ABSTRACT
Objective:
To assess the relationship between malocclusion severity and quality of life in children.
Materials and Method:
Two hundred and seventy-eight children aged 11 to 14 years were recruited voluntarily from the Dental and Maxillofacial Centre of the Almana General Hospital in Alkhobar, Saudi Arabia. The children were asked to fill out the Arabic version of the Child Perception Questionnaire for 11- to 14-year-old children (CPQ11–14) and were then clinically examined to determine the severity of their malocclusion using the Dental Aesthetic Index (DAI). Multivariate analysis of variance was used to compare the four domains and the total CPQ11–14 scores between the four DAI severity groups.
Results:
Significant differences were found between DAI severity groups for the four domains and the total CPQ11–14 scores. Although children with very severe (handicapping) malocclusion had significantly higher domain and total CPQ11–14 scores than all the other groups (differences of up to 6 and 22 units, respectively, compared to children with no/minor malocclusion), there were no differences between those with no/minor, definite, and severe malocclusion.
Conclusion:
These findings suggest that only very severe malocclusion had an impact on the quality of life of the participants. Orthodontists should focus not only on clinical measures of malocclusion but should also consider the impact of severe malocclusion on patients' quality of life.
Keywords: Oral health–related quality of life, Malocclusion, Orthodontic treatment need
INTRODUCTION
A review concluded that there is a need for a more comprehensive and rigorous evaluation of the impacts of malocclusion and its associated need for orthodontic treatment on people's quality of life.1 The use of standardized measures to assess malocclusion and the Oral Health Related Quality of Life (OHRQoL) was therefore encouraged to produce uniform findings across studies that are amenable to meta-analysis.1,2
The assessment of malocclusion in epidemiologic studies is often conducted using clinical indices.3 The Dental Aesthetic Index (DAI) was developed to rank dental esthetics and orthodontic treatment needs on a scale of social norms for a socially acceptable dental appearance.4,5 The DAI has proven to be a reliable, valid, simple, and easily applied index.6,7 It has been adopted by the World Health Organization as a cross-cultural index8 and applied in diverse ethnic groups without modification.9–11 All these reasons made it a suitable epidemiologic index for use in developing countries that lack a specifically developed orthodontic treatment need index.
A number of OHRQoL measures have been developed for use with children, but none is widely accepted. The Child Oral Health Quality of Life Questionnaire (COHQoL) is a set of multidimensional scales measuring the effects of oral and orofacial conditions on the functional, emotional, and social well-being of children and their families. The COHQoL consists of the Parental-Caregiver Perceptions Questionnaire,12 the Family Impact Scale,13 and three age-specific questionnaires for children (Child Perceptions Questionnaires, CPQs).14,15 The choice of one or more of these measures depends on the specific objectives of the research under development. The long version of the CPQ for 11- to 14-year-old children (CPQ11–14) has been cross-culturally validated among Saudi children.16
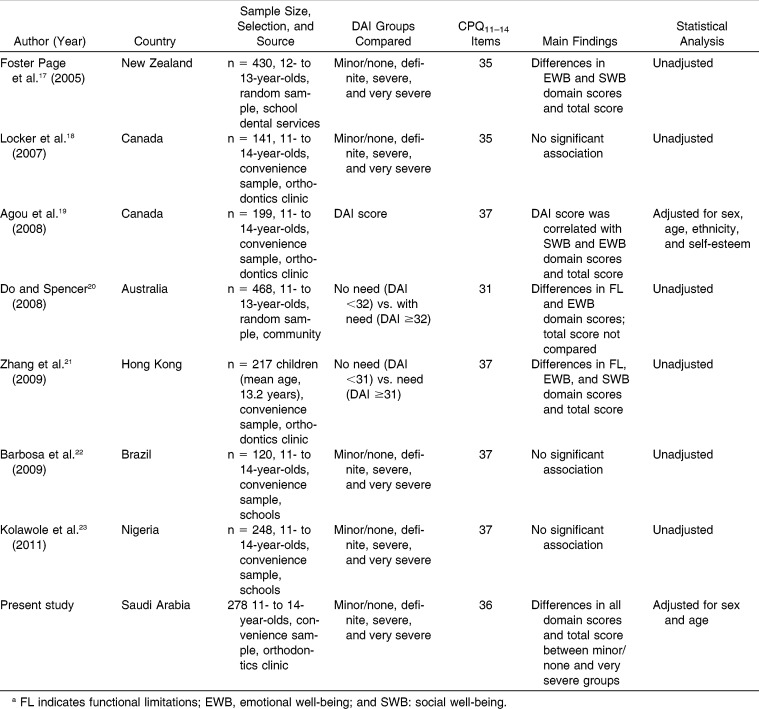
Although some studies have explored how malocclusion affects children's quality of life using both the DAI and the long version of the CPQ11–14,17–23 results are conflicting; some report a significant association between DAI and CPQ11–14 scores17,19–21 and others fail to do so (Table 1).18,22,23 In addition, most studies come from developed countries.17–22 It is thus uncertain whether these findings can be generalized to cultures and settings like those in the Middle East and other developing countries, which have different patterns of oral diseases, use of dental services, and perceptions of oral conditions. As the demand for orthodontic care rises in Saudi Arabia, a better understanding of the functional and psychosocial consequences of malocclusion may help improve orthodontic treatment needs assessment and prioritize orthodontic care.
