Abstract
Purpose of Review
Physician communication skills are a critical part of care for amyotrophic lateral sclerosis (ALS) patients and caregivers. They shape the development of autonomy and quality of life, and they mitigate emotional trauma. Communication skills are especially critical at 2 different time points in the course of the disease: early when delivering and establishing the diagnosis, and later when clarifying goals of care.
Recent Findings
Several techniques for physician communication of difficult information are available, including SPIKES (Setting up the interview, assessing the patient's Perception, obtaining the patient's Invitation, giving Knowledge and information to the patient, addressing the patient's Emotions with Empathetic responses, and Strategy and Summary), ABCDE (Advance preparation, Build a therapeutic environment/relationship, Communicate well, Deal with patient and family reactions, Encourage and validate emotions), and BREAKS (Background, Rapport, Exploring, Announce, Kindling, Summarize). These emphasize the physician's accountability and responsibility for communicating effectively. Formal training in these techniques is limited, and their applicability specifically to ALS is inexact.
Summary
We propose an ALS-specific technique which we call ALS ALLOW to guide physicians in conducting difficult communications with ALS patients and caregivers to develop their understanding, establish autonomy, set goals, and mitigate emotional trauma. The techniques are useful in discussions both early and late stages in the disease.

Defining Bad News
Bad news has been medically defined as “unfavorable information that adversely and seriously affects an individual's view of his or her future.”1 Conveying bad news to patients is an arduous and emotionally challenging task for which experience and education go hand-in-hand.2–5 Many physicians feel that they are not well prepared for this task and medical curricula devoted to this are limited.6–10
Importance of Delivering bad News Effectively
Effective physician communication has been shown to help patients understand their disease process and treatment options, which subsequently improves patient communication of needs, future planning, sense of control, pain tolerance, and daily functioning.11–13 Studies that investigate the importance of physician delivery of bad news have been performed in various patient populations, ranging from healthy volunteers (i.e., analog patients) to patients in oncology, neurology, general medicine, and traumatic injuries.2,14–19 Physicians with good interpersonal skills and compassionate communication are clearly important.20,21 In both diagnostic and prognostic scenarios, patients reported better recall, reduced stress, and more hopefulness when communicating with physicians who employed robust communication techniques. Warning statements, empathic statements, and “positive” framing of future healthcare outcomes were especially effective.22 Patients report increased quality of life when physicians have good communication and when patients feel that they are given decisional control over how they would like to proceed with their care.23–26
Challenges of Conveying Bad News
A patient's perception of “bad news” is personal and highly variable. The burden falls to the physician to identify the effect of such news and accordingly tailor its delivery. While this may seem easy in theory, when the moment arrives, it may be very difficult to adequately convey the gravity of the news, while simultaneously addressing the associated psychosocial ramifications.14,27 This is an even greater hardship for inexperienced physicians (e.g., interns, residents), particularly when there is a poor prognosis or little therapeutic hope.15,28,29 Patients typically want to know their diagnosis and to discuss treatment options, therapy side effects, and likelihood for a cure.30 Barriers to an effective physician communication include gravity of conversation, patient preparedness, individual personality, cultural and language differences, physician's own emotion, lack of time in productivity-driven healthcare systems,31–33 and inexperience. Some patients desire to know the bad news in one setting, while others prefer to receive piece-meal information and most patients wanted their doctors to address their emotional needs in the same setting of receiving their bad news.34
Physicians and trainees report feeling fear and/or psychological distress that negatively affects their own well-being and their ability to provide high-quality care in disclosing bad news.35–37 Moreover, a physician may be reluctant to deliver bad news given associated feelings of anxiety and fear of ensuing patient response, a phenomenon that psychologists have termed the “mum effect.”38 The mum effect can lead to a delay in diagnosis and follow-up care while delivery of the bad news is avoided.
It is thus imperative that physicians become better trained in the task of delivering bad news, that it becomes a skill, and that standards of care ensure good communication and optimal information to every patient.
