuropsychological battery was applied before and after the ECT course. All test scores were presented as continuous data.
None of the studies provided information on any of the other outcome measures as described in the methodology section of this review.
Missing outcomes All trials except Stoppe 2006 presented findings in graphs or p‐values only. Stoppe 2006 described remission based on the preset criteria of numbers of patients, however, response was not specified in this way. Standard deviations and/or means were not provided in all studies. In Fraser 1980 it was also possible to calculate dichotomous outcome from the data provided in the report. Because only Stoppe 2006 used pre‐defined criteria for responders or non‐responders, it was impossible to obtain or calculate any dichotomous outcome measures in other studies.
Stoppe 2006 reported cognitive outcome, but only literate participants (28 out of 39) could participate in this part of the study. Information on the efficacy and possible side‐effects of ECT in the medium and long term was sparse or lacking completely. In the Nottingham trial (O'Leary 1994), data on cognitive side‐effects were not collected .
None of the trials provided information on cause‐specific and non‐specific morbidity/mortality or suicide rates in the short or longer term. Data on physical co‐morbidity and mortality/suicide rates were not collected in any of the trials. No trial reported on economic or functional outcomes
Risk of bias in included studies
See: Characteristics of Included Studies table
Randomisation No studies achieved a quality rating of "A" for their descriptions of methods used to randomise. It was not clear exactly how randomisation had occurred in any of the studies, resulting in all of them receiving a rating of "B" (methods used unclear). The information provided in the studies did not rule out the possibility that bias could have been introduced.
Blinding to interventions and outcomes No study clearly described their procedures for blinding of assessors. They all described that assessors were blinded for the procedure under study, but adequate information to determine this with certainty was missing.
Follow‐up In the Nottingham trial participants were followed up until six months after the end of treatment with ECT. O'Leary 1994 mentions that "at 1, 3 and 6 months after the study there were no significant differences in the change in HDRS or MADRS score between the three treatment types". No analysable data were provided on this point, and the statistical procedures on which these conclusions were based were not clear. The number of drop‐outs was not reported, neither was it clear how the significant differences had been calculated. Fraser 1980 and Kellner 1992 make no mention of follow‐up data. No study analysed their data on an intention‐to‐treat basis. O'Leary 1994 performed a separate analysis on completers and non‐completers. Stoppe 2006 reports a maximum follow‐up of one month post ECT.
Because of the lack of information on the adequacy of randomisation, the adequacy of blinding of outcome assessors and all the other limitations, interpretation of the results of the included studies is difficult and necessitates caution.
Effects of interventions
No study addressing the primary objective of this review was identified. The study by O'Leary 1994 was the only study to examine one of the primary objectives, but the methodological problems and insufficient data prohibited a comparison. Only one study on one of the secondary objectives was available for inclusion in a comparison (Fraser 1980). The trial by Kellner 1992 could not be included in a comparison because the relevant data were missing and could not be supplied. The trial by Stoppe 2006 was not included in a comparison, because the relevant continuous data were not presented, and dichotomous data were limited to numbers of participants who remitted at the end of the study. Other well‐designed randomised controlled trials evaluating ECT in the depressed elderly were lacking, especially trials in which the efficacy of ECT was compared with antidepressants, or trials in which the efficacy and safety of ECT in subpopulations of depressed elderly were studied. Therefore it was possible to undertake one comparison only, on the efficacy of unilateral versus bilateral ECT, on the basis of the study by Fraser 1980. A comparison in MetaView could be presented for this outcome (see Comparison 2). We decided to give an overview of the major findings as reported by O'Leary 1994, Kellner 1992 and Stoppe 2006, given the fact that no other randomised evidence was available. We provide these findings in Comparisons 1 to 3, without being able to present them in MetaView. Because of the small numbers of studies found, heterogeneity and sensitivity analyses could not be performed.
Comparison 1: Real ECT versus simulated ECT One study compared real ECT with simulated ECT (O'Leary 1994). The authors performed an analysis both on the completers and non‐completers. No intention to treat analysis was performed. Post hoc analyses of the completers showed that after six study ECT‐treatments the mean MADRS scores of the unilateral and bilateral groups differed significantly from the simulated group (p<0.05). Because the investigators had not supplied means and/or standard deviations, a quantitative analysis could not be made on this outcome. A two‐way analysis of variance of treatment group and number of ECT‐treatments showed a significant interaction between treatment group and number of ECT‐ treatments (p<0.01). Again, because means in the treatment and control conditions were not provided, the analysis we had intended to undertake (change of baseline scores using a fixed effect model) was not possible. The authors of this trial performed a separate analysis on the non‐completers. Among the non‐completers, there was a significant improvement in the real treatment group compared to the simulated group as measured by the mean and percentage changes in the HRDS and MADRS (p<0.02). In our opinion, interpreting results on non‐completers without performing an intention to treat analysis necessitates caution.
Comparison 2: Unilateral versus bilateral ECT Three trials compared unilateral with bilateral ECT (Fraser 1980, O'Leary 1994, Stoppe 2006). Continuous data were available in the first two studies only. However, O'Leary 1994 did not provide means and/or standard deviations, therefore the comparison could not be included in the quantitative analysis. The analysis was therefore based only on the data supplied by Fraser 1980. Although the authors suggested superior efficacy of unilateral ECT over bilateral ECT, the findings are not wholly convincing with WMDs of 6.06 (CI ‐5.20, 17.32) after 5 treatments, and ‐0.37 (‐5.02, 4.28) after 3 weeks of treatment. It should be noted that the sample size was small (13 receiving unilateral ECT and 16 bilateral ECT). In the study by Stoppe 2006, the authors reported that 15 out of 17 patients (88.2%) from the RUL ECT group and 15 out of 22 patients (68%) of the BL ECT patients were in remission at the end of the study, a non‐significant difference between groups (p=0.25). The number of participants who partially responded or did not respond were not reported. In addition, there was a marked difference in pre‐ECT MADRS scores between the two groups.
Stoppe 2006 and Fraser 1980 did not provide standard deviations on the outcomes for the cognitive side effects. Therefore, these outcomes could not be included in the quantitative analysis. Comparison 3: Once weekly ECT versus three‐times weekly ECT Kellner 1992 compared once‐weekly ECT with three‐times‐weekly ECT. Scores on the HAM‐D showed statistically significant improvement in both groups (p<0.001), with HAM‐D scores significantly lower in the three‐times weekly group compared to the once‐weekly ECT‐group at week 4 of treatment only (p<0.001). No statistically significant difference was found between pre‐treatment and post treatment or between groups on cognitive measures. Information on standard deviations was lacking for both the outcomes on the HAM‐D and cognitive measurements. No quantitative analysis could be performed because the principal investigator for the Kellner study has informed us that no additional information is available.
Discussion
Methodological considerations and limited data Given the fact that elderly people are particularly prone to the side effects of antidepressants and that ECT in the elderly may be a more effective and safer treatment, it is important to have randomised data available on this specific topic. The lack of well conducted randomised prospective trials in which the efficacy and safety of ECT was compared with antidepressants, made it impossible to test the major hypothesis of this review, namely that modified ECT has a greater and/or more rapid antidepressant effect than simulated ECT, antidepressant drug treatment or non‐pharmacological interventions. Evidence on the superiority of real over simulated ECT in elderly could only be based on one study, which contained several methodological shortcomings (O'Leary 1994). Ethically, it does not seem justified to employ sham ECT in further trials because comparative active treatments are available for depressive disorder in the elderly. Evidence for the superiority of ECT over antidepressants in depressed elderly patients was simply lacking. There was no clear evidence to support or refute the use of ECT for particular subgroups of depressed elderly patients, such as those with concomitant dementia, cerebrovascular disorders or Parkinson's disease, because randomised evidence on this topic is also lacking. Although a large number of studies appeared on the major topic and subtopics of this review, they mostly consisted of non‐randomised studies. Summarising the results of these non‐randomised studies was not the objective of this review.
Only one study on one of the secondary objectives of this review (Fraser 1980) generated data that could be included in the quantitative analyses. The data did not convincingly demonstrate a superior efficacy of unilateral ECT over bilateral ECT. Because of the small number of studies on the efficacy and safety of ECT in elderly people, considerable caution must be taken in generalising these findings. We hope to be able to obtain continuous data from the study by Stoppe 2006, for pooling with the continuous data from the Fraser 1980 study, in the next update of the review.
Generalisability Randomised evidence on the efficacy and safety of ECT in depressed elderly people was sparse. Three eligible studies out of four randomised participants without operationally diagnosed disorders. Extensive information on somatic and psychiatric co‐morbidity, as well as information on previous treatments and depressive episodes, was missing. Therefore, how the participants resemble those seen in general practice is hard to know.
Limited data Randomised trials on the efficacy and safety of ECT in depressed elderly was sparse. The collection and quality of reporting data was disappointing. In two of the four included trials means and/or standard deviations were not given, or data were presented in graphs that made it almost impossible to extract useful information.
Sensitivity analysis and publication bias It was not possible to undertake the proposed funnel graph for publication bias or undertake a sensitivity analysis on subgroups of depressed elderly people (those with concomitant dementia, cerebrovascular disorders and Parkinson's disease). The absence of any controlled studies that attempted to replicate the included studies was surprising, given the daily use of ECT in such patients. This leads to the question of whether there might be some bias against research in this understudied area.
Authors' conclusions
Implications for practice.
The main conclusions from this review are as follows: 1. Randomised evidence on the efficacy and safety of ECT in depressed elderly people is sparse, based on trials with a limited number of participants and with shortcomings in methodology and in presentation of outcome data. This leads us to conclude that none of the objectives of this review could be adequately tested. These findings are noteworthy given the relatively frequent usage of ECT in elderly people. 2. One trial concluded that real ECT was superior to simulated ECT. Because of the many methodological problems of this study, replication of these findings with a larger number of participants may be justified. 3. The efficacy of unilateral over bilateral ECT or vice versa has not been convincingly proved. 4. The superiority of three‐weekly ECT over ECT once a week has not been convincingly proved. 5. Randomised evidence on the efficacy and safety of ECT in subpopulations of depressed elderly patients is completely lacking.
Implications for research.
1. Given the specific problems in the treatment of depressed elderly people, it is important to conduct a well designed randomised controlled trial in which the efficacy of ECT is compared to one or more antidepressants or transcranial magnetic stimulation (TMS). 2. In such trials, it is important to establish the medium and long term effects of ECT in outcome, morbidity, mortality and economic values. 3. More studies on the safety and efficacy of ECT compared to antidepressants in specific subpopulations of depressed elderly patients (such as those with concomitant dementia or cerebrovascular disorders) need to be performed. 4. Attention should be paid to the presentation of outcome data in future trials.
Feedback
Feedback on 'Electroconvulsive therapy for the depressed elderly', 9 December 2014
Summary
Comment 1. The authors write that "approximately 50‐60% of patients are thought to improve clinically as a consequence of antidepressant treatment." This is not correct. The FDA's meta‐analysis of 100,000 people found that about 50% of the patients got better on an antidepressant and 40% on placebo, ie. only a 10% difference (1), and a Cochrane review of treatment of depressed patients in primary care reported similar results (2). However, these trials were not effectively blinded, and if atropine is put in the placebo to blind the trials better, there is no effect, which another Cochrane review has shown (3, 4).
