Abstract
Background. The COVID-19 epidemic has resulted in a massive surge in the need for intensive care unit (ICU) care. To avoid being overwhelmed, hospitals had to adapt and support the ICU teams in structured ICU care including involving surgical teams. This work aims at describing the collaborative efforts between the ICU care team and the Surgical Task Force (STF) during a surge of ICU activity in a University Hospital in a French high-density COVID-19 cluster. Study Design. This retrospective single center study analyzed the STF workflow and the ICU population. The study included 55 patients hospitalized in our ICU, ICU-converted step-down units, and post-anesthesia care units. The primary measure was the global daily STF activity. The secondary measure was the daily activity for each of the 5 tasks accomplished by the STF. Results. The STF attempted 415 phone calls for 55 patients’ families, 237 mobilizations of patients requiring prone positions, follow-up of 20 patients requiring medevac, and contribution to ethical discussion for 2 patients. The mean (SD) daily number of successful phones calls, ethical discussions, mobilizations of patients requiring prone positions and medevac follow-up were 18 (7), .1 (.4), 10 (7), and 2 (3), respectively. No actions for discharge summaries writing were required. The maximum number of daily mobilizations for patients requiring prone positions was 25. The maximum number of daily attempted phone calls and successful phone calls were 37 and 26, respectively. Conclusion. Surgeons’ technical and nontechnical skills represented an effective support for ICU teams during the COVID-19 pandemic.
Keywords: COVID-19, surgical technical skills, surgical non-technical skills, intensive care unit
Introduction
Since December 2019, a worldwide outbreak of the coronavirus 2 (SARS-CoV-2) infections has led to a pandemic.1-5 The clinical symptoms, dominated with respiratory impairment, were labelled coronavirus disease 2019 (COVID-19) by the World Health Organization.6,7 The spread of COVID-19 has led to a massive surge of severely ill patients in intensive care units (ICUs).8-10 Hospitals had to rapidly prepare and adapt to the abrupt increase in the need for ICU beds without simultaneous and proportionate increase in available resources.11,12 In France, Grand EST region, was a high-density COVID-19 cluster since March 2020.13 In response, Strasbourg University Hospital, Strasbourg, France, rapidly increased ICU bed availability by converting postoperative care units (PACU) and step-down unit into high-dependency ICUs. However, there was a shortage of physicians to support the ICU team. Because performance of nonurgent surgery was severely curtailed, and only urgent and emergent procedures were allowed,12 surgical volume was significantly reduced. Surgeons represented a precious medical resource readily available to reinforce COVID-19 care, which prompted development of a Surgical Task Force (STF).
In this study, we aim at reporting the setup of a STF in one of the Strasbourg University Hospitals to reinforce ICU patient care. We also present the feasibility and efficiency of this COVID-19 STF.
Methods
The study design and report aim at fulfilling the Strengthening the Reporting of the Observational Studies in Epidemiology statement.14 Under French regulatory Law, as this study was considered as observational research on routine clinical data, the need for informed consent was waived, and confirmed by the Institutional Review Board approval (approval #IRB00010254-2020-064, French Society of Anesthesiology Review Board, Chairman Pr Jean-Etienne Bazin).
Study Design, Population, and Setting
This retrospective cohort study was performed at the Hautepierre Hospital, which is one of the Strasbourg University Hospitals, Strasbourg, France. Strasbourg University Hospitals were involved in the regional strategy to face a high-density COVID-19 cluster situation since the beginning of March 2020. The Department of Anesthesiology and Intensive Care usually runs 18 ICU beds. To face the epidemic requirements, 4 PACUs and a step down unit were modified to high-dependency ICUs (Supplemental Figure 1). A total of 59 ICU beds were made available within a week. Theses ICUs were staffed with Anesthesiology & Intensive care physicians and nurses. Because of a rapid increase in occupancy, ICU patients had to be transferred (medevac) by car, air, and train to other French locations or foreign countries, which overwhelmed physicians and nurses. Furthermore, family–patient visits were strictly restricted, which also overwhelmed the ICU staff.