Bad News Delivery Techniques
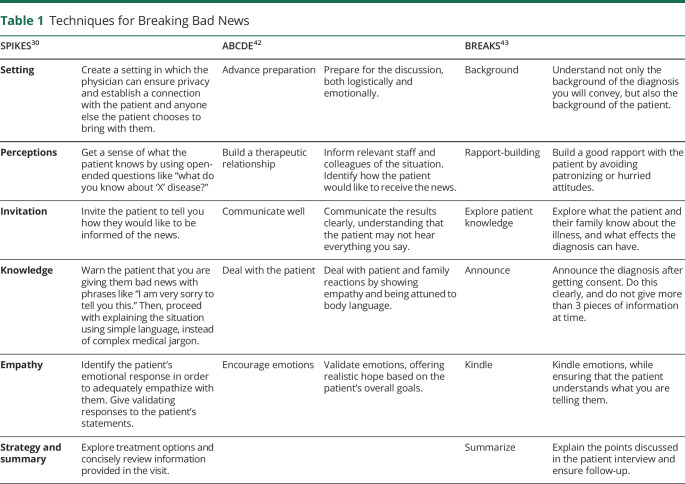
A number of techniques have been developed to assist physicians with delivering bad news more easily and effectively (Table 1). These techniques incorporate many of the variables identified by patients and caregivers based on surveys. Although all typically share common principles, each has its own unique emphasis. The SPIKES (Setting up the interview, assessing the patient's Perception, obtaining the patient's Invitation, giving Knowledge and information to the patient, addressing the patient's Emotions with Empathetic responses, and Strategy and Summary) technique was developed to enable physicians to deliver bad news about cancer in a patient-centered manner by addressing concerns about patient care and long-term outcomes.13,30,39–41 The ABCDE (Advance preparation, Build a therapeutic environment/relationship, Communicate well, Deal with patient and family reactions, Encourage and validate emotions) protocol addresses the steps in the SPIKES technique, while additionally taking into account the feelings of the physician.42 The BREAKS (Background, Rapport, Exploring, Announce, Kindling, Summarize) protocol outlines a strategy similar to SPIKES but highlights the importance of understanding a patient's cultural and ethnic background.43
Table 1.
Techniques for Breaking Bad News
Challenges for Amyotrophic Lateral Sclerosis Patients and Their Caregivers
The majority of literature examining the effects of patient-physician communication of bad news has focused on oncologic diagnoses, which often have substantial treatments and often cure.44–46 This is fundamentally different from amyotrophic lateral sclerosis (ALS), which remains progressive and fatal usually from respiratory insufficiency in essentially all cases even despite extensive biomedical research, new medications, and availability of clinical trials.47–53 Furthermore, ALS patients often receive bad news at 2 different stages of the disease. Early in the disease, they typically learn of their diagnosis when they are highly functional. They may even initially self-diagnose after long internet searches. Ineffective communication at this early stage may cause emotional trauma, and the patient’s quality of life may be compromised by posttraumatic stress disorder. Then, later in the disease, after a variable period of time usually ranging between 1 and 3 years, they must formally reckon with prognosis, and these discussions involve respiratory failure, goals of care, palliation, dying, and advanced directives. Ineffective communication in this stage may cause unrealistic expectations, unpreparedness, and respiratory crises. All of this is further complicated by the fact that the disease manifestations of ALS are markedly heterogeneous. The onset of muscle weakness can occur in variable regions including the limbs, bulbar, truncal, or respiratory muscles. Motor manifestations can be of upper or lower motor neuron character. Higher cortical functions including affect and executive functions can also be affected. Disease progression can be slow or rapid. It is often challenging even for experienced ALS neurologists to predict a timeline for patient prognosis. In addition, there is an abundance of information on the internet about ALS, some of it distressing and some misleading, but it is important to lay out a framework with which to educate and enhance patient understanding.
The SPIKES technique has been studied in ALS.54 Expressing empathy and emotional support, giving information and time to process information, and discussing next steps including multidisciplinary and palliative care were important. Although the SPIKES technique has thus been shown to have efficacy, there are parts of the protocol that can be specifically tailored to ALS patients to better meeting their needs.