Table 1.
Summary of Studies Exploring the Association Between Children's Malocclusion, According to the Dental Aesthetic Index (DAI), and Quality of Life, According to the Long Version of the Child Perception Questionnaire for 11- to 14-year-old Children (CPQ11–14)a
Therefore, the aim of this study was to assess the relationship between malocclusion severity, as assessed by the DAI, and children's quality of life, as assessed by the CPQ11–14. We hypothesized that children's quality of life deteriorates with increasing levels of malocclusion severity.
MATERIALS AND METHODS
Study Sample
This was a cross-sectional study based on a convenience sample of hospital volunteers. A total of 278 children aged 11 to 14 years old were consecutively recruited from those attending the Dental and Maxillofacial Centre of the Almana General Hospital (Alkhobar, Saudi Arabia) between May and June 2012. All participants were Saudi nationals (both parents were born in the country) with full permanent dentition and no history of orthodontic treatment or congenital anomalies. A minimum sample size of 188 subjects (47 in each of the four levels of malocclusion according to the DAI) was required to estimate a mean difference in the total CPQ11–14 score equal or greater than 10 units between two of those groups, with an 80% statistical power, a 95% confidence level, and a common standard deviation (SD) of 17 units (as reported by Locker et al.18 among children with malocclusion).
The study protocol was approved by King's College London Research Ethics Committee (BDM/11/12-71). Written informed consent was obtained from parents or guardians and verbal assent was obtained from children before participation in the study.
Data Collection
Data were collected through self-administered questionnaires and clinical examinations. Children were asked to fill out the Arabic version of the CPQ11–14 questionnaire in the presence of their parents, but without any help from them. Each child was given an explanation on how to fill out the questionnaire and instructed that only one answer should be marked per item. The Arabic version of the CPQ11–14 consists of 36 items enquiring about effects on four health domains: 0ral Symptoms (6 items), functional limitations (9 items), emotional well-being (9 items), and social well-being (12 items).16 The only difference between the English and Arabic versions of the CPQ11–14 is that one of the 13 items originally included in the social well-being domain (difficulty playing musical instruments) was dropped during the validation process as Saudi children rarely study music.16 Questions ask about the frequency of events in the past 3 months in relation to child's oral/orofacial condition. The response options are never (0), once/twice (1), sometimes (2), often (3), and everyday/almost every day (4). The four domain scores were computed by adding up all the item responses in a particular domain, and the overall CPQ11–14 score was computed by summing up the four domain scores. Lower scores indicated better OHRQoL. In this sample, Cronbach's alpha was 0.954 for the full CPQ11–14 questionnaire and ranged between 0.824 and 0.912 for individual domains.
Thereafter, children were clinically examined by one calibrated orthodontist using the DAI,4,8 which assesses the relative social acceptability of dental appearance by collecting and weighting data on 10 intraoral measurements. The DAI score for a child was obtained by using the following regression equation: (Number of missing incisor, canine, and premolar teeth [0 to 20] × 6) + (Number of incisal segments with crowding [0 to 2]) + (Number of incisal segments with spacing [0 to 2]) + (Midline diastema [mm] × 3) + (Largest anterior maxillary irregularity [mm]) + (Largest anterior mandibular irregularity [mm]) + (Anterior maxillary overjet [mm] × 2) + (Anterior mandibular overjet [mm] × 4) + (Vertical anterior openbite [mm] × 4) + (Antero-posterior molar relation [Largest deviation from normal relation: 0 = normal, 1 = half cusp, and 2 = full cusp] × 3) + 13. Higher DAI scores indicate less socially accepted dental esthetics.
