Abstract
Objective
To assess patient experiences with rapid implementation of ambulatory telehealth during the coronavirus disease 2019 (COVID-19) pandemic.
Methods
A mixed-methods study was performed to characterize the patients' experience with neurology telehealth visits during the first 8 weeks of the COVID-19 response. Consecutive patients who completed a telehealth visit were contacted by telephone. Assenting patients completed a survey quantifying satisfaction with the visit followed by a semistructured telephone interview. Qualitative data were analyzed using the principles of thematic analysis.
Results
A total of 2,280 telehealth visits were performed, and 753 patients (33%) were reached for postvisit feedback. Of these, 47% of visits were by video and 53% by telephone. Satisfaction was high, with 77% of patients reporting that all needs were met, although only 51% would consider telehealth in the future. Qualitative themes were constructed, suggesting that positive patient experiences were associated not only with the elimination of commute time and associated costs but also with a positive physician interaction. Negative patient experiences were associated with the inability to complete the neurologic examination. Overall, patients tended to view telehealth as a tool that should augment, and not replace, in-person visits.
Conclusion
In ambulatory telehealth, patients valued convenience, safety, and physician relationship. Barriers were observed but can be addressed.

Telemedicine has been used in neurology since the early 2000s with the implementation of telestroke.1-3 Not only did this technology provide a safe alternative to in-person care, but it also expanded access to acute specialist-driven care for patients within the therapeutic window for ischemic stroke interventions, and it is now the standard in acute stroke when an in-person neurologist is unavailable. Since then, telemedicine has been used in other areas of neurology to improve health care access. This has been particularly beneficial for patients who reside in areas without access to subspecialty neurologists or have barriers to care such as limited transportation, mobility concerns, or caregiver needs.4
Previous studies have demonstrated the clinical and financial benefits of telehealth, including elimination of travel expenses, travel time, and improved triage of patients needing tertiary care.5-7 Barriers have also been identified including specific examination techniques (e.g., deep tendon reflexes and fundoscopy) in neurology.4,8 Widening health disparities were revealed; older, male, Black patients with Medicare or Medicaid insurance were less likely to adopt video visits.9 In response to the coronavirus disease 2019 (COVID-19) pandemic, telehealth has increased exponentially. Moving forward, a telemedicine-driven paradigm shift in care delivery may persist into the postpandemic era. Specifically, the implementation of web-based applications, which support appointment scheduling, online consultation, test result follow-up, prescription completion, medication delivery, and most importantly, health insurance coverage, has been shown to increase patient familiarity with and utilization of telemedicine services.10 Further studies will be necessary to assess the utility of virtual platforms in advancing clinical research via pretrial screening, participant training, or real-time video evidence of participants complying with pharmacologic treatment.
No study has comprehensively assessed the current and future role of telehealth in ambulatory neurology through qualitative exploration of the patient experience. We sought to quantify and characterize the patient perspective during implementation of telehealth in the neurology ambulatory setting.
Methods
Design
A sequential mixed-methods study was conducted including the following: (1) quantitative survey of patients undergoing ambulatory telehealth visits and (2) qualitative assessment of postvisit telephone interviews to characterize the benefits, challenges, and patient recommendations.
Ethics
This study was reviewed and approved by the Wake Forest School of Medicine Institutional Review Board (IRB#00065375).
Standard Protocol Approvals, Registrations, and Patient Consents
This study was classified as Expedited Category 5. It meets criteria for a waiver of consent and a waiver of HIPAA authorization.
Intervention
In response to the COVID-19 pandemic, the Department of Neurology at Wake Forest Baptist Medical Center rapidly implemented ambulatory telehealth as previously described.7 All clinic visits for new and established patients of all ages were converted to telehealth visits, except for urgent complaints when emergency care was in question. Appointment schedulers offered video visits as the preferred modality, and a telephone visit was scheduled only if a video visit was not possible. Ambulatory clinical staff adapted their training to support telehealth visits. Certified Medical Assistants (CMAs) were given standardized training on scheduling new visit types, scripting on how to discuss logistics with patients, and stepwise instructions on guiding patients through technology and software. CMAs contacted all patients and rescheduled in-person clinic visits to telehealth visits.
All patients who completed an ambulatory telehealth visit between March 24 and May 8, 2020, were contacted for participation. One of 8 study team members (C.O., S.T., K.D., A.A., L.S., A.S., L.S., and C.C.) contacted each patient by telephone within 1 to 4 weeks of the appointment. Patients were contacted once, and no voicemails were left. Quantitative and qualitative feedback was gathered from patients who were successfully contacted and verbally assented. Patient reasoning for choosing not to participate in the study included the following: the patient hung up the telephone, was unavailable or busy, did not recall the specific telehealth visit under question, had rescheduled the televisit to a later date, was Spanish-speaking only, could not hear the survey administrator because of poor phone connection, or, in rare cases, had deceased.