Comment 2. The authors write that, "Currently there is no evidence to suggest that ECT causes any kind of brain damage, although temporary cognitive impairment is frequently reported" and that "ECT seems to be a safe procedure". This is not the case. ECT is highly controversial (5), patients report permanent memory problems (6), and there seems to be a death rate of about 1 per 1000 (7).
Comment 3. Only one RCT met the inclusion criteria and that trial was a post‐hoc analysis of data in elderly people who participated in the Nottingham trial. It would be of interest to readers to know what the Nottingham trial showed.
Comment 4. The authors write that, "The original search was performed in collaboration with John Geddes and others, who were kind enough to share their search results with us. The Geddes group have conducted a review on the safety and efficacy of ECT for depressive illness, but not specifically in the elderly." There is no reference to Geddes' review, and I have been unable to find it on PubMed. I also think other readers than me would be interested in knowing what this review found.
I agree with the conflict of interest statement below:
I certify that I have no affiliations with or involvement in any organization or entity with a financial interest in the subject matter of my feedback.
1. Laughren TP. Overview for December 13 Meeting of Psychopharmacologic Drugs Advisory Committee (PDAC). 2006 Nov 16. Available online at: www.fda.gov/ohrms/dockets/ac/06/briefi ng/2006‐4272b1‐01‐FDA.pdf (accessed 22 October 2012). 2. Arroll B, Elley CR, Fishman T, et al. Antidepressants versus placebo for depression in primary care. Cochrane Database of Systematic Reviews 2009;3:CD007954. 3. Moncrieff J, Wessely S, Hardy R. Active placebos versus antidepressants for depression. Cochrane Database Systematic Reviews 2004;1:CD003012. 4. Gøtzsche PC. Why I think antidepressants cause more harm than good. Lancet Psychiatry 2014;1:104‐6. 5. Carney S, Geddes J. Electroconvulsive therapy. BMJ 2003;326:1343‐4. 6. Rose D, Wykes T, Leese M, Bindman J, Fleischmann P. Patients perspectives on electroconvulsive therapy: systematic review. BMJ 2003;326:1363‐5. 7. Read J, Bentall R. The effectiveness of electroconvulsive therapy: a literature review. Epidemiol Psichiatr Soc 2010 Oct‐Dec;19:333‐47.
Reply
Dear colleague
Thank you for your comments on the Cochrane review ‘Electroconvulsive therapy for the depressed elderly’ originally dating from 2003, with a minor update in 2009. We are aware that the review is outdated now and that a review on this topic is needed, given the wealth of new research in this area in the last period. Indeed we plan to start an update of this review this year, with the help of the improved Cochrane methods today.
Considering your comments:
1. Indeed a wealth of trials in primary care arrangements in depressed people, also in the elderly, concludes that the effect of pharmacotherapy is restricted and sometimes hardly better than placebo. The main problem here is the depression diagnosis that has been seriously flawed by our classification system. I think the reference you comment is indeed not applicable to the ECT population. Elderly patients who receive ECT are in a large majority hospitalised during at least the index episode of their mood disorder (1, 2, 3) and not in any way comparable to the participants in the studies you mention.
2. Safety of the procedure during ECT is has to be considered in the light of the life threatening effects of the severe mood disorder of the majority of patients who receive ECT like suicidality, decreased intake of fluids and food, agitation etc. Serious depression in the elderly, often with psychomotor symptoms, psychotic and melancholic features, is a life threatening condition. Considering the memory problems, you are right that this problem has not been solved, for a large part because studying cognitive impairment in ECT is methodologically very complicated. Nevertheless a lot of effort has been spent recently to study more in detail important domains of cognition in depressed patients. It will be part of the update of this review. To date, still the majority of patients treated with ECT have no lasting effect on cognition after six months (4, 5). The stigma on ECT as a treatment modality makes it (still) controversial; opinions in this respect differ also. This aspect will not be part of our review.
3. You mention an important issue when studying ECT. Ideally a ‘double blinded sham condition’ should be performed to fulfil RCT conditions. This was only feasible in an era when there was serious doubt on the efficacy alone of the treatment as shown in the Nottingham trial. Indeed a post‐hoc analysis of older people is the only data available in this respect. I am pretty sure it will stay that way, because a controlled RCT with sham ECT in seriously depressed older people is unlikely to be accepted by respected ethical committee.
4. The protocol by Geddes and colleagues was withdrawn from The Cochrane Library; the review was then published in the Lancet in March 2003 (6). Our review was first published on the Cochrane Library in April of the same year. Because at that time Cochrane reviews were published quarterly, no reference to the Lancet paper could be included as our review would have already been marked for publication. We will address this in the upcoming review update by starting a completely new search.
Max L Stek
Professor in old age Psychiatry
1. Spaans et al. Speed of remission in elderly patients with depression: elctroconvulsive therapy v. medication. Br J Psychiatry 2015;206:67‐71.
2. Oudega ML et al. White matter hyperintensities, medial temporal lobe atrophy, cortical atrophy and response to electroconvulsive therapy in severely depressed elderly patients. J Clin Psychiatry 2011;72:104‐12.
3. Kellner et al. Depression severity in electroconvulsive therapy (J ECT) versus pharmacotherapy trials. J ECT 2015;31:31‐3.
4. Semkovska M & McLoughlin M. Objective cognitive performance associated with electroconvulsive therapy for depression: a systematic review and meta‐analysis. Biol Psychiatry 2012;15:568‐77
5. Verwijk et al. Short and long term neurocognitive functioning after electroconvulsive therapy in depressed elderly: a prospective naturalistic study. Int Psychogeriatr 2014;26:315‐24.
6. Geddes J et al. Efficacy and safety of electroconvulsive therapy in depressive disorders. A systematic review and meta‐analysis. Lancet 2003;361: 799‐808.
Contributors
Feedback submmitted by: Peter C Gøtzsche
Response submitted by: Max L Stek
What's new
| Date | Event | Description |
|---|---|---|
| 14 April 2015 | Feedback has been incorporated | Feedback incorporated |
History
Protocol first published: Issue 2, 2002 Review first published: Issue 2, 2003
| Date | Event | Description |
|---|---|---|
| 1 November 2008 | Amended | Converted to new review format. |
| 18 February 2003 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
We are very grateful for the collaboration with John Geddes and Stuart Carney on the search process. We also are grateful for the considerable support and input provided by the CCDAN Editorial Team. We acknowledge Rob Scholten from the Dutch Cochrane Centre and Bernard Uitdehaag from the Department of Neurology and Epidemiology, VUmc, Amsterdam, The Netherlands.
Data and analyses
Comparison 1. unilateral versus bilateral ECT/after 5 treatments.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Hamilton Depression Rating Scale | 1 | 29 | Mean Difference (IV, Fixed, 95% CI) | 6.06 [‐5.20, 17.32] |
1.1. Analysis.
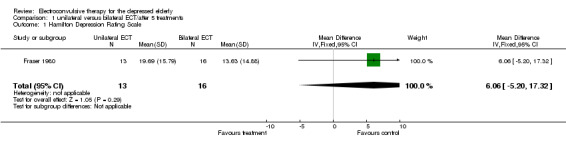
Comparison 1 unilateral versus bilateral ECT/after 5 treatments, Outcome 1 Hamilton Depression Rating Scale.
Comparison 2. unilateral versus bilateral ECT/after 3 weeks treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Hamilton Depression Rating Scale | 1 | 29 | Mean Difference (IV, Fixed, 95% CI) | ‐0.37 [‐5.02, 4.28] |
2.1. Analysis.
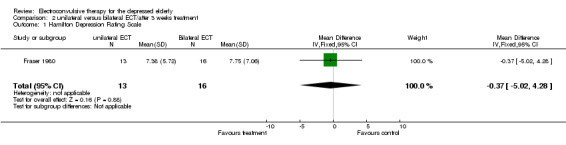
Comparison 2 unilateral versus bilateral ECT/after 3 weeks treatment, Outcome 1 Hamilton Depression Rating Scale.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Fraser 1980.
| Methods | Allocation: Randomised controlled trial, randomisation procedure not described and allocation concealment unclear; Duration: not specified; patient and outcome assessor blinding seems appropriate; no follow‐up period; Intention‐to‐treat analysis not mentioned, possible 4 patients dropped‐out, authors seem to have used an end‐point analysis; | |
| Participants | Diagnosis: Depressive illness, based on Feigner criteria; Age 64 ‐ 86 years; N = 33, 5 participatns dropped‐out; Sex: 8 M, 25 F; Inclusion criteria: depression of a least a month duration, dementia was not an exclusion criterium, other inclusion criteria not specified. | |
| Interventions | Unilateral versus bilateral ECT; no information is provided on the adequacy of seizures or the method by which seizures were induced; unilateral ECT n = 13 bilateral ECT n = 16 | |
| Outcomes | Mood change: Hamilton Rating Scale (HAM‐D) and the Nursus' Observation scale for Inpatient evaluation; Cognitive side‐effects: the Wechsler Memory Scale Other side‐effects by questionnaire |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Kellner 1992.
| Methods | Allocation: Randomised controlled trial, randomisation procedure not described and allocation concealment unclear; Duration: not described; No follow‐up period; Patient blinding: not possible; Outcome blinding: procedure not described, bias seems possible, cannot be excluded; Intention to treat analysis not mentioned, none of the participants dropped out of treatment. | |
| Participants | Diagnosis: DSM‐III criteria for major depression; Age 53‐87 years; participants had been referred for ECT treatment, no information is provided on earlier antidepressant treatment in any of the participants; N = 15; Sex: 11M and 4F | |
| Interventions | ECT once a week versus three‐times‐weekly ECT; bilateral treatment in all participants; method of seizure induction adequately described | |
| Outcomes | Mood change: Hamilton Rating Scale for Depression (HAM‐D), the Beck Depression Inventory (BDI), the Clinical Global Improvement Scale (CGI) and the Brief Psychiatric Rating Scale (BPRS) Cognitive side effects: Mini Mental Status Examination (MMSE) and the Wechsler Memory Scale‐Revised (WMS‐R) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
O'Leary 1994.
| Methods | Allocation: Randomised controlled trial, Duration: not described; Follow‐up period: six month; Patient blinding adequate; Outcome blinding: seems adequate; Intention to treat analysis not mentioned, 12 of the participants dropped out of treatment. | |
| Participants | Diagnosis: DSM‐III criteria for major depression; Age 60 ‐ 85 years; participants had been referred for ECT treatment, no information is provided on earlier antidepressant treatment in any of the participants; N = 35; Sex: not provided | |
| Interventions | Sham ECT, versus unilateral or bilateral ECT; maximum number of study ECT‐treatment 6; method of seizure induction described | |
| Outcomes | Mood change: Hamilton Depression Rating Scale (HDRS), Montgomery Asberg Depression Rating Scale (MADRS) Side effects: no information provided. |
|
| Notes | Reexamination of outcome data from the Nottingham ECT trial from 1985 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Stoppe 2006.
