Abstract
Purpose
The knowledge of genetics among medical students was assessed to identify and analyze gaps that serve as bases for the revision of the current genetics curriculum of the (Bachelor of Medicine, Bachelor of Surgery) MBBS Program of the College of Medicine at Princess Nourah bint Abdulrahman University (PNU).
Methods
A 65-item multiple-choice (MCQs) test in Genetics was administered to 71 second and fourth-year medical students to assess their knowledge in Genetics. MCQs were validated and tested for their reliability. Self-assessment of students’ genetics knowledge was also determined by asking them whether their knowledge in genetics is sufficient or not sufficient for their future clinical practice. Data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 20.
Results
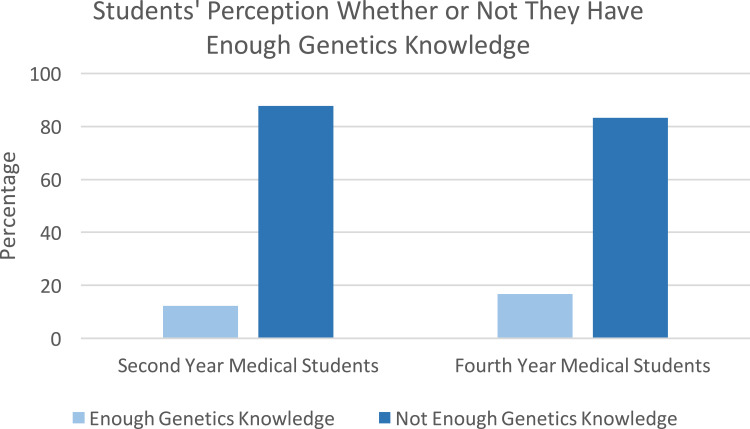
Forty-one second-year and thirty fourth-year medical students took the Genetic test. Exam results showed insufficient knowledge of Genetics, with 43.85% among the students answering the exam correctly. In self-assessment, the majority (83.3% to 87.8%) of the respondents considered their knowledge of genetics insufficient for future clinical practice. A higher knowledge level of basic genetics compared with clinically related genetics concepts was observed. Generally, second-year students significantly scored higher in molecular and cytogenetics (P=0.012), principles of genetic transmission (P=0.022), and inheritance of genetic diseases (P=0.024), compared with the fourth-year medical students who only scored higher in items related to cancer genetics (P=0.022).
Conclusion
Medical students’ genetics knowledge is insufficient, especially on clinically oriented concepts like genetic testing and genetic counseling and should be strengthened for future clinical practice. The fourth-year medical students do not retain the knowledge of genetics; thus, integrating medical genetics in clinical years is imperative.
Keywords: genetics knowledge, medical genetics, genomic medicine, genetics curriculum, assessment
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Even after the discovery of the DNA structure, genetics had a limited role in human health professions. Still, in the late 1980s, human genetics was not a required course for students seeking to enter the medical profession.1 The revelation of the genetic susceptibility to prevalent conditions like cancer, cardiovascular disease, and even psychiatric illness was eventually recognized as a significant contribution of genetics to medicine. The discovery of rare genetic illnesses and disorders only added to this.2 Indeed, Genetics should be taught at every medical school. However, the completion of the Human Genome Project (HGP) and breakthroughs in DNA sequencing technology have improved our understanding of rare diseases, allowing for the development of noninvasive prenatal screening strategies and precision medicine treatment.3 Since then, human and medical genetics has undergone a substantial transition into genomic medicine.
According to the National Human Genome Research Institute (NHGRI), Genomic medicine is an interdisciplinary medical specialty including the use of genomic information in clinical care and health outcomes.4 It promises disease prevention and early diagnosis in the context of precision medicine.5 Precision medicine was, in fact, conceptualized on the strength of genomic sequence analysis.6 Indeed, genomic medicine’s journey from Mendel through next-generation sequencing (NGS) to HGP opened the way for a paradigm shift toward using a person’s genetic profile to guide decisions about disease prevention, diagnosis, and treatment.7 The completion of the HGP has revolutionized clinical approaches to diagnosis.8 Currently, genomic testing is being employed for tumor molecular characterization, preconception carrier screening, prenatal and postnatal detection of atypical disorders, and infectious disease diagnosis.9 We now face the prospect of employing gene-editing technology to not only precisely predict illness risk and tailor existing treatments based on genetic and non-genetic factors but also to potentially cure or even eliminate some diseases.10
We are currently witnessing a shift in medical genomics, with an average of ten new genetic testing items being produced every day, indicating that genomic testing is becoming more common in clinical practice.11 Genetic services are in high demand in clinical and direct-to-consumer (DTC) settings due to advancements in technology, lower testing prices, and more public awareness.12 However, these advancements raise the demand for health care clinicians who are competent and efficient in their use of emerging genomic technologies in clinical practice.9,12 Is there a sufficient number of physicians and genetics specialists to deliver these transformative approaches? According to several research studies, physicians are primarily unprepared to use genetic and genomic data.13–15 It was also noted that the rapid expansion of genomic medicine created a gap between the need for genetics services and the workforce capacity needed to increase the number of clinical geneticists and satisfy the rising patient demands.16