Quantitative Methods
Assenting participants were asked 3 multiple-choice questions to quantify the following: (1) the type of telehealth visit, (2) whether the telehealth visit met the patient's needs (4-point Likert: [4] all needs were met; [3] some needs were met; [2] a few needs were met but not all, because this was a telehealth visit; and [1] needs were not met because this was a telehealth visit), and (3) whether the patient would consider a future telehealth visit (4-point Likert: [4] would definitely consider a future telehealth visit; [3] might consider; [2] would consider it only if required; and [1] would not consider). Questionnaire responses were summarized using descriptive statistics. Relative proportions of each question were calculated and compared between patients undergoing video vs telephone visits.
Qualitative Methods
After answering 3 multiple-choice questions, assenting participants were prompted to provide general feedback, including surprises, challenges, or benefits that they experienced from meeting with a neurologist through video or telephone. A semistructured interview prompt was used. Patient responses were primarily documented verbatim. Patient responses were analyzed using Strauss and Corbin constant comparative method for thematic analysis. An initial codebook was developed by 2 study facilitators (C.O. and S.T.) using a random sample of 100 patient responses. These 2 study facilitators independently coded 50 patient responses and then debriefed to compare codes, discuss discrepancies, add or amend codes, and revise the codebook. This process was successively repeated 2 additional times for a total of 150 coded responses. Two study facilitators (C.O. and S.T.) individually coded the remaining patient responses. The codes were then closely compared and revised, when needed, to ensure code accuracy. Response codes were analyzed for thematic redundancies and generation of representative meta-themes and subthemes for the data set, including distinctions among emergent themes based on the type of telehealth visit (i.e., video visit vs telephone visit).
Data Analysis and Synthesis
Quantitative and qualitative data were collected contemporaneously and synthesized at analysis. Quantitative results were analyzed first. Descriptive statistics were performed. To compare patient feedback by visit type, responses were dichotomized (4 vs 1–3) and 2-sided Fisher exact test used with predetermined statistical significance of α < 0.05. Trends of interest were further explored in qualitative analysis.
Data Availability
The data that support study findings are available on request.
Results
Demographics
Between March 24 and May 8, 2020, 2,280 patients completed an ambulatory telehealth visit and were contacted through postvisit telephone call. Contact was successfully made with 858 patients (38%); 753 assented (33%). Reasons for choosing not to participate included lack of time or interest, failure to recall the specific visit, or inability to speak English. All assenting participants completed 3 quantitative multiple-choice questions. Of these participants, 551 chose to also respond to a single open-ended qualitative question. The 202 patients who chose not to answer the qualitative question stated “no comment.”
Mean age was 47.6 ± 24.2 years. Participants identified as White or Caucasian (80%), Black or African American (14%), Asian (<1%), and other, including Latin American, American Indian or Alaskan Native (6%), or they did not define their race (0.4%); 145 identified as female (56%). Sex did not significantly differ between participants who completed video vs telephone visits. Participants who completed video visits were younger (42 years vs 52, p < 0.00001) and more likely to identify as White or Caucasian (85% vs 75%, p = 0.00122) (Table 1).
Table 1.
Demographic Features of Assenting Participants (n = 753) and Nonparticipants (n = 1,527)
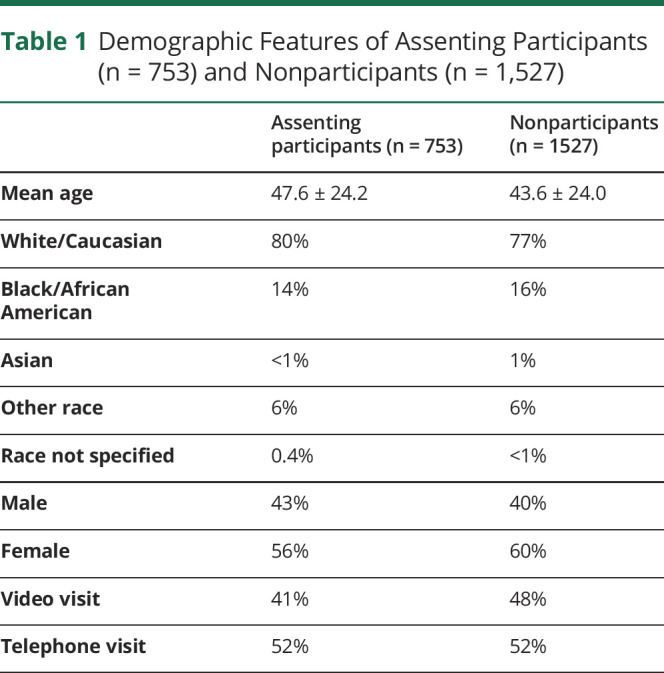
Nonparticipants who were not successfully contacted or chose not to participate in the study (n = 1,527) had similar demographics including age (43.6 ± 24.0 years); White or Caucasian (77%), Black or African American (16%), Asian (1%), other (6%), or did not define their race (<1%); and female (60%). Visit type was similar for participants (41% video, 52% telephone, 7% converted from video to telephone) and nonparticipants (48% video, 52% telephone) (Table 1).