The DAI score enables each child to be placed on a dental appearance continuum ranging from 13 (the most socially acceptable) to 100 (the least acceptable), and orthodontic treatment can then be prioritized using the predefined categories of no or slight (DAI score ≤25), elective (26–30), highly desirable (31–35), and mandatory need (≥36).5,8 Intraexaminer reliability was assessed by conducting replicated examinations on 30 dental casts; an intraclass correlation coefficient of 0.99 was attained. The mean difference in DAI score between examinations was 0.13 units (SD = 0.51).
Statistical Analysis
Domain and total scores were slightly skewed, suggesting the use of nonparametric tests. However, we used the multivariate analysis of variance (MANOVA) to compare, first jointly and then individually, the four domain scores and the total score as MANOVA has several advantages over nonparametric tests. It allows comparison of multiple and inter-correlated outcome measures (five in this study, namely the four domain and the total CPQ11–14 scores), compensating for multiple comparisons by using omnibus tests for multiple outcomes and multiple groups, controlling for confounders (sex and age in this study, both of which were treated as categoric) and testing for interactions between explanatory variables. Post hoc comparisons between pairs of malocclusion groups were conducted using Scheffe's test and only when omnibus tests were statistically significant.
RESULTS
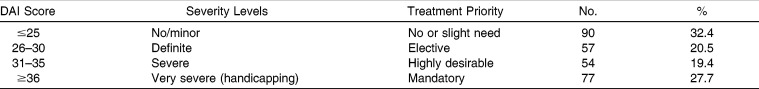
This study included 278 children (139 boys and 139 girls) with a mean age of 12.6 years (SD = 1.7; range = 11–14 years). The mean DAI score was 30.7 (SD = 9.1; range = 15–59). The distribution of the sample by severity of malocclusion is reported in Table 2. Conditions related to spacing/crowding were the most common malocclusion traits in this group.
Table 2.
Distribution of the Sample by Severity of Malocclusion (n = 278)
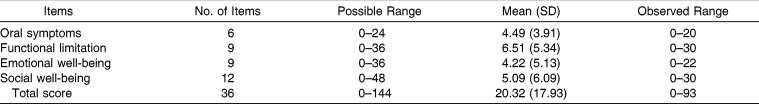
Mean scores for the oral symptoms, functional limitations, emotional well-being, and social well-being domains were 4.49 (SD = 3.91), 6.51 (SD = 5.34), 4.22 (SD = 5.13), and 5.09 units (SDG6.09), respectively (Table 3). The mean total score was 20.32 units (SD = 17.93). Three participants had floor effects (ie, zero total score), but no participants had ceiling effects (ie, maximum total score).
Table 3.
Domain and Total Scores on the Child Perception Questionnaire for 11- to 14-year-old Children in the Sample (n = 278)
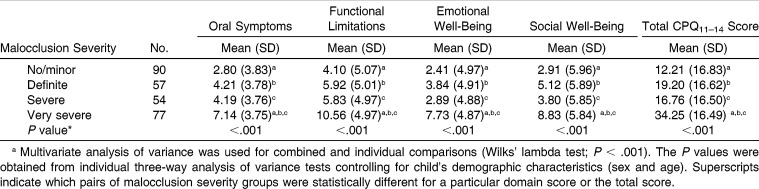
There were significant differences between the DAI severity groups in terms of domain and total CPQ11–14 scores, both jointly (Wilks' lambda test, P < .001) and individually (ANOVA test; P < .001 for each score). In the comparisons by pairs, it was found that children with very severe malocclusion had significantly higher scores than all the other groups, but there were no differences in scores between children with no/minor, definite, and severe malocclusion. Differences of up to 6 units in domain scores and 22 units in the total score were found between the two extreme groups (Table 4). There were no differences in domain and total CPQ11–14 scores by sex or age (Wilks' lambda test; P = .063 and .363, respectively). The interaction terms of malocclusion severity with sex and age were not statistically significant either (Wilks' lambda test; P = .761 and .640, respectively).