STF Setup
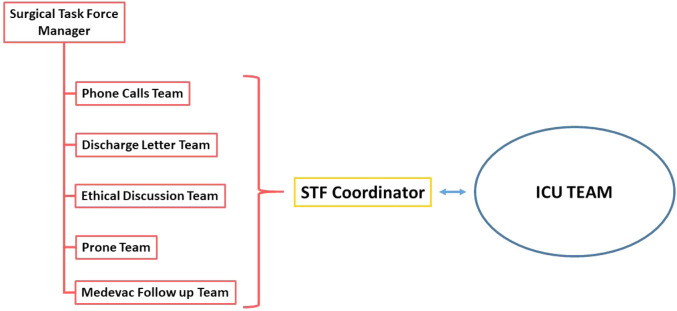
As the ICU admission rate was rapidly increased, surgeons and radiologists of the hospital were structured into a STF with an aim to assist with multiple ICU staff requests including help with making phone calls to family members, assistance with writing discharge summaries, participation in multidisciplinary ethical discussions, assisting with prone positioning, and follow-up of medevac patients (Figure 1). Surgeon volunteers were allocated to each of these tasks on a daily basis except for making daily phone calls to family members which were allocated weekly. Older surgeons or surgeons with chronic illnesses were less likely to be affected to the prone team to avoid direct contact with infected patients The STF was managed by a senior surgeon who established the team planning, gathered activity status, centralized communication request with ICU staff and adjusted STF procedures as necessary. An ICU nurse, acting as STF coordinator, was dedicated to assist and coordinate with STF (eg, communicate medical information obtained from the family members to the ICU staff). The participants of the STF were encouraged to undergo learning sessions on specific COVID-19 ICU institutional personal protection procedures. Personal protective equipment used by the STF included head cover, protective glasses, filtering face piece class 2 face masques, disposable fluid-resistant gown and gloves (Supplemental Figure 2).
Figure 1.
Surgical Task Force design. Note. ICU = intensive care unit.
In an effort to improve interoperator communication quality, a standard operating procedure and checklist were established for communication with family members.
Clinical Data collection
Patient files who were hospitalized from March 23, 2020 to April 16, 2020, in specialized COVID ICU were screened. Inpatient data were obtained from the institutional electronic and paper health record. The daily STF workflow that was centralized by the STF coordinator was also analyzed. Epidemiological data concerning the daily regional number of ICU-hospitalized patients for the Moselle, Bas-Rhin, and Haut-Rhin counties, were extracted from the open-access French National authority database: Santé Publique France.15
Demographic patient data collected included age, gender, ICU location, and familial status of the patient contact. Data collected regarding the tasks performed by STF included daily activity reports of the numbers and duration of family phone calls, and the topics discussed during the calls.
Statistical Analysis
Data are described using frequency and proportion (n, %) for categorical variables and mean (standard deviation) for quantitative data. Computations were made using GraphPad© Prism 8.4.2. As the study’s primary objective is descriptive, the sample size was not calculated. We choose the sample size that reflects the consecutives actions of the STF during the study period.
Results
The maximal number of ICU patients hospitalized in the Moselle, Bas-Rhin, and Haut-Rhin area was reached on April 3rd with 614 patients.
During the study period, 90 surgeons including 36 residents and remaining consultants were involved in the STF. The surgical specialty included orthopedic, trauma, gastrointestinal, interventional radiology, pediatric, neurosurgery, plastic and maxillofacial surgery. The mean daily number of participants to the STF were 17 (7).
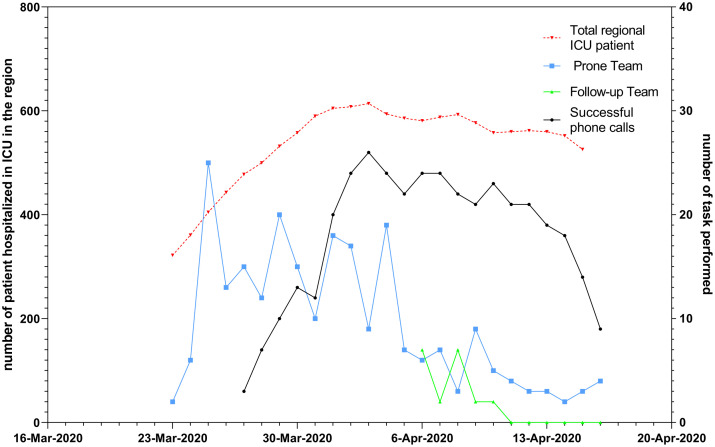
During the study period, the STF attempted and succeeded in 415 and 378 phone calls, respectively, for 55 patients’ families, performed 237 mobilizations of patients requiring prone positions, follow-up of 20 patients requiring medevac, and participated in ethical discussions for 2 patients. The daily workflow is represented in Figure 2. The mean daily number of successful phones calls, ethical discussions, mobilization of patients requiring prone position and medevac follow-up were 18 (7), .1 (.4), 10 (7), and 2 (3), respectively. No actions for discharge summaries were required. The maximum number of daily mobilizations for patient requiring prone position was 25. The maximum number of attempts and successful phone call attempts were 37 and 26, respectively. The characteristics of the STF phones calls are reported in Table 1. The most frequent topics of discussions were related to technical care (64%), patient comfort (56%), and patient evolution expectations (47%).
