Abstract
Objective
Six per cent of hospital patients experience a patient safety incident, of which 12% result in severe/fatal outcomes. Acutely sick patients are at heightened risk. Our aim was to identify the most frequently reported incidents in acute medical units and their characteristics.
Design
Retrospective mixed methods methodology: (1) an a priori coding process, applying a multi-axial coding framework to incident reports; and, (2) a thematic interpretative analysis of reports.
Setting
Patient safety incident reports (10 years, 2005–2015) collected from the National Reporting and Learning System, which receives reports from hospitals and other care settings across England and Wales.
Participants
Reports describing severe harm/death in acute medical unit were identified.
Main outcome measures
Incident type, contributory factors, outcomes and level of harm were identified in the included reports. During thematic analysis, themes and metathemes were synthesised to inform priorities for quality improvement.
Results
A total of 377 reports of severe harm or death were confirmed. The most common incident types were diagnostic errors (n = 79), medication-related errors (n = 61), and failures monitoring patients (n = 57). Incidents commonly stemmed from lack of active decision-making during patient admissions and communication failures between teams. Patients were at heightened risk of unsafe care during handovers and transfers of care. Metathemes included the necessity of patient self-advocacy and a lack of care coordination.
Conclusion
This 10-year national analysis of incident reports provides recommendations to improve patient safety including: introduction of electronic prescribing and monitoring systems; forcing checklists to reduce diagnostic errors; and increased senior presence overnight and at weekends.
Keywords: Clinical, emergency medicine, health service research, medical error/patient safety, medical management, other emergency medicine, other statistics and research methods, quality improvement
Introduction
Patient safety incidents occur in 6% of patient cases acutely admitted to hospital, with 12% resulting in severe or fatal outcomes. 1 In 2004, the Royal College of Physicians advocated acute medical units to relieve pressures on emergency departments 2 and improve patient outcomes. 3 Ten years later, a single Irish hospital study has reported decreased mortality since the introduction of an acute medical unit (a 60% reduction in relative risk for individual patients). 4 It is still the case that, despite major redesign of care delivery, little is known about patient safety incidents occurring in acute medical units.
Handovers and care transfers, diagnostic cognitive overload and staffing levels may be important factors. 5 For example, a UK team conducted a single site observational study (four one-week periods over 18 months involving 36 staff and 71 patients) identifying delays in 44% of admissions. 6 An observational and interview study from the same team demonstrated 46% (318/688) of medication charts contained errors, the majority of which involved omission of medication. This study highlighted variances in medication history-taking including a lack of collaborative histories before prescribing. 7 These data correlate with the findings of a 2008 narrative review of Australian medication incidents that described multifactorial underlying causes of errors with a paucity of evidence-based solutions.8,9 Another Australian study, examining routine reporting of handover related incidents in acute care, found omission of critical information in one-third of incidents (153/459). 10
The existing evidence base for improvement in safety and quality in acute medical units (aside from studies about the management of specific diseases) is also fragmented and neither extensive nor strong. A systematically conducted narrative review (published 2018) only identified nine studies in the UK or Ireland. These suggested potential benefit from increased pharmacy services, occupational therapy and medical consultant input plus enhanced handovers. 11 Further to this, identifiable evidence includes a multivariate analysis using survey data from England which showed statistically significant reductions in adjusted case fatality rates and readmission rates when consultants were present for at least four hours per day. 12 A smaller Italian study, also using routine data compared nursing staff levels with in-hospital mortality in 2017, drew similar conclusions: more experienced staff presence is safer for patients. 13 More recently, interest in use of electronic systems to reduce errors has grown, including a Danish observational study showing a resulting reduction in medication administration errors. 14 Further small studies suggest electronic handovers and the use of checklists are perceived as useful instruments by doctors.15,16 Evidence of clinical impact from these interventions is still required.
Large datasets from incident reporting systems, such as the National Reporting and Learning System in England and Wales, can enable learning from patient safety incidents through identification of underlying contributing factors. Contributory factors can be both active errors, such as staff mistakes, and latent conditions in the working environment or system, for example staff shortages. Analysis can provide an evidence base for targeting interventions at ‘real life’ challenges to prevent recurrence.
Aims
To understand the most frequent patient safety incidents resulting in severe harm or death, and their characteristics, from acute medical units in England and Wales.
Objectives
Describe the characteristics of incidents, including type, contributory factors and harm outcomes.
Interpret contributory factors in relation to incident types.
Identify incident themes and metathemes to inform priorities for improvement.
Methods
National reporting and learning system
The National Reporting and Learning System receives incident reports from staff in NHS organisations across England and Wales. Each report has a structured section (incident type, harm severity, location, specialty and medication involved), and an unstructured free-text section (detailing what happened and any preceding events). 17
Sample formation
All incidents reported from the acute medical unit (including related synonyms) from 5 April 2005 to 21 December 2015.