Table 4.
Domain and Total Scores on the Child Perception Questionnaire for 11- to 14-year-old Children (CPQ11–14) by Dental Aesthetic Index (DAI) Malocclusion Severity (n = 278)a
DISCUSSION
This study shows that malocclusion affects children's quality of life. Both the domain and total CPQ11–14 scores were lowest for the no/minor malocclusion category and highest for the very severe (handicapping) category, with between-group differences of up to 6 units and 22 units in the domain and total scores, respectively. However, and contrary to what was hypothesized, a clear ascending gradient was not observed across the four DAI severity groups as only children with very severe malocclusion had significantly higher scores than children in the other three groups, and no differences were found between groups with no/minor, definite, and severe malocclusion.
The lack of an ascending gradient in CPQ11–14 scores by malocclusion severity could be explained by a number of reasons. First is sample size. A smaller sample size may affect the distribution of subjects in each DAI category, thereby affecting the correlation between malocclusion severity and CPQ11–14 scores.18 However, in this study differences between groups with no/minor, definite, and severe malocclusion ranged between 2 and 7 units for the total score. As the minimally importance difference for the CPQ11–14 has been set at 7 units,24 the aforementioned differences may not be regarded as clinically important, even when significant findings may be found with larger sample sizes. A second explanation relates to the questionnaire itself, as the CPQ11–14 was not developed specifically with malocclusion in mind, and symptoms like pain and bleeding are irrelevant to malocclusion and can be due to other oral conditions. Items in the oral symptoms and functional limitations domains are generic and affected more by other oral conditions, whereas the emotional and social well-being domains contain items that could be affected in eminently orthodontic samples.18 As this is the first study reporting significant differences in all four CPQ11–14 domains between the two extreme groups (Table 1), further research is needed to corroborate the present findings. New studies will benefit from using various indices to assess malocclusion as a way to control for their known differences.3 A final explanation is that moderate forms of malocclusion (ie, groups with definite and severe malocclusion for which treatment is respectively elective or highly desirable according to the DAI) may not really affect children's quality of life, and only those with handicapping forms of malocclusion truly had a clinically important effect on their quality of life. This interpretation is supported by the fact that the two previous studies in developing countries did not show significant associations between malocclusion severity and quality of life22,23 whereas most studies in developed countries reported significant findings.17,19–21 It can therefore be argued that cultural influences, treatment expectations, and access to orthodontic services may play a role in how malocclusion affects children's quality of life. Although Saudi nationals are provided with free dental and orthodontic treatment at Ministry of Health hospitals, some do not use those services or prefer to seek care in the private sector.
Our findings suggest that orthodontists should consider not only the patients' clinical characteristics but also their effects on quality of life and render treatment accordingly. The OHRQoL measures have the potential to provide insights into how oral conditions affect aspects of everyday life that are important to people.25–27 As such, they can complement traditional or professionally determined outcome measures for the assessment of orthodontic treatment needs and prioritization of care to those who need it most.25 Providing orthodontic treatment to those who are not aware or do not care about their dental appearance and denying treatment to those who are functionally or psychosocially affected by malocclusion is a waste of valuable limited manpower resources.
Some limitations of this study need to be addressed. First, the present findings are based on a convenience sample and may not represent the general population of children in Saudi Arabia. However, we preferred using a hospital-based sample rather than a population-based sample as the latter might not have provided sufficient cases with severe or very severe malocclusion for a meaningful comparison. Second, the CPQ11–14 questionnaire used in this study is a generic OHRQoL measure, and as such, it captures effects on quality of life attributed not only to malocclusion but also to all oral conditions. The use of condition-specific OHRQoL measures is therefore encouraged in further studies, as they can help distinguishing the effects attributed to malocclusion from those caused by other oral conditions.28–30 A final limitation relates to the role of potential confounders, particularly socioeconomic factors and other oral conditions present in a child's mouth (such as dental caries), which are known to be related to malocclusion and OHRQoL. However, most patients attending the selected hospital were from high socioeconomic status, which may have provided a way to control for socioeconomic characteristics (ie, by sample restriction). Similarly, patients at this hospital are referred to the orthodontic clinic once they have completed their treatment for other oral conditions. Nevertheless, new studies may benefit from taking into consideration some other factors when exploring the association between malocclusion and quality of life.
