Abstract
Background
Coronavirus disease 2019 (COVID-19) is generally asymptomatic or mild in otherwise healthy children, however, severe cases may occur. In this study, we report the clinical characteristics of children classified as critical COVID-19 in Korea to provide further insights into risk factors and management in children.
Methods
This study was a retrospective case series of children < 18 years of age classified as critical COVID-19. Cases were identified by the Korea Disease Control and Prevention Agency surveillance system and medical records were reviewed. Critical COVID-19 was defined as cases with severe illness requiring noninvasive (high flow nasal cannula, continuous positive airway pressure, or bilevel positive airway pressure) or invasive mechanical ventilation, extracorporeal membrane oxygenation (ECMO) or continuous renal replacement therapy (CRRT), between January 20, 2020 and October 7, 2021.
Results
Among 39,146 cases diagnosed with COVID-19 in subjects < 18 years of age, eight cases (0.02%) were identified as critical COVID-19. The median age was 13 years (range 10 month–17 years) and male-to-female ratio was 1:1. Three children had underlying diseases; one child has asthma and major depressive disorder, one child had Lennox-Gastaut syndrome and one child had mental retardation and was newly diagnosed with type 2 diabetes mellitus with the diagnosis of COVID-19. Among the eight children, seven were obese (body mass index range [BMI] median 29.3, range 25.9–38.2, weight-for-length > 97% for infant) and one was overweight (BMI 21.3). All patients had fever, six patients had dyspnea or cough and other accompanied symptoms included sore throat, headache, lethargy and myalgia. Radiologic findings showed pneumonia within 1–8 days after symptom onset. Pneumonia progressed in these children for 2–6 days and was improved within 5–32 days after diagnosis. Among the eight critical cases, remdesivir was administered in six cases. Steroids were provided for all cases. Inotropics were administered in one case. Six cases were treated with noninvasive mechanical ventilator and three required mechanical ventilator. One case required ECMO due to acute respiratory distress syndrome. All cases were admitted to the intensive care unit and admission period ranged from 9–39 days. Among all critical COVID-19 cases < 18 years of age, there were no fatal cases.
Conclusion
To develop appropriate policies for children in the COVID-19 pandemic, it is important to monitor and assess the clinical burden in this population.
Keywords: COVID-19, Child, Critical Care, Korea
Graphical Abstract
INTRODUCTION
The clinical spectrum of coronavirus disease 2019 (COVID-19) differs according to age groups and has been shown to be generally asymptomatic or mild in previously healthy children.1,2,3,4,5,6 However, severe cases may occur among children. According to data reported in the US, approximately 7.0% require hospitalization and among hospitalized cases 26.5–31.4% are admitted in intensive care units (ICUs), approximately 4.9–9.0% require mechanical ventilation and mortality is seen in 0.2–0.7% of cases.7,8,9 Among age groups in children, admission rates are highest in 0–4 years of age followed by 12–17 years and lowest among children 5–11 years of age,8 whereas mortality has been reported in younger (0–2 years) or older age groups (12–19 years).10
Risk factors for hospitalization in children have been identified as type 1 diabetes, obesity, cardiac and circulatory congenital anomalies and other chronic complex diseases.11,12,13 Prematurity is also a risk factor for children younger than 2 years and having multiple underlying diseases increase risk of severe infection.11 It is important to identify children with risk for severe COVID-19 for appropriate intervention.
As of October 7, 2021, 325,804 cases have been diagnosed with COVID-19 and 46,688 cases are ≤ 19 years of age in Korea. The proportion of children ≤ 19 years of age has been increasing gradually during the COVID-19 pandemic from 7.0% to 14.0%.14 According to the current policies in Korea, all patients diagnosed with COVID-19 are subject for hospitalization or mandatory isolation at residential treatment centers, regardless of patient's age or symptoms except for limited exceptions where homecare may be provided.15,16 Therefore, it is difficult to assess the true clinical burden of COVID-19 among children in Korea. However, critical cases are reported to the Central Disease Control Headquarters of the Korea Disease Control and Prevention Agency (KDCA). In this study, we report the clinical characteristics of children classified as critical COVID-19 in Korea to provide further insights into risk factors and management in children.