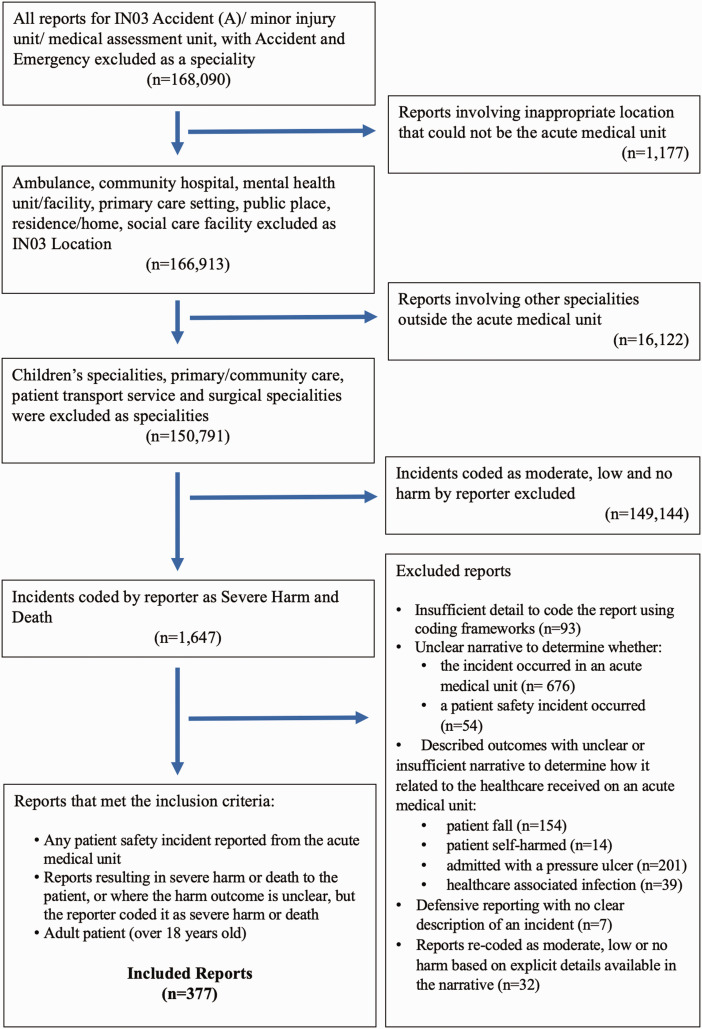
All National Reporting and Learning System reports with the (IN03) category ‘location Accident (A)/Minor Injury Unit/Medical Assessment Unit’ were extracted (n = 168,090), subsequent exclusions are given in Figure 1.
Figure 1.
Flow chart showing the number of reports and how the data sample was selected. AMU: acute medical unit.
Initial data cleaning (Figure 1) of 150,791 reports identified that 1647 had severe harm or death outcomes. These were read in full by one researcher to confirm eligibility against pre-set inclusion/exclusion criteria complied by the research team. A second researcher reviewed reports flagged as problematic to match to the pre-set criteria and 177 randomly selected reports for inclusion/exclusion. Borderline reports (n = 28) were included/excluded if both researchers reached consensus after discussion or after discussing with a third member of the research team. During this process, reports were classified with a primary incident code (i.e. code used to describe the incident which occurred directly prior to the patient experiencing a harmful outcome or the code to exclude a report).
Methodology
The study was informed by a constructionist approach accepting that our understanding of incidents is contingent on the human practices and interactions occurring within the context that each incident occurred and our own judgements as clinical researchers. We first conducted a descriptive analysis using an a priori coding framework drawn from the multi-axial classification system developed by the Patient Safety (PISA) group at Cardiff University (the application of which is informed by nine rules from the recursive model of incident analysis developed by the Australian Patient Safety Foundation). 17 Following this, we conducted an interpretative thematic analysis. 18 The use of a pre-existing framework alongside interpretative analysis provided us with checks and balances between theory and empirical data and between members of the research team. 19
A priori coding and descriptive analysis
Each incident report was configured into a sequence of events resulting in the outcome (including severity) and identifying contributory incidents and factors. Codes from the PISA framework were applied to represent the incident type, contributory factors, outcome and harm severity. The PISA framework codes the severity based on the WHO International Classification for Patient Safety definitions (Table 1). The classification with primary incident codes by one researcher was independently duplicated by a second research on a random sample (n = 149). Following this, a Cohen's kappa for interrater reliability was calculated for the primary incident coding to be 0.73 (p < 0.05). All discrepancies were discussed with a third person arbitrator (ACS).
Table 1.
The primary incident types from the included reports and the harm outcomes from the a priori coding using the PISA classification.