Figure 2.
Daily workflow of the Surgical Task Force. Note. Daily workflow of the Hautpierre Hospital Surgical Task Force (right Y-axis) for the prone team (squares), phone call team (circles), and Follow-up Team (continuous line with triangles). The left axis represent daily number of ICU patient (doted line with triangles) in the surrouding areas (Moselle, Bas-Rhin and Haut-Rhin counties).
Table 1:
Characteristics of the STF Phone Calls.
| STF Phone Calls | |
|---|---|
| Patients, n | 55 |
| Age, years, mean (SD) | 62 (12) |
| Phone call attempts, n | 415 |
| Successful phone calls, n (%) | 378/415 (91) |
| Topic of discussion | |
| Technical care, % | 64 |
| Patient comfort, % | 56 |
| Expected progress/outcomes, % | 47 |
| Planned exams, % | 12 |
| Medical clarifications, % | 34 |
| Requests for additional discussion with ICU physicians, % | 13 |
| Requests to thank the ICU team, % | 23 |
Abbreviations: SD = standard deviation; % = percentage; n = number; STF = Surgical Task Force; ICU = intensive care unit.
Discussion
This study shows that the STF was effective to support ICU staff. We observed high workflow for two of the STF tasks. First, the phone calls to family members were increasingly effective. Contribution to patient/family information is an important feature of medical practice particularly in these unprecedented times and for critically ill patients. This communication aims at involving family members in clinical decision-making, minimize psychological distress, and improve family satisfaction.16,17 Surgeons are highly skilled in communication with patients and their family members because of their experience with shared decision-making process that has become a standard of care for usual surgical planning.18 They also have significant background knowledge on the ICU environment and patient pathway.
The daily phone calls by the ICU physician to the patient family were aimed toward alleviating psychological distress amongst family members. The most frequent topics of discussion during these phone calls included questions about technical care and patient comfort. These questions are usually addressed during the family’s ICU visit; however, these visits were prevented during the COVID pandemic. Initial report confirmed that the COVID-19 epidemic induced high prevalence of psychological distress among the population.19,20 A online survey of 1210 patients during the epidemic in China, found that 54% of respondents rated the psychological impact as moderate to severe, with as significant proportion reporting moderate or severe depression (17%) or anxiety (29%) symptoms.19 In addition, 75% of the respondents were “very worried” or “somewhat worried” about other family members contracting COVID-19.19 Additional stress may be induced by lack of contact with their relatives in the ICU or lack of information from staff.
The second STF task with high workflow was acting as a “prone team.” As per international acute respiratory distress syndrome (ARDS) recommendations,21-23 prone position is an important therapeutic feature for severe ARDS patients. However, prone positioning can be a challenging and resource consuming technical skill. Although there are specialized beds that can facilitate prone positioning, that was not possible with the extended ICU beds. Surgeons are highly skilled with this prone positioning required for some surgical procedures. Given that the STF performed up to 25 daily interventions for prone positioning, it is clear that they provided a critical support for the ICU team facing surge in severe COVID-19 patients’ admissions.
Some of the STF missions presented lower workflow. For example, the assistance with writing discharge summaries was not required, probably because ICU physicians preferred to write them due to complexity of transmitting all the required medical information concerning such a complex medical condition. The STF participation to ethical discussions was also rarely activated. This may probably be explained by the numerous ICU specialized staff available to conduct such discussions.
Our study has several limitations. First, this study only involved 1 center, thus reducing the generalizability of our results. However, technical and nontechnical skills of surgeons are universal worldwide. Second, some underreporting of the daily activities may have occurred; however, the STF manger and coordinators tried to minimize such underreporting by performing routine task reports as part of their daily activities.