Quantitative Study Results
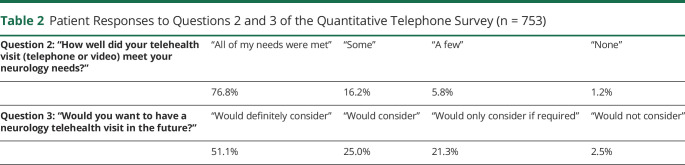
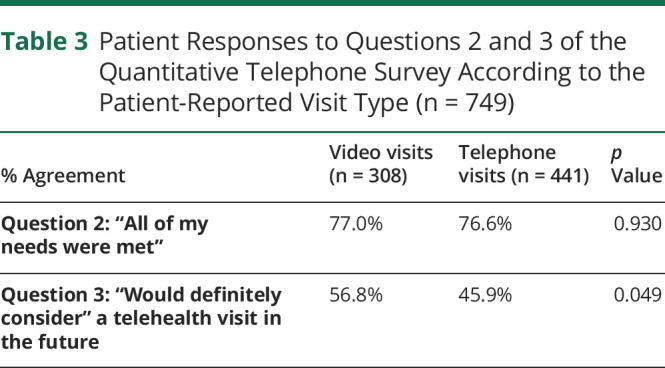
The majority of participants reported that all needs were met with their telehealth visit (77%, Table 2). Needs were met equivalently by the ambulatory telehealth visit regardless of visit type (Table 3). Although only 51% would definitely consider, another 25% would consider a future telehealth visit, and an additional 21% would consider a future telehealth visit if required (Table 3). When stratifying by visit type, 57% of patients who completed video visits would definitely consider a future telehealth visit compared with 46% of patients who completed a telephone visit (p = 0.049).
Table 2.
Patient Responses to Questions 2 and 3 of the Quantitative Telephone Survey (n = 753)
Table 3.
Patient Responses to Questions 2 and 3 of the Quantitative Telephone Survey According to the Patient-Reported Visit Type (n = 749)
Qualitative Study Results
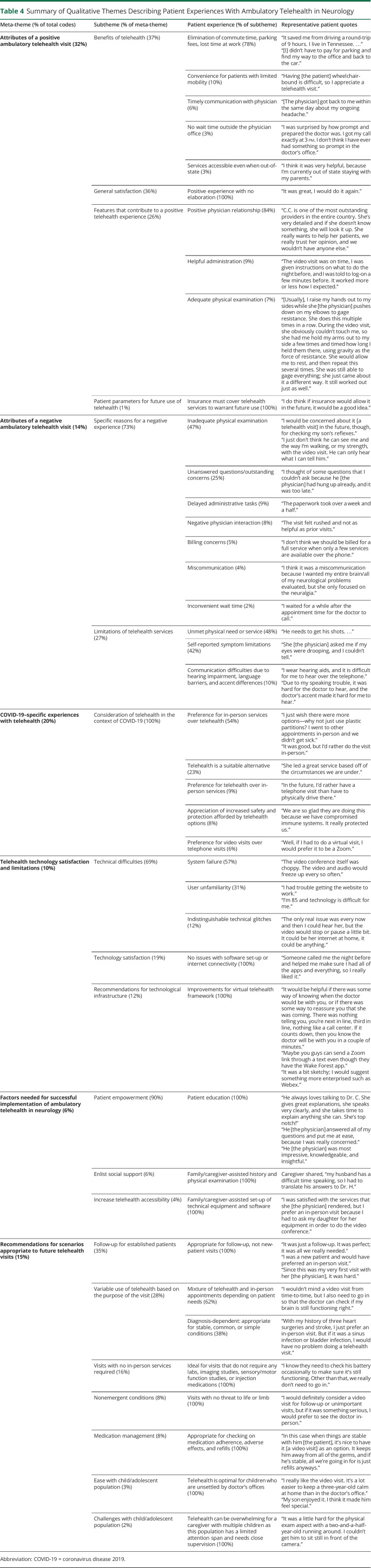
A total of 551 responses were coded, and 6 major categories describing the patient experience were constructed, including: (1) attributes of a positive experience, (2) attributes of a negative experience, (3) experiences with telehealth unique to COVID-19, (4) comments regarding the technology used, (5) factors required to facilitate ambulatory telehealth in neurology, and (6) recommendations for future telehealth visits (Table 4).
Table 4.
Summary of Qualitative Themes Describing Patient Experiences With Ambulatory Telehealth in Neurology
Attributes of a Positive Ambulatory Telehealth Visit
Thirty-two percent of all qualitative responses described attributes of a positive telehealth experience. These included the general benefits of ambulatory telehealth (37% of codes), the overall pleasant experience (36%), factors that contributed to a positive patient experience (26%), and guidelines for future telehealth (1%).
Benefits of Telehealth
The most frequently cited benefit of telehealth was the elimination of commute time, inconveniences of finding and paying for parking, and lost time at work. Together, these accounted for 78% of all codes relating to the benefits of telehealth. Participants also commented on the convenience of telehealth, especially for people with limited mobility (10% of codes in this category). Participants indicated that they were satisfied with timely physician communication, which allowed prompt response to patient questions and concerns (6%). Participants were thrilled by the elimination of wait time outside the physician office (3%) and that telehealth expanded access to rural and out-of-state areas (3%).
General Satisfaction
Participants often offered general positive feedback with no further elaboration (36% of codes) saying, “It was great. I would do it again.”