ALS-Specific Recommendations
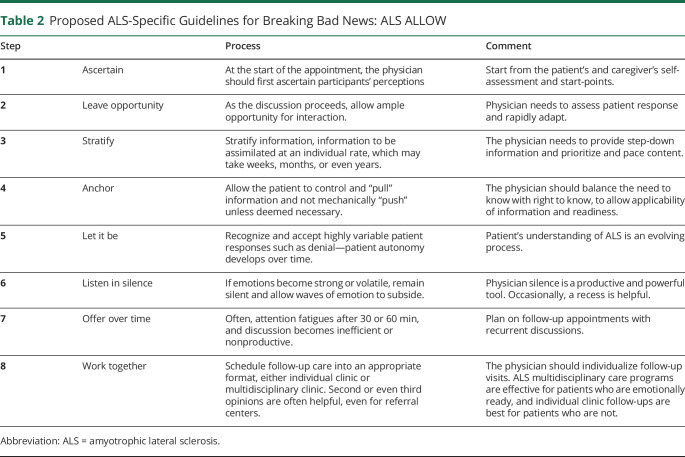
Here, we propose a protocol, ALS ALLOW, modified from existing protocols in an effort to directly address the unique communication challenges of ALS, both early and late in the disease course (Table 2).
Table 2.
Proposed ALS-Specific Guidelines for Breaking Bad News: ALS ALLOW
Step 1: Ascertain
At the beginning of the discussion, the physician needs to ascertain start-points. They do this by asking the patients and also their caregivers their thoughts, opinions, and beliefs. Thus, the physician's delivery and discussion can be tailored to the exact start-points of participants; many difficult discussions can be avoided if start-points are correct. Early in the disease when delivering the diagnosis, ask what they think might be wrong and what they have been told. Later in the disease when the conversation is about prognosis and goals of care, ask where they think they are heading, if they looked ahead and what they think about these.
Step 2: Leave Opportunity
Begin discussion gradually leaving ample opportunity for interaction—the physician must rapidly adapt and direct the discussion to the immediate audience.
Step 3: Stratify
Present information in a step-down approach that allows the patient and their caregivers to understand the information without becoming overwhelmed. Although patient and caregiver thoughts, questions, and emotions may be unfiltered and uncontrolled, it is the role of the physician to organize and prioritize and stratify discussion. Assimilating information is a process that occurs over time, and it is easy to become tangential. Furthermore, explaining the best sources of information, including verified and peer-reviewed websites, may be helpful.
Step 4: Anchor
Both early and late in the disease course, too much or too little information is problematic, and the physician must anchor it. Early in delivering the diagnosis, too much information may be overwhelming, premature, or unnecessary, but too little information may be frustrating, misleading, and leave them unprepared. Later in the disease, too little discussion about goals of care and advanced directive leaves patients and caregivers unprepared and leads to crises.
Step 5: Let It Be
Accommodate various responses including denial especially early in the disease. Understanding ALS is a process that evolves over time, and denial is a critical defense mechanism—pushing against it moves into an uncomfortable emotional space for little gain and may sacrifice long-term trust. “Letting it be” does not apply to denial late in the disease course when it leads to unpreparedness and crises, and at such time, the physician must press the patient to important discussions about goals.
Step 6: Listen in Silence
Physician silence is powerful and important and is not well taught in training. When patients and caregivers are overwhelmed by emotions, silence is golden and sometimes even stepping out of the room to allow privacy is helpful. Trying to communicate during surges of emotion is unproductive.
Step 7: Offer Over Time
Productive discussions need time, and single visits are fatiguing and saturating for patients, caregivers, and physicians. A single visit often becomes ineffective after 30–60 minutes, and discussions at different times need to occur.
Step 8: Work Together
ALS care is both medical and psychosocial. ALS Multidisciplinary Clinics are a critical resource. However, these may be overwhelming especially early on, and some patients and their caregivers are not ready mentally or emotionally, in which case single physician follow-up visits are the best. Late in the disease, home care or hospice may be most appropriate. The physician should individualize follow-up formats and timelines.
Conclusion and Recommendations
Effective physician delivery of bad news is essential for providing humanistic and individualized patient care for ALS. The recommendations for delivering bad news to ALS patients outlined in this paper address the unique complexity of ALS and are adapted from SPIKES, ABCDE, and BREAKS protocols that take a patient-centered approach. These recommendations apply to both delivering initial diagnosis and later discussions of goals of care and end of life. Patient autonomy is built over time on a patient-physician alliance that starts early in the disease course and evolves over time. Future discussions by the ALS and palliative care communities are required to explore complex boundaries between physician duty and patient autonomy.