Our study has several strengths. First, as we used structured phone call report, extraction bias was reduced. Second, our study involved data collection during and after the peak ICU admissions, which allowed comparison of workflow tasks at different time points in the COVID-19 cycle. For example, after ICU admissions peaked, the need for the prone team decreased, whereas the need to make phone calls remained high. This can be explained as the clinical requirements of severe COVID-19 patients resolve earlier (eg, need for prone position) than the need for family information which remains as long as the patient is in the ICU. Surgical department strategies to help hospitals facing COVID-19 epidemic have been reported.24 Our result confirms that surgical departments may have a major role in supporting ICU adaptation to the COVID-19 epidemic.
Conclusion
The STF support to our ICU team facing a massive surge in severe COVID-19 cases was feasible and efficient. The high workflow observed for providing family phone calls and prone positioning reflects the critical utility of some surgical technical and nontechnical skills during the COVID-19 outbreak.
Supplemental Material
Supplemental Material, Supplemental_Material for Surgical Support for Severe COVID-19 Patients: A Retrospective Cohort Study in a French High-Density COVID-19 Cluster by Eric Noll, Christophe Muccioli, Pierre-Olivier Ludes, Julien Pottecher, Pierre Diemunsch, Sophie Diemunsch, Anaëlle Tchentcheli, Philippe Clavert, Girish P. Joshi and Philippe A. Liverneaux in Surgical Innovation
Acknowledgments
The author would like to thank all the surgeons involved in the STF: Adam Philippe, Al-Ansari Rawan, Antoni Maxime, Assouline Shoshana, Auque Anna, Baldairon Florent, Baltassat Antoine, Barthel Louis, Bensa Marie, Bodin Fréderic, Boeri Cyril, Bonnomet Francois, Brinkert David, Bruant Catherine, Byfili Younes, Charles Yann-Philippe, Charton Jeanne, Chilintseva Natalia, Collinet Arnaud, Coman Alexandre, Coudray Alice, De Mathelin Pierre, Debry Christian, Delhorme Jean Baptiste, Di Marco Antonio, Dissaux Caroline, Ducournau Francois, Ehlinger Matthieu, Eichler David, Etourneau Pierre, Facca Sybille, Faitot Francois, Furioli Edouard, Gabriel Charlotte, Gagnard Yohan, Gaudet Camille, Giordano Nicolas, Gisonni Vincent, Gouzou Stéphanie, Grigoras Eduard Florentin, Gross Christiane, Hargat Julie, Henry Guillaume, Hollard Kissel Fréderic, Honecker Sophie, Jenny Jean-Yves, Kempf Jean-François, Kock Arne, Kuster Camille, Lazarus Priscille, Lucidarme Quentin, Lutz Jean-Christophe, Manier Ianis, Mathiot Adeline, Mereb Thomas, Mesli Yannis, Moliere Sébastien, Monsch Edgar, Moog Raphael, Ndedi Penda Didier Xavier, Nibbio Alice, Nicolau Xavier, Niglis Lucas, Ntilikina Yves, Paul Chloé, Petry Arnaud, Pierret Marie, Plesa-Furda Roxana, Proust Francois, Puliero Benjamin, Robert Emeric, Romain Benoit, Ruffenach Laetitia, Saur Maurise, Sauvinet Guillaume, Schenck Benoit, Schott Xavier, Schroeder Alice, Seynaeve Philippe, Simeu Blandine, Steib Jean-Paul, Talon Isabelle, Thery Charles, Thomas Maxence, Tomos Georgios, Virbel Guillaume, Voisinet Marlène, and Zink Simone. The authors would like to thank all the participants of the Surgical Task Force.
Author Contributions
Eric Noll, Christophe Muccioli, Julien Pottecher, Anaelle Tchentcheli, Pierre Diemunsch, and Philippe Liverneaux helped with study design, data collection, data analysis, and manuscript drafting. Pierre-Olivier Ludes, Sophie Diemunsch, Philippe Clavert, and Girish Joshi helped with data analysis and article editing. All authors reviewed and approved the final article.
Study conception and design: Eric Noll, Christophe Muccioli, Julien Pottecher, Anaëlle Tchentcheli, Pierre Diemunsch, and Philippe A. Liverneaux
Acquisition of data: Eric Noll, Anaëlle Tchentcheli, and Philippe A. Liverneaux
Analysis and interpretation of data: Eric Noll, Pierre-Olivier Ludes, Sophie Diemunsch, Philippe Clavert, and Girish P. Joshi
Study supervision: Eric Noll, Anaëlle Tchentcheli, Pierre Diemunsch, and Philippe A. Liverneaux
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval
#IRB00010254-2020-064
ORCID iD
Eric Noll https://orcid.org/0000-0001-5655-6866
Supplemental Material
Supplemental material for this article is available online.