Features That Contributed to a Positive Telehealth Experience
The main feature of a positive experience was a positive physician relationship, described in 84% of codes. Additional features that contributed to a positive experience included administrative staff who helped patients navigate the logistics of transitioning from in-person to telehealth visits (9%) and the belief that telehealth allows for a comprehensive physical examination (7%). Regarding a positive physician relationship, one patient shared, “she's very detailed and if she doesn't know something, she will look it up. She really wants to help her patients, we really trust her opinion, and we wouldn't have anyone else.”
Patient Parameters for Future Use of Telehealth
Participants (1%) remarked that they “will continue to use telehealth if insurance covers visits in the future.”
Attributes of a Negative Ambulatory Telehealth Visit
Fourteen percent of all qualitative responses described attributes of a negative telehealth experience including specific reasons for an unfavorable experience (73% of codes) and limitations of telehealth services (27% of codes).
Specific Reasons for a Negative Telehealth Experience
The most frequently cited reason for a negative telehealth experience was the absence of a comprehensive physical examination, which accounted for 47% of all codes in this category. One patient said, “I just don't think he can see me and the way I'm walking, or my strength, with the video visit. He can only hear what I can tell him.” Other reasons reported by participants included unanswered questions and/or outstanding concerns (25%), delayed administrative tasks between physician and laboratory offices or pharmacy (9%), negative physician interactions (8%), billing concerns (5%), miscommunication (4%), and inconvenient wait time from the point of patient login to being seen in the online portal (2%).
Limitations of Telehealth Services
Limitations identified by patients included the following: (1) unavailable services such as blood draws, nerve conduction tests, or medication injections (48% of responses in this category), (2) ambiguities or errors associated with self-reported symptom progression, improvement, or recurrence (42%), and (3) increased communication difficulties owing to hearing impairment, language insufficiency, or differences in phonation and pronunciation (10%).
COVID-19–Specific Experiences With Telehealth
Twenty percent of all qualitative responses described opinions regarding telehealth in the context of the current coronavirus pandemic. This included patient preference for in-person visits despite possible exposure to the virus (54% of codes in this category), patient acceptance of telehealth as a suitable alternative during the pandemic (23%), patient preference for telehealth visits over in-person visits (9%), patient appreciation of safety and protection from unnecessary exposures (8%), and patient preference for video visits over telephone visits during the pandemic (6%).
Telehealth Technology Satisfaction and Limitations
Ten percent of all qualitative responses commented on the technological infrastructure used to facilitate telehealth visits. These included details regarding technical difficulties such as video conferencing system failure, user unfamiliarity, and suboptimal internet connectivity (69% of codes in this category), reports of successful software set-up and use (19%), and recommendations to improve the virtual telehealth framework (12%).
Factors Needed for Successful Implementation of Ambulatory Telehealth in Neurology
Six percent of all qualitative responses detailed 3 elements to increase the successful implementation and integration of ambulatory telehealth in daily clinical practice of neurology. These include the following: (1) patient empowerment through patient education about diagnosis, symptom management, medication management, and prognosis (90% of codes in this category), (2) encouragement of social support through family/caregiver-assisted history and physical examination (6%), and (3) improvement in telehealth accessibility through family/caregiver assistance with software and technical equipment (4%).
Recommendations for Scenarios Appropriate to Future Telehealth Visits
Fifteen percent of all qualitative responses commented on specific scenarios in which telehealth should be maximized in the future. These scenarios include the following: (1) follow-up appointments for established patients as opposed to new patients (35% of responses in this category), (2) patients with stable diagnoses or visits depending on patient needs (28%), (3) visits that do not require any in-person services (16%), (4) nonemergent chief concerns (8%), (5) medication management visits (8%), and (6) children and adolescent visits that do not require an extensive physical examination (3%). Specific anecdotes from patients include, “it was just a follow-up. It was perfect; it was all we really needed” and “with my history of three heart surgeries and stroke, I just prefer an in-person visit. But if it was a sinus infection or bladder infection, I would have no problem doing a telehealth visit.” Notably, 2% of responses described difficulty with completing telehealth visits for toddlers who have limited attention span and require close supervision at all times.