| Methods | Allocation: Randomised controlled trial | |
| Participants | Diagnosis: DSM IV criteria; CAMDEX diagnosis | |
| Interventions | Unilateral versus bilateral ECT | |
| Outcomes | Mood change: MADRS Cognition: MMSE neuropsychological battery | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Alexopoulos 1984 | not a randomized controlled trial ‐ retrospective chart review |
| Alexopoulos 1989 | not a randomized controlled trial ‐ review |
| Allen 1982 | not a randomized controlled trial ‐ case report |
| Allman 1987 | not a randomized controlled trial ‐ case report |
| Andersen 1987 | not a randomized controlled trial on depression in Parkinson's disease |
| Asnis 1977 | not a randomized controlled trial ‐ case report |
| Atre‐Vaidya 1988 | not a randomized controlled trial ‐ case report |
| Avery 1976 | not a randomized controlled trial, naturalistic study |
| Awata 2002 | case series |
| Aziz 2005 | no RCT; cost utility study |
| Babigian 1984 | not a randomized controlled trial ‐ epidemiologic follow‐up study |
| Ball 1995 | not a randomized controlled trial ‐ retrospective chart review |
| Balldin 1980 | not a randomized controlled trial on depression in Parkinson's disease |
| Barnes 1997 | not a randomized controlled trial ‐ case report on maintenance ECT |
| Beale 1996 | not a randomized controlled trial ‐ case report on maintenance ECT |
| Benbow 1987 | not a randomized controlled trial ‐ retrospective chart review |
| Benbow 1988 | not a randomized controlled trial ‐ letter |
| Benbow 1989 | not a randomized controlled trial ‐ traditional review |
| Blackburn 1994 | not a randomized controlled trial ‐ case report |
| Bosboom 2006 | naturalistic study of cognitive side effects |
| Bosworth 2002 | not a randomized controlled trial |
| Bracken 1987 | not a randomized controlled trial ‐ case report |
| Brodaty 2000 | not a randomized controlled trial, naturalistic study |
| Brodaty 2001 | not a randomized controlled trial, naturalistic study |
| Burd 1998 | not a randomized controlled trial, naturalistic study |
| Burke 1985 | not a randomized controlled trial ‐ retrospective chart review |
| Burke 1987 | not a randomized controlled trial ‐ retrospective chart review |
| Burke 1988 | not a randomized controlled trial ‐ case report |
| Calloway 1981 | not a randomized controlled trial ‐ retrospective chart review |
| Casey 1994 | not a randomized controlled trial ‐ traditional review |
| Casey 1996 | not a randomized controlled trial ‐ retrospective chart review |
| Cattan 1990 | not a randomized controlled trial ‐ retrospective chart review |
| Chacko 1983 | not a randomized controlled trial ‐ case report |
| Coffey 1987 | not a randomized controlled trial ‐ case report |
| Coffey 1988a | not a randomized controlled trial, naturalistic study |
| Coffey 1988b | not a randomized controlled trial ‐ retrospective chart review |
| Coffey 1989 | not a randomized controlled trial, naturalistic study |
| Currier 1992 | not a randomized controlled trial ‐ retrospective chart review |
| Cybulska 1997 | not a randomized controlled trial ‐ case report |
| D'Mello 1988 | not a randomizedcontrolled trial ‐ case report |
| Devanand 1994 | not a randomized controlled trial ‐ review |
| Dighe‐Deo 1998 | not a randomizedcontrolled trial ‐ case report |
| Dinan | |
| Dinan 1989 | no separate analysis of elderly possible |
| Douyon 1989 | not a randomized controlled trial ‐ case report |
| Drop 1988 | not a randomized controlled trial ‐ case report |
| Dubin 1992 | maintenance ECT, not a randomized controlled trial |
| Duncan 1990 | maintenance ECT, not a randomized controlled trial |
| Dysken 1976 | not a randomized controlled trial, case report |
| Ehrenberg 1955 | not a randomized controlled trial, not modified ECT |
| Erman 1979 | not a randomized controlled trial, retrospective chart review |
| Faber 1991 | traditional review on Parkinson's disease and ECT |
| Fall 1999 | not a randomized controlled trial, case report |
| Figiel 1989 | not a randomized controlled trial, naturalistic study |
| Figiel 1990a | not a randomized controlled trial, naturalistic study |
| Figiel 1990b | not a randomized controlled trial, naturalistic study |
| Figiel 1991 | not a randomized controlled trial, case report |
| Flaherty 1984 | not a randomized controlled trial, case report |
| Flint 1997 | not a randomized trial, open study |
| Frances 1989 | not a randomized controlled trial, case report |
| Frasca 2003 | no separate analysis of elderly possible |
| Fraser 1978 | not a randomized controlled trial, case reports |
| Fu 1999 | not a randomised trial on the efficacy of ECT in depressed elderly |
| Gallinek 1947 | Not modified ECT |
| Gaspar 1982 | not a randomized controlled trial, retrospective chart review |
| Godber 1983 | letter |
| Godber 1987 | not a randomized controlled trial, naturalistic study |
| Gormley 1998 | not a randomized controlled trial, retrospective chart review |
| Gournelis 2006 | review article |
| Greenberg 1992 | traditional review |
| Greenwald 1989 | not a randomized controlled trial on the outcome of ECT in depression |
| Grunhaus 2003 | RCT of ECT versus TMS; no separate analysis of elderly possible |
| Guttmacher 1989 | not a randomized controlled trial, case series |
| Hay 1989 | not a randomized controlled trial, retrospecitve chart review |
| Heshe 1978 | mixed unipolar and bipolar group, no separate analysis of unipolar depressive elderly possible |
| Hickie 1995 | not a randomized controlled trial, naturalistic study |
| Hihn 2006 | case series on cognition |
| Holcomb 1983 | not a randomized controlled trial, case report |
| Hordynska 2003 | review article |
| Hunt 1998 | not a randomized controlled trial, case report |
| Husain 2004 | no analysis on elderly possible; RCT on M‐ECT |
| Hussar 1968 | not a randomized controlled trial, case report |
| Huuhka 2003 | case series on cardiac arrhytmia and ECT |
| Huuhka 2004 | naturalistic study |
| Jenike 1983 | not a randomized controlled trial, traditional review |
| Jenike 1989 | not a randomized controlled trial, traditional review |
| Kajala 2004 | naturalistic study |
| Kamat 2003 | review article |
| Karlinsky 1984 | not a randomized controlled trial, retrospective chart review |
| Kellner 2004 | single blind study; no separate analysis of elderly possible |
| Kelly 2000 | not a randomized controlled trial, traditional review |
| Kelsey 1995 | not a randomized controlled trial, retrospective chart review |
| Kramer 1986 | not a randomized controlled trial, case report |
| Kramer 1987 | not a randomized controlled trial, retrospective chart review |
| Krause 1988 | not a randomized controlled trial, retrospective chart review |
| Kroessler 1993 | not a randomized controlled trial, retrospective chart review |
| Krystal 2000 | randomized trial on the predictive power of Ictal EEG Indices on respons of unilateral or bilateral ECT. No outcome measures of depression provided. Therefore, study excluded. No additional information obtained. |
| Kuruvilla 2006 | no RCT, patient's view study |
| Lambourn 1978 | allthough randomisation took place, no reliable extraction on data in elderly possible |
| Lebensohn 1975 | not a randomized controlled trial, case report |
| Lekwauwa 2006 | no RCT, hippocampal volume and cognition/ ECT |
| Levy 1983 | not a randomized controlled trial, case report |
| Liang 1988 | not a randomized controlled trial, case report |
| Liberzon 1991 | not a randomized controlled trial, case report |
| Lipman 1993 | not a randomized controlled trial, follow‐up study |
| Little 2004 | retrospective study |
| Loo 1991 | not a randomized controlled trial, case report |
| Lovell 1948 | not a randomized controlled trial, traditional review |
| Magni 1988 | not a randomized controlled trial, retrospective chart review |
| Malcolm 1989 | not a randomized controlled trial, letter |
| Mandel 1980 | not a randomized controlled trial, case report |
| Manly 2000 | not a randomized controlled trial, retrospective chart review |
| Martin 1992 | not a randomized controlled trial, case series |
| Mattingly 1991 | not a randomized controlled trial, case report |
| Meyers 1985 | not a randomized controlled trial, retrospective chart review |
| Mielke 1984 | not a randomized controlled trial, retrospective chart review |
| Morris 1991 | not a randomized controlled trial, naturalistic study |
| Mulsant 1991 | not a randomized controlled trial, naturalistic study |
| Murray 1986 | not a randomized controlled trial, retrospective chart review |
| Nahshoni 2001 | naturalistic study on heart rate variability and ECT |
| Nelson 1989 | not a randomized controlled trial, retrospective chart review |
| Nelson 1991 | not a randomized controlled trial, retrospective chart review |
| O' Connor 2001 | not a randomized controlled trial on the efficacy of ECT, randomisation on maintenance ECT versus pharmacotherapy |
| O'Leary 1996 | not a randomized controlled trial, naturalistic study |
| O'Shea 1987 | not a randomized controlled trial, case report |
| Palmer 1990 | not specifically on elderly with a depression |
| Pande 1990 | not a randomized controlled trial, naturalistic study |
| Petrides 1996 | not a randomized controlled trial, case report |
| Pettinati 1984 | not a randomized controlled trial, retrospective chart review |
| Philibert 1995 | not a randomized controlled trial, naturalistic study |
| Price 1989 | not a randomized controlled trial, traditional review |
| Prudic 1987 | no separate analysis of elderly possible |
| Rabkeru 2003 | review article |
| Rao 2000 | not a randomized controlled trial, retrospective chart review |
| Regestein 1980 | not a randomized controlled trial, case report |
| Reynolds 1987 | not a randomized controlled trial, naturalistic study |
| Rice 1994 | not a randomized controlled trial, retrospective chart review |
| Rosen 1992 | not a randomized controlled trial, naturalistic study |
| Rubin 1993 | not a randomized controlled trial, retrospective chart review |
| Ruxin 1994 | not a randomized controlled trial, case reports |
| Salaris 2000 | not a randomized controlled trial, case report |
| Salzman 1982 | not a randomized controlled trial, traditional review |
| Salzman 2002 | review article |
| Scott 1990 | not a randomized controlled trial, letter |
| Scott 1991 | not a randomized controlled trial, letter |
| Serra 2006 | no clear outcome criteria, small numbers |
| Simpson 1998 | not a randomized controlled trial, naturalistic study |
| Smith 2000 | not a randomized controlled trial, case report |
| Sommer 1989 | not a randomized controlled trial on the efficacy of ECt in depressed elderly |
| Spear 1997 | not a randomized controlled trial, case report |
| Stack 1988 | not a randomized controlled trial, naturalistic study |
| Stern 1997 | not a randomized controlled trial, case report |
| Stoudemire 1990 | not a trial on the efficacy or side effects of ECT in depressed elderly, naturalisitic study |
| Stoudemire 1991 | not a randomized controlled trial, naturalistic study |
| Stoudemire 1993 | not a randomized controlled trial, naturalistic study |
| Stoudemire 1994 | not a randomized controlled trial, naturalistic study |
| Stoudemire 1995 | not a randomized controlled trial, naturalistic study |
| Strain 1971 | not a randomized controlled trial, case report |
| Suzuki 2006 | case study |
| Swett 1977 | not a randomized controlled trial, naturalistic study |
| Tamam 2003 | naturalistic study |
| Tancer 1987 | not a randomized controlled trial, case report |
| Tew 1999 | not a randomized controlled trial, naturalistic study |
| Tew 2002 | age of elderly do not correspond with inclusion criteria |
| Thienhaus 1990 | study of the efficacy of maintenance ECT |
| Thompson 2001 c | no data available |
| Tomac 1997 | not a randomized controlled trial, retrospective chart review |
| Van Marwijk 1988 | not a randomized controlled trial, retrospective chart review |
| Van Waarde 2001 | not a randomized controlled trial, retrospective chart review |
| Ware 1990 | not a randomized controlled trial, case report |
| Weiner 1982 | not a randomized controlled trial, traditional review |
| Weisberg 1991 | not a randomized controlled trial, case report |
| Wesson 1997 | not a randomized controlled trial, naturalistic study |
| West 1999 | not a randomized controlled trial, case report |
| Wetterling 1998 | not a randomized controlled trial, retrospective chart review |
| Wijeratne 1999 | not a randomized controlled trial, case report |
| Wilkinson 1993 | not a randomized controlled trial, naturalistic study |
| Williams 1997 | not a randomized control trial, naturalistic study |
| Wolff 1954 | no modified ECT |
| Yesavage 1980 | not a randomized controlled trial, retrospective chart review |
| Young 1985 | not a randomized controlled trial, case report |
| Yudofsky 1979 | not a randomized controlled trial, case report |
| Zorumski 1988 | not a randomized controlled trial, review |
| Zubenko 1994 | not a randomized controlled trial, naturalistic study |
| Zwil 1992 | not a randomized controlled trial, traditional review |
| Zwil 1997 | not a randomized controlled trial, case report |
should be Kajala 2002
Characteristics of ongoing studies [ordered by study ID]
Kellner 2006.