Refrences
- 1.Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708‐1720. doi: 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect Dis. 2020;20(6):669-677. doi: 10.1016/S1473-3099(20)30243-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. The Lancet. 2020;395:507-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid-19 in critically ill patients in the Seattle region - Case series. N Engl J Med. 2020;382(21):2012-2022. doi: 10.1056/NEJMoa2004500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McMichael TM, Currie DW, Clark S, et al. Epidemiology of Covid-19 in a long-term care facility in King County, Washington. N Engl J Med 2020;382(21):2005-2011. doi: 10.1056/NEJMoa2005412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coronavirus Disease (COVID-19) Pandemic at. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 [Google Scholar]
- 7.Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475-481. doi: 10.1016/S2213-2600(20)30079-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bouadma L, Lescure F-X, Lucet J-C, Yazdanpanah Y, Timsit J-F. Severe SARS-CoV-2 infections: Practical considerations and management strategy for intensivists. Intensive Care Med. 2020;46:579-582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. J Am Med Assoc. 2020;323:1061-1069. doi: 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy. J Am Med Assoc. 2020;323:1545. doi: 10.1001/jama.2020.4031 [DOI] [PubMed] [Google Scholar]
- 12.Carenzo L, Costantini E, Greco M, et al. Hospital surge capacity in a tertiary emergency referral centre during the COVID‐19 outbreak in Italy. Anaesthesia. 2020;75:928-934. doi: 10.1111/anae.15072 [DOI] [PubMed] [Google Scholar]
- 13.Santé Publique France: COVID-19 : point épidemiologique 2020 at. https://www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-et-infections-respiratoires/infection-a-coronavirus/documents/bulletin-national/covid-19-point-epidemiologique-du-2-avril-2020
- 14.Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet Lond Engl. 2007;370:1453-1457. [DOI] [PubMed] [Google Scholar]
- 15.SantéPublique France: Données hospitalières relatives à l’épidémie de COVID-19 - data.gouv.fr at. https://www.data.gouv.fr/fr/datasets/donnees-hospitalieres-relatives-a-lepidemie-de-covid-19/
- 16.Black MD, Vigorito MC, Curtis JR, et al. A multifaceted intervention to improve compliance with process measures for ICU clinician communication with ICU patients and families. Crit Care Med. 2013;41:2275-2283. [DOI] [PubMed] [Google Scholar]
- 17.Mistraletti G, Umbrello M, Mantovani ES, et al. A family information brochure and dedicated website to improve the ICU experience for patients’ relatives: An Italian multicenter before-and-after study. Intensive Care Med. 2017;43:69-79. [DOI] [PubMed] [Google Scholar]
- 18.de Mik SML, Stubenrouch FE, Balm R, Ubbink DT. Systematic review of shared decision-making in surgery. Br J Surg. 2018;105:1721-1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Publ Health. 2020;17.5):1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xiao H, Zhang Y, Kong D, Li S, Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in january 2020 in China. Med Sci Monit Int Med J Exp Clin Res. 2020;26:e923921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.ARDS Definition Task Force, Ranieri VM Rubenfeld GD, et al. Acute respiratory distress syndrome: The Berlin definition. J Am Med Assoc. 2012;307:2526-2533. [DOI] [PubMed] [Google Scholar]
- 22.Fan E, Brodie D, Slutsky AS. Acute respiratory distress syndrome. J Am Med Assoc. 2018;319:698-710. [DOI] [PubMed] [Google Scholar]
- 23.Ferguson ND, Fan E, Camporota L, et al. The Berlin definition of ARDS: An expanded rationale, justification, and supplementary material. Intensive Care Med. 2012;38:1573-1582. [DOI] [PubMed] [Google Scholar]
- 24.Lancaster EM, Sosa JA, Sammann A, et al. Rapid response of an academic surgical department to the COVID-19 pandemic: Implications for patients, surgeons, and the community. J Am Coll Surg. 2020;230:1064-1073. doi: 10.1016/j.jamcollsurg.2020.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, Supplemental_Material for Surgical Support for Severe COVID-19 Patients: A Retrospective Cohort Study in a French High-Density COVID-19 Cluster by Eric Noll, Christophe Muccioli, Pierre-Olivier Ludes, Julien Pottecher, Pierre Diemunsch, Sophie Diemunsch, Anaëlle Tchentcheli, Philippe Clavert, Girish P. Joshi and Philippe A. Liverneaux in Surgical Innovation