METHODS
Study population
This study included cases < 18 years of age diagnosed with COVID-19 and classified as critical during January 20, 2020 to October 7, 2021. Cases of COVID-19 were diagnosed by detecting SARS-CoV-2 RNA in nasopharyngeal and oropharyngeal swab or sputum by real-time reverse transcription-polymerase chain reaction (RT-PCR).6 Since the beginning of the COVID-19 pandemic, all COVID-19 cases have been reported daily to the Central Disease Control Headquarters of the KDCA and critical cases and mortality are reported according to age groups. The critical COVID-19 clinical case definition developed by the KDCA includes cases with severe illness requiring noninvasive (high flow nasal cannula, continuous positive airway pressure, or bilevel positive airway pressure) or invasive mechanical ventilation, extracorporeal membrane oxygenation (ECMO) or continuous renal replacement therapy (CRRT). Critical cases were identified by the surveillance system of the KDCA which includes the hospital, age and date of diagnosis for each case.
Data collection
Data was collected through a case report form developed for this study and filled out by physicians at each hospital. Data collected included age, sex, height, weight, underlying disease, date of diagnosis, exposure history, symptoms, laboratory test results, radiologic tests, treatment and outcome. Exposure history was based on the epidemiology report by the local government which is part of the public health response for all COVID-19 diagnosed cases.
Ethics statement
The study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (approval no. B-2110-714-108) and the Institutional Review Board at each hospital. Informed consent was waived for this study.
RESULTS
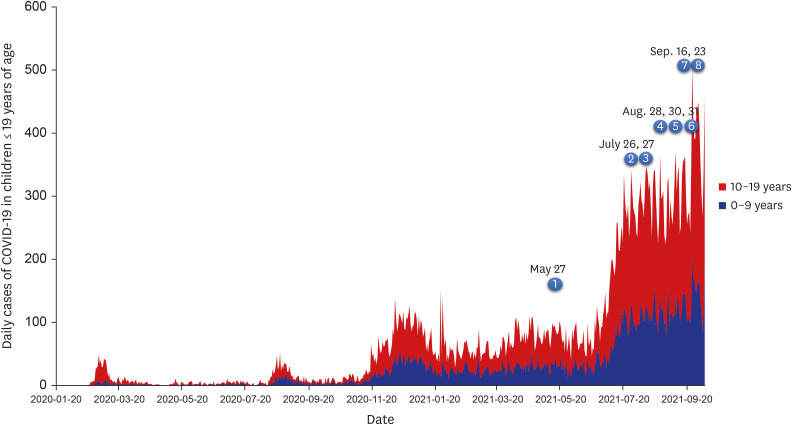
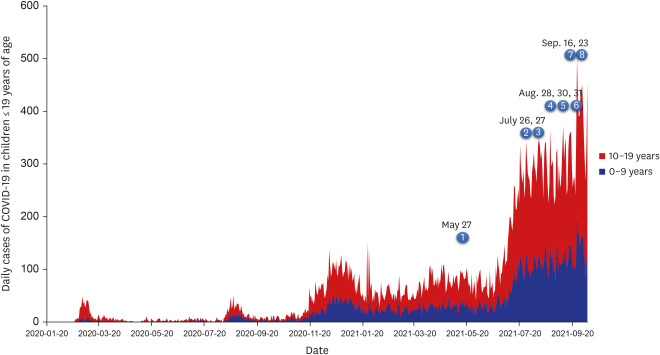
During January 20, 2020 to October 7, 2021 among 39,146 cases diagnosed with COVID-19 in subjects < 18 years of age, eight cases (0.02%) were identified as critical COVID-19 (Table 1, Fig. 1). The median age was 13 years (range 10 month-17 years) and male-to-female ratio was 1:1. Three children had underlying diseases; one child has asthma and major depressive disorder, one child had Lennox-Gastaut syndrome and one child had mental retardation and was newly diagnosed with type 2 diabetes mellitus with the diagnosis of COVID-19. Among the eight children, seven children were obese (body mass index [BMI] median 29.3 (range 26.4–38.2) > 95th percentile and Weight-for-Length > 97th percentile in infant) and one child was overweight (BMI 21.3 ≥ 90–95th percentile).17
Table 1. Demographics, clinical features, treatments and outcomes of children with critical COVID-19 in Korea.