CONCLUSIONS
Malocclusion affects the quality of life of 11- to 14-year-old children.
Children with very severe (handicapping) malocclusion reported more oral symptoms and functional limitations as well as poorer emotional and social well-being than those with normal or minor malocclusion.
However, there were no differences in the domain and total CPQ11–14 scores between children with no/minor, definite, and severe malocclusion.
ACKNOWLEDGMENT
We would like to thank Mr Ebrahim M. Almana, chairman, Almana General Hospitals, for granting us permission to conduct the study at the hospital and Dr Aisha Dawoodbhoy for data management.
REFERENCES
- 1.Liu Z, McGrath C, Hagg U. The impact of malocclusion/orthodontic treatment need on the quality of life. A systematic review. Angle Orthod. 2009;79:585–591. doi: 10.2319/042108-224.1. [DOI] [PubMed] [Google Scholar]
- 2.Cunningham SJ, Hunt NP. Quality of life and its importance in orthodontics. J Orthod. 2001;28:152–158. doi: 10.1093/ortho/28.2.152. [DOI] [PubMed] [Google Scholar]
- 3.Jarvinen S. Indexes for orthodontic treatment need. Am J Orthod Dentofacial Orthop. 2001;120:237–239. doi: 10.1067/mod.2001.114830. [DOI] [PubMed] [Google Scholar]
- 4.Cons NC, Jenny J, Kohout FJ. DAI The Dental Aesthetic Index. Iowa City, Iowa: College of Dentistry, University of Iowa; 1986. [Google Scholar]
- 5.Jenny J, Cons NC. Establishing malocclusion severity levels on the Dental Aesthetic Index (DAI) scale. Aust Dent J. 1996;41:43–46. doi: 10.1111/j.1834-7819.1996.tb05654.x. [DOI] [PubMed] [Google Scholar]
- 6.Jenny J, Cons NC. Comparing and contrasting two orthodontic indices, the Index of Orthodontic Treatment Need and the Dental Aesthetic Index. Am J Orthod Dentofacial Orthop. 1996;110:410–416. doi: 10.1016/s0889-5406(96)70044-6. [DOI] [PubMed] [Google Scholar]
- 7.Beglin FM, Firestone AR, Vig KW, Beck FM, Kuthy RA, Wade D. A comparison of the reliability and validity of 3 occlusal indexes of orthodontic treatment need. Am J Orthod Dentofacial Orthop. 2001;120:240–246. doi: 10.1067/mod.2001.116401. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. Oral Health Surveys Basic Methods. Geneva, Switzerland: World Health Organization; 1997. [Google Scholar]
- 9.Cons NC, Jenny J, Kohout FJ, Songpaisan Y, Jotikastira D. Utility of the dental aesthetic index in industrialized and developing countries. J Public Health Dent. 1989;49:163–166. doi: 10.1111/j.1752-7325.1989.tb02054.x. [DOI] [PubMed] [Google Scholar]
- 10.Cons NC, Jenny J. Comparing perceptions of dental aesthetics in the USA with those in eleven ethnic groups. Int Dent J. 1994;44:489–494. [PubMed] [Google Scholar]
- 11.Cons NC, Jenny J, Kohout FJ, et al. Comparing ethnic group-specific DAI equations with the standard DAI. Int Dent J. 1994;44:153–158. [PubMed] [Google Scholar]
- 12.Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G. Measuring parental perceptions of child oral health-related quality of life. J Public Health Dent. 2003;63:67–72. doi: 10.1111/j.1752-7325.2003.tb03477.x. [DOI] [PubMed] [Google Scholar]
- 13.Locker D, Jokovic A, Stephens M, Kenny D, Tompson B, Guyatt G. Family impact of child oral and oro-facial conditions. Community Dent Oral Epidemiol. 2002;30:438–448. doi: 10.1034/j.1600-0528.2002.00015.x. [DOI] [PubMed] [Google Scholar]
- 14.Jokovic A, Locker D, Tompson B, Guyatt G. Questionnaire for measuring oral health-related quality of life in eight- to ten-year-old children. Pediatr Dent. 2004;26:512–518. [PubMed] [Google Scholar]
- 15.Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G. Validity and reliability of a questionnaire for measuring child oral-health-related quality of life. J Dent Res. 2002;81:459–463. doi: 10.1177/154405910208100705. [DOI] [PubMed] [Google Scholar]
