To the editor,
Breast cancer (BC) is the second leading cause of cancer-related mortality and the most common malignancy among women [1]. Most of the BC subtypes are being associated with mutations in BRCA1 and BRCA2; however, p53 mutations are associated with more aggressive disease outcomes and poor prognosis [2]. Besides, BC cells are shown to express ACE2, TMPRSS2, and DPP-IV [3]. However, most aggressive BC cells are known to be associated with the lower expression of ACE2 along with a concomitant increase in the expression of TMPRSS2 and DPP-IV [4], [5], [6], [7]. Here, it is interesting that ACE2 is the main receptor for the entry of SARS-CoV-2 via binding of viral spike protein (S) and TMPRSS2 contribute to the priming of S protein, whereas DPP-IV was thought to be a co-receptor for the entry of SARS-CoV-2 and the main receptor for MERS-CoV entry [3]. Last two decades witnessed the ONYX-015 oncolytic adenovirus therapy mainly for solid tumors. This adenovirus virus has a deletion of 827 bp in E1B region of the viral genome and also having a point mutation that generates premature stop codon through which it prevents expression of truncated form of the E1B55K protein. Therefore, these mutations render ONYX-015 incapable of blocking the p53 functions and its degradation in p53 (+) cells. Hence, in healthy cells where p53 is a functional-wild type and/or its pathway is also intact, this infection will trigger the accumulation of p53 in nucleoplasm which will evoke growth arrest or apoptosis resulting abortion of viral replication. In contrast, tumor cells do not possess functional p53, thus ONYX-015 selectively replicates in those tumor cells, resulting the selective destruction of tumor cells [8].
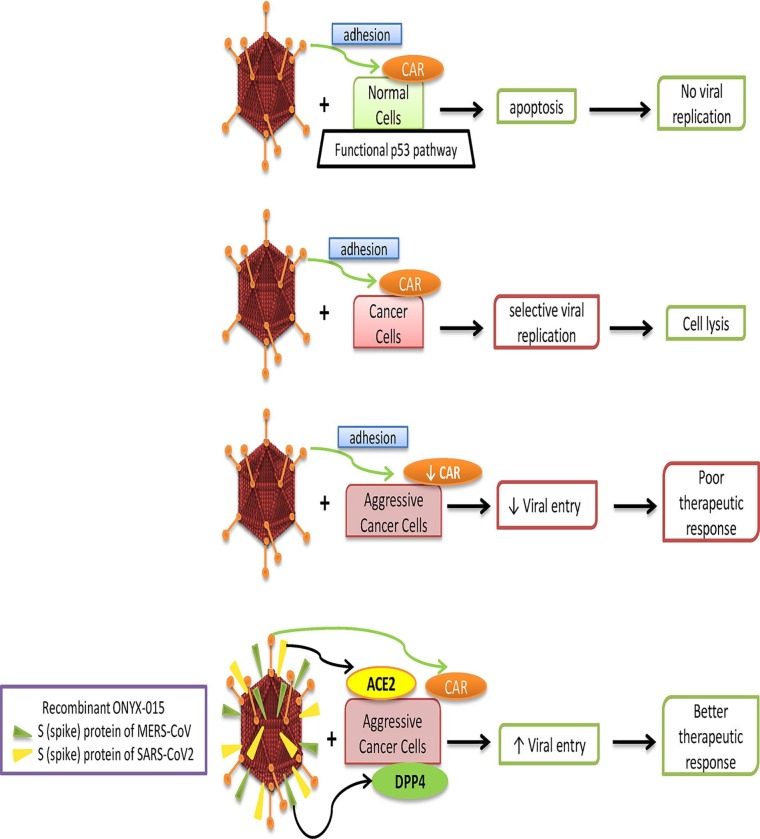
However, entry of this engineered virus depends upon the expression of cell surface Coxsackie-and adenovirus receptor (CAR) by the host cells [9], [10]. Several oncolytic adenovirus therapies including ONYX-015 have shown to be effective against breast cancer [11], [12]. Although, most aggressive malignant cells are shown to down-regulate CAR, thereby reducing the efficacy of ONYX-015 therapy [10], [13]. Here, we hypothesize that restructuring of ONYX-015 by incorporation of spike protein coding genes (‘S’) from SARS-CoV-2 and MERS-CoV may enhance the entry of ONYX-015 virus into the aggressive BC cells that may result in the efficient remission of cancer cells.
In fact, ‘S’ protein of SARS-CoV-2 is involved into the cellular entry of virus through ACE2 receptors after priming by a protease enzyme TMPRSS2, whereas ‘S’ protein of MERS-CoV is responsible for its entry via DPP-IV receptors [3]. Here, it is noteworthy that DPP-IV is also thought to be a co receptor for the entry of SARS-CoV-2. It is pertinent that in most of the aggressive breast cancers lower expression of ACE2 and CAR were observed with the concomitantly increased expression of TMPRSS2 and DPP-IV [2], [3], [10], [13].