Appendix. Authors
Study Funding
No targeted funding reported.
Disclosure
The authors report no disclosures relevant to the manuscript. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
TAKE-HOME POINTS
→ Physician communication with ALS patients and their caregivers has unique challenges.
→ Skillful communications are especially important at 2 different time points: early in the disease when delivering the diagnosis and later in the disease when establishing goals of care. These communications have different aims, but the skills are essentially the same.
→ One essential skill is to first establish start-points of conversations from patients and caregivers and then based on those, individualize communication, prioritize topics, and pace.
→ Physician communication is a skill that can be taught and learned.
References
- 1.Buckman R. Breaking Bad News: A Guide for Health Care Professionals . 15. Baltimore, MD: Johns Hopkins University Press; 1992. [Google Scholar]
- 2.Ichikura K, Matsuda A, Kobayashi M, Noguchi W, Matsushita T, Matsushima E. Breaking bad news to cancer patients in palliative care: a comparison of national cross-sectional surveys from 2006 and 2012. Palliat Support Care 2015;13:1623–1630. [DOI] [PubMed] [Google Scholar]
- 3.Luttenberger K, Graessel E, Simon C, Donath C. From board to bedside—training the communication competences of medical students with role plays. BMC Med Educ 2014;14:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hurst SA, Baroffio A, Ummel M, Burn C. Helping medical students to acquire a deeper understanding of truth-telling. Med Educ Online 2015;20:28133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aminiahidashti H, Mousavi SJ, Darzi MM. Patients' attitude toward breaking bad news; a brief report. Emerg (Tehran) 2016;4:34. [PMC free article] [PubMed] [Google Scholar]
- 6.Monden KR, Gentry L, Cox TR. Delivering bad news to patients. Proc (Bayl Univ Med Cent) 2016;29:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosenbaum ME, Ferguson KJ, Lobas JG. Teaching medical students and residents skills for delivering bad news: a review of strategies. Acad Med 2004;79:107–117. [DOI] [PubMed] [Google Scholar]
- 8.Sanson-Fisher R, Maguire P. Should skills in communicating with patients be taught in medical schools? Lancet 1980;316:523–526. [DOI] [PubMed] [Google Scholar]
- 9.Orlander JD, Fincke B, Hermanns D, Johnson GA. Medical residents' first clearly remembered experiences of giving bad news. J Gen Intern Med 2002;17:825–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sullivan AM, Lakoma MD, Block SD. The status of medical education in end-of-life care: a national report. J Gen Intern Med 2003;18:685–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chesanow N. Delivering “Bad” vs “Serious” News to Patients. Medscape Available at: www.medscape.com/viewarticle/856955. Accessed March 1, 2017. [Google Scholar]
- 12.Ha JF, Longnecker N. Doctor-patient communication: a review. Ochsner J 2010;10:38–43. [PMC free article] [PubMed] [Google Scholar]
- 13.Maguire P, Pitceathly C. Key communication skills and how to acquire them. BMJ 2002;325:697–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fallowfield L, Jenkins V. Communicating sad, bad, and difficult news in medicine. Lancet 2004;363:312–319. [DOI] [PubMed] [Google Scholar]
- 15.Kirshblum S, Fichtenbaum J. Breaking the news in spinal cord injury. J Spinal Cord Med 2008;31:7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maguire P. Breaking bad news: talking about death and dying. Medicine (Baltimore) 2005;33:29–31. [Google Scholar]
- 17.Dean A, Willis S. The use of protocol in breaking bad news: evidence and ethos. Int J Palliat Nurs 2016;22:265–271. [DOI] [PubMed] [Google Scholar]
- 18.Back AL, Trinidad SB, Hopley EK, Arnold RM, Baile WF, Edwards KA. What patients value when oncologists give news of cancer recurrence: commentary on specific moments in audio-recorded conversations. Oncologist 2011;16:342–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Merckaert I, Libert Y, Razavi D. Communication skills training in cancer care: where are we and where are we going? Curr Opin Oncol 2005;17:319–330. [DOI] [PubMed] [Google Scholar]