| Incident type | Severe harm | Death | Unclear (severe harm or death) | Total |
|---|---|---|---|---|
| Treatment or procedure | 23 | 43 | 41 | 107 |
| Insufficient treatment/care/monitoring | 13 | 28 | 16 | 57 |
| Treatment not given in a timely fashion | 4 | 7 | 9 | 20 |
| Error in conducting procedure | 3 | 1 | 3 | 7 |
| Complication | 1 | 5 | 6 | |
| No treatment/care give | 2 | 4 | 6 | 12 |
| Other | 1 | 2 | 2 | 5 |
| Diagnosis and assessment | 32 | 35 | 38 | 105 |
| Diagnostic error | 30 | 25 | 24 | 79 |
| Insufficient assessment of patient | 2 | 4 | 7 | 13 |
| Errors in discharge, including premature discharge | 3 | 3 | 6 | |
| Delayed assessment | 3 | 4 | 7 | |
| Medication | 19 | 14 | 28 | 61 |
| Clinical treatment decision | 6 | 5 | 10 | 21 |
| Prescribing | 6 | 3 | 2 | 11 |
| Drug omission | 1 | 7 | 8 | |
| Administration | 1 | 1 | 5 | 7 |
| Timeliness of medication | 3 | 2 | 2 | 7 |
| Other (dispensing, adverse events, overdose) | 3 | 2 | 2 | 7 |
| Referral | 9 | 10 | 25 | 44 |
| Staff errors during referral of a patient | 4 | 7 | 14 | 25 |
| Errors in transfer (wrong location or transfer delayed) | 4 | 3 | 10 | 17 |
| Other | 1 | 1 | 2 | |
| Investigation | 4 | 9 | 13 | 26 |
| Laboratory tests and results | 3 | 6 | 3 | 12 |
| Imaging investigations | 1 | 2 | 10 | 13 |
| Other investigations | 1 | 1 | ||
| Equipment | 1 | 2 | 15 | 18 |
| Failure of equipment | 6 | 6 | ||
| Insufficient supply of equipment | 1 | 6 | 7 | |
| Other | 1 | 1 | 3 | 5 |
| Administration | 1 | 5 | 6 | |
| Communication | 2 | 2 | 3 | 7 |
| Other | 1 | 2 | 3 |
The harm severity of reports was coded according to the harm severity levels from the WHO International Classification for Patient safety: 20 • No harm: Patient has no symptoms and no further treatment is necessary • Low harm: Mild symptoms experienced that are short term. None or little treatment is necessary. • Moderate harm: Patient experiences symptoms, further interventions or a longer admission are needed, and the resulting harm or loss of function is either permanent or long standing • Severe harm: Major or life-saving treatment/intervention is required which leads to a reduced life expectancy or permanent or long-term serious loss of function or harm • Death: The incident caused the death of the patient
The results of applying the PISA classification codes were used as quantitative categorical variables to explore inter-code relationships. Frequency charts, line graphs and cross tabulations were created (using Microsoft Excel version 2016, Microsoft Corporation). These were used to examine associations between codes, including relationships between the most common contributory factors, incident types, outcomes and harm severity, for example the incident type ‘medication errors’ and contributory factor ‘staff mistakes'. The inter-code relationships between type and outcome are shown in Table 1. Contributory factors by incident type are shown in Table 2. Purposive sampling of reports supporting emerging hypotheses, including the most common or harmful relationships between incidents and contributory factors or outcomes, from the quantitative analysis were then analysed using thematic analysis.
Table 2.
Contributory factors by incident type (see supplemental Appendix 1 for a more detailed breakdown).
| Incident type | Contributory factors |
|||
|---|---|---|---|---|
| Patient factors | Staff factors | Equipment/ medication | Transfer of care/handovers | |
| Referrals and transfers of patients | 2 | 6 | 1 | 23 |
| Diagnostic error | 8 | 19 | 0 | 15 |
| Errors in assessment | 1 | 2 | 0 | 9 |
| Treatment errors | 5 | 20 | 5 | 39 |
| Medication errors | 5 | 17 | 1 | 10 |
| Investigation/imaging errors | 1 | 4 | 0 | 8 |
| Communication errors | 1 | 1 | 0 | 3 |
| Equipment incidents | 1 | 1 | 4 | 1 |
| Administration errors | 0 | 0 | 0 | 3 |
Interpretative thematic analysis
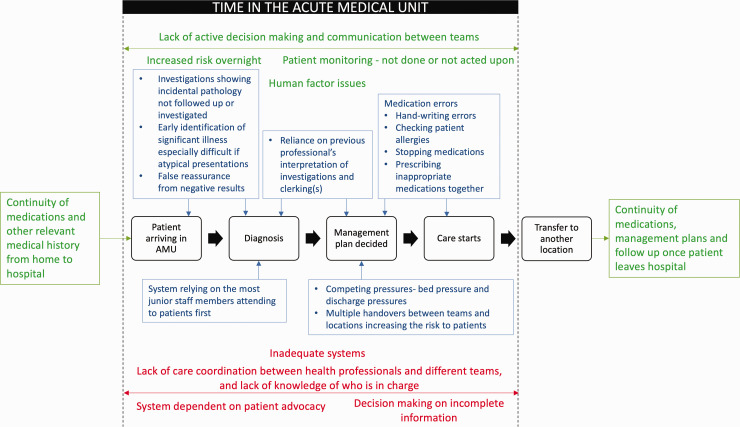
Taking an in vivo approach to the same dataset, the free-text data were analysed using qualitative interpretative codes, and themes and metathemes were sought to understand the context, sequence of events and human interactions leading to incidents. ‘Metathemes’ is a term describing themes that are overarching and cross-cutting (i.e. intersecting with each other) in the data. A member of the research team (who had not conducted the a priori coding) reviewed the data for tentative interpretative codes independently to the rest of the team. Reports were then collectively re-read and group analysis by the whole team undertaken to identify our final interpretative codes. These were collated into themes. Themes and codes were then mapped onto a theoretical process map (Figure 2) of the movement of a patient through the acute medical unit, from which the metathemes were developed.