| Trial name or title | CORE 2001 |
| Methods | |
| Participants | all ages; large part elderly |
| Interventions | M‐ECT versus pharmacotherapy (Li + nortrip) |
| Outcomes | HAM‐D relapse |
| Starting date | |
| Contact information | Kellner CH |
| Notes | awaiting answer on possibilty to analyse data in the elderly |
Contributions of authors
Max Stek (MS) and Frits van der Wurff (FvdW) were the main review authors, and performed the review. MS undertook the identification of the studies. The two review authors independently assessed the relevance of each trial. In case of disagreement on whether to include a trial, this was resolved by discussion and consensus together with the third and fourth authors, Aartjan Beekman and Witte Hoogendijk.
Sources of support
Internal sources
Department of Psychiatry, Vrije Universiteit Medical Centre/GGZ‐Buitenamstel, Amsterdam, Netherlands.
External sources
College voor Zorgverzekeringen (CVZ), The Netherlands, Netherlands.
Declarations of interest
None
Edited (no change to conclusions), comment added to review
References
References to studies included in this review
Fraser 1980 {published data only}
- Fraser RM, Glass IB. Unilateral and bilateral ECT in elderly patients. A comparative study.. Acta Psychiatrica Scandinavica 1980;62(1):13‐31. [DOI] [PubMed] [Google Scholar]
Kellner 1992 {published data only}
- Kellner CH, Monroe J, Pritchett J, Jarrell MP, Bernstein HJ, Burns CM. Weekly ECT in geriatric depression. Convulsive Therapy 1992;8(4):245‐52. [PubMed] [Google Scholar]
O'Leary 1994 {published data only}
- O' Leary DA, Gill D, Gregory S, Shawcross CR. The effectiveness of real versus simulated electroconvulsive therapy in depressed elderly patients. International Journal of Geriatric Psychiatry 1994;9(7):567‐71. [Google Scholar]
Stoppe 2006 {published data only}
References to studies excluded from this review
Alexopoulos 1984 {published data only}
- Alexopoulos GS, Shamoian CJ, Lucas J, Weiser N, Berger H. Medical problems of geriatric psychiatric patients and younger controls during electroconvulsive therapy. Journal of the American Geriatrics Society 1984;32(9):651‐4. [DOI] [PubMed] [Google Scholar]
Alexopoulos 1989 {published data only}
- Alexopoulos GS, Young RC, Abrams R. ECT in the high‐risk geriatric patients. Convulsive Therapy 1984;5:75‐87. [PubMed] [Google Scholar]
Allen 1982 {published data only}
- Allen RM. Pseudodementia and ECT. Biological Psychiatry 1982;17(12):1435‐43. [PubMed] [Google Scholar]
Allman 1987 {published data only}
- Allman P, Hawton K. ECT for post‐stroke depression: Beta blockade to modify rise in blood pressure. Convulsive Therapy 1987;3:218‐21. [PubMed] [Google Scholar]
Andersen 1987 {published data only}
- Andersen K, Balldin J, Gottfries CG, Granerus AK, Modigh K, Svennerholm L, et al. A double‐blind evaluation of electroconvulsive therapy in Parkinson's disease with "on‐off" phenomena. Acta Neurologica Scandinavica 1987;76(3):191‐9. [DOI] [PubMed] [Google Scholar]
Asnis 1977 {published data only}
- Asnis G. Parkinson's disease, depression and ECT: a review and case study. American Journal of Psychiatry 1977;134(2):191‐5. [DOI] [PubMed] [Google Scholar]
Atre‐Vaidya 1988 {published data only}
- Atre‐Vaidya N, Jampala VC. Electroconvulsive therapy in parkinsonism with affective disorder. British Journal of Psychiatry 1988;152:55‐8. [DOI] [PubMed] [Google Scholar]
Avery 1976 {published data only}
- Avery D, Winokur G. Mortality in depressed patients treated wih electroconvulsive therapy and antidepressants. Archives of General Psychiatry 1976;33(9):1029‐37. [DOI] [PubMed] [Google Scholar]
Awata 2002 {published data only}
Aziz 2005 {published data only}
Babigian 1984 {published data only}
- Babigian HM, Guttmacher LB. Epidemiologic considerations in electroconvulsive therapy. Archives of General Psychiatry 1984;41(3):246‐53. [DOI] [PubMed] [Google Scholar]
Ball 1995 {published data only}
- Ball CJ, Fashola Y, Herzberg JL. Length of hospital stay and the timing of ECT. International Journal of Geriatric Psychiatry 1995;10(9):783‐6. [Google Scholar]
Balldin 1980 {published data only}
- Balldin J, Eden S, Granerus AK, Modigh K, Svanborg A, Wallinder J, et al. Electroconvulsive therapy in Parkinson's syndrome with " on‐off" phenomena. Journal of Neural Transmission 1980;47(1):11‐21. [DOI] [PubMed] [Google Scholar]
Barnes 1997 {published data only}
- Barnes RC, Hussein A, Anderson DN, Powell D. Maintenance electroconvulsive therapy and cognitive function. British Journal of Psychiatry 1997;170:285‐7. [DOI] [PubMed] [Google Scholar]
Beale 1996 {published data only}
- Beale MD, Bernstein HJ, Kellner CH. Maintenance electroconvulsive therapy for geriatric depression: A one year follow‐up. Clinical Gerontologist 1996;16(4):86‐90. [Google Scholar]
Benbow 1987 {published data only}
- Benbow SM. The use of electroconvulsive therapy in old age. International Journal of Geriatric Psychiatry 1987;2(1):25‐30. [Google Scholar]
Benbow 1988 {published data only}
- Benbow SM. ECT for depression in dementia. British Journal of Psychiatry 1988;152:859. [DOI] [PubMed] [Google Scholar]
Benbow 1989 {published data only}
- Benbow SM. The role of electroconvulsive therapy in the treatment of depressive illness in old age. British Journal of Psychiatry 1989;155:147‐52. [DOI] [PubMed] [Google Scholar]
Blackburn 1994 {published data only}
- Blackburn PA, Decalmer P. Is ECT safe in patients with cerebrovascular disease. International Journal of Geriatric Psychiatry 1994;9(9):757‐61. [Google Scholar]
Bosboom 2006 {published data only}
Bosworth 2002 {published data only}
Bracken 1987 {published data only}
- Bracken P, Ryan M, Dunne D. Electroconvulsive therapy in the elderly. British Journal of Psychiatry 1987;150:713. [DOI] [PubMed] [Google Scholar]
Brodaty 2000 {published data only}
- Brodaty H, Hickie I, Mason C, Prenter L. A prospective follow‐up study of ECT outcome in older depressed patients. Journal of Affective Disorders 2000;60(2):101‐11. [DOI] [PubMed] [Google Scholar]
Brodaty 2001 {published data only}
- Brodaty H, Berle D, Hickie I, Mason C. ' Side effects' of ECT are mainly depressive phenomena and are independent of age. Journal of Affective Disorders 2001;66(2‐3):237‐45. [DOI] [PubMed] [Google Scholar]
Burd 1998 {published data only}
- Burd J, Kettl P. Incidence of asystole in electroconvulsive therapy. American Journal of Geriatric Psychiatry 1998;6(3):203‐11. [PubMed] [Google Scholar]
Burke 1985 {published data only}
- Burke WJ, Rutherford JL, Zorumski CF, Reich T. Electroconvulsive therapy and the elderly. Comprehensive Psychiatry 1985;26(5):480‐6. [DOI] [PubMed] [Google Scholar]
Burke 1987 {published data only}
- Burke WJ, Rubin EH, Zorumski CF, Wetzel RD. The safety of ECT in geriatric psychiatry. Journal of the American Geriatrics Society 1987;35(6):516‐21. [DOI] [PubMed] [Google Scholar]
Burke 1988 {published data only}
- Burke WJ, Peterson J, Rubin EH. Electroconvulsive therapy in the treatment of combined depression and Parkinson's disease. Psychosomatics 1988;29(3):341‐6. [DOI] [PubMed] [Google Scholar]
Calloway 1981 {published data only}
- Calloway SP, Dolan RJ, Jacoby RJ, Levy R. ECT and cerebral atrophy. A computed tomographic study. Acta Psychiatrica Scandinavica 1981;64(5):442‐5. [DOI] [PubMed] [Google Scholar]
Casey 1994 {published data only}
- Casey DA. Depression in the elderly. Southern Medical Journal 1994;87(5):559‐63. [PubMed] [Google Scholar]
Casey 1996 {published data only}
- Casey DA, Davis MH. Electroconvulsive therapy in the very old. General Hospital Psychiatry 1996;18(6):436‐9. [DOI] [PubMed] [Google Scholar]
Cattan 1990 {published data only}
- Cattan RA, Barry PP, Mead G, Reefe WE, Gay A, Silverman M. Electroconvulsive therapy in octogenarians. Journal of the American Geriatrics Society 1990;38(7):753‐8. [DOI] [PubMed] [Google Scholar]
Chacko 1983 {published data only}
- Chacko RC, Root L. ECT and tardive dyskinesia: two cases and a review. Journal of Clinical Psychiatry 1983;44(7):265‐6. [PubMed] [Google Scholar]
Coffey 1987 {published data only}
- Coffey CE, Hinkle PE, Weiner RD, Nemeroff CB, Krishnan KR, Varia I, et al. Electroconvulsive therapy of depression in patients with white matter hyperintensity. Biological Psychiatry 1987;22(5):629‐36. [DOI] [PubMed] [Google Scholar]
Coffey 1988a {published data only}
- Coffey CE, Figiel GS, Djang WT, Sullivan DC, Herfkens RJ, Weiner RD. Effects of ECT on brain structure: a pilot prospective magnetic resonance imaging study. American Journal of Psychiatry 1988;145(6):701‐6. [DOI] [PubMed] [Google Scholar]
Coffey 1988b {published data only}
- Coffey CE, Figiel GS, Djang WT, Cress M, Saunders WB, Weiner RD. Leukoencephalopathy in elderly depressed patients referred for ECT. Biological Psychiatry 1988;24(2):143‐61. [DOI] [PubMed] [Google Scholar]
Coffey 1989 {published data only}
- Coffey CE, Figiel GS, Djang WT, Saunders WB, Weiner RD. White matter hyperintensity on magnetic resonance imaging: clinical and neuroanatomic correlates in the depressed elderly. Journal of Neuropsychiatry & Clinical Neurosciences 1989;1(2):135‐44. [DOI] [PubMed] [Google Scholar]
Currier 1992 {published data only}
- Currier MB, Murray GB, Welch CC. Electroconvulsive therapy for post‐stroke depressed geriatric patients. Journal of Neuropsychiatry & Clinical Neurosciences 1992;4(2):140‐4. [DOI] [PubMed] [Google Scholar]
Cybulska 1997 {published data only}
- Cybulska EM. Globus Hystericus ‐ A somtic symptom of depression? The role of electroconvulsive therapy and antidepressants. Psychosomatic Medicine 1997;59(1):67‐9. [DOI] [PubMed] [Google Scholar]
D'Mello 1988 {published data only}