Because genomic medicine is not fully addressed in the most existing medical curriculum, medical students and educators recognize the need for training in genomic medicine.12,17,18 More importantly, medical students’ knowledge of genetics is critical for their future clinical practice. The American Society of Human Genetics (ASHG) and the Association of Professors of Human and Medical Genetics (APHMG) both stressed the need of every physician to have a thorough understanding of human genetics concepts and their application to a wide range of clinical problems.19 Medical School Core Curriculum was developed to guide medical schools regarding medical genetics knowledge, skills, and behaviors that future physicians require. The structure and function of genes and the general organization of the human genome are among the genetic knowledge requirements proposed by ASHG and APHMG. Other topics include genes and diseases, chromosomes and their abnormalities, population genetics, and the application of genetics in medical practice. Future physicians must be trained in applying basic genetic principles and genomic technologies to diverse fields of medicine.19
The Kingdom of Saudi Arabia (KSA) has large family sizes and high rates of consanguinity20,21 when compared to other populations. Genetic diseases have become a burden for the kingdom due to increasing autosomal recessive disorders.22 Because of the high prevalence of genetic abnormalities in the population, the Saudi government has made premarital genetic disease testing mandatory.23 There are approximately 40 qualified Saudi clinical geneticists and 14 certified Saudi genetic counselors in practice, with several more in training both locally and overseas.21 Given the scarcity of clinical geneticists and counselors and the increased demand for genetic services, medical graduates should be equipped with the needed genetics knowledge and skills. These medical graduates can do initial genetic screening and counseling for common familial inherited disorders. The 2030 vision of the Saudi government has a positive impact on genetic services within the kingdom like clinical diagnostic, therapeutic facilities, prevention programs such as neonatal screening, premarital screening, and preimplantation genetic diagnosis. The Saudi Human Genome Program is the largest genome initiative in the Middle East, which aims to reduce and prevent genetic diseases. Saudi geneticists with advanced training are so critical to the establishment and continuity of genetic services in KSA. Clinical diagnostic, therapeutic, and preventative programs such as neonatal screening, premarital screening, and preimplantation genetic diagnosis are currently accessible in Saudi Arabia.21
In this study, the current Genetics Curriculum of the Bachelor of Medicine, Bachelor of Surgery (MBBS) Program of PNU is presented and evaluated in regards to the genetics knowledge requirements that future physicians should manifest as proposed by the ASHG and the APHMG. The Genetics knowledge of the second-year and fourth-year medical students was assessed through the Multiple Choice Questions (MCQs) test and self-assessment survey questionnaire. Results were used to identify the gaps in students’ knowledge of genetics that served as bases for the revision improvement of the current Genetics curriculum of the MBBS Program of the College of Medicine at Princess Nourah bint Abdulrahman University (PNU).
Materials and Methods
Study Setting
The Bachelor of Medicine and Surgery Program of the College of Medicine at PNU in Saudi Arabia has followed a unique Problem-based hybrid curriculum from its inception in 2012. The program begins with a two-year pre-clinical basic sciences course that is delivered in a block system. These include the Foundation Block, Musculoskeletal, Cardiovascular, Respiratory, and Renal Blocks for first-year students. Blocks for second-year students include the Central Nervous System, Endocrine, Gastrointestinal and Hematology, and Reproduction.
Following the weekly themes, basic science courses such as anatomy, physiology, biochemistry, genetics, pathology, microbiology, and pharmacology are integrated into each block. Within each block, there are lectures, practical or laboratory sessions in various subjects, learning skills, medical professionalism, self-directed learning (SDL), an introduction to clinical skills sessions such as intramuscular injection (IM) and cardiopulmonary resuscitation (CPR), and problem-based learning (PBL). In their third and fourth years, medical students attend clinical courses with integrated Hospital rotations.24
Since the commencement of the MBBS program in 2012, the genetics curriculum of PNU’s MBBS program has undergone substantial changes. Limited topics like Human Chromosomes; Genotypes and Phenotypes; Chromosome Anomalies; Patterns of Inheritance; Genetic Counseling Exercise; and Genetics of Breast and Ovarian Cancers were covered originally in Genetics lectures. These lectures lasted 7 hours and were given during the Foundation and Reproduction Blocks. Since then, various medical genetics and biochemistry topics have been added to the various blocks, totaling 29 contact hours, as indicated in Table 1. The Foundation Block covers the vast majority of genetics topics (48.3%).
Table 1.