| Characteristics | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | |
|---|---|---|---|---|---|---|---|---|---|
| Age, yr | 17 | 9 | 17 | 17 | 0.83 | 13 | 11 | 14 | |
| Sex | F | M | F | M | M | F | F | M | |
| BMI, kg/m2 (percentile for age) | 32.3 (> 95th percentile) | 21.3 (90–95th percentile) | 26.4 (> 95th percentile) | 38.2 (> 95th percentile) | 21.4 (WFL > 97th percentile) | 32.3 (> 95th percentile) | 25.9 (> 95th percentile) | 30.0 (> 95th percentile) | |
| Risk factors or underlying disease | Obesity, asthma, major depressive disorder | Lennox-Gastaut Syndrome | Obesity | Obesity | Obesity | Obesity, type 2 DM, mental retardation | Obesity | Obesity, fatty liver, prediabetic state | |
| Exposure history | Unknown | Family member (mother, father, sibling) | Family member (older brother) | Non-familial exposure | Family member (mother) | Family member (mother) | Unknown | Family member (father) | |
| Date of diagnosis | May 27, 2021 | July 26, 2021 | July 27, 2021 | August 28, 2021 | August 30, 2021 | August 31, 2021 | September 17, 2021 | September 23, 2021 | |
| Date of initial symptom | May 25, 2021 | July 28, 2021 | July 24, 2021 | August 27, 2021 | September 3, 2021 | August 30, 2021 | September 15, 2021 | September 21, 2021 | |
| Date classified as critical COVID-19 (days after diagnosis, after initial symptoms) | June 2, 2021 (6, 8) | July 28, 2021 (2, 1) | July 31, 2021 (4, 7) | September 4, 2021 (7, 8) | September 7, 2021 (8, 4) | September 9, 2021 (9, 10) | September 23, 2021 (5, 8) | September 30, 2021 (7, 9) | |
| Initial symptoms | Cough, headache, chills | Fever, seizure | Fever | Cough, myalgia | Dyspnea | Fever, headache, sore throat, sputum | Fever, cough, sore throat, chill | Cough, sputum, abdominal pain | |
| Clinical signs and symptoms | |||||||||
| Fever | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Fever peak, °C | 38.9 | 39.8 | 38.4 | 37.5 | 37.6 | 38.2 | 40.7 | 38.1 | |
| Fever duration, days | 8 | 12 | 5 | NA | 4 | 11 | 5 | 8 | |
| Cough | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | |
| Sputum | No | Yes | No | No | Yes | Yes | Yes | Yes | |
| Dyspnea | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | |
| Rhinorrhea | No | No | No | No | Yes | No | No | No | |
| Sore throat | Yes | No | Yes | No | No | Yes | Yes | No | |
| Myalgia | Yes | No | Yes | Yes | No | No | No | No | |
| Lethargy/Fatigue/Malaise | Yes | Yes | No | No | No | Yes | No | Yes | |
| Headache | Yes | No | No | No | No | Yes | No | Yes | |
| Abdominal pain | No | No | No | No | No | No | No | Yes | |
| Nausea/Vomit/Diarrhea | No | No | No | No | Yes (Diarrhea) | No | Yes (Diarrhea) | No | |
| Anosmia/Ageusia | No | No | No | No | No | No | No | No | |
| Seizure | No | Yes | No | No | No | No | No | No | |
| Lowest oxygen saturation, % | 85 | 56 | 88 | 81 | 90 | 88 | 88 | 85 | |
| Laboratory markersa | |||||||||
| Leukocyte (neutrophil %), /µL | 15,260 (89.6) | 17,490 (87.2) | 12,000 (87.2) | 15,300 (81.8) | 30,210 (63.0) | 11,700 (50.3) | 8,060 (70.6) | 13,750 (53.0) | |
| Platelet, 103/µL | 568 | 159 | 435 | 121 | 190 | 401 | 321 | 469 | |
| CRP, mg/dL | 9.7 | 13.5 | 3.39 | 8.98 | 2.23 | 8.27 | 1.82 | 3.46 | |
| Procalcitonin, ng/mL | 0.55 | 1.83 | 0.029 | 2.12 | NT | 0.05 | 0.49 | 0.31 | |
| D-dimer, µg/mL | 0.59 | 1.23 | 1.40 | 1.92 | NT | 1.53 | 0.77 | 0.76 | |
| AST/ALT, U/L | 206/544 | 194/97 | 23/29 | 206/133 | 35/17 | 98/64 | 47/70 | 388/304 | |
| Total bilirubin, mg/dL | 1.1 | 0.52 | 0.74 | 3.51 | NT | 1.05 | 0.37 | 0.73 | |
| BUN/Cr, mg/dL | 31/0.66 | 15/0.79 | 19.6/0.62 | 22/0.62 | 10.5/< 0.25 | 13/0.42 | 15.4/0.54 | 15/0.68 | |
| Glucose, mg/dL | 293 | 116 | 135 | 180 | 96 | 338 | 100 | 145 | |
| proBNP, pg/mL | NT | 226 | NT | 479.4 | NT | 679.1 | NT | 43.9 | |
| Microbiology | |||||||||
| Blood culture | Negative | Negative | Negative | Negative | NT | Negative | NT | Negative | |
| Respiratory virus PCR | NT | Rhinovirus | NT | NT | Negative | Negative | Negative | Negative | |