Figure 2.
Process map of the complexities, and interacting elements of a patient journey through the acute medical unit, showing the qualitative codes in blue, the themes in green and the overarching metathemes in red. Themes and metathemes are shown to overlap as ‘Metathemes’ is a term describing themes that are overarching and cross-cutting (i.e. intersecting with each other) in the data. For example, ‘Lack of active decision making and communication between teams’ is a specific theme which interacts with (i.e. both results from and exacerbates). ‘Lack of care coordination between health professionals and different teams, lack of knowledge of who is in charge’, while the latter is also resulting from and exacerbated by other themes such as patient monitoring = not done or acted on, and indeed codes such as reliance on the most junior members of staff attending to patients first.
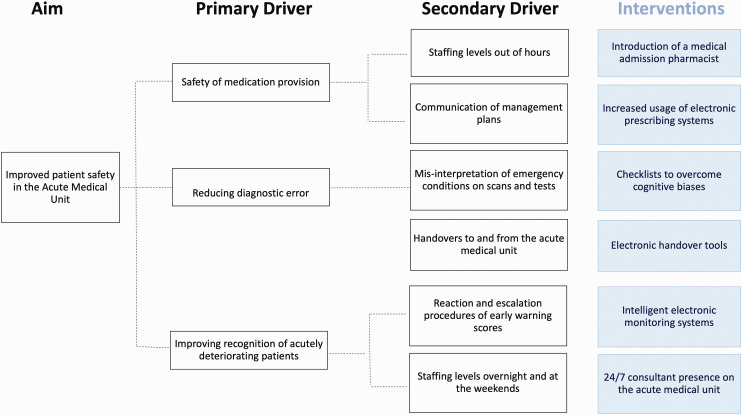
Synthesis of mixed methods analysis
The multiple analytic techniques were synthesised collectively to interpret findings, from both descriptive and interpretative analyses, and identify priority areas for interventions to reduce healthcare associated harm. These were then mapped onto a driver diagram, linked to pre-existing evidence for interventions to target these areas. Together, Figures 2 and 3 provide a summary of the theory of change generated through this study.
Figure 3.
Driver diagram showing the key areas causing iatrogenic harm to patients in the acute medical unit and potential interventions to target these areas.12,15,16,21–23 These exemplar interventions were identified in scoping searches of pre-existing literature.
Results
A total of 377 confirmed reports of severe harm or death were included in our final analyses following application of the PISA framework to identify the primary incident (Figure 1 for final inclusion and exclusion criteria). Due to the anonymisation of data, it was not possible to be certain how many unique patients this equated to. The most common incidents were: diagnostic error (n = 79), medication error (n = 61) and monitoring errors (n = 57) (Table 1). A total of 216 reports (57%) contained one or more identifiable contributory factors: most commonly failure to follow protocols (n = 30) and staff mistakes (n = 23).
Using the PISA framework, 116 reports described a patient death, 91 described other severe harm. The PISA harm level was unclear for 170 reports, because no outcome was described by the reporter or the report had insufficient detail to reach an unequivocal conclusion. Such reports were included when the research team, judged drawing on their own clinical expertise that severe harm or death was likely given the raw data that was provided. Using the PISA framework, of the reports with a pre-assigned National Reporting and Learning System code of severe harm 189 reports (72%) were reclassified according to the WHO harm severities and 55 of the death reports (38%) were reclassified (Table 1). Of the included reports (n = 377), outcomes were explicit in 259 reports (69%), the most common outcome was death (n = 116, 31%), followed by delays in management (n = 37, 10%).
Patient trajectory
A common theme with patient trajectory was lack of active decision-making and communication between teams (Figure 2). Errors occurred due to a lack of clarity regarding responsibilities for patient care co-ordination, especially during emergency situations or out-of-hours. Poor documentation of long-term management plans and no reliable review system to ensure follow-up by the most appropriate teams contributed.
Patient monitoring errors (n = 57) occurred throughout acute medical units from arrival to discharge. Over half of reports involving errors in monitoring resulted in death of patients (n = 30). One-third of these incidents occurred overnight (n = 11), see example 10 (Table 3). Lack of continuity of care between different locations in the hospital was described in 36 reports, commonly overnight (n = 24), see example 8 (Table 3). Errors in continuity of care included lack of necessary treatment, failure to follow management plans, results not acted on appropriately, and observations not done or acted upon when informing early warning scores, see example 10. Communication errors occurred during handovers between teams or transfer of patients between locations in the hospital (n = 9). These resulted in patients not receiving the necessary treatment (n = 12), see example 11, specialist care they require (n = 5) or senior review (n = 3), see example 9.
Table 3.