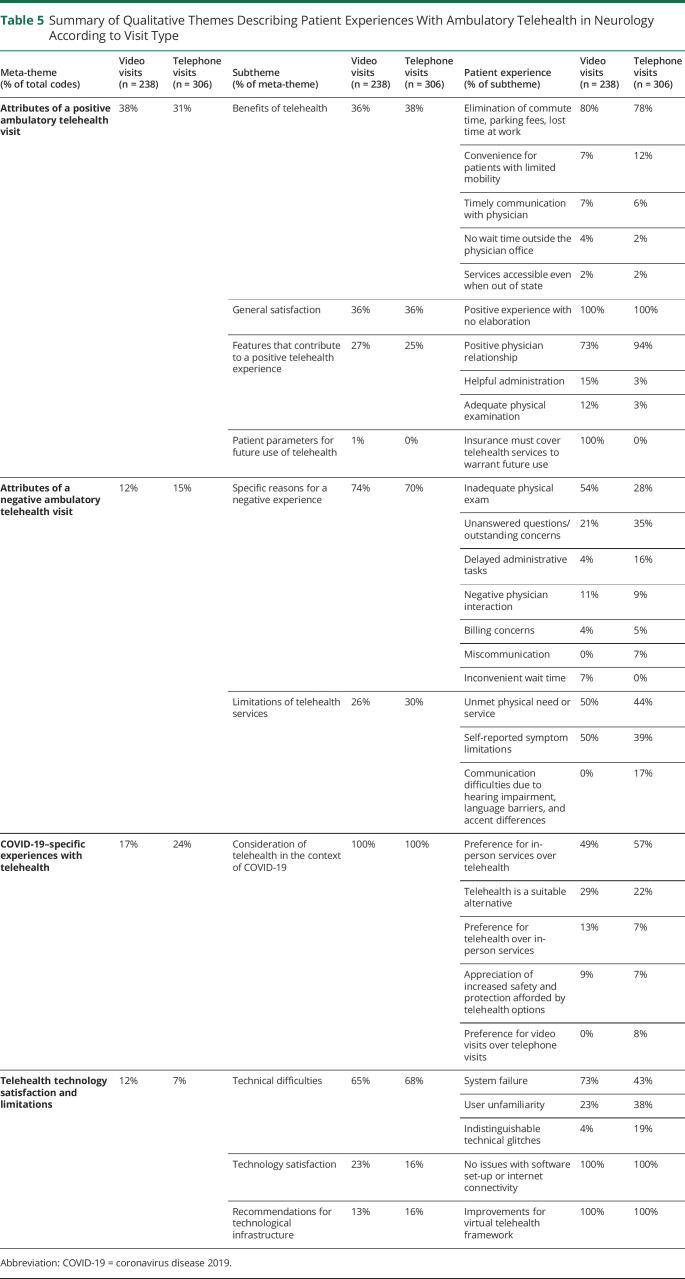
Positive Attributes According to the Type of Telehealth Visit
The distribution of meta-themes was similar when analyzed by visit type (i.e., video vs telephone visit) (Tables 5 and 6). Patients completing video visits were more likely to discuss positive attributes of an ambulatory telehealth visit (38% vs 31% of telephone users) and less likely to discuss negative attributes (12% vs 15% of telephone users). Among participants who commented on the benefits of telehealth, the elimination of commute time was the most frequent response across both video and telephone visits (80% and 78%, respectively). The convenience of telehealth for patients with limited mobility was more likely to be valued for patients completing telephone visits (12% vs 7%). Of the patients describing features of a positive experience, 94% of telephone participants indicated that a positive physician relationship was essential, compared with only 73% of video visit participants. Video visit participants were more likely to value helpful administrative staff support (15% vs 3%) and view the virtual physical examination as adequate (12% vs 3%). This sentiment is emphasized by the following patient comment, “the video visit was on time, I was given instructions on what to do the night before, and I was told to log-on a few minutes before. It worked more or less how I expected.”
Table 5.
Summary of Qualitative Themes Describing Patient Experiences With Ambulatory Telehealth in Neurology According to Visit Type
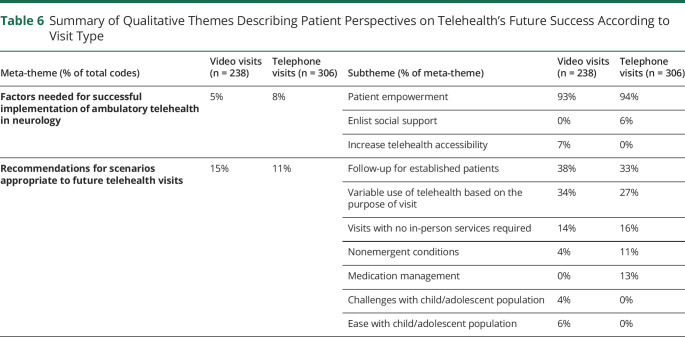
Table 6.
Summary of Qualitative Themes Describing Patient Perspectives on Telehealth's Future Success According to Visit Type
Negative Attributes According to the Type of Telehealth Visit
Among patients who described reasons for a negative telehealth experience, patients who completed a video visit were more likely to cite the lack of a comprehensive neurologic examination and inconvenient wait time compared with telephone visits (28% and 0%, respectively). Among reasons for a negative telehealth experience, patients completing telephone visits were more likely to report remaining questions or outstanding concerns (35%) and miscommunication issues (7%) compared with video visits (21% and 0%, respectively).
COVID-19–Specific Experiences According to the Type of Telehealth Visit
Of the participants who shared opinions regarding telehealth in the context of the COVID-19 pandemic, 57% of patients who completed telephone visits commented on wanting future in-person visits over telehealth visits, whereas the remaining 43% of patients commented on the following: (1) telehealth visits as a suitable alternative given the dangers associated with the pandemic, (2) increased safety offered by telehealth, (3) preference for telehealth over in-person visits, and (4) preference for video visits over telephone visits. Of those who completed video visits and commented on COVID-specific experiences, 49% of patients desired in-person visits over telehealth visits, whereas 29% of patients agreed that telehealth was a suitable alternative, 9% recognized the increased safety associated with telehealth, and 13% preferred telehealth over in-person visits.