Interestingly, several clinical studies have shown that CAR expression is higher in low-grade breast cancer [13], [14] and it increased adenoviral transduction that resultantly improved selective vulnerability of chemotherapy-resistant tumors along with inhibition of metastasis [15]. CAR has also been shown to perform tumor suppressor functions via inhibition of prosurvival and EMT pathways [16], whereas loss of CAR was found to be associated with increase in invasion and metastasis [17], but co-administration of paclitaxel with replication-incompetent oncolytic adenovirus was shown to be synergistically effective [18]. These reports clearly suggest down regulation of CAR in aggressive BC, thus ONYX-015 cannot treat such cancer cases efficiently due to poor entry in the aggressive BC cells and therefore, we hypothesize to restructure ONYX-015 for efficient therapy of aggressive breast cancer.
To develop more efficient oncolytic therapy including aggressive BC, we conceptualize that: 1. low malignant cells will express more ACE2 and CAR, so the virus can easily enter into these cells, 2. highly malignant cells will over express DPP-IV and TMPRSS2, so viral entry will be facilitated by DPP-IV receptors to those cells, 3. whereas in moderate malignant cells viral entry will be facilitated by overall more options of entry into the cells (besides CAR, ACE2 and DPP-IV) (Fig. 1 ). Another reason for low viral availability to the target was the presence of stroma (collagen fibers and CAR-negative fibroblasts) along with the necrotic areas within the tumors; diminish the amount of virus available to the target cells [19]. Hence, addition of ‘S’ protein genes in ONYX-015 will also compensate for the diluting effects of CAR-ve fibroblasts and necrotic areas by multiple viral entry points.
Fig. 1.
Effects of ONYX-015 and restructured virus on various cell types. This figure shows the therapeutic response of ONYX-015 on normal, cancer and aggressive breast cancer cells. Restructuring of ONYX-015 using spike protein genes from SARS-CoV-2 and MERS-CoV may improve the therapeutic response by facilitated viral entry.
Another limitation of ONYX-015 is the immune response that triggers via recognition of viral antigens causing elimination of the infected cells before the production of sufficient viral copies for infecting the neighboring cells. In ONYX-015 there is a deletion of E3B region where viral gp19k gene was located which inhibits MHC class I antigen presentation at the cell surface [20]. In clinical trials of ONYX-015 on solid tumor patients, an increase in pro-inflammatory cytokine TNF-α was observed through which viral clearance was accelerated. However, anti-TNF drug Enbrel was found to be effective to improve the efficacy of ONYX-015 [19]. Hence, we hypothesize that ONYX-015 can be restructured by using spike (S) protein genes from SARS-CoV-2 and MERS-CoV to develop additional entry points besides CAR via ACE2 and DPP-IV receptors, respectively. In addition, anti-TNF drug Enbrel along with ONYX-015 may be administered to enhance the oncolytic efficacy of the restructured virus.
Funding
The work was supported by the CSIR-JRF fellowships to Ms. Pooja Jaiswal (File No. 09/301 (0137)/2019-EMR-I) and Ms. Versha Tripathi (09/301 (0138)/2019-EMR-I). We also acknowledge the India-Belarus joint project (DST/ INT/BLR/P-24/2019) funded by Department of Science and Technology, New Delhi, sanctioned to Dr. Hamendra Singh Parmar.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Jaiswal P., Tripathi V., Nayak A., Kataria S., Lukashevich V., Das A.K., et al. A molecular link between diabetes and breast cancer: Therapeutic potential of repurposing incretin-based therapies for breast cancer. Curr Cancer Drug Targets. 2021;21(10):829–848. doi: 10.2174/1568009621666210901101851. [DOI] [PubMed] [Google Scholar]
- 2.Gasco M., Shami S., Crook T. The p53 pathway in breast cancer. Breast Cancer Res. 2002;4:70–76. doi: 10.1186/bcr426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parmar H.S., Nayak A., Gavel P.K., Jha H.C., Bhagwat S., Sharma R. Cross talk between COVID-19 and breast cancer. Curr Cancer Drug Targets. 2021;21(7):575–600. doi: 10.2174/1568009621666210216102236. [DOI] [PubMed] [Google Scholar]