Examples of the acute medical unit severe harm and death reports from the National Reporting and Learning System.
| Example 1 |
| Missed diagnosis of MI – ECG had ST elevation, delay to thrombolysis. |
| Example 2 |
| MEAU. Patient admitted with a headache of sudden onset. CT was reported as normal when subtle blood was visible. [Lumbar puncture] not done by medical team. Patient discharged but readmitted with massive subarachnoid haemorrhage and died. |
| Example 3 |
| GP referral with central chest pain, radiating to left arm, troponin test was elevated, seen by on call physician and sent home, continued to have chest pain readmitted to CCU with substantial further rise in troponin and widespread ECG changes |
| Example 4 |
| Patient was prescribed ACS treatment as? NSTEMI positive trop T. The aspirin 300 mg, clopidogrel 300 mg and fondaparinux 2.5 mg were not signed for on Cerner or on any paper chart which points to a missed dose. |
| Example 5 |
| Admitted generally unwell. Referred in with a raised INR (8.8), repeat INR 8.3. Delay in recognition of elevated INR (missed in clerking and post take ward round). Identified on evening [night round]. Vit K prescribed but not given. |
| Example 6 |
| Patient prescribed IV Augmentin. First dose given at 03:10 approx. Patient later arrested and died. As patient appeared to be fitting, I checked the drug chart for Diazemuls to realise she was penicillin allergic. An arrest call was put out and doctors informed of allergy. Patient immediately given IV [adrenaline] and hydrocortisone 200 mg IV. CPR was not successful, and patient died. |
| Example 7 |
| Patient referred by GP with a diagnosis of acute renal failure and urinary sepsis, arrived at hospital 16:30, initial bloods showed [creatinine] 812 and [potassium] 7.8, [arterial blood gas] showed lactate 8.1. Unclear to what extent this was recognised and treated over the 9 h from admission – the drug chart did not show any treatments running – patient remained anuric and became increasingly hypotensive then had a cardiac arrest at 01:30. Transiently resuscitated with adrenaline but then re-arrested and died. |
| Example 8 |
| [Patient] presented 16:30 with urosepsis (septic shock). Treated with fluids and IV antibiotics, but failed to maintain parameters (HR, BPP, HR, SATS). No further entry in the notes after clerking. No handover to night SpR. Nurse on shift no handover from colleague for further medical involvement. Called to see patient peri-arrest. Failed to resuscitate after 1 h and 1 return of circulation midway. Stopped due to multiorgan failure, aspiration, futility and failure to re-establish output. |
| Example 9 |
| Patient admitted on [date] with sepsis. She was referred to outreach due to deteriorating observations. It was found later that the patient had MRSA but she could not be transferred to side room for barrier nursing due to needing high dependency care. She later needed to be transferred to ITU but no beds available and the [patient’s] condition continued to deteriorate. She died [three days later] with neither transfer to ITU taking place and or a decision being made to withdraw care. There were no hourly observations carried out prior to death. |
| Example 10 |
| Patient admitted on [date 1] at 13:00 to A&E with fall. Cardiac [observations] recorded at 13:10, [track and trigger] score of 2 next set in A&E at 16:05 [track and trigger] score of 2. [Patient] transferred to CDU; seen by medical team at 18:30 no observations recorded on admission to CDU. [Patient] suffered cardiac arrest at 06:48 a.m. on the [next day]. No observations recorded from 16:05 on [date 1] until post arrest the [next morning]. Patient [died] (on end of life care) on [3 days later]. |
| Example 11 |
| [Patient] transferred from A&E at 15:45 h, staff nurse from A&E given handover about [patient] to [specialist nurse]. The [specialist nurse] was told that [patient] had been admitted with right-sided weakness and headache, nurse was not informed that [patient] had chest pain or that an ECG taken whilst [patient] in A&E indicated that [patient] experienced anterior myocardial infarction. [Patient] experienced a respiratory arrest whilst being seen by [doctor]. |
Note: Exemplar quotes have been pseudoanonymised and spelling corrected for clarification purposes. In some cases, this required removal of data elements (e.g. a rare condition). Edits are indicated in square brackets with […] indicating the need to remove identifiable data.
Arrival in an acute medical unit to diagnosis
Common errors that occurred immediately after patients arrived in an acute medical unit included problems identifying significant illnesses early, especially if presentations were atypical. Errors involved ‘routine’ investigations that are commonly requested for all patients, the results of which were often not acted upon or false reassurance was gained from negative results when the most appropriate investigation may not have been requested. Diagnostic error was the most common incident type occurring in the reports (n = 79). Delayed diagnosis was the most common (n = 36) diagnostic error, and cancer was the most commonly missed diagnosis (n = 11). Diagnostic errors resulted in death (n = 24) and delays in management (n = 20). Staff mistakes were frequently identified as having led up to diagnostic errors (n = 15), and these were most often mistakes interpreting investigations, including ECGs and imaging tests (n = 9), see examples 1 and 2 (Table 3). The most common diagnosis associated with delays in management was myocardial infarction (n = 4), often due to misinterpretation of ECGs, see examples 1 and 3.
Our analysis shows the system relies on the most junior doctors and staff members seeing patients first. A lack of experience led to problems recognising acutely unwell patients, selecting appropriate proformas to use or accessing senior help.
Management and commencement of care
Between diagnosis and initiation of a management plan, errors occurred due to reliance on earlier professionals’ interpretation of investigations or patient histories and examinations. Errors were perpetuated through this mechanism. Patients were at a higher risk of patient safety incidents when there were multiple handovers between teams, transfers between wards and the out-of-hours settings including during the night (Figure 2).