- D'Mello DA, Vicent FM, Lerner MP. Yawning as a complication of electroconvulsive therapy and concurrent neuroleptic withdrawal. Journal of Nervous & Mental Disease 1988;176(3):188‐9. [DOI] [PubMed] [Google Scholar]
Devanand 1994 {published data only}
- Devanand DP, Krueger RB. Electroconvulsive therapy in the elderly. Current Opinion in Psychiatry 1994;7:364‐9. [Google Scholar]
Dighe‐Deo 1998 {published data only}
- Dighe‐Deo D, Shah A. Electroconvulsive therapy in patients with long bone fractures. Journal of ECT 1998;14(2):115‐9. [PubMed] [Google Scholar]
Dinan {published data only}
Dinan 1989 {published data only}
Douyon 1989 {published data only}
- Douyon R, Shah A. ECT and Parkinson's disease revisited: a " naturalistic" study. American Journal of Psychiatry 1989;146(11):1451‐5. [DOI] [PubMed] [Google Scholar]
Drop 1988 {published data only}
- Drop LJ, Bouckoms AJ, Welch CA. Arterial hypertension and multiple cerebral aneurysms in a patient treated with electroconvulsive therapy. Journal of Clinical Psychiatry 1988;49(7):280‐2. [PubMed] [Google Scholar]
Dubin 1992 {published data only}
- Dubin WR, Jaffe R, Roemer R, Siegel L, Shoyer B, Venditti ML. The efficacy and safety of maintenance ECT in geriatric patients. Journal of the American Geriatrics Society 1992;40(7):706‐9. [DOI] [PubMed] [Google Scholar]
Duncan 1990 {published data only}
- Duncan AJ, Ungvari GS, Russell RJ, Seifert A. Maintenance ECT in very old age: Case report. Annals of Clinical Psychiatry 1990;2(2):139‐44. [Google Scholar]
Dysken 1976 {published data only}
- Dysken M, Evans HM, Chan CH, Davis JM. Improvement of depression and parkinsonism during ECT: a case study. Neuropsychobiology 1976;2(2‐3):81‐6. [DOI] [PubMed] [Google Scholar]
Ehrenberg 1955 {published data only}
- Ehrenberg R, Gullingsrud MJ. Electroconvulsive therapy in elderly patients. American Journal of Psychiatry 1955;111:743‐7. [DOI] [PubMed] [Google Scholar]
Erman 1979 {published data only}
- Erman MK, Welch CA, Mandel MR. A comparison of two unilateral ECT electrode placements: efficacy and electrical energy considerations. American Journal of Psychiatry 1979;136(10):1317‐9. [DOI] [PubMed] [Google Scholar]
Faber 1991 {published data only}
- Faber R, Trimble MR. Electroconvulsive therapy in Parkinson's disease and other movement disorders. Movement Disorders 1991;6(4):293‐303. [DOI] [PubMed] [Google Scholar]
Fall 1999 {published data only}
- Fall PA, Granerus AK. Maintenance ECT in Parkinson's disease. Journal of Neural Transmission 1999;106(7‐8):737‐41. [DOI] [PubMed] [Google Scholar]
Figiel 1989 {published data only}
- Figiel G, Coffey CE, Weiner RD. Brain magnetic resonance imaging in elderly depressed patients receiving electroconvulsive therapy. Convulsive Therapy 1989;5(1):26‐34. [PubMed] [Google Scholar]
Figiel 1990a {published data only}
- Figiel GS, Coffey CE, Djang WT, Hoffman G, Doraiswamy PM. Brain magnetic resonance imaging findings in ECT‐induced delirium. Journal of Neuropsychiatry & Clinical Neurosciences 1990;2(1):53‐8. [DOI] [PubMed] [Google Scholar]
Figiel 1990b {published data only}
- Figiel GS, Krishnan KR, Doraiswamy PM. Subcortical structural changes in ECT‐induced delirium. Journal of Geriatric Psychiatry & Neurology 1990;3(3):172‐6. [DOI] [PubMed] [Google Scholar]
Figiel 1991 {published data only}
- Figiel GS, Hassen MA, Zorumski C, Krishnan KR, Doraiswamy, Jarvis MR, et al. ECT‐induced delirium in depressed patients with Parkinson's disease. Journal of Neuropsychiatry & Clinical Neurosciences 1991;3(4):405‐11. [DOI] [PubMed] [Google Scholar]
Flaherty 1984 {published data only}
- Flaherty JA, Naidu J, Dysken M. ECT, emergent dyskinesia, and depression. American Journal of Psychiatry 1984;141(6):808‐9. [DOI] [PubMed] [Google Scholar]
Flint 1997 {published data only}
- Flint AJ, Rifat SL. The treatment of psychotic depression in later life: a comparison of pharmacotherapy and ECT. International Journal of Geriatric Psychiatry 1998;13(1):23‐8. [PubMed] [Google Scholar]
Frances 1989 {published data only}
- Frances A, Weiner RD, Coffey CE. ECT for an elderly man with psychotic depression and concurrent dementia. Hospital & Community Psychiatry 1989;40(3):237‐8. [DOI] [PubMed] [Google Scholar]
Frasca 2003 {published data only}
Fraser 1978 {published data only}
- Fraser RM, Glass IB. Recovery from ECT in elderly patients. British Journal of Psychiatry 1978;133:524‐8. [DOI] [PubMed] [Google Scholar]
Fu 1999 {published data only}
- Fu W, White PF. Dexmedetomidine failed to block the acute hyperdynamic response to electroconvulsive therapy. Anesthesiology 1999;90(2):422‐4. [DOI] [PubMed] [Google Scholar]
Gallinek 1947 {published data only}
- Gallinek A. Electroconvulsive therapy in geriatrics. New York State Journal of Medicine 1947;47:1233‐41. [PubMed] [Google Scholar]
Gaspar 1982 {published data only}
- Gaspar D, Samarasinghe LA. ECT in psychogeriatric practice‐‐a study of risk factors, indications and outcome. Comprehensive Psychiatry 1982;23(2):170‐5. [DOI] [PubMed] [Google Scholar]
Godber 1983 {published data only}
- Godber C. Depression in old age. British Medical Journal Clinical Research Ed 1983;287(6394):758. [DOI] [PMC free article] [PubMed] [Google Scholar]
Godber 1987 {published data only}
- Godber C, Rosenvinge H, Wilkinson D, Smithies J. Depression in old age: prognosis after ECT. International Journal of Geriatric Psychiatry 1987;2(1):19‐24. [Google Scholar]
Gormley 1998 {published data only}
- Gormley N, Cullen C, Walters L, Philpot M, Lawlor B. The safety and efficacy of electroconvulsive therapy in patients over age 75. International Journal of Geriatric Psychiatry 1998;13(12):871‐4. [DOI] [PubMed] [Google Scholar]
Gournelis 2006 {published data only}
Greenberg 1992 {published data only}
- Greenberg L, Fink M. The use of electroconvulsive therapy in geriatric patients. Clinics in Geriatric Medicine 1992;8(2):349‐54. [PubMed] [Google Scholar]
Greenwald 1989 {published data only}
- Greenwald BS, Kramer‐Ginsberg E, Marin DB, Laitman LB, Hermann CK, Mohs RC, et al. Dementia with coexistent major depression. American Journal of Psychiatry 1989;146(11):1472‐8. [DOI] [PubMed] [Google Scholar]
Grunhaus 2003 {published data only}
Guttmacher 1989 {published data only}
- Guttmacher LB, Greenland P. Effects of electroconvulsive therapy on the electrocardiogram in geriatric patients with stable cardiovascular diseases. Convulsive Therapy 1989;6(1):5‐12. [PubMed] [Google Scholar]
Hay 1989 {published data only}
- Hay DP. Electroconvulsive therapy in the medically ill elderly. Convulsive Therapy 1989;5(1):8‐16. [PubMed] [Google Scholar]
Heshe 1978 {published data only}
- Heshe J, Roder E, Theilgaard. A psychiatric and psychological study of therapeutic effect and side effects. Acta Psychiatrica Scandinavica, Supplementum 1978;275:1‐180. [PubMed] [Google Scholar]
Hickie 1995 {published data only}
- Hickie I, Scott E, Mitchell P, Wilhelm K, Austin MP, Bennett B. Subcortical hyperintensities on magnetic resonance imaging: clinical correlates and prognostic significance in patients with severe depression. Biological Psychiatry 1995;37(3):151‐60. [DOI] [PubMed] [Google Scholar]
Hihn 2006 {published data only}
Holcomb 1983 {published data only}
- Holcomb HH, Sternberg DE, Heninger GR. Effects of electroconvulsive therapy on mood, parkinsonism, and tardive dyskinesia in a depressed patient: ECT and dopamine systems. Biological Psychiatry 1983;18(8):865‐73. [PubMed] [Google Scholar]
Hordynska 2003 {published data only}
Hunt 1998 {published data only}
- Hunt SA, Kaplan E. ECT in the presence of a cerebral aneurysm. Journal of ECT 1998;14(2):123‐4. [DOI] [PubMed] [Google Scholar]
Husain 2004 {published data only}
Hussar 1968 {published data only}
- Hussar AE, Pachter M. Myocardial infarction and fatal coronary insufficiency during electroconvulsive therapy. JAMA 1968;204(11):1004‐7. [PubMed] [Google Scholar]
Huuhka 2003 {published data only}
Huuhka 2004 {published data only}
Jenike 1983 {published data only}
- Jenike MA. Electroconvulsive therapy: what are the facts?. Geriatrics 1983;38(4):33‐8. [PubMed] [Google Scholar]
Jenike 1989 {published data only}
- Jenike MA. Treatment of affective illness in the elderly with drugs and electroconvulsive therapy. Journal of Geriatric Psychiatry 1989;22(1):77‐112. [PubMed] [Google Scholar]
Kajala 2004 {published data only}
Kamat 2003 {published data only}
Karlinsky 1984 {published data only}
- Karlinsky H, Shulman KI. The clinical use of electroconvulsive therapy in old age. Journal of the American Geriatrics Society 1984;32(3):183‐6. [DOI] [PubMed] [Google Scholar]
Kellner 2004 {published data only}
Kelly 2000 {published data only}
- Kelly KG, Zisselman M. Update on electroconvulsive therapy (ECT) in older adults. Journal of the American Geriatrics Society 2000;48(5):560‐6. [DOI] [PubMed] [Google Scholar]
Kelsey 1995 {published data only}
- Kelsey MC, Grossberg GT. Safety and efficacy of caffeine‐augmented ECT in elderly depressives: a retrospective study. Journal of Geriatric Psychiatry & Neurology 1995;8(3):168‐72. [DOI] [PubMed] [Google Scholar]
Kramer 1986 {published data only}
- Kramer BA. Severe confusion in a patient receiving electroconvulsive therapy and atenolol. Journal of Nervous & Mental Disease 1986;174(9):562‐3. [DOI] [PubMed] [Google Scholar]
Kramer 1987 {published data only}
- Kramer BA. Electroconvulsive therapy use in geriatric depression. Journal of Nervous & Mental Disease 1987;175(4):233‐5. [DOI] [PubMed] [Google Scholar]
Krause 1988 {published data only}
- Krause P, Genz A, Knorr W. Prospective study of the late sequelae of electronvulsive treatment [Prospektive studie zur spatfolge des elektroconvulsionsbehandlung]. Psychiatrie, Neurologie und Medizinische Psychologie 1988;40:532‐6. [PubMed] [Google Scholar]