- 16.Brown A, Al-Khayal Z. Validity and reliability of the Arabic translation of the child oral-health-related quality of life questionnaire (CPQ11–14) in Saudi Arabia. Int J Paediatr Dent. 2006;16:405–411. doi: 10.1111/j.1365-263X.2006.00775.x. [DOI] [PubMed] [Google Scholar]
- 17.Foster Page LA, Thomson WM, Jokovic A, Locker D. Validation of the Child Perceptions Questionnaire (CPQ 11–14) J Dent Res. 2005;84:649–652. doi: 10.1177/154405910508400713. [DOI] [PubMed] [Google Scholar]
- 18.Locker D, Jokovic A, Tompson B, Prakash P. Is the Child Perceptions Questionnaire for 11–14 year olds sensitive to clinical and self-perceived variations in orthodontic status. Community Dent Oral Epidemiol. 2007;35:179–185. doi: 10.1111/j.1600-0528.2006.00324.x. [DOI] [PubMed] [Google Scholar]
- 19.Agou S, Locker D, Streiner DL, Tompson B. Impact of self-esteem on the oral-health-related quality of life of children with malocclusion. Am J Orthod Dentofacial Orthop. 2008;134:484–489. doi: 10.1016/j.ajodo.2006.11.021. [DOI] [PubMed] [Google Scholar]
- 20.Do LG, Spencer AJ. Evaluation of oral health-related quality of life questionnaires in a general child population. Community Dent Health. 2008;25:205–210. [PubMed] [Google Scholar]
- 21.Zhang M, McGrath C, Hagg U. Orthodontic treatment need and oral health-related quality among children. Community Dent Health. 2009;26:58–61. [PubMed] [Google Scholar]
- 22.Barbosa TS, Tureli MC, Gaviao MB. Validity and reliability of the Child Perceptions Questionnaires applied in Brazilian children. BMC Oral Health. 2009;9:13. doi: 10.1186/1472-6831-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kolawole KA, Otuyemi OD, Oluwadaisi AM. Assessment of oral health-related quality of life in Nigerian children using the Child Perceptions Questionnaire (CPQ 11–14) Eur J Paediatr Dent. 2011;12:55–59. [PubMed] [Google Scholar]
- 24.Agou S, Malhotra M, Tompson B, Prakash P, Locker D. Is the child oral health quality of life questionnaire sensitive to change in the context of orthodontic treatment? A brief communication. J Public Health Dent. 2008;68:246–248. doi: 10.1111/j.1752-7325.2008.00093.x. [DOI] [PubMed] [Google Scholar]
- 25.Locker D, Allen F. What do measures of ‘oral health-related quality of life’ measure. Community Dent Oral Epidemiol. 2007;35:401–411. doi: 10.1111/j.1600-0528.2007.00418.x. [DOI] [PubMed] [Google Scholar]
- 26.Sischo L, Broder HL. Oral health-related quality of life: what, why, how, and future implications. J Dent Res. 2011;90:1264–1270. doi: 10.1177/0022034511399918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Slade GD. Oral health-related quality of life is important for patients, but what about populations. Community Dent Oral Epidemiol. 2012;40(suppl 2):39–43. doi: 10.1111/j.1600-0528.2012.00718.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bernabé E, de Oliveira CM, Sheiham A. Condition-specific sociodental impacts attributed to different anterior occlusal traits in Brazilian adolescents. Eur J Oral Sci. 2007;115:473–478. doi: 10.1111/j.1600-0722.2007.00486.x. [DOI] [PubMed] [Google Scholar]
- 29.Bernabé E, Sheiham A, de Oliveira CM. Condition-specific impacts on quality of life attributed to malocclusion by adolescents with normal occlusion and Class I, II and III malocclusion. Angle Orthod. 2008;78:977–982. doi: 10.2319/091707-444.1. [DOI] [PubMed] [Google Scholar]
- 30.Bernabé E, Sheiham A, de Oliveira CM. Impacts on daily performances attributed to malocclusions by British adolescents. J Oral Rehabil. 2009;36:26–31. doi: 10.1111/j.1365-2842.2008.01899.x. [DOI] [PubMed] [Google Scholar]