| Mycoplasma PCR | NT | Negative | NT | NT | NT | Negative | Negative | Negative | |
| Radiologic findings | |||||||||
| Chest X-ray (most severe), days after diagnosis | 8 | 8 | 6 | 9 | 12 | 8 | 5 | 9 | |
| Chest X-ray (most severe), days after symptom onset | 10 | 6 | 9 | 10 | 8 | 9 | 7 | 11 | |
| Improved chest X-ray, days after pneumonia diagnosis | 24 | 11 | 15 | 32 | 9 | 5 | 4 | 8 | |
| Chest CT | Yes | No | Yes | No | Yes | Yes | No | Yes | |
| Treatment | |||||||||
| Remdesivir | Yes | No | Yes | Yes | Nob | Yes | Yes | Yes (1 dose) | |
| Steroids | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Antibiotics | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | |
| Inotropics | No | Yes | No | No | No | No | No | No | |
| CRRT | No | No | No | No | No | No | No | No | |
| Noninvasive mechanical ventilator | Yes | No | Yes | No | Yes | Yes | Yes | Yes | |
| Mechanical ventilator | Yes | Yes | No | Yes | No | No | No | No | |
| ECMO | No | No | No | Yes | No | No | No | No | |
| Outcome | |||||||||
| ICU admission | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | |
| Hospitalization, days | 24 | 20 | 25 | 39 | 15 | 9 | 12 | 13 | |
| Discharge | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
Critical COVID-19 clinical case definition includes cases with severe illness requiring noninvasive (high flow nasal cannula, continuous positive airway pressure, or bilevel positive airway pressure) or invasive mechanical ventilation, ECMO or CRRT.
COVID-19 = coronavirus disease 2019, F = female, M = male, BMI = body mass index, WFL = weight-for-length, DM = diabetes mellitus, CRP = C-reactive protein, NT = not tested, AST = aspartate aminotransferase, ALT = alanine aminotransferase, BUN = blood urea nitrogen, PCR = polymerase chain reaction, CT = computed tomography, CRRT = continuous renal replacement, ECMO = extracorporeal membrane oxygenation therapy, ICU = intensive care unit.
aLaboratory markers show highest or lowest value, bIntravenous gamma globulin was administered.
Fig. 1. Daily number of COVID-19 cases among children 0–19 years of age, South Korea, January 20th, 2020–October 7th, 2021. The occurrences of the 8 cases of critical COVID-19 cases and date of diagnosis are indicated.
COVID-19 = coronavirus disease 2019.
The onset from initial symptoms to critical COVID-19 ranged from 7–10 days except the case with Lennox-Gastaut syndrome who was rapidly deteriorated on the day of symptom onset with seizure recurred. All patients experienced fever ≥ 37.5°C and seven patients showed prolonged fever from 4–12 days. All subjects had cough, seven patients had dyspnea, other accompanied symptoms included sore throat, headache, lethargy, myalgia and diarrhea. Lowest oxygen saturation ranged from 56% to 88%.
Laboratory findings showed mild to moderate leukocytosis (range 8,060–17,490/μL) and CRP was elevated. Six cases showed elevated hepatic enzymes Among the five cases who received respiratory virus PCR, one case was co-infected with rhinovirus and among cases who were tested for Mycoplasma pneumoniae there was no evidence of infection.
Radiologic findings showed pneumonia within 1–8 days after symptom onset. Pneumonia progressed in these children for 2–6 days and was improved within 5–32 days after diagnosis.
Among the eight critical cases, remdesivir was administered in six cases, however one case was discontinued due to high liver enzymes. Steroids were provided for all cases and antibiotics in seven cases. Inotropics were administered for one case. Among the eight critical cases, six cases were treated with noninvasive mechanical ventilator (high flow nasal cannula) and three cases required mechanical ventilator (one case used both high flow nasal cannula and invasive mechanical ventilator). One case required ECMO due to acute respiratory distress syndrome. Seven cases were admitted to the ICU and admission period ranged from 8–32 days. Among all critical COVID-19 cases < 18 years of age, there were no fatal cases.