Kroessler 1993 {published data only}
- Kroessler D, Fogel BS. Electroconvulsive therapy for major depression in the oldest old. American Journal of Geriatric Psychiatry 1993;1(1):30‐7. [DOI] [PubMed] [Google Scholar]
Krystal 2000 {published data only}
- Krystal AD, Holsinger T, Weiner RD, Coffey CE. Prediction of the utility of a switch from unilateral to bilateral ECT in the elderly using treatment 2 ictal EEG indices. Journal of ECT 2000;16(4):327‐37. [DOI] [PubMed] [Google Scholar]
Kuruvilla 2006 {published data only}
Lambourn 1978 {published data only}
- Lambourn J, Gill D. A controlled comparison of simulated and real ECT. British Journal of Psychiatry 1978;133:514‐9. [DOI] [PubMed] [Google Scholar]
Lebensohn 1975 {published data only}
- Lebensohn ZM, Jenkins RB. Improvement of Parkinsonism in depressed patients treated with ECT. American Journal of Psychiatry 1975;132(3):283‐5. [DOI] [PubMed] [Google Scholar]
Lekwauwa 2006 {published data only}
Levy 1983 {published data only}
- Levy LA, Savit JM, Hodes M. Parkinsonism: improvement by electroconvulsive therapy. Archives of Physical Medicine & Rehabilitation 1983;64(9):432‐3. [PubMed] [Google Scholar]
Liang 1988 {published data only}
- Liang RA, Lam RW, Ancill RJ. ECT in the treatment of mixed depression and dementia. British Journal of Psychiatry 1988;152:281‐4. [DOI] [PubMed] [Google Scholar]
Liberzon 1991 {published data only}
- Liberzon I, Dequardo JR, Sidell G, Mazzara C, Tandon R. Post‐ECT dyskinesia. Convulsive Therapy 1991;7(1):40‐4. [PubMed] [Google Scholar]
Lipman 1993 {published data only}
- Lipman RS, Brown EA, Silbert GA, Rains DG, Grady DA. Cognitive performance as modified by age and ECT history. Progress in Neuro‐Psychopharmacology & Biological Psychiatry 1993;17(4):581‐94. [DOI] [PubMed] [Google Scholar]
Little 2004 {published data only}
Loo 1991 {published data only}
- Loo H, Galinowski A, Carvalho W, Bourdel MC, Poirier MF. Use of maintenance ECT for elderly depressed patients. American Journal of Psychiatry 1991;148(6):810. [DOI] [PubMed] [Google Scholar]
Lovell 1948 {published data only}
- Lovell HW. Electric shock therapy in the aging. Geriatrics 1948;3:285‐93. [PubMed] [Google Scholar]
Magni 1988 {published data only}
- Magni G, Fisman M, Helmes E. Clinical correlates of ECT‐resistant depression in the elderly. Journal of Clinical Psychiatry 1988;49(10):405‐7. [PubMed] [Google Scholar]
Malcolm 1989 {published data only}
- Malcolm K, Peet M. ECT in old age. British Journal of Psychiatry 1989;155:713‐4. [DOI] [PubMed] [Google Scholar]
Mandel 1980 {published data only}
- Mandel MR, Madsen J, Miller AL, Baldessarini RJ. Intoxication associated with lithium and ECT. American Journal of Psychiatry 1980;137(9):1107‐9. [DOI] [PubMed] [Google Scholar]
Manly 2000 {published data only}
- Manley DT, Oakley SP, Bloch RM. Electroconvulsive therapy in old‐old patients. American Journal of Geriatric Psychiatry 2000;8(3):232‐6. [PubMed] [Google Scholar]
Martin 1992 {published data only}
- Martin M, Figiel G, Mattingly G, Zorumski CF, Jarvis MR. ECT‐induced interictal delirium in patients with a history of a CVA. Journal of Geriatric Psychiatry & Neurology 1992;5(3):149‐55. [DOI] [PubMed] [Google Scholar]
Mattingly 1991 {published data only}
- Mattingly G, Figiel GS, Jarvis MR, Zorumski CF. Prospective uses of ECT in the presence of intracranial tumors. Journal of Neuropsychiatry & Clinical Neurosciences 1991;3(4):459‐63. [DOI] [PubMed] [Google Scholar]
Meyers 1985 {published data only}
- Meyers BS, Tal Mei V. Empirical study on an inpatient psychogeriatric unit: Biological treatment in patients with depressive illness. International Journal of Psychiatry in Medicine 1985;15(2):111‐24. [DOI] [PubMed] [Google Scholar]
Mielke 1984 {published data only}
- Mielke DH, Winstead DK, Goethe JW, Schwartz BD. Multiple‐monitored electroconvulsive therapy: safety and efficacy in elderly depressed patients. Journal of the American Geriatrics Society 1984;32(3):180‐2. [DOI] [PubMed] [Google Scholar]
Morris 1991 {published data only}
- Morris PD. Which elderly depressives will respond to ect?. International Journal of Geriatric Psychiatry 1991;6(3):159‐63. [Google Scholar]
Mulsant 1991 {published data only}
- Mulsant BH, Rosen J, Thorton JE, Zubenko GS. A prospective naturalistic study of electroconvulsive therapy in late‐life depression. Journal of Geriatric Psychiatry & Neurology 1991;4(1):3‐13. [DOI] [PubMed] [Google Scholar]
Murray 1986 {published data only}
- Murray GB, Shea V, Conn DK. Electroconvulsive therapy for poststroke depression. Journal of Clinical Psychiatry 1987;47(5):258‐60. [PubMed] [Google Scholar]
Nahshoni 2001 {published data only}
Nelson 1989 {published data only}
- Nelson JP, Benjamin L. Efficacy and safety of combined ECT and tricyclic antidepressant drugs in the treatment of depressed geriatric patients. Convulsive Therapy 1989;5(4):321‐9. [PubMed] [Google Scholar]
Nelson 1991 {published data only}
- Nelson JP, Rosenberg RD. ECT treatment of demented elderly patients with major depression: A retrospective study of efficacy and safety. Convulsive Therapy 1991;7(3):157‐65. [PubMed] [Google Scholar]
O' Connor 2001 {published data only}
- O'Connor MK, Knapp R, Husain M, Rummans TA, Petrides G, Smith G, et al. The influence of age on the response of major depression to electroconvulsive therapy: a C.O.R.E. report. American Journal of Geriatric Psychiatry 2001;9(4):382‐90. [PubMed] [Google Scholar]
O'Leary 1996 {published data only}
- O'Leary DA, Lee AS. Seven year prognosis in depression. Mortality and readmission risk in the Nottingham ECT cohort. British Journal of Psychiatry 1996;169:423‐9. [DOI] [PubMed] [Google Scholar]
O'Shea 1987 {published data only}
- O'Shea B, Lynch T, Falvey J, O'Mahoney G. Electroconvulsive therapy and cognitive impairment in a very elderly depressed patient. British Journal of Psychiatry 1987;150:255‐7. [DOI] [PubMed] [Google Scholar]
Palmer 1990 {published data only}
- Palmer RL, Mani C, Abdel‐Kariem AA, Brandon S. Dexamethason suppression tests in the context of a double‐blind trial of electroconvulsive therapy and simulated ECT. Convulsive Therapy 1990;6(1):13‐8. [PubMed] [Google Scholar]
Pande 1990 {published data only}
- Pande AC, Grunhaus LJ, Aisen AM, Haskett RF. A preliminary magnetic resonance imaging study of ECT‐treated depressed patients. Biological Psychiatry 1990;27(1):102‐4. [DOI] [PubMed] [Google Scholar]
Petrides 1996 {published data only}
- Petrides G, Fink M. Atrial fibrillation, anticoagulation, and electroconvulsive therapy. Convulsive Therapy 1996;12(2):91‐8. [PubMed] [Google Scholar]
Pettinati 1984 {published data only}
- Pettinati HM, Bonner KM. Cognitive functioning in depressed geriatric patients with a history of ECT. American Journal of Psychiatry 1984;141(1):49‐52. [DOI] [PubMed] [Google Scholar]
Philibert 1995 {published data only}
- Philibert RA, Richards L, Lynch CF, Winokur G. Effect on ECT on mortality and clinical outcome in geriatric unipolar depression. Journal of Clinical Psychiatry 1995;56(9):390‐4. [PubMed] [Google Scholar]
Price 1989 {published data only}
- Price TR, McAllister TW. Safety and efficacy of ECT in depressed patients with dementia; A review of clinical evidence. Convulsive Therapy 1989;5(1):61‐74. [PubMed] [Google Scholar]
Prudic 1987 {published data only}
Rabkeru 2003 {published data only}
Rao 2000 {published data only}
- Rao V, Lyketsos CG. The benefits and risks of ECT for patients with primary dementia who also suffer from depression. International Journal of Geriatric Psychiatry 2000;15(8):729‐35. [DOI] [PubMed] [Google Scholar]
Regestein 1980 {published data only}
- Regestein QR, Lind LJ. Management of electroconvulsive treatment in an elderly woman with severe hypertension and cardiac arrhytmias. Comprehensive Psychiatry 1980;21(4):288‐91. [DOI] [PubMed] [Google Scholar]
Reynolds 1987 {published data only}
- Reynolds CF, Perel JM, Kupfer DJ, Zimmer B, Stack JA, Hoch CC. Open‐trial response to antidepressant treatment in elderly patients with mixed depression and cognitive impairment. Psychiatry Research 1987;21(2):111‐22. [DOI] [PubMed] [Google Scholar]
Rice 1994 {published data only}
- Rice EH, Sombrotto LB, Markowitz JC, Leon AC. Cardiovascular morbidity in high‐risk patients during ECT. American Journal of Psychiatry 1994;151(11):1637‐41. [DOI] [PubMed] [Google Scholar]
Rosen 1992 {published data only}
- Rosen J, Mulsant BH, Nebes RD. A pilot study of interictal cognitive changes in elderly patients during ECT. International Journal of Geriatric Psychiatry 1992;7(6):407‐10. [Google Scholar]
Rubin 1993 {published data only}
- Rubin EH, Kinscherf DA, Figiel GS, Zorumski CF. The nature and time course of cognitive side effects during electroconvulsive therapy in the elderly. Journal of Geriatric Psychiatry & Neurology 1993;6(2):78‐83. [DOI] [PubMed] [Google Scholar]
Ruxin 1994 {published data only}
- Ruxin EH, Ruedrich S. ECT in combined multiple system atrophy and major depression. Convulsive Therapy 1994;10(4):298‐300. [PubMed] [Google Scholar]
Salaris 2000 {published data only}
- Salaris S, Szuba MP, Traber K. ECT and intracranial vascular masses. Journal of ECT 2000;16(2):198‐203. [DOI] [PubMed] [Google Scholar]
Salzman 1982 {published data only}
- Salzman C. Electroconvulsive therapy in the elderly patient. Psychiatric Clinics of North America 1982;5(1):191‐7. [PubMed] [Google Scholar]
Salzman 2002 {published data only}
Scott 1990 {published data only}