Topics in Genetics Covered in the Pre-Clinical Years of the MBBS Program
| First & Second Years Blocks which Integrate Genetic Lectures | Topics | Number of Hours |
|---|---|---|
| Foundation Block | Nucleic acid structure and function; Regulation of gene expression; Types of Mutation in Genetic Diseases; Human Chromosomes; Genotypes &Phenotype; Chromosome Anomalies; Patterns of Inheritance; Karyotyping in genetic (practical); DNA Extraction (practical); Genetic Counseling Exercise | 14 |
| MSK Block | Inheritance of Muscular Dystrophy | 1 |
| Cardio-vascular Block | Inheritance of Arrhythmias and Cardiomyopathy | 1 |
| Respiratory Block | Genetics of Cystic Fibrosis | 1 |
| Renal Block | Genetics of Renal Disorders | 1 |
| Nervous System Block | Genetics of Common Hereditary Neurological Disorders | 1 |
| Gastro-intestinal Block | Inherited Disorders of Gastro-intestinal Tract | 1 |
| Endocrine Block | Genetic Basis of Common Thyroid Disorders Inheritance of Polygenic and Monogenic Diabetes |
2 |
| Reproduction Block | Genetics of breast and ovarian cancers; Genetic Counselling for Breast Cancer; Introduction to next generation sequencing; Problem-based Learning: Monosomy | 7 |
Study Participants
The study included 41 second-year and 30 fourth-year medical students from PNU’s College of Medicine. Students in the second year have just finished their pre-clinical, basic science courses, which included genetic lectures and practical sessions. The fourth year students are taking clinical courses like surgery, medicine, gynecology, and dermatology with integrated hospital rotations. Because genetics is taught only in the first and second (pre-clinical) years of the MBBS program, fourth-year students took genetics lectures during their pre-clinical years. Prior to the start of the study, the students were asked to participate voluntarily in the self-assessment survey and in the genetics MCQs test.
Preparation and Administration of Genetics MCQs
The Genetics MCQs were prepared from different topics in Genetics in our MBBS curriculum, including molecular and cytogenetics, biochemical genetics, gene regulation, Mendelian inheritance, polygenic inheritance, cancer genetics, and genetic counseling. A test blueprint was prepared to specify what the test should cover and determine the number of MCQs to formulate. The researchers prepared 70 MCQs using the required genetics reference book provided to the students, from the lectures given, and other references written in each blocks’ student guide. Two medical genetics experts, one biology professor specializing in genetics, and one biochemistry expert validated the 70 MCQs. The validators recommended removing four questions because they were “less relevant” to Genetics and more focused on Biochemistry. For the sake of clarity, two questions were rephrased. The remaining 66 multiple-choice questions (MCQs) were pilot tested with 15 students. The majority of the students indicated that they did not comprehend one question; thus, it was eliminated. The remaining 65 MCQs were used to test medical students’ genetics knowledge. The reliability of the exam questions was tested by calculating the difficulty index and discrimination index, and MCQs were also tested for internal consistency using Cronbach alpha. Box 1 shows the examples of the MCQs given to second and fourth-year medical students.
Box 1.
Examples of Genetics MCQs
| 1. Which of the following mutations is a point mutation that changes a codon specifying an amino acid into a stop codon? |
| A. Deletion C. Missense |
| B. Insertion D. Nonsense* |
| 2. Mosaic individuals who have cells with different numbers of chromosomes are most likely caused by which of the events in cell division? |
| A. Failure of chromosome to replicate |
| B. Interference during the crossing over |
| C. Non-disjunction during meiosis |
| D. Non-disjunction during mitosis* |
| 3. Taysach’s disease is an autosomal recessive disorder which is manifested in a person with homozygous recessive for the trait (tt). A couple who do not have Taysachs gave birth to a baby with Taysachs. Which of the following are the genotypes of the parents? |
| A. Tt x tt C. TT x Tt |
| B. Tt x Tt * D. TT x TT |
| 4. A 28 year-old mentally retarded patient presents with hypotonia, obesity, short stature with small hands, feet, and mouth as well as impaired sexual development. His karyotype reveals deletion in the proximal arm of chromosome 15. Which among the following syndromes is the most likely diagnosis? |
| A. Angelman syndrome |
| B. Beckwith-Wiedemann syndrome |
| C. Prader-Willi syndrome * |
| D. Silver–Russell syndrome |
| 5. Karyotyping can be used to diagnose which of the following genetic disorders? |
| A. Color blindness C. Edward’s syndrome* |
| B. Hemophilia D. Muscular dystrophy |
| 6. A 36-year-old male’s family pedigree showed an inheritance of LQT1 (Romano-Ward Syndrome) and genetic test showed that he is a carrier of a mutated KCNQ1 gene but never develops features of the syndrome. Which of the following patterns of inheritance is shown in this case? |
| A. Autosomal dominant C. New mutation |
| B. Autosomal recessive D. Reduced penetrance* |
| 7. To reduce the risk of having a child with a genetic disorder, genetic testing can be offered. Which of the following testing methodologies can be used to detect genetic changes in embryos that were created using in-vitro fertilization? |
| A. Carrier test C. Pre-natal test |
| B. New born screening D. Pre-implantation test* |
| 8. A 20-year-old male presents with more than 100 colorectal polyps and a carrier of APC gene mutation on chromosome 5q21 resulting in an autosomal dominant condition. Which of the given types of CRC is most likely shown in this case? |
| A. Familial adenomatous polyposis* |
| B. Attenuated Familial adenomatous polyposis |
| C. MUTYH-associated polyposis |
| D. Hereditary Non-polyposis colorectal cancer |
Note: An asterisk symbol (*) indicates the correct answer from the given choices.
Self-Assessment of Genetics Knowledge
Second-year and fourth-year medical students were also asked to self-assess their understanding of essential genetics topics. They were requested to indicate whether their knowledge of genetics is sufficient or not sufficient in preparation for future clinical practice.