Medication errors were the second most common incident occurring, representing 16% (n = 61) of severe harm and death reports. The commonest contributory factors were failure to follow protocol (n = 8) and staff mistakes (n = 6). Staff mistakes arose from failures in continuity of care provided to patients. This discontinuity of care included errors responding to test results (n = 4), such as failure to act on a raised INR, and prescribed medications being omitted (n = 4), or deteriorating vital signs, see examples 4, 5 and 7 (Table 3). Within the medication error reports, the main theme was human factors issues, including errors with handwriting or allergies not being checked or documented appropriately. One-fifth of the medication errors resulted in patient death (n = 13); these commonly occurred overnight (n = 6). The most common medication type associated with death following a medication error was antibiotics (n = 5), see example 6.
Transfer
Errors commonly occurred when the care of patients was being transferred from an acute medical unit to the community or another specialty. Errors in continuity of medication, care plans and follow-up for patients after discharge were common themes. Patient care was often delayed due to a lack of available beds, delaying access to specialist care.
Metathemes
The strongest metatheme throughout reports was:
The system largely depending on patient advocacy, and patients who were unable to self-advocate were often overlooked due to system pressures. Self-advocacy was necessary due to a lack of care coordination during the patient journey, resulting in patients having to remind staff about investigations or referrals.
Further metathemes were:
Lack of care coordination, which was prominent in reports involving patients with terminal illness or who were very frail, when there was a lack of appreciation for the final aim of treatment, where interventions were leading, or the reversibility of conditions. This was often due to only the subsequent step of the management plan being communicated, rather than the overall aims of management.
Decision-making using incomplete information leading to errors, which, similar to a lack of care coordination, meant that the decisions made were not always the most appropriate for the patient (Figure 2).
Driver diagram
Priority areas and existing evidence (from scoping pre-existing published literature) for targeted interventions, that could be implanted in acute medical units or on a wider system level, were mapped onto a driver diagram (Figure 3).
Discussion
Principal findings
This is the first analysis of all the severe harm and death incident reports occurring in acute medical units across England and Wales. The depth of qualitative analysis is novel for work of this nature as is the identification of overarching and cross-cutting metathemes that intersect across a given patient’s journey through the acute medical unit. Our work adds value methodologically as well as pinpointing to practitioners where and how they could improve their own systems through quality improvement.
Our study confirms that diagnostic error was very prevalent. Lack of attention paid by healthcare staff or patients to coincidental signs and symptoms can prevent differential diagnoses being considered. 24 Diagnostic error was often due to misinterpretation of ‘routine’ investigations and results were not acted upon or tests were requested without a clear understanding of what results would add to care.
Medication error is a large-scale problem across healthcare, not just within the acute medical unit. In 2015, medication error accounted for just over 10% of the total National Reporting and Learning System reports in England. 25 This study identified that discontinuity of care between different healthcare providers commonly led to medication errors, due to management plans not being implemented following communication failures. 8 Many medication error reports in the acute medical unit occurred overnight and mentioned the inability to reach the out-of-hours pharmacist. The Royal Pharmaceutical Society and NHS England support the need for seven-day pharmacy services in acute hospitals to improve care. 26
Higher patient–doctor ratios and decreased senior presence could explain increased risk of incidents overnight. 2 In this study, patients’ vital signs and early warning scores were often not handed over. 27 The National Patient Safety Agency recognised this concern in ‘Safer Care for Acutely Ill Patients’, as failures to recognise or act on patient deterioration were a major cause of deaths. 27
Strengths and weaknesses
The National Reporting and Learning System reports in this study came from front-line healthcare professionals over a 10-year period and provide deeper insight to the most frequently occurring and severe incidents. However, it is likely underreporting of incidents occurs in the acute medical unit as elsewhere. While we have taken great care to produce a representative sample, it remains possible that some elements may be under or over-represented as the database is dependent on what people choose to report. Reporting bias may influence reporting of near misses or incidents with lesser consequences disproportionately as it is harder to overlook reporting of severe consequences. Seventy-five per cent of the most severe acute medical unit-related incidents in the acute medical unit had to be excluded from the full mixed method analysis, often because of insufficient detail, which could represent the loss of vital learning opportunities. However, this analysis provides the first insight into what is reported as narrative. To reduce confirmation bias, double-coding was used with a high degree of inter-rater reliability of bilaterally included and excluded reports, and collective approaches to analysis were used to increase reflexivity. Despite the limitations outlined, in comparison to previous studies in acute medical units, using National Reporting and Learning System data over a 10-year period, this study provides not just understanding of the categories of incidents leading to severe harm and death but also a methodologically robust interpretation of where gaps in reporting may lie. We also highlight the links between contributing factors (including human factors issues) and the existing evidence base for interventions which can be targeted at the priority themes and metathemes found. Specific interventions that might help are shown in Figure 3.
Meaning of the study
Diagnostic errors are frequently caused by errors in the cognitive processes underpinning diagnosis. 27 These errors can be prevented by using checklists which provide a layout for assessing patients, this can alert clinicians to any areas where more information needs to be collected. 16 In the process map (Figure 2), diagnostic errors were common and often due to inexperience of staff so checklists could help ensure important diagnoses are not missed.