- Scott AI, Turnbull LW. Do repeated courses of ECT cause brain damage detectable by MRI?. American Journal of Psychiatry 1990;147(3):371‐2. [DOI] [PubMed] [Google Scholar]
Scott 1991 {published data only}
- Scott AI, Turnbull LW, Blane A, Douglas RH. Electroconvulsive therapy and brain damage. Lancet 1991;338(8761):264. [DOI] [PubMed] [Google Scholar]
Serra 2006 {published data only}
Simpson 1998 {published data only}
- Simpson S, Baldwin RC, Jackson A, Burns AS. Is subcortical disease associated with a poor response to antidepressants? Neurological, neuropsychological and neuroradiological findings in late‐life depression.. Psychological Medicine 1998;28(5):1015‐26. [DOI] [PubMed] [Google Scholar]
Smith 2000 {published data only}
- Smith K, Keepers G. Nonconvulsive status epilepticus after ECT. American Journal of Psychiatry 2000;157(9):1524. [DOI] [PubMed] [Google Scholar]
Sommer 1989 {published data only}
- Sommer BR, Satlin A, Friedman L, Cole JO. Glycopyrrolate versus atropine in post‐ECT amnesia in the elderly. Journal of Geriatric Psychiatry & Neurology 1989;2(1):18‐21. [DOI] [PubMed] [Google Scholar]
Spear 1997 {published data only}
- Spear J, Ranger M, Herzberg J. The treatment of stupor associated with MRI evidence of cerebrovascular disease. International Journal of Geriatric Psychiatry 1997;12(8):791‐4. [PubMed] [Google Scholar]
Stack 1988 {published data only}
- Stack JA, Reynolds CF, Perel JM, Houck PR, Hoch CC, Kupfer DJ. Pretreatment systolic orthostatic blood pressure (PSOP) and treatment response in elderly depressed inpatients. Journal of Clinical Psychopharmacology 1988;8(2):116‐20. [PubMed] [Google Scholar]
Stern 1997 {published data only}
- Stern L, Hirschman S, Grunhaus L. ECT in patients with major depressive disorder and low cardiac output. Convulsive Therapy 1997;13(2):68‐73. [PubMed] [Google Scholar]
Stoudemire 1990 {published data only}
- Stoudemire A, Knos G, Gladson M, Markwalter H, Sung YF, Morris R, et al. Labetolol in the control of cardiovascular responses to electroconvulsive therapy in high‐risk depressed medical patients. Journal of Clinical Psychiatry 1990;51(12):508‐12. [PubMed] [Google Scholar]
Stoudemire 1991 {published data only}
- Stoudemire A, Hill CD, Morris R, Martino‐Saltzman D, Markwalter H, Lewison B. Cognitive outcome following tricyclic and electroconvulsive treatment of major depression in the elderly. American Journal of Psychiatry 1991;148(10):1336‐40. [DOI] [PubMed] [Google Scholar]
Stoudemire 1993 {published data only}
- Stoudemire A, Hill CD, Morris R, Martino‐Saltzman D, Lewison B. Long‐term affective and cognitive outcome in depressed older adults. American Journal of Psychiatry 1993;150(6):896‐900. [DOI] [PubMed] [Google Scholar]
Stoudemire 1994 {published data only}
- Stoudemire A, Hill CD, Dalton ST, Marquardt MG. Rehospitalization rates in older depressed adults after antidepressant and electroconvulsive therapy treatment. Journal of the American Geriatrics Society 1994;42(12):1282‐5. [DOI] [PubMed] [Google Scholar]
Stoudemire 1995 {published data only}
- Stoudemire A, Hill CD, Morris R, Dalton ST. Improvement in depression‐related cognitive dysfunction following ECT. Journal of Neuropsychiatry & Clinical Neurosciences 1995;7(1):31‐4. [DOI] [PubMed] [Google Scholar]
Strain 1971 {published data only}
- Strain JJ, Bidder TG. Transient cerebral complication associated with multiple monitored electroconvulsive therapy. Diseases of the Nervous System 1971;32(2):95‐100. [PubMed] [Google Scholar]
Suzuki 2006 {published data only}
Swett 1977 {published data only}
- Swett CP, Shader RI. Cardiac side effects and sudden death in hospitalized psychiatric patients. Diseases of the Nervous System 1977;38(2):69‐72. [PubMed] [Google Scholar]
Tamam 2003 {published data only}
Tancer 1987 {published data only}
- Tancer ME, Pedersen CA, Evans DL. ECT and anticoagulation. Convulsive Therapy 1987;3:222‐7. [PubMed] [Google Scholar]
Tew 1999 {published data only}
- Tew JD, Mulsant BH, Haskett RF, Prudic J, Thase ME, Crowe RR, et al. Acute efficacy of ect in the treatment of major depression in the old‐old. American Journal of Psychiatry 1999;156(12):1865‐70. [DOI] [PubMed] [Google Scholar]
Tew 2002 {published data only}
Thienhaus 1990 {published data only}
- Thienhaus OJ, Margletta S, Bennett JA. A study of the clinical efficacy of maintenance ECT. Journal of Clinical Psychiatry 1990;51(4):141‐4. [PubMed] [Google Scholar]
Thompson 2001 c {unpublished data only}
Tomac 1997 {published data only}
- Tomac TA, Pileggi TA, Rummans TS, Hongzhe L. Safety and efficacy of electroconvulsive therapy in patients over age 85. American Journal of Geriatric Psychiatry 1997;5(2):126‐30. [PubMed] [Google Scholar]
Van Marwijk 1988 {published data only}
- Marwijk HW, Bekker FM, Hop WC, Jansen PA, Nieuwkerk JF. Elelctroconvulsive therapy in depressed elderly subjects; a retrospective study of efficacy and safety [Electroconvulsietherapie bij depressieve bejaarde; een retrospectief onderzoek naar werkzaamheid en veiligheid]. Nederlands Tijdschrift voor Geneeskunde 1988;132(30):1396‐9. [PubMed] [Google Scholar]
Van Waarde 2001 {published data only}
- Waarde JA, Stek ML. Electroconvulsive therapy effective and safe in 55 patients aged 56 years and older with mood disorders and physical comorbidity [Elektroconvulsietherapie effectief en veilig bij 55 patienten van 56 jaar en ouder met stemmingsstoornissen en somatische comorbiditeit]. Nederlands Tijdschrift voor Geneeskunde 2001;145(35):1693‐7. [PubMed] [Google Scholar]
Ware 1990 {published data only}
- Ware MR, Frost ML, Berger JJ, Stewart RB, DeVane CL. Electroconvulsive therapy complicated by insecticide ingestion. Journal of Clinical Psychopharmacology 1990;10(1):72‐3. [DOI] [PubMed] [Google Scholar]
Weiner 1982 {published data only}
- Weiner RD. The role of electroconvulsive therapy in the treatment of depression in the elderly. Journal of the American Geriatrics Society 1982;30(11):710‐2. [DOI] [PubMed] [Google Scholar]
Weisberg 1991 {published data only}
- Weisberg LA, Elliott D, Mielke D. Intracerebral hemorrhage following electroconvulsive therapy. Neurology 1991;41(11):1849. [DOI] [PubMed] [Google Scholar]
Wesson 1997 {published data only}
- Wesson ML, Wilkinson AM, Anderson DN, Cracken CM. Does age predict the long‐term outcome of depression treated with ECT? (a prospective study of the long‐term outcome of ECT‐treated depression with respect to age). International Journal of Geriatric Psychiatry 1997;12(1):45‐51. [DOI] [PubMed] [Google Scholar]
West 1999 {published data only}
- West S, Hewitt J. Prolonged hypertension: A case report of a potential interaction between electroconvulsive therapy and venlafaxine. International Journal of Psychiatry in Clinical Practice 1999;3(1):55‐7. [DOI] [PubMed] [Google Scholar]
Wetterling 1998 {published data only}
- Wetterling T, Michels R, Dilling H. Electroconvulsive therapy in therapy refractory depression in the elderly. Report of experiences [Elektrokrampftherapie bei therapieresistenter altersdepression. Ein erfahrungsbericht]. Nervenartz 1998;69(7):617‐21. [DOI] [PubMed] [Google Scholar]
Wijeratne 1999 {published data only}
- Wijeratne C, Shome S. Electroconvulsive therapy and subdural hemorrhage. Journal of ECT 1999;15(4):275‐9. [PubMed] [Google Scholar]
Wilkinson 1993 {published data only}
- Wilkinson AM, Anderson DN, Peters S. Age and the effects of ECT. International Journal of Geriatric Psychiatry 1993;8(3):401‐6. [Google Scholar]
Williams 1997 {published data only}
- Williams JH, O'Brien JT, Cullum S. Time course of response to electroconvulsive therapy in elderly depressed subjects. International Journal of Geriatric Psychiatry 1997;12(5):563‐6. [PubMed] [Google Scholar]
Wolff 1954 {published data only}
- Wolff GE, Garrett FH. Electric shock treatments in elderly mental patients. Geriatrics 1954;9:316‐8. [PubMed] [Google Scholar]
Yesavage 1980 {published data only}
- Yesavage JA, Berens ES. Multiple monitored electroconvulsive therapy in the elderly. Journal of the American Geriatrics Society 1980;28(5):206‐9. [DOI] [PubMed] [Google Scholar]
Young 1985 {published data only}
- Young RC, Alexopoulos GS, Shamoian CA. Dissociation of motor response from mood and cognition in a parkinsonian patient treated with ECT. Biological Psychiatry 1985;20(5):566‐9. [DOI] [PubMed] [Google Scholar]
Yudofsky 1979 {published data only}
- Yudofsky SC. Parkinson's disease, depression, and electroconvulsive therapy: a clinical and neurobiologic synthesis. Comprehensive Psychiatry 1979;20(6):579‐81. [DOI] [PubMed] [Google Scholar]
Zorumski 1988 {published data only}
- Zorumski CF, Rubin EH, Burke WJ. Electroconvulsive therapy for the elderly: a review. Hospital & Community Psychiatry 1988;39(6):643‐47. [DOI] [PubMed] [Google Scholar]
Zubenko 1994 {published data only}
- Zubenko GS, Mulsant BH, Hind Rifai A, Sweet RA, Pasternak RE, Marino LJ, et al. Impact of acute psychiatric inpatient treatment on major depression in late life and prediction of response. American Journal of Psychiatry 1994;151(7):987‐94. [DOI] [PubMed] [Google Scholar]
Zwil 1992 {published data only}
- Zwil AS, McAllister TW, Price TR. Safety and efficacy of ECT in depressed patients with organic brain disease: a review of clinical experience. Convulsive Therapy 1992;8(2):103‐9. [PubMed] [Google Scholar]
Zwil 1997 {published data only}
- Zwil AS, Pomerantz A. Transient postictal psychosis associated with a course of ECT. Convulsive Therapy 1997;13(1):32‐6. [PubMed] [Google Scholar]
References to ongoing studies
Kellner 2006 {published data only (unpublished sought but not used)}
- CORE 2001. Ongoing study Starting date of trial not provided. Contact author for more information.