Data Analysis
The data were reported using descriptive statistics, including percentage, mean, and standard deviation (SD). The MCQs’ difficulty and discrimination index and internal consistency using Cronbach alpha were analyzed. The mean exam scores of second-year and fourth-year medical students in each topic were compared using the t-test, and p = < 0.05 was considered significant. The Statistical Package for the Social Sciences (SPSS) version 20 was used for data analysis.
Results
Genetics Knowledge of Medical Students: MCQs Test
The Genetics MCQs test and the self-survey questionnaire were completed by forty-one (41) second-year and thirty (30) fourth-year medical students. Table 2 summarizes the results of the genetics exam. In general, results revealed a lack of knowledge of genetics, with 43.85% of students correctly answering the exam. The correct responses in six important topics ranged from 29.2% to 63.1% among second-year students and 30.8% to 58.5% among fourth-year students. Both groups had low scores on the “Genetic Testing” test but slightly higher scores on the “Molecular and Cytogenetics” test.
Table 2.
MCQs Exam Results
| Topics Covered | % of Correct Answers | Mean | SD | t | P value | |
|---|---|---|---|---|---|---|
|
Molecular and Cytogenetics Nucleic acid structure and function; gene expression; Mutation; Numerical and structural chromosome aberrations; Karyotyping |
2nd Year | 63.1 | 41.06 | 4.88 | 1.97 | 0.012* |
| 4th Year | 58.5 | 38.10 | 4.11 | |||
|
Principles of Genetic Transmission Patterns of inheritance; autosomal dominant/recessive; sex-linked; atypical patterns (Mitochondrial; codominance, anticipation, etc.) |
2nd Year | 60.0 | 39.20 | 3.86 | 1.99 | 0.022* |
| 4th Year | 56.9 | 37.02 | 2.99 | |||
|
Inheritance of Genetic Diseases Common inherited diseases of the different body Systems: Down Syndrome; Muscular Dystrophy; Cystic Fibrosis; Arrhythmias; Cardiomyopathies |
2nd Year | 55.4 | 36.30 | 4.07 | 2.01 | 0.024* |
| 4th Year | 52.3 | 34.10 | 3.18 | |||
|
Cancer Genetics Breast Cancer, Ovarian cancer; Colorectal cancer; Esophageal cancer |
2nd Year | 47.7 | 31.23 | 2.52 | 1.98 | 0.022* |
| 4th Year | 50.8 | 33.15 | 2.17 | |||
|
Genetic Testing Types of Genetic tests and their uses |
2nd Year | 29.2 | 19.20 | 2.48 | 2.03 | 0.09 |
| 4th Year | 30.8 | 20.26 | 2.40 | |||
|
Genetic Counseling Pedigree analysis; recurrence risk assessment |
2nd Year | 35.4 | 23.16 | 1.92 | 2.07 | 0.13 |
| 4th Year | 36.9 | 24.25 | 3.15 |
Note: p = < 0.05 was considered significant. Number of MCQs=65. N= 41 second year and 30 fourth year students. *Indicates a significant P value.
Based on their MCQ test performance, second and fourth-year medical students were compared in their knowledge of several genetic topics. Table 2 shows that knowledge of molecular and cytogenetics, principles of genetic transmission, inheritance of hereditary illnesses, and cancer genetics differs significantly between second and fourth-year medical students. Second-year students significantly scored higher in the first three topics mentioned in the preceding sentence with P=0.012, 0.022, and 0.024, respectively. The fourth-year significantly (P=0.022) scored higher in the test items related to cancer genetics. No significant difference was observed between the two groups in genetic testing and genetic counseling topics.
The Genetics MCQs have a computed difficulty index ranging from 22.72 to 68.80%. The calculated values show that most of the questions are within the recommended difficulty index, with a few more difficult. Item difficulty is relevant for determining whether students have learned the concept being tested. Difficulty index (P), which ranges from 0 to 100%, describes the percentage of students who correctly answered the item. The higher the percentage means, the easier the question is. A difficulty index of 30 to 70% is recommended. Items having p-values less than 30% and above 70% are considered difficult and easy items, respectively.25
The discrimination index determines how well the question can tell the difference between high and low performers, which usually range from −1.0 to 1.0. It is the correlation of responses to individual items with the overall test score. The higher the correlation, the more the item results are consistent with the test as a whole. Determination index of 0–0.19 means Poor; 0.2–0.29 Acceptable; 0.3–0.39 Good; and more than 0.4 is Excellent. The calculated discrimination index (D) of the Genetics test ranges from 0.27 to 0.66, indicating that questions included in the test range from acceptable, good, and excellent.
Results show an internal consistency of 0.78 to 0.92. A measure of the internal consistency of the exam is expressed in statistics ranging from 0 (no reliability) to 1.0 (perfect reliability). It indicates the extent to which items on the test measure the same thing. The higher the value, the better the test is likely to produce consistent scores. High reliability means that the questions of a test tended to “pull together.” Students who answered a given question correctly were more likely to answer other questions correctly. Low reliability means that the questions tended to be unrelated to each other in terms of who answered them correctly. Box 1 shows the examples of the MCQs included in the test given to the second and fourth medical students.