DISCUSSION
In this study we analyzed the clinical manifestations of cases with critical COVID-19 among children < 18 years of age. During January 20, 2020 to October 7, 2021, 39,146 cases among < 18 years of age were diagnosed with COVID-19. Of these cases, eight were of critical COVID-19 which accounts for 0.02% and there has been no mortality in this age group. The proportion of critical COVID-19 in children ≤ 19 years of age ranges from 0.0–0.27% daily up to October 7, 2021. Although COVID-19 may be a mild infection in most children, a small proportion develop severe illness requiring ICU care and may lead to fatal outcomes.18,19 In this study, the first critical case occurred in May, 2021 and seven of the eight critical cases occurred since late July, 2021, after the B.1.617.2 (Delta) variant became predominant. This is more likely due to the increase of cases in children in relation to the high transmission of the SARS-CoV-2 delta variant, rather than increase in severity.8 According to a study which compared COVID-19 and influenza in children in countries such as Europe, the US, and South Korea, COVID-19 showed low fatality however complications including hospitalization, hypoxemia, and pneumonia were more frequent in COVID-19 than with influenza.20 Therefore, it is important to identify children with high risk and those progressing in illness.
Children with underlying diseases show higher risk for severe manifestations of COVID-19.9,10,11,12,13,19,21 Recent studies in children have identified type 1 diabetes, obesity, cardiac and circulatory congenital anomalies, epilepsy and convulsions, neurodevelopmental disorders, type 2 diabetes, other chronic complex diseases and prematurity in children < 2 years as high risk of need for hospitalization or severe COVID-19.11,12,13 Among various risk factors, diabetes mellitus is identified as a high risk for hospitalization and severe COVID-19. Potential mechanisms on the association of diabetes mellitus and severe COVID-19 include effects of impaired glucose homeostasis, inflammation, altered immune status and activation of the renin–angiotensin–aldosterone system and cardiovascular and renal complications of diabetes mellitus.22,23 Among the seven critical COVID-19 cases in this study, six were obese and one case was overweight. Obesity has been acknowledged as an important risk factor for severe COVID-19 in both adults and children.24,25 Proposed mechanisms include dysregulation of the immune system in relation to cytokine and adipokine secretion from adipose tissues which leads to a pro-inflammatory state in obese patients, predisposing thrombosis, alterations of innate and adaptive immune responses and cytokine storm.26 Impaired lung function has been demonstrated in obese subjects in relation with chest wall physiology such as reduced chest wall elasticity, low respiratory muscle strength and increased airway resistance.26,27,28,29 Obesity is also associated with various comorbidities including hypertension, cardiovascular disease and diabetes mellitus.26
Treatment guidelines for COVID-19 are continuously evolving during the pandemic. Although no treatment other than supportive care is necessary for a great majority of children with COVID-19, antiviral therapy, steroids or other immunomodulatory treatment may need to be considered in severe or critical disease.30 Early in the COVID-19 pandemic hydroxychloroquine and lopinavir-ritonavir had been proposed as therapeutic options, however later studies have shown ineffectiveness of these medication and these medications are currently no recommended.31,32,33,34,35,36
Decisions for treatment should be based on severity categories which can be extrapolated from clinical trials (Table 2).30 Remdesivir, a nucleoside analog prodrug that binds to viral RNA polymerase resulting in premature RNA chain termination may be used in COVID-19.37 Remdesivir is authorized for use in patients who require supplemental oxygen, invasive or noninvasive mechanical ventilation, or ECMO.30 Clinical trials demonstrated that patients treated with remdesivir had median time to recovery of 10 days compared with 15 days in the placebo group.38 Treatment duration is recommended up to 5 days for children with severe COVID-19 and among critical cases not improving after 5 days of treatment durations up to 10 days may be considered.30 Reported adverse effects of remdesivir include nausea, vomiting, and transaminase elevations and in a study of compassionate use in children, remdesivir was well tolerated, with a low incidence of serious adverse events.39
Table 2. Suggested use of antiviral agents in coronavirus disease 2019 by illness severity.
| Disease category | Respiratory support requirement | Management |
|---|---|---|
| Mild | No new or increased supplemental oxygen requirement, with symptoms limited to the upper respiratory tract | Supportive care |
| Moderate | No new or increased supplemental oxygen requirement, with symptoms involving the lower respiratory tract, or radiographic findings on chest X-ray | Supportive care |
| Severe | New or increase from baseline supplemental oxygen requirement without need for new or increase in baseline noninvasive/invasive mechanical ventilation | Remdesivir is suggested for all children with severe COVID-19, unless there are contraindications |
| Critical | New or increase requirement for invasive or noninvasive mechanical ventilation, sepsis, or multiorgan failure OR rapidly worsening clinical trajectory that does not yet meet these criteria | Remdesivir is suggested for all children with critical COVID-19, unless there are contraindications |
Noninvasive mechanical ventilation includes high-flow nasal canula, continuous positive airway pressure, or bilevel positive airway pressure.