Additional references
Alexopoulos 1997
- Alexopoulos GS, Meyers BS, Young RC, Campbell S, Silbersweig D, Charlson M. Vascular depression hypothesis. Archives of General Psychiatry 1997;54(10):915‐22. [DOI] [PubMed] [Google Scholar]
Beekman 1999
- Beekman AT, Copeland JR, Prince MJ. Review of community prevalence of depression in late life. Britisch Journal of Psychiatry 1999;174:307‐11. [DOI] [PubMed] [Google Scholar]
Beekman 2000
- Beekman AT, Beurs E, Balkom AJ, Deeg DJ, Dyck R, Tilburg W. Anxiety and depression in later life: Co‐occurence and communality of risk factors. American Journal of Psychiatry 2000;157(1):89‐95. [DOI] [PubMed] [Google Scholar]
Coffey 1988
- Coffey CE, Figiel GS, Djang WT, Cress M, Saunders WB, Weiner RD. Leukoencephalopathy in elderly depressed patients referred for ECT. Biological Psychiatry 1988;24(2):143‐61. [DOI] [PubMed] [Google Scholar]
Deuschle 1997
- Deuschle M, Cotthardt U, Schweige U, Webe B, Kunen A, Standhardt H, et al. With aging in humans the activity of the hypothalamus‐pituitary‐adrenal system increases and the diurnal amplitude flattens. Life Sciences 1997;61(22):2239‐46. [DOI] [PubMed] [Google Scholar]
Devanand 1994
- Devanand DP, Dwork AJ, Hutchinson ER, Bolwig TG, Sackeim HA. Does ECT alter brain structure?. American Journal of Psychiatry 1994;151(7):957‐70. [DOI] [PubMed] [Google Scholar]
Feighner 1972
- Feighner JP, Robins E, Guze SB, Woodruff RA, Winokur G, Munoz R. Diagnostic criteria for use in psychiatric research. Archives of General Psychiatry 1972;26(1):57‐63. [DOI] [PubMed] [Google Scholar]
Flint 1998
- Flint AJ, Rifat SL. The treatment of psychotic depression in later life: A comparison of pharmacotherapy and ECT. International Journal of Geriatric Psychiatry 1998;13(1):23‐8. [PubMed] [Google Scholar]
Frasure‐Smith 1993
- Frasure‐Smith N, Lesperance F, Talajic M. Depression following myocardial infarction. Impact on 6‐month survival. JAMA 1993;270(15):1819‐25. [PubMed] [Google Scholar]
Glen 1999
- Glen T, Scott A. Rates of electroconvulsive therapy use in Edinburgh 1992‐1997. Journal of Affective Disorders 1999;54(1‐2):81‐5. [DOI] [PubMed] [Google Scholar]
Gregory 1985
- Gregory S, Shawcross CR, Gill D. The Nottingham ECT study. A double‐blind comparison of bilateral, unilateral and simulated ECT in depressive illness. British Journal of Psychiatry 1985;146:520‐4. [DOI] [PubMed] [Google Scholar]
Hamilton 1960
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry 1960;23:56‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2005
- Higgins JPT, Greens S, Editors. Cochrane Handbook for Systematic Reviews of Interventions 4.2.5 [updated May 2005].. www.cochrane.org/resources/handbook/hbook.htm.
Holsboer 1995
- Holsboer F, Lauer CJ, Schreiber W, Krieg JC. Altered hypothalamic‐pituitary‐adrenocortical regulation in healthy subjects at high familial risk for affective disorders. Neuroendocrinology 1995;62(3):340‐7. [DOI] [PubMed] [Google Scholar]
Holsboer 1996
- Holsboer F, Barden N. Antidepressants and hypothalamic‐hypopituitary‐adrenocortical regulation. Endocrine Reviews 1996;17(2):187‐205. [DOI] [PubMed] [Google Scholar]
Lancaster 1958
- Lancaster NP, Steinert RR, Frost I. Unilateral electroconvulsive therapy. Journal of Mental Science 1958;104:221‐7. [DOI] [PubMed] [Google Scholar]
Maes 1995
- Maes M, Smith R, Scharpe S. The Monocyte‐T‐Lymfocyte Hypothesis of major depression. Psychoneuroendocrinology 1995;20(2):111‐6. [DOI] [PubMed] [Google Scholar]
Montgomery 1979
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. British Journal of Psychiatry 1979;134:382‐9. [DOI] [PubMed] [Google Scholar]
Moskowitz 1986
- Moskowitz H, Burns MM. Cognitive performance in geriatric subjects after acute treatment with antidepressants. Neuropsychobiology 1986;15(Suppl 1):38‐43. [DOI] [PubMed] [Google Scholar]
Mottram 2006
- Mottram P, Wilson K, Strobl J. Antidepressants for elderly depressed. Cochrane Database of Systematic Reviews 2006, Issue 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ormel 1999
- Ormel J, Vonkorff M, Oldehinkel AJ, Simon G, Timens BG, Ustun TB. Onset of disability in depressed and non‐depressed primary care patients. Psychological Medicine 1999;29(4):847‐53. [DOI] [PubMed] [Google Scholar]
Pantoni 1995
- Pantoni L, Garcia JH. The significance of cerebral white matter abnormalities 100 years after Binswanger's report, a review. Stroke 1995;26(7):1293‐301. [DOI] [PubMed] [Google Scholar]
Pantoni 1997
- Pantoni L, Garcia JH. Pathogenesis of leukoaraiosis: A review. Stroke 1997;28(3):652‐9. [DOI] [PubMed] [Google Scholar]
Penninx 1999
- Penninx BW, Geerlings SW, Deeg DJ, Eijk JT, Tilburg W, Beekman AT. Minor and major depression and the risk of death in older persons. Archives of General Psychiatry 1999;56(10):889‐95. [DOI] [PubMed] [Google Scholar]
Rice 1994
- Rice EH, Sombrotto LS, Markowitz JC, Leon AC. Cardiovascular morbidity in high‐risk patients during ECT. American Journal of Psychiatry 1994;151(11):1637‐41. [DOI] [PubMed] [Google Scholar]
Roose 2004
- Roose SP, Sackeim HA. Late‐life depression. US: Oxford University Press Inc, 2004. [Google Scholar]
Salzman 1992
- Sackeim H. Electroconvulsive therapy in late‐life depression. Clinical Geriatric Psychopharmacology. US: Lippincott Williams & Wilkins, 1992. [Google Scholar]
Schneider 1995
- Schneider LS, Olin JT. Efficacy of acute treatment for geriatric depression. International Psychogeriatrics 1995;7(Suppl):7‐25. [DOI] [PubMed] [Google Scholar]
Scott 1995
- Scott AL. Does ECT alter brain structure. American Journal of Psychiatry 1995;152(9):1403. [DOI] [PubMed] [Google Scholar]
Simpson 1997
- Simpson S, Jackson A, Baldwin RC, Burns A. Subcortical hyperintensities in late‐life depression: acute response to treatment and neuropsychological impairment. International Psychogeriatrics 1997;9(3):257‐75. [DOI] [PubMed] [Google Scholar]
Simpson 1998
- Simpson S, Baldwin RC, Jackson A, Burns AS. Is subcortical disease associated with a poor response to antidepressants? Neurological, neuropsychological and neuroradiological findings in late‐life depression. Psychological Medicine 1998;28(5):1015‐26. [DOI] [PubMed] [Google Scholar]
Song 1998
- Song C, Lin A, Bonaccorso S, Heide C, Verkerk R, Kenis G, et al. The inflammatory response system and the availability of plasma tryptophan in patients with primary sleep disorders and major depression. Journal of Affective Disorders 1998;49(3):211‐9. [DOI] [PubMed] [Google Scholar]
Stromgren 1973
- Stromgren LS. Unilateral versus bilateral electroconvulsive therapy. Investigations into the therapeutic effect in endogenous depression. Acta Psychiatrica Scandinavica, Supplementum 1973;240:8‐65. [PubMed] [Google Scholar]
van der Wurff 2003
- Wurff FB, Stek ML, Hoogendijk WJ, Beekman AT. The efficacy and safety of ECT in depressed older adults: a literature review. International Journal of Geriatric Psychiatry 2003;18(10):894‐904. [DOI] [PubMed] [Google Scholar]
Wilson 2001
- Wilson K, Mottram P, Sivanranthan A, Nightingale A. Antidepressants versus placebo for the depressed elderly (Cochrane Review). The Cochrane Library 2001, Issue 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Woodhouse 1992
- Woodhouse K. Wyne HA. Age related changes in hepatic function. Implications for drug therapy. Drugs Aging 1992;2:243‐55. [DOI] [PubMed] [Google Scholar]