Limitations of Technology According to the Type of Telehealth Visit
Of those who discussed dissatisfaction with technology, technical system failure was cited by 73% of patients completing a video visit compared with 43% of telephone visits. In contrast, user unfamiliarity was discussed by 38% of patients completing telephone visits compared with 23% of video visits.
Factors Needed for Successful Telehealth Integration and Recommendations for Future Video and Telephone Visits
Patients who completed telephone visits were more likely to discuss the need for social support such as family members or caregivers when conducting the history and physical examination (6% telephone vs 0% video). For instance, 1 telephone user shared that her husband has a difficult time speaking, so she had to translate his answers to the physician. However, patients who completed video visits were more likely to discuss the need for assistance in setting up the technical equipment and software (7% of video users vs 0% of telephone users). When noting specific scenarios in which future telehealth use would be optimal, telephone users were more likely to consider using telehealth for treating nonemergent conditions (11% telephone vs 4% video) and for aiding in medication management (13% telephone vs 0% video).
Discussion
The COVID-19 pandemic was a catalyst for expanding the utilization of telemedicine in clinical neurology. However, the ability of telephone and video visits to adequately meet patients' needs and provide care in an equivocal manner to the in-person setting has yet to be thoroughly examined. By investigating patient experiences with telehealth through both quantitative and qualitative methods, this study provides several important findings. First, we confirm that the overall experience is positive, with >75% of patients reporting that all their needs were met, regardless of modality. Positive patient experiences were frequently attributed to the elimination of commute time and associated finances including gas, parking, and accommodation costs, as well as a positive physician interaction and relationship. Second, negative patient experiences were most frequently attributed to the inability to complete a traditional neurologic examination. Third, patients perceive technology (including software, internet connection, and user ability) as a barrier to telemedicine. Finally, patients tend to view telehealth as a tool that may augment traditional means of providing health care, rather than a replacement for in-person visits altogether.
With reduction of transportation burden, one of the greatest potential benefits of telemedicine is its ability to expand access to care, particularly to subspecialists.11 Previously, telemedicine has been shown to increase patient adherence to clinical recommendations, expand access to subspecialty services, allow health care to be provided in rural areas where patients would otherwise have to travel long distances to see a provider, and facilitate out-of-state care.12,13 Of these known findings, however, out-of-state coverage was mentioned only by 3% of respondents who commented on the benefits of telehealth in the current study, and no patients specifically mentioned the ability to improve access to subspecialty services. This may be due to the evolving policies surrounding out-of-state telemedicine provision and implementation; however, this study was performed at an early time in the pandemic when telehealth coverage had expanded most broadly. Alternatively, this may be due to few or no individuals being out-of-state among the surveyed population. Patients were far more likely, across both video and telephone visits, to comment on the ability of telehealth to eliminate commute time or associated travel finances, often calling it convenient and comfortable. Patients, especially those who had a telephone visit, emphasized telehealth's convenience in the setting of limited mobility due to ischemic strokes, demyelinating CNS lesions or in the setting of driving restrictions due to vision loss or epilepsy.
Beyond access to care, an additional factor that strongly contributed to a positive telehealth experience was the patient-physician relationship. This association has been well documented for in-person experiences because positive patient-physician interactions have been shown to improve patient satisfaction, improve health care outcomes, and even decrease malpractice lawsuits.14,15 In our study, patients were equally likely to provide general positive comments about their physician (e.g., “he is amazing”) as they were to comment on the provider's ability to diagnose, treat, and educate patients (e.g., “it was informative and she answered all of my questions”). Of interest, patients who completed a telephone visit reported a relatively stronger reliance on the patient-physician relationship compared with patients who had video visits. This may be due to the fact that video visits allow for interpersonal connection via both sight and sound, compared with only the sense of hearing in a telephone visit. Moreover, those who had a video visit were more likely to comment on the value of administrative staff in setting up the visit. In both cases, communication with the patient was critical to a positive patient experience. In the case of video visits, frequent communication and support from staff will be important moving forward (e.g., “your doctor will be with you in 5 minutes,” “this is how you turn on your camera,” etc), whereas a focus on clear and direct verbal communication from providers is essential with telephone visits.
In comparison, negative patient experiences were often attributed to the inability to perform the complete neurologic examination. Although video visits, rather than telephone visits, were primarily offered during the scheduling of telehealth appointments, only 47% of visits in this study were conducted via video. Patients frequently specified that physicians could not accurately assess gait, strength, ocular abnormalities, and reflexes, and they were concerned that this limited the provider's ability to assess their symptoms. In this cohort, patients were more likely to definitely consider a future video compared with telephone visit. This prompts postulation regarding the impact of the virtual physical examination on visit satisfaction and consideration of future telehealth visits. When the data set was stratified based on the type of visit, a larger proportion of patients with video visits—not patients with telephone visits—were unsettled by the lack of a comprehensive neurologic examination. This is likely due to differences in patient expectations. A limited or absent physical examination is a known limitation of the telephone visit; thus, patients do not expect an examination to be attempted over the telephone. Instead, patients placed greater emphasis on communication and having all questions answered. Patients completing video visits held providers to a different standard because of the inherent capability of this modality.