Self-Assessment of Genetics Knowledge
Medical students were also asked if they believe their genetics knowledge is adequate for their future clinical practice. Figure 1 demonstrates that 87.8% of second-year medical students and 83.3% of fourth-year medical students believe their genetics knowledge is insufficient for their future clinical practice.
Figure 1.
Students’ perception of their genetics knowledge.
Discussion
This study assessed the second and fourth-year medical students’ genetic knowledge using a multiple-choice questions test and self-assessment survey questionnaire. The assessment results were utilized to identify gaps in students’ genetics knowledge and served as bases to revise and improve the genetics curriculum at the PNU College of Medicine’s MBBS program.
The study’s findings reveal insufficient genetics knowledge among second and fourth-year medical students. A slightly higher knowledge level of basic genetics concepts was noted when compared with clinically related genetics concepts. This finding could be attributed to a strong grasp of biochemical and genetic principles learned in high school and was reinforced in the Preparatory Year Program of the Health and Sciences at PNU, where various biochemical, genetic principles were studied in Biology and Biochemistry. Clinically oriented genetic topics, on the other hand, were not given priority. A thorough examination of the coverage of genetics in different blocks (Table 1) reveals that clinically-oriented genetic topics such as genetic testing and genetic counseling receive less than 20% of the total 29 hours of the complete genetics curriculum. The information about genetic testing was included in the lectures on various inherited diseases, but it was not highlighted. This outcome is consistent with what has been found in other studies.26,27 In a study on genetics knowledge and skills of medical students in Clinical Neurogenetics, it was reported that exam results showed a higher level of knowledge of genetic concepts learned in their basic science during pre-clinical years when compared with clinical Neurogenetics concepts.26 The students have a strong grasp of the fundamental concepts as well as the clinical presentation of the major genetic diseases, but they struggle to connect the clinical implications of the genetic abnormality.26 Similarly, results from cohort research conducted in Cameroon among medical students and physicians reveal a lack of knowledge about genetics, particularly concerning genetic testing.27 There has been little research on medical students’ genetics knowledge and skills, but multiple studies have been on physicians’ genetic literacy.8 Findings from these studies reveal a lack of genetics knowledge, making it unable to adequately respond to patients’ questions regarding medical genetics, genetic tests, and new developments in the field of genomic medicine.8,14,15,28,29 Thus, improving the undergraduate medical genomics curriculum should be addressed to improve physician genomic literacy. Undergraduate medical students must have a strong foundation in genetics and genomics to apply for genomic medicine across a range of specialties.9
Our findings also show that second-year MCQs test scores in molecular and cytogenetics, principles of genetic transmission, and inheritance of genetic illness are much higher than fourth-year MCQs exam scores. The fourth-year students, on the other hand, scored much higher in cancer genetics. These findings could indicate that fourth-year students have already forgotten basic genetics/medical genetic concepts learned two years back during their pre-clinical years. In our current genetics curriculum, genetics is not taught during the clinical years. Students’ better performance in cancer genetics could be attributed to their clinical exposure to varied cancer cases in various hospitals, which may have given them the opportunity to strengthen their understanding of this subject.
Similarly, a study examined whether third-year medical students retained specific knowledge and abilities taught during their first-year genetics course. The findings revealed that medical genetics knowledge and skills learned in the first year of medical school are not retained by third-year medical students. It was recommended that medical schools integrate the genetics curriculum throughout the four years of medical school.30 Another study on medical students nearing graduation revealed a deficient knowledge of genetics that is important to daily medical practice.31 Medical students lacked genetics knowledge to respond adequately to changes of relevance to genetics in medicine. Thus, changes in the basic medical curriculum should be considered.31 As a result, it is critical to incorporate clinical genetics into the clerkship years and emphasize teaching more genetic skills in the clinical curriculum.26
The Genetics curriculum has been changed at PNU since the commencement of the MBBS program in 2012 to enhance the students’ genetics knowledge. Initially, genetic concepts were taught in seven lectures over seven contact hours, but now, additional medical genetic concepts and skills are taught over 29 contact hours. Despite the improvements made to the curriculum, we recognize that we must continue to improve our genetics curriculum. Four (4) relevant aspects of our Medical Genetics Curriculum must be addressed as a result of the current study’s findings: 1) strengthening the curriculum content; 2) increasing the number of contact hours for lectures and skill development; 3) incorporating medical genetics throughout the four years of the medical curriculum, and 4) designing and implementing appropriate teaching and assessment strategies.