COVID-19 = coronavirus disease 2019.
Adapted from “Multicenter Interim Guidance on Use of Antivirals for Children With Coronavirus Disease 2019/Severe Acute Respiratory Syndrome Coronavirus 2”, by Chiotos et al. J Pediatr Infect Dis Soc 2021;10(1):34-48. Copyright 2021 by Oxford University Press. Reprinted with permission.
Corticosteroids may be considered in severe or critical COVID-19.34,40 Based on results in adults, corticosteroids may be considered in children with severe or critical COVID-19, however are not routinely recommended for children who require only low levels of oxygen support (i.e., administered via a nasal cannula only) and use in severe COVID-19 in profoundly immunocompromised subjects should be considered on a case-by-case basis.34 Other therapeutics include baricitinib with dexamethasone or tocilizumab with dexamethasone for control of inflammation in adults.35 The FDA has issued emergency use for these medications for patients ≥ 2 years of age hospitalized with COVID-19 and require oxygen or ventilatory support, or ECMO, however there is limited information about the benefits and risks in children.
Another consideration in treatment of severe or critical COVID-19 is prophylaxis and treatment of COVID-19 related venous thromboembolism (VTE). COVID-19 has been associated with high rates of thrombo-embolic complications, thus thromboprophylaxis is recommended in hospitalized patients.35 However for children, the risk is not well assessed, thus indications for VTE prophylaxis are currently same as those in children without COVID-19.35
With the short history of COVID-19, various potential medications are under study and treatment guidelines will evolve. Continuous monitoring on the efficacy and safety of treatment in severe and critical COVID-19 will be needed. This study has limitations as only critical COVID-19 cases were included and severe cases such as those with supplemental oxygen requirement without need for noninvasive or invasive mechanical ventilation were not included in this study. For developing policies for children in the COVID-19 pandemic, it is important to monitor and assess the clinical burden and the risk-benefit for children.
ACKNOWLEDGMENTS
The authors thank the staff at each hospital for their dedication and efforts in treating these critical COVID-19 cases in children and the members of the epidemiological investigation analysis of the Korean Disease Control and Prevention Agency for all their support during the ongoing COVID-19 pandemic.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Lee H.
- Data curation: Lee H, Choi SH, Park JY, Jo DS, Choi UY, Jung YT, Jung IH, Kim JY.
- Formal analysis: Lee H.
- Investigation: Lee H, Choi EH.
- Methodology: Choe YJ.
- Validation: Park YJ.
- Writing - original draft: Lee H.
- Writing - review & editing: Lee H, Choi EH.
References
- 1.Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109(6):1088–1095. doi: 10.1111/apa.15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mansourian M, Ghandi Y, Habibi D, Mehrabi S. COVID-19 infection in children: a systematic review and meta-analysis of clinical features and laboratory findings. Arch Pediatr. 2021;28(3):242–248. doi: 10.1016/j.arcped.2020.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taheri L, Gheiasi SF, Taher M, Basirinezhad MH, Shaikh ZA, Dehghan Nayeri N. Clinical features of COVID-19 in newborns, infants, and children: a systematic review and meta-analysis. Compr Child Adolesc Nurs. 2021 doi: 10.1080/24694193.2021.1930288. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 4.Viner RM, Ward JL, Hudson LD, Ashe M, Patel SV, Hargreaves D, et al. Systematic review of reviews of symptoms and signs of COVID-19 in children and adolescents. Arch Dis Child. 2021;106(8):802–807. doi: 10.1136/archdischild-2020-320972. [DOI] [PubMed] [Google Scholar]
- 5.Shoji K, Akiyama T, Tsuzuki S, Matsunaga N, Asai Y, Suzuki S, et al. Clinical characteristics of hospitalized COVID-19 in children: report from the COVID-19 registry in Japan. J Pediatric Infect Dis Soc. 2021 doi: 10.1093/jpids/piab085. Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Han MS, Choi EH, Chang SH, Jin BL, Lee EJ, Kim BN, et al. Clinical Characteristics and viral RNA detection in children with coronavirus disease 2019 in the Republic of Korea. JAMA Pediatr. 2021;175(1):73–80. doi: 10.1001/jamapediatrics.2020.3988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bailey LC, Razzaghi H, Burrows EK, Bunnell HT, Camacho PE, Christakis DA, et al. Assessment of 135 794 pediatric patients tested for severe acute respiratory syndrome coronavirus 2 across the United States. JAMA Pediatr. 