- 4.Cheng H.C., Abdel-Ghany M., Zhang S., Pauli B.U. Is the Fischer 344/CRJ rat a protein-knock-out model for dipeptidyl peptidase IV-mediated lung metastasis of breast cancer? Clin Exp Metastasis. 1999;17:609–615. doi: 10.1023/a:1006757525190. [DOI] [PubMed] [Google Scholar]
- 5.Choi H.J., Kim J.Y., Lim S.C., Kim G., Yun H.J., Choi H.S. Dipeptidyl peptidase 4 promotes epithelial cell transformation and breast tumorigenesis via induction of PIN1 gene expression. Br J Pharmacol. 2015;172:5096–5109. doi: 10.1111/bph.13274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yu C., Tang W., Wang Y., Shen Q., Wang B., Cai C., et al. Downregulation of ACE2/Ang-(1–7)/Mas axis promotes breast cancer metastasis by enhancing store-operated calcium entry. Cancer Lett. 2016;376(2):268–277. doi: 10.1016/j.canlet.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 7.Chi M, Shi X, Huo X, Wu X, Zhang P, Wang G. Dexmedetomidine promotes breast cancer cell migration through Rab11-mediated secretion of exosomal TMPRSS2. Ann Transl Med. 2020; 8: 531. [DOI] [PMC free article] [PubMed]
- 8.Kelly E., Russell S.J. History of oncolytic viruses: genesis to genetic engineering. Mol Ther. 2007;15(4):651–659. doi: 10.1038/sj.mt.6300108. [DOI] [PubMed] [Google Scholar]
- 9.Bergelson J.M., Cunningham J.A., Droguett G., Kurt-Jones E.A., Krithivas A., Hong J.S., et al. Isolation of a common receptor for Coxsackie B viruses and adenoviruses 2 and 5. Science. 1997;275(5304):1320–1323. doi: 10.1126/science.275.5304.1320. [DOI] [PubMed] [Google Scholar]
- 10.Li Y., Pong R.C., Bergelson J.M., Hall M.C., Sagalowsky A.I., Tseng C.P., et al. Loss of adenoviral receptor expression in human bladder cancer cells: a potential impact on the efficacy of gene therapy. Cancer Res. 1999;59:325–330. [PubMed] [Google Scholar]
- 11.Hartkopf A.D., Fehm T., Wallwiener D., Lauer U.M. Oncolytic virotherapy of breast cancer. Gynecol Oncol. 2011;123(1):164–171. doi: 10.1016/j.ygyno.2011.06.021. [DOI] [PubMed] [Google Scholar]
- 12.Wang J., Hu P., Zeng M., Rabkin S.D., Liu R. Oncolytic herpes simplex virus treatment of metastatic breast cancer. Int J Oncol. 2012;40:757–763. doi: 10.3892/ijo.2011.1266. [DOI] [PubMed] [Google Scholar]
- 13.Auer D., Reimer D., Porto V., Fleischer M., Roessler J., Wiedemair A., et al. Expression of coxsackie-adenovirus receptor is related to estrogen sensitivity in breast cancer. Breast Cancer Res Treat. 2009;116(1):103–111. doi: 10.1007/s10549-008-0108-0. [DOI] [PubMed] [Google Scholar]
- 14.Martin T.A., Watkins G., Jiang W.G. The Coxsackie-adenovirus receptor has elevated expression in human breast cancer. Clin Exp Med. 2005;5(3):122–128. doi: 10.1007/s10238-005-0076-1. [DOI] [PubMed] [Google Scholar]
- 15.Sakhawat A., Ma L., Muhammad T., Khan A.A., Chen X., Huang Y. A tumor targeting oncolytic adenovirus can improve therapeutic outcomes in chemotherapy resistant metastatic human breast carcinoma. Sci Rep. 2019;9:7504. doi: 10.1038/s41598-019-43668-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nilchian A., Johansson J., Ghalali A., Asanin S.T., Santiago A., Rosencrantz O., et al. CXADR-Mediated Formation of an AKT Inhibitory Signalosome at Tight Junctions Controls Epithelial-Mesenchymal Plasticity in Breast Cancer. Cancer Res. 2019;79(1):47–60. doi: 10.1158/0008-5472.CAN-18-1742. [DOI] [PubMed] [Google Scholar]
- 17.Johansson J., Berg T., Kurzejamska E., Pang M.-F., Tabor V., Jansson M., et al. MiR-155-mediated loss of C/EBPβ shifts the TGF-β response from growth inhibition to epithelial-mesenchymal transition, invasion and metastasis in breast cancer. Oncogene. 2013;32(50):5614–5624. doi: 10.1038/onc.2013.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kasala D., Lee S.-H., Hong J.W., Choi J.-W., Nam K., Chung Y.H., et al. Synergistic antitumor effect mediated by a paclitaxel-conjugated polymeric micelle-coated oncolytic adenovirus. Biomaterials. 2017;145:207–222. doi: 10.1016/j.biomaterials.2017.08.035. [DOI] [PubMed] [Google Scholar]
- 19.Nemunaitis J., Senzer N., Sarmiento S., Zhang Y.-A., Arzaga R., Sands B., et al. A phase I trial of intravenous infusion of ONYX-015 and enbrel in solid tumor patients. Cancer Gene Ther. 2007;14(11):885–893. doi: 10.1038/sj.cgt.7701080. [DOI] [PubMed] [Google Scholar]
- 20.Ries S., Korn W.M. ONYX-015: mechanism of action and clinical potential of replication-selective adenovirus. Br J Cancer. 2002;86:5–11. doi: 10.1038/sj.bjc.6600006. [DOI] [PMC free article] [PubMed] [Google Scholar]