Inclusion of important topics not covered in our genetics curriculum, such as population genetics, contemporary topics like personalized medicine, direct-to-consumer testing, and ethical challenges surrounding clinical genetic and genomic testing, will help strengthen our existing genetics curriculum content. Also, essential subtopics should be added to some of the current topics. For example, in Genetic Counseling lectures, we only cover Pedigree Analysis and Recurrence Risk Assessment, and due to the limited contact hours, these topics are not addressed in depth. Ordering genetic tests, interpreting genetic test findings, and communicating with patients are all essential clinical sub-topics that should be introduced or integrated into the existing related lectures. It is worth noting that in strengthening the content of the genetics curriculum, it is recommended to look into the Core Curriculum for Medical School Genetics Education developed by APHMG.32 This proposed curriculum ensures that medical education reflects the current understanding of genetics/genomics and its impact on medical practice. Medical students should be provided with a thorough understanding of the genetics and genomics principles, starting from the basic science to clinical application.32 They should be taught the basic principles of genetics and genomic technologies and their application to various areas of medicine to prepare and train them to practice medicine in the age of genomics.18 The APHMG-recommended genetics core curriculum was built around the six competencies defined by the Accreditation Council for Graduate Medical Education (ACGME) and the American Board of Medical Specialties for residency training in the United States (ABMS). The six competencies include medical knowledge, patient care, interpersonal and communication skills, practice-based learning and improvement, professionalism, and systems-based practice, respectively.32 Table 3 shows the Core Curriculum for Medical School Genetics Education established by the APHMG parallel with the first and second competencies, Medical Knowledge and Patient Care.
Table 3.
Medical Genetics Curriculum Content Under Medical Knowledge and Patient Care (APHMG and ACGME)
| Genetics/Genomics Knowledge Under Medical Knowledge Competency | Genetics/Genomics Knowledge and Skills Under Patient Care Competency |
|---|---|
| Genetic variation Population genetics Inheritance Cytogenetics and molecular genetics Biochemical genetics Cancer genetics |
Medical genetics and inheritance Genetic testing Genetic counselling Cancer genetics Reproductive and pre-natal genetics Treatment and management of genetic disorders |
The additional number of contact hours for lectures to cover crucial medical genomics concepts and skills development is another aspect of our curriculum that needs to be addressed. This is challenging since our MBS curriculum is already overburdened with many topics to cover in order to meet the Intended Learning Outcomes (ILOs) of the MBBS program. One option for addressing this issue is to strengthen self-directed learning (SDL) in our curriculum to help students become more independent in their learning.
The integration of medical genetics across the medical curriculum, from pre-clinical, basic sciences to clinical years, is another part of our genetics curriculum that should be addressed. This would ensure that medical students maintain and improve their genetic knowledge throughout their clinical years, strengthening the application of medical genetics during clinical rotations. During the clinical years, case-based learning may also be used. This will connect basic science with clinical application and enhance information transfer, resulting in improved diagnostic abilities and long-term retention33,34
Furthermore, appropriate instructional strategies and assessments must be designed and implemented to meet the overburdened medical curriculum. Currently, we use the lecture method with self-directed learning (SDL) during the pre-clinical years, but we are gradually introducing problem-based learning (PBL) as part of our genetics instruction. In fact, in the Reproduction Block, we have already begun integrating PBL cases on numerical and structural chromosomal abnormalities. It is possible to implement non-lecture-based teaching methodologies that emphasize the application of genetic and genomics principles to clinical care. Team-based learning (TBL), problem-based learning (PBL), case-based learning (CBL), flipped class activities, and patient simulation are examples of strategies that demonstrate a shift toward learner-centered, competency-based education with an emphasis on active learning.35,36 Active learning, as opposed to traditional lectures, focuses on the application of knowledge and has been found to increase student involvement and possibly performance.37,38 It is also important to note the use of standardized patient (SPs) to enable medical students to improve their skills in assessing genetic risks and communicating genetic information to patients. According to another study, the effective use of SPs in medical genetics instruction may improve medical students’ self-confidence in their clinical genetics skills.39
The findings of our study pose a challenge on how to incorporate the breadth of knowledge and skills required to achieve the competencies outlined by APHMG and ACGME during this time of genomic and precision medicine. However, these do not provide us with specific information about the demands and challenges that our medical students have when it comes to the content and implementation of our genetics curriculum. As a result, there is an ongoing effort to collect feedback from our medical students and genetics educators on the difficulties they have faced to address these issues. Furthermore, there is a current endeavor in developing and implementing genomics content through active learning strategies that emphasize clinical application across pre-clinical and clinical years of our undergraduate medical curriculum.
We also look forward to having linkage and update with the researches related to genomic medicine and different genetic services within the kingdom like the Saudi Human Genome Program (SHGP) which is the largest genome initiative in the Middle East. The SHGP aims to reduce and prevent genetic diseases.
Conclusion
Medical students’ genetics knowledge is insufficient, particularly in clinically relevant concepts such as genetic testing and genetic counseling, and should be reinforced in preparation for future clinical practice. Fourth-year medical students do not retain genetics knowledge.
Integrating medical genetics into clinical years is critical for retaining and strengthening medical students’ knowledge of genetics. ASHG and APHMG have stated that every physician must have an in-depth knowledge of genetic principles and their application to a wide range of clinical conditions.
Acknowledgments
The authors would like to express their gratitude to all medical students who participated in this study.
Funding Statement
Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2022R147), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia.
Ethical Approval
This study was approved by Princess Nourah Bint Abdulrahman University Internal Review Board. Participants were informed about the nature and objectives of the research. Their voluntary consent to participate was obtained prior to the conduct of the study. Participants were also informed that whatever data and information gathered will be kept safe and confidential and destroyed upon the publication of the research.