Medication errors can be reduced by the presence of an additional medical admission pharmacist seven days a week, as this can improve the number of full medication histories taken on admission. 21 Many of the medication errors occurring in the acute medical unit could be reduced with wider implementation of electronic prescribing systems. However, in 2013 only 13% of acute NHS hospitals surveyed had a hospital-wide electronic prescribing system. 22 As well as those systems, an integrated electronic health record would allow the prescription chart, patient monitoring and notes to be stored in one place to improve the continuity of care and monitoring of patients, as well as reducing medication errors. 28
Errors related to patient monitoring can be due to ‘alarm fatigue’, where the high volume of alarms causes staff to become unresponsive. Intelligent integrated monitoring systems combine patient parameters to trigger a single alarm for an acutely deteriorating patient, based on their baseline parameters. These alarms are more patient-specific, reducing the risk of redundant alarms causing ‘alarm fatigue’. 23 Intelligent monitoring systems also minimise risk of common human factors issues associated with miscalculating early warning scores and omitted observations, by allowing electronic recording of patients' observations, a recommendation from the Francis Report.23,28,29 Since the introduction of the European Working Time Directive, an increased number of handovers occur in hospitals. Electronic handover systems allow doctors to provide up-to-date patient information, including monitoring, and create lists of outstanding tasks, improving the safety of handovers. 15 Problems during handover were a common cause of errors in patient monitoring and many of these errors occurred overnight. One study showed that having a consultant on the acute medical unit at all times decreased the fatality rate of patients. 12
Future research
Future research in this area should focus on the themes and metathemes in our priority areas to improve the safety of patients in the acute medical unit. This study focussed on the most severe and harmful reports, and future learning from low, moderate and no harm incidents could provide vital learning about common and near miss incidents which account for 99% of the acute medical unit-related National Reporting and Learning System reports.
Conclusion
Underlying incidents within the acute medical unit were decision-making based on incomplete information, lack of care coordination and the necessity of self-advocacy from patients as a safety net. The learning from these reports represents an invaluable opportunity to improve the safety of the acute medical unit for future patients.
Supplemental Material
Supplemental material, sj-pdf-1-jrs-10.1177_01410768211032589 for Learning from patient safety incidents involving acutely sick adults in hospital assessment units in England and Wales: a mixed methods analysis for quality improvement by Alexandra Urquhart, Sarah Yardley, Elin Thomas, Liam Donaldson and Andrew Carson-Stevens in Journal of the Royal Society of Medicine
Footnotes
Funding and Sponsorship: None declared. Cardiff University is the sponsor of the study.
Ethics approval: The Cardiff University School of Medicine Research Ethics Committee reviewed the protocol and waived the need for ethics review (SMREC 16/59). A data sharing agreement exists between Cardiff University and NHS Improvement for this project.
Guarantor: Dr Andrew Carson-Stevens is the guarantor of this study.
Contributorship: All authors have made a substantial contribution to the research design and approved the final version of this paper. AU and ET conducted the initial descriptive analysis under the supervision of ACS and LD. SY independently reviewed this, and leads the interpretative thematic analysis working closely with AU, ET and ACS. LD reviewed the analytic synthesis. AU and SY drafted the article with all authors critically revising the intellectual content.
Data accessibility: The data for this study are held by NHS Improvement (NHSI) who considers applications to use National Reporting and Learning System data on a case-by-case basis. Permission was granted to Cardiff University through a data sharing agreement for the duration of the study.
Acknowledgements: We are grateful to Adele Webb, Peter Buckle, Maisie McKenzie, and Martin Rolph who kindly reviewed Figure 2 from a patient and public involvement (PPI) perspective. We are thankful to Dr Huw Williams for co-supervising elements of this project.
Provenance: Not commissioned; peer-reviewed by Julie Morris, Peter Ross, and Bill Kirkup.
ORCID iD: Sarah Yardley https://orcid.org/0000-0002-1645-642X
Declarations
Competing Interests: None declared.