2021;175(2):176–184. doi: 10.1001/jamapediatrics.2020.5052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Delahoy MJ, Ujamaa D, Whitaker M, O’Halloran A, Anglin O, Burns E, et al. Hospitalizations associated with COVID-19 among children and adolescents - COVID-NET, 14 states, March 1, 2020-August 14, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(36):1255–1260. doi: 10.15585/mmwr.mm7036e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Havers FP, Whitaker M, Self JL, Chai SJ, Kirley PD, Alden NB, et al. Hospitalization of adolescents aged 12–17 years with laboratory-confirmed COVID-19 - COVID-NET, 14 states, March 1, 2020-April 24, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(23):851–857. doi: 10.15585/mmwr.mm7023e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCormick DW, Richardson LC, Young PR, Viens LJ, Gould CV, Kimball A, et al. Deaths in children and adolescents associated with COVID-19 and MIS-C in the United States. Pediatrics. 2021;148(5):e2021052273. doi: 10.1542/peds.2021-052273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kompaniyets L, Agathis NT, Nelson JM, Preston LE, Ko JY, Belay B, et al. Underlying medical conditions associated with severe COVID-19 illness among children. JAMA Netw Open. 2021;4(6):e2111182. doi: 10.1001/jamanetworkopen.2021.11182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tsankov BK, Allaire JM, Irvine MA, Lopez AA, Sauvé LJ, Vallance BA, et al. Severe COVID-19 infection and pediatric comorbidities: a systematic review and meta-analysis. Int J Infect Dis. 2021;103:246–256. doi: 10.1016/j.ijid.2020.11.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bellino S, Punzo O, Rota MC, Del Manso M, Urdiales AM, Andrianou X, et al. COVID-19 disease severity risk factors for pediatric patients in Italy. Pediatrics. 2020;146(4):e2020009399. doi: 10.1542/peds.2020-009399. [DOI] [PubMed] [Google Scholar]
- 14.Yoon Y, Kim KR, Park H, Kim S, Kim YJ. Stepwise school opening and an impact on the epidemiology of COVID-19 in the children. J Korean Med Sci. 2020;35(46):e414. doi: 10.3346/jkms.2020.35.e414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yun KW, Kim KM, Kim YK, Kim MS, Kwon H, Han MS, et al. Limited benefit of facility isolation and the rationale for home care in children with mild COVID-19. J Korean Med Sci. 2021;36(5):e45. doi: 10.3346/jkms.2021.36.e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee Y, Han JO, Lee H, Lim S. The development and operation of a home management system during the COVID-19 pandemic: experience of the local government Gyeonggi-do in Korea. J Korean Med Sci. 2021;36(19):e134. doi: 10.3346/jkms.2021.36.e134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yi DY, Kim SC, Lee JH, Lee EH, Kim JY, Kim YJ, et al. Clinical practice guideline for the diagnosis and treatment of pediatric obesity: recommendations from the Committee on Pediatric Obesity of the Korean Society of Pediatric Gastroenterology Hepatology and Nutrition. Korean J Pediatr. 2019;62(1):3–21. doi: 10.3345/kjp.2018.07360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chao JY, Derespina KR, Herold BC, Goldman DL, Aldrich M, Weingarten J, et al. Clinical characteristics and outcomes of hospitalized and critically ill children and adolescents with coronavirus disease 2019 at a tertiary care medical center in New York City. J Pediatr. 2020;223:14–19.e2. doi: 10.1016/j.jpeds.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Götzinger F, Santiago-García B, Noguera-Julián A, Lanaspa M, Lancella L, Calò Carducci FI, et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health. 2020;4(9):653–661. doi: 10.1016/S2352-4642(20)30177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Duarte-Salles T, Vizcaya D, Pistillo A, Casajust P, Sena AG, Lai LY, et al. Thirty-day outcomes of children and adolescents with COVID-19: an international experience. Pediatrics. 2021;148(3):e2020042929. doi: 10.1542/peds.2020-042929. [DOI] [PubMed] [Google Scholar]