As telehealth is a new modality to many providers and patients, it is not surprising that technology barriers were frequently mentioned. These barriers included difficulty with video conferencing, problems with internet connection, poor audio or video quality, and user proficiency. Technical system failure was much more commonly reported among patients completing video visits, likely because of factors that are outside the patients' control (e.g., internet connection, poor video resolution, and suboptimal audio quality). Comparatively, patient unfamiliarity was prominent among telephone visits and may even suggest a reason for patient reluctance to attempt a video visit. However, it is also notable that 15% of patients completing video visits detailed a positive experience with the process of setting up relevant equipment, software, and virtual applications, which is likely due to the increased logistical burden of the video visit compared with the telephone visit. This finding further reinforces the importance of technological support staff in a telehealth workflow. Technologically adept family members and caregivers were perceived to play an integral role in improving telehealth's accessibility and sustainability. Suggestions for improving the virtual telehealth framework included the following: (1) using an online queue wherein patients can identify whether they are next in line on the physician's schedule, (2) implementing dual or triple appointment reminder alerts using any combination of encrypted voicemail, text message, or email, in addition to the health portal, and (3) transitioning to a more enterprised video conferencing system that is standardized, reviewed, and approved by the institution to uphold the highest standards of care.
Ultimately, participants tended to view telehealth as something that should augment traditional means of providing health care, rather than as a replacement for in-person visits altogether. This patient perspective is critical as providers and health systems find a new normal in delivering ambulatory care after the COVID-19 pandemic. Participants indicated that they would be most comfortable with the use of telehealth for established care of patients when an in-person physical examination or additional testing is not required. Many patients acknowledged that in-person visits are necessary for certain physical services such as labs, shots, or imaging studies, which may explain why some patients still prefer the in-person visit despite the advances in telehealth capabilities. During the pandemic, patients completing video visits were more likely to appreciate telehealth's ability to increase patient safety.
Clinical models implemented postpandemic will incorporate the patient perspective as well as staff and provider workflows and adequate reimbursement. Future studies will assess how the patient perspective changes as technological barriers are improved and familiarity with telemedicine increases. Application of future technological advancements such as using machine learning tools to objectively gather and trend physical examination data (e.g., extraocular movements, gait patterns) is one example that may influence preferences over time. Communication, or lack thereof, was frequently cited as contributing to positive and negative telehealth experiences. Continued medical education for providers, and perhaps medical school trainees, must shift to incorporate formal telehealth training in an effort to improve provider communication.
Strengths of this study include the large, clinically diverse population and rigorous documentation of patient feedback through semistructured interview soon after the appointment. Determination of the telehealth visit type was confirmed by interview. This question corrected the visit type for patients who converted from video to telephone but is limited by recall bias. By defaulting visits to video, patient preference did not confound visit type.
This study is not without limitations. Visits were canceled because of the statewide stay-at-home order during the first week of telehealth implementation. This resolved rapidly within 5 weeks when ambulatory visit volumes returned to pre-COVID levels, although this could influence early patient feedback. The study population is restricted to this single academic institution and may not be generalizable to all ambulatory neurology practices. Patients were contacted soon after their visit; however, not all patients could be reached. Many patients commented on the limitations of telehealth technology, including software malfunction and user unfamiliarity. This may be attributed to the timing of the study during the early pandemic response. Opinions regarding technological limitations have likely evolved as the novelty of the technology has worn off, and users are now increasingly familiar with platforms. Telehealth software has also undergone rigorous updates to improve user-friendliness and functionality.
The patient voice is critical in defining the optimal role of telemedicine in neurology. Future models will focus on telehealth as an adjunct to traditional in-person visits while maintaining closed-loop verbal and written communication, immediate access to after-visit summaries, pending lab orders, and available appointment dates. Patients value the convenience of telehealth, particularly when they already have an established relationship with their provider. The telehealth patient experience may be improved with the involvement of administrative staff, caregivers, social support, and emphasis on communication strategies that facilitate the virtual patient-physician relationship.