References
- 1.Panagioti M, Khan K, Keeps RN, et al. Prevalence, severity, and nature of preventable patient harm across medical care settings: systematic review and meta-analysis. BMJ 2019; 366: l4185–l4185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The Royal College of Physicians of London. Acute Medicine: Organisation and Training for the Next Decade, London: The Royal College of Physicians of London, 2004. [Google Scholar]
- 3.Martin IC, Mason DG, Stewart J, et al. Emergency Admissions: A Journey in the Right Direction?, London, UK: National Confidential Enquiry into Patient Outcome and Death, 2007. [Google Scholar]
- 4.Conway R, O'Riordan D, Silke B. Long-term outcome of an AMAU – a decade's experience. QJM 2013; 107: 7–7. [DOI] [PubMed] [Google Scholar]
- 5.Bangor-Raju D, Mudannayake RS, Subbe CP. Safety in the acute medical unit: the role of severity of illness, structure of communication and staffing. Br J Hosp Med 2015; 76(9): C141--144–C141--144. [DOI] [PubMed] [Google Scholar]
- 6.Basey AJ, Kennedy TD, Mackridge AJ, et al. Delays and interruptions in the acute medical unit clerking process: an observational study. J R Soc Med Open 2016; 7: 2054270415619323–2054270415619323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Basey AJ, Krska J, Kennedy TD, et al. Prescribing errors on admission to hospital and their potential impact: a mixed-methods study. BMJ Qual Safe 2014; 23: 17–25. [DOI] [PubMed] [Google Scholar]
- 8.Roughead EE, Semple SJ. Medication safety in acute care in Australia: where are we now? Part 1: a review of the extent and causes of medication problems 2002–2008. Aust New Zealand Health Policy 2009; 6: 18–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Semple SJ, Roughead EE. Medication safety in acute care in Australia: where are we now? Part 2: a review of strategies and activities for improving medication safety 2002-2008. Aust New Zealand Health Policy 2009; 6: 24–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thomas M, Schultz T, Hannaford N, et al. Failures in transition: learning from incidents relating to clinical handover in acute care. J Healthcare Qual 2013; 35: 7–7. [DOI] [PubMed] [Google Scholar]
- 11.Reid LEM, Crookshanks AJF, Jones MC, et al. How is it best to deliver care in acute medical units? A systematic review. QJM 2018; 111: 9–9. [DOI] [PubMed] [Google Scholar]
- 12.Bell D, Lambourne A, Percival F, et al. Consultant input in acute medical admission and patient outcomes in hospitals in England: a multivariate analysis. PLoS One 2013; 35(3): 49--56–49--56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ambrosi E, De Togni S, Guarnier A, et al. In-hospital elderly mortality and associated factors in 12 Italian acute medical unit: findings from an exploratory longitundinal study. Aging Clin Exp Res 2017; 29: 10–10. [DOI] [PubMed] [Google Scholar]
- 14.Risor BW, Lisby M, Sorensen J. Complex automated medication systems reduce medication administration errors in a Danish acute medical unit. Int J Qual Health Care 2018; 30: 8–8. [DOI] [PubMed] [Google Scholar]
- 15.Till A, Sall H, Wilkinson J. Safe handover: safe patients – the electronic handover system. BMJ Qual Improve Rep 2014; 2(2): u202926.w1359. doi: 10.1136/bmjquality.u202926.w1359. eCollection 2014–u202926.w1359. doi: 10.1136/bmjquality.u202926.w1359. eCollection 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Papoutsi C, Poots A, Clements J, et al. Improving patient safety for older people in acute admissions: implementation of the Frailsafe checklist in 12 hospitals across the UK. Age Age 2018; 47: 7–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carson-Stevens A, Hibbert P, Williams H, et al. Characterising the nature of primary care patient safety incident reports in England and Wales National Reporting and Learning System: a mixed-methods agenda-setting study for general practice. Health Serv Deliv Res 2016; 4(27). [PubMed] [Google Scholar]
- 18.Huberman M, Miles M. The Qualitative Researcher's Companion, Thousand Oaks, CA: SAGE Publications, 2002. [Google Scholar]
- 19.Crotty M. The Foundations of Social Research, London: Sage, 1998. [Google Scholar]
- 20.The World Alliance for Patient Safety. Conceptual Framework for the International Classification for Patient Safety. See http://www.who.int/patientsafety/taxonomy/icps_full_report.pdf (last checked 30 June 2020).
- 21.Marotti SB, Cheh RMT, Phuong H. The utility of a medical admissions pharmacist in a hospital in Australia. Int J Clin Pharm 2017; 39: 5–5. [DOI] [PubMed] [Google Scholar]
- 22.Ahmed Z, McLeod MC, Barber N, et al. The use and functionality of electronic prescribing systems in English acute NHS trusts: a cross-sectional survey. PLoS One 2013; 8(11): e80378–e80378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vincent J-L, Einav S, Pearse R, et al. Improving detection of patient deterioration in the general hospital ward environment. Eur J Anaesthesiol 2018; 35: 8–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Croskerry P, Singhal G and Mamede S. Cognitive debiasing 1: origins of bias and theory of debiasing. BMJ Qual Safe 2013; 22: ii58. [DOI] [PMC free article] [PubMed]
- 25.NHS England. Patient safety incident reporting continues to improve. 2015. See https://www.england.nhs.uk/2015/09/patient-safety-reporting/ (last checked 30 June 2020).
- 26.Office of the Chief Pharmaceutical Officer and Medical Directorate. Transformation of seven day clinical pharmacy services in acute hospitals. 2016. See https://www.england.nhs.uk/wp-content/uploads/2016/09/7ds-clinical-pharmacy-acute-hosp.pdf (last checked 30 June 2020).
- 27.World Health Organization. Communication During Patient Hand-Overs, Geneva: World Health Organization, 2007. [Google Scholar]
- 28.National Patient Safety Agency. Safer Care for the Acutely Ill Patient: Learning from Serious Incidents, England: National Patient Safety Agency, 2007. [Google Scholar]
- 29.Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. Executive Summary, London: The Stationary Office, 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-jrs-10.1177_01410768211032589 for Learning from patient safety incidents involving acutely sick adults in hospital assessment units in England and Wales: a mixed methods analysis for quality improvement by Alexandra Urquhart, Sarah Yardley, Elin Thomas, Liam Donaldson and Andrew Carson-Stevens in Journal of the Royal Society of Medicine