Author Contributions
Both authors contributed to data analysis, drafting, or revising the article, have agreed on the journal to which the article was submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Singh RS, Gupta BP. Genes and genomes and unnecessary complexity in precision medicine. NPJ Genom Med. 2020;5(1):21. doi: 10.1038/s41525-020-0128-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turnpenny P, Ellard S. Emery’s Elements of Medical Genetics. 15th ed. Churchill Livingstone: Elsevier; 2017. [Google Scholar]
- 3.Shendure J, Findlay GM, Snyder MW. Genomic medicine-progress, pitfalls, and promise. Cell. 2019;177(1):45–57. doi: 10.1016/j.cell.2019.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roth SC. What is genomic medicine? J Med Libr Assoc. 2019;107(3):442–448. doi: 10.5195/jmla.2019.604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hasanzad M, Sarhangi N, Naghavi A, et al. Genomic medicine on the frontier of precision medicine. J Diabetes Metab Disord. 2021. doi: 10.1007/s40200-021-00880-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caskey T. Precision medicine: functional advancements. Annu Rev Med. 2018;69:1–18. PMID: 29261360. doi: 10.1146/annurev-med-041316-090905 [DOI] [PubMed] [Google Scholar]
- 7.Jin P. Medical genetics: towards precision medicine. J Genet Genomics. 2018;45(2):55–56. doi: 10.1016/j.jgg.2018.02.005 [DOI] [PubMed] [Google Scholar]
- 8.Rubanovich CK, Cheung C, Mandel J, Bloss CS. Physician preparedness for big genomic data: a review of genomic medicine education initiatives in the United States. Hum Mol Genet. 2018;27(R2):R250–R258. PMID: 29750248; PMCID: PMC6061688. doi: 10.1093/hmg/ddy170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hyland K, Garber K, Dasgupta S. From helices to health: undergraduate medical education in genetics and genomics. Per Med. 2019;16(3):211–220. doi: 10.2217/pme-2018-0081 [DOI] [PubMed] [Google Scholar]
- 10.McGuire AL, Gabriel S, Tishkoff SA, et al. The road ahead in genetics and genomics. Nat Rev Genet. 2020;21(10):581–596. doi: 10.1038/s41576-020-0272-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Phillips KA, Deverka PA, Hooker GW, Douglas MP. Genetic test availability and spending: where are we now? Where are we going? Health Aff. 2018;37(5):710–716. doi: 10.1377/hlthaff.2017.1427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Campion M, Goldgar C, Hopkin RJ, Prows CA, Dasgupta S. Genomic education for the next generation of health-care providers. Genet Med. 2019;21(11):2422–2430. doi: 10.1038/s41436-019-0548-4 [DOI] [PubMed] [Google Scholar]
- 13.McGrath S, Ghersi D. Building towards precision medicine: empowering medical professionals for the next revolution. BMC Med Genomics. 2016;9(1):23. doi: 10.1186/s12920-016-0183-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feero WG. Introducing “Genomics and Precision Health”. JAMA. 2017;317(18):1842–1843. doi: 10.1001/jama.2016.20625 [DOI] [PubMed] [Google Scholar]
- 15.Hamilton JG, Abdiwahab E, Edwards HM, et al. Primary care providers’ cancer genetic testing-related knowledge, attitudes, and communication behaviors: a systematic review and re- search agenda. J Gen Intern Med. 2017;32(3):315–324. doi: 10.1007/s11606-016-3943-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jenkins BD, Fischer CG, Polito CA, et al. The 2019 US medical genetics workforce: a focus on clinical genetics. Genet Med. 2021;23(8):1458–1464. doi: 10.1038/s41436-021-01162-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eden C, Johnson KW, Gottesman O, Bottinger EP, Abul-Husn NS. Medical student preparedness for an era of personalized medicine: findings from one US medical school. Pers Med. 2016;13(2):129–141. doi: 10.2217/pme.15.58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Plunkett-Rondeau J, Hyland K, Dasgupta S. Training future physicians in the era of genomic medicine: trends in undergraduate medical genetics education. Genet Med. 2015;17(11):927–934. doi: 10.1038/gim.2014.208 [DOI] [PubMed] [Google Scholar]
- 19.Hyland K, Dasgupta S, Garber K, et al. Medical school core curriculum in genetics. Association of Professors of Human and Medical Genetics; 2013. Available from: http://media.wix.com/ugd/3a7b87_7064376a9eb346cfa1b85bc2f137c48f.pdf. Accessed December 13, 2021. [Google Scholar]
- 20.Alkuraya FS. Genetics and genomic medicine in Saudi Arabia. Mol Genet Genomic Med. 2014;2(5):369–378. PubMed PMID: 25333061; PubMedCentral PMCID: PMC4190871. doi: 10.1002/mgg3.97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Aam J, Alhashem A. Genetic disorder in the arab world: an overview of medical genetic services in Saudi Arabia; 2018. Available from: https://cags.org.ae/contentfiles/uploads/files/chapter%203.pdf. Accessed December 13, 2021.