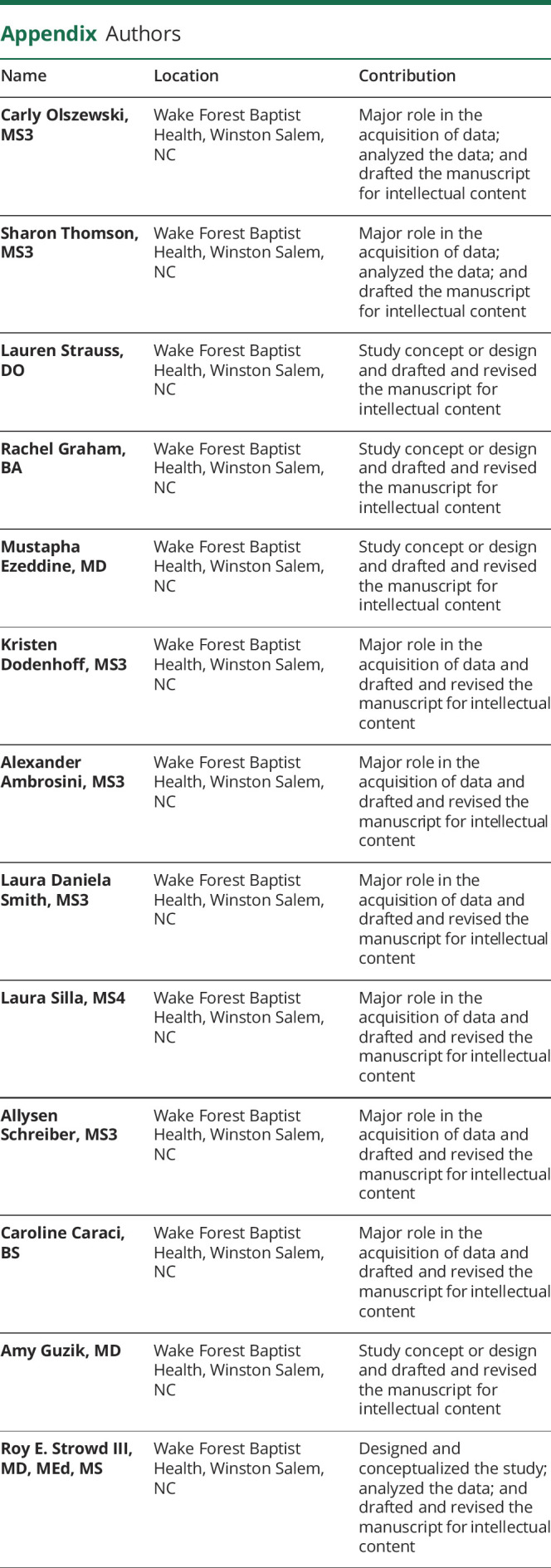
Appendix. Authors
Study Funding
No targeted funding reported.
Disclosure
C. Olszewski, S. Thomson, L. Strauss, R. Graham, M. Ezzedine, K. Dodenhoff, A. Ambrosini, L.D. Smith, L. Silla, A. Schreiber, C. Caraci, and A. Guzik report no disclosures relevant to the manuscript. R.E. Strowd: serves as a consultant for Monteris Medical Inc, Novocure, and Nanobiotix; he receives an editorial stipend as Section Editor of the Resident and Fellow Section of Neurology® and has received research/grant support from the American Academy of Neurology, American Society for Clinical Oncology, Southeastern Brain Tumor Foundation, and Jazz Pharmaceuticals. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Schwamm LH, Holloway RG, Amarenco P, et al. A review of the evidence for the use of telemedicine within stroke systems of care: a scientific statement from the American Heart Association/American Stroke Association. Stroke. 2009;40(7):2616-2634. [DOI] [PubMed] [Google Scholar]
- 2.Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46-e110. [DOI] [PubMed] [Google Scholar]
- 3.Adeoye O, Nystrom KV, Yavagal DR, et al. Recommendations for the establishment of stroke systems of care: a 2019 update: a policy statement from the American Stroke Association. Stroke. 2019;50(7):e187-e210. [DOI] [PubMed] [Google Scholar]
- 4.Hatcher-Martin JM, Adams JL, Anderson ER, et al. Telemedicine in neurology: telemedicine work group of the American Academy of neurology update. Neurology. 2020;94(1):30-38. [DOI] [PubMed] [Google Scholar]
- 5.Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8):e016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wechsler LR, Tsao JW, Levine SR, et al. Teleneurology applications: report of the telemedicine work group of the American Academy of Neurology. Neurology. 2013;80(7):670-676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wechsler LR. Advantages and limitations of teleneurology. JAMA Neurol. 2015;72(3):349-354. [DOI] [PubMed] [Google Scholar]
- 8.Hassan A, Dorsey ER, Goetz CG, et al. Telemedicine use for movement disorders: a global survey. Telemed E-Health. 2018;24(12):979-922. [DOI] [PubMed] [Google Scholar]
- 9.Strowd RE, Strauss L, Graham R, et al. Rapid implementation of outpatient teleneurology in rural Appalachia: barriers and disparities. Neurol Clin Pract. 2021;11(3):232-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tang Y, Xing Y, Cui L, et al. Neurology practice during the COVID‐19 outbreak and post‐pandemic era: experiences and challenges. Eur J Neurol. 2020;27(12):e81–e83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guzik AK, Switzer JA. Teleneurology is neurology. Neurology. 2019;94(1). [DOI] [PubMed] [Google Scholar]
- 12.Nelson EL, Duncan AB, Peacock G, Bui T. Telemedicine and adherence to national guidelines for ADHD evaluation: a case study. Psychol Serv. 2012;9(3):293-297. [DOI] [PubMed] [Google Scholar]
- 13.Ray KN, Demirci JR, Bogen DL, Mehrotra A, Miller E. Optimizing telehealth strategies for subspecialty care: recommendations from rural pediatricians. Telemed E-Health. 2015;21(8):622-629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lester GW, Smith SG. Listening and talking to patients. A remedy for malpractice suits? West J Med. 1993;158(3):268-272. [PMC free article] [PubMed] [Google Scholar]
- 15.Bartlett EE, Grayson M, Barker R, et al. The effects of physician communications skills on patient satisfaction. Recall, and Adherence. 1984;37(9-10):755-764. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support study findings are available on request.