- 21.Oliveira EA, Colosimo EA, Simões E Silva AC, Mak RH, Martelli DB, Silva LR, et al. Clinical characteristics and risk factors for death among hospitalised children and adolescents with COVID-19 in Brazil: an analysis of a nationwide database. Lancet Child Adolesc Health. 2021;5(8):559–568. doi: 10.1016/S2352-4642(21)00134-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lim S, Bae JH, Kwon HS, Nauck MA. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol. 2021;17(1):11–30. doi: 10.1038/s41574-020-00435-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Holman N, Knighton P, Kar P, O’Keefe J, Curley M, Weaver A, et al. Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study. Lancet Diabetes Endocrinol. 2020;8(10):823–833. doi: 10.1016/S2213-8587(20)30271-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kompaniyets L, Goodman AB, Belay B, Freedman DS, Sucosky MS, Lange SJ, et al. Body mass index and risk for COVID-19-related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death - United States, March-December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(10):355–361. doi: 10.15585/mmwr.mm7010e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Popkin BM, Du S, Green WD, Beck MA, Algaith T, Herbst CH, et al. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes Rev. 2020;21(11):e13128. doi: 10.1111/obr.13128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aghili SM, Ebrahimpur M, Arjmand B, Shadman Z, Pejman Sani M, Qorbani M, et al. Obesity in COVID-19 era, implications for mechanisms, comorbidities, and prognosis: a review and meta-analysis. Int J Obes. 2021;45(5):998–1016. doi: 10.1038/s41366-021-00776-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dixon AE, Peters U. The effect of obesity on lung function. Expert Rev Respir Med. 2018;12(9):755–767. doi: 10.1080/17476348.2018.1506331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mahadev S, Salome CM, Berend N, King GG. The effect of low lung volume on airway function in obesity. Respir Physiol Neurobiol. 2013;188(2):192–199. doi: 10.1016/j.resp.2013.05.021. [DOI] [PubMed] [Google Scholar]
- 29.Spathopoulos D, Paraskakis E, Trypsianis G, Tsalkidis A, Arvanitidou V, Emporiadou M, et al. The effect of obesity on pulmonary lung function of school aged children in Greece. Pediatr Pulmonol. 2009;44(3):273–280. doi: 10.1002/ppul.20995. [DOI] [PubMed] [Google Scholar]
- 30.Chiotos K, Hayes M, Kimberlin DW, Jones SB, James SH, Pinninti SG, et al. Multicenter interim guidance on use of antivirals for children with coronavirus disease 2019/severe acute respiratory syndrome coronavirus 2. J Pediatric Infect Dis Soc. 2021;10(1):34–48. doi: 10.1093/jpids/piaa115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tang W, Cao Z, Han M, Wang Z, Chen J, Sun W, et al. Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: open label, randomised controlled trial. BMJ. 2020;369:m1849. doi: 10.1136/bmj.m1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Horby P, Mafham M, Linsell L, Bell JL, Staplin N, Emberson JR, et al. Effect of hydroxychloroquine in hospitalized patients with Covid-19. N Engl J Med. 2020;383(21):2030–2040. doi: 10.1056/NEJMoa2022926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, et al. A trial of lopinavir-ritonavir in adults hospitalized with severe Covid-19. N Engl J Med. 2020;382(19):1787–1799. doi: 10.1056/NEJMoa2001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bhimraj AM, Shumaker AH, Lavergne V, Baden L, Cheng VC, Edwards KM, et al. Infectious Diseases Society of America Guidelines on the treatment and management of patients with COVID-19. Clin Infect Dis. 2021 doi: 10.1093/cid/ciaa478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.NIH. Coronavirus disease 2019 (COVID-19) Treatment guidelines 2021. [Updated 2021]. [Accessed September 15, 2021]. https://www.covid19treatmentguidelines.nih.gov/
- 36.FDA. Coronavirus (COVID-19) update: FDA revokes emergency use authorization for chloroquine and hydroxychloroquine. [Updated 2020]. [Accessed September 15, 2021]. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-revokes-emergency-use-authorization-chloroquine-and .
- 37.Yin W, Mao C, Luan X, Shen DD, Shen Q, Su H, et al. Structural basis for inhibition of the RNA-dependent RNA polymerase from SARS-CoV-2 by remdesivir. Science. 2020;368(6498):1499–1504. doi: 10.1126/science.abc1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, et al. Remdesivir for the treatment of Covid-19 - final report. N Engl J Med. 2020;383(19):1813–1826. doi: 10.1056/NEJMoa2007764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Goldman DL, Aldrich ML, Hagmann SH, Bamford A, Camacho-Gonzalez A, Lapadula G, et al. Compassionate use of remdesivir in children with severe COVID-19. Pediatrics. 2021;147(5):e2020047803. doi: 10.1542/peds.2020-047803. [DOI] [PubMed] [Google Scholar]
- 40.Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384(8):693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]