- 22.Al-Owain M, Al-Zaidan H, Al-Hassan Z. Map of autosomal recessive genetic disorders in Saudi Arabia: concepts and future directions. Am J Med Genet. 2012;158A(10):2629–2640. doi: 10.1002/ajmg.a.35551 [DOI] [PubMed] [Google Scholar]
- 23.Qari AA, Balobaid AS, Rawashdeh RR, Al-Sayed MD. The development of genetic counseling services and training program in Saudi Arabia. J Genet Couns. 2013;22(6):835–838. PMID: 24037027. doi: 10.1007/s10897-013-9645-8 [DOI] [PubMed] [Google Scholar]
- 24.Cordero M, Abdur Rashid N, El Hasnaoui R, Ganesh K, Khired Z. Tutors and self-assessment of medical students’ performance in pre-clinical problem-based learning tutorial sessions. MedEdPublish. 2018;7(4):44. doi: 10.15694/mep.2018.0000265.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller MD, Linn RL, Gronlund NE, editors. Measurement and Assessment in Teaching. 10th ed. Upper Saddle River, NJ: Prentice-Hall; 2009. [Google Scholar]
- 26.Pearl PL, Pettiford JM, Combs SE, et al. Assessment of genetics knowledge and skills in medical students: insight for a clinical neurogenetics curriculum. Biochem Mol Biol Educ. 2011;39(3):191–195. PMID: 21618382. doi: 10.1002/bmb.20489 [DOI] [PubMed] [Google Scholar]
- 27.Wonka A, Njamnshi A, Angwafo F. Knowledge and attitudes concerning medical genetics amongst physicians and medical students in Cameroon (sub-Saharan Africa). Genet Med. 2006;8(6):331–338. doi: 10.1097/01.gim.0000223542.97262.21 [DOI] [PubMed] [Google Scholar]
- 28.Baars MJ, Henneman L, Ten Kate LP, et al. Deficiency of knowledge of genetics and genetic tests among general practitioners, gynecologists, and pediatricians: a global problem. Genet Med. 2005;7(9):605–610. doi: 10.1097/01.gim.0000182895.28432.c7 [DOI] [PubMed] [Google Scholar]
- 29.Čargonja P, Mavrinac M, Ostojić S, et al. The impact of needs-based education on the change of knowledge and attitudes towards medical genetics in medical students. Eur J Hum Genet. 2021;29(5):726–735. doi: 10.1038/s41431-020-00791-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Greb A, Brennan S, McFarlane L, et al. Retention of medical genetics knowledge and skills by medical students. Genet Med. 2009;11(5):365–370. doi: 10.1097/GIM.0b013e31819c6b2d [DOI] [PubMed] [Google Scholar]
- 31.Baars MJ, Scherpbier AJ, Schuwirth LW, et al. Deficient knowledge of genetics relevant for daily practice among medical students nearing graduation. Genet Med. 2005;7(5):295–301. PMID:15915080. doi: 10.1097/01.gim.0000162877.87333.9 [DOI] [PubMed] [Google Scholar]
- 32.Hyland K, Dasgupta S, Garber K, et al. Medical school core curriculum in genetics. Association of Professors of Human and Medical Genetics. Available from: http://media.wix.com/ugd/3a7b87_7064376a9eb346cfa1b85bc2f137c48f.pdf. Accessed December 13, 2021. [Google Scholar]
- 33.Woods NN. Science is fundamental: the role of biomedical knowledge in clinical reasoning. Med Educ. 2007;41(12):1173–1177. PMID: 18045369. doi: 10.1111/j.1365-2923.2007.02911.x [DOI] [PubMed] [Google Scholar]
- 34.Lisk K, Agur AM, Woods NN. Exploring cognitive integration of basic science and its effect on diagnostic reasoning in novices. Perspect Med Educ. 2016;5(3):147–153. PMID: 27246965; PMCID: PMC4908035. doi: 10.1007/s40037-016-0268-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Prober CG, Heath C. Lecture halls without lectures–a proposal for medical education. N Engl J Med. 2012;366(18):1657–1659. PMID: 22551125. doi: 10.1056/NEJMp1202451 [DOI] [PubMed] [Google Scholar]
- 36.Hagiwara N. Application of active learning modalities to achieve medical genetics competencies and their learning outcome assessments. Adv Med Educ Pract. 2017;8:817–829. PMID: 29276425; PMCID: PMC5733911. doi: 10.2147/AMEP.S145696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen F, Lui AM, Martinelli SM. A systematic review of the effectiveness of flipped classrooms in medical education. Med Educ. 2017;51(6):585–597. PMID: 28488303. doi: 10.1111/medu.13272 [DOI] [PubMed] [Google Scholar]
- 38.Reimschisel T, Herring AL, Huang J, Minor TJ. A systematic review of the published literature on team-based learning in health professions education. Med Teach. 2017;39(12):1227–1237. PMID: 28664760. doi: 10.1080/0142159X.2017.1340636 [DOI] [PubMed] [Google Scholar]
- 39.McGovern MM, Johnston M, Brown K, Zinberg R, Cohen D. Use of standardized patients in, undergraduate medical genetics education. Teach Learn Med. 2006;18(3):203–207. doi: 10.1207/s15328015tlm1803_3 [DOI] [PubMed] [Google Scholar]