- 20.Mager WM, Andrykowski MA. Communication in the cancer “bad news” consultation: patient perceptions and psychological adjustment. Psychooncology 2002;11:35–46. [DOI] [PubMed] [Google Scholar]
- 21.Fogarty LA, Curbow BA, Wingard JR, McDonnell K, Somerfield MR. Can 40 seconds of compassion reduce patient anxiety? J Clin Oncol 1999;17:371–379. [DOI] [PubMed] [Google Scholar]
- 22.Porensky EK, Carpenter BD. Breaking bad news: effects of forecasting diagnosis and framing prognosis. Patient Educ Couns 2016;99:68–76. [DOI] [PubMed] [Google Scholar]
- 23.Street RL, Voigt B. Patient participation in deciding breast cancer treatment and subsequent quality of life. Med Decis Making 1997;17:298–306. [DOI] [PubMed] [Google Scholar]
- 24.Andersen MR, Urban N. Involvement in decision-making and breast cancer survivor quality of life. Ann Behav Med 1999;21:201–209. [DOI] [PubMed] [Google Scholar]
- 25.Gattellari M, Butow PN, Tattersall MH. Sharing decisions in cancer care. Soc Sci Med 2001;52:1865–1878. [DOI] [PubMed] [Google Scholar]
- 26.Arora NK. Interacting with cancer patients: the significance of physicians' communication behavior. Soc Sci Med 2003;57:791–806. [DOI] [PubMed] [Google Scholar]
- 27.Buckman R. Breaking bad news: why is it still so difficult? Br Med J (Clin Res Ed) 1984;288:1597–1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sarafis P, Tsounis A, Malliarou M, Lahana E. Disclosing the truth: a dilemma between instilling hope and respecting patient autonomy in everyday clinical practice. Glob J Health Sci 2014;6:128–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Silani V, Borasio GD. Honesty and hope: announcement of diagnosis in ALS. Neurology 1999;53:S37–S39; discussion S40–42. [PubMed] [Google Scholar]
- 30.Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES—a six-step protocol for delivering bad news: application to the patient with cancer. Oncologist 2000;5:302–311. [DOI] [PubMed] [Google Scholar]
- 31.Dosanjh S, Barnes J, Bhandari M. Barriers to breaking bad news among medical and surgical residents. Med Educ 2001;35:197–205. [DOI] [PubMed] [Google Scholar]
- 32.Trude S. So much to do, so little time: physician capacity constraints, 1997-2001. Track Rep 2003;8:1–4. [PubMed] [Google Scholar]
- 33.Kentros C, Barbato C. Using normalized RVU reporting to evaluate physician productivity. Healthc Financ Manage 2013;67:98–105. [PubMed] [Google Scholar]
- 34.Ishaque S, Saleem T, Khawaja FB, Qidwai W. Breaking bad news: exploring patient's perspective and expectations. J Pak Med Assoc 2010;60:407–411. [PubMed] [Google Scholar]
- 35.Panagopoulou E, Mintziori G, Montgomery A, Kapoukranidou D, Benos A. Concealment of information in clinical practice: is lying less stressful than telling the truth? J Clin Oncol 2008;26:1175–1177. [DOI] [PubMed] [Google Scholar]
- 36.Tang WR, Fang JT, Fang CK, Fujimori M. Truth telling in medical practice: students' opinions versus their observations of attending physicians' clinical practice. Psychooncology 2013;22:1605–1610. [DOI] [PubMed] [Google Scholar]
- 37.Milton AC, Mullan B. Views and experience of communication when receiving a serious mental health diagnosis: satisfaction levels, communication preferences, and acceptability of the SPIKES protocol. J Ment Health Abingdon Engl 2017;26:1–10. [DOI] [PubMed] [Google Scholar]
- 38.Tesser A, Rosen S, Tesser M. On the reluctance to communicate undesirable messages (the MUM effect): a field study. Psychol Rep 1971;29:651–654. [Google Scholar]
- 39.Baile WF. Giving bad news. Oncologist 2015;20:852–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Park I, Gupta A, Mandani K, Haubner L, Peckler B. Breaking bad news education for emergency medicine residents: a novel training module using simulation with the SPIKES protocol. J Emerg Trauma Shock 2010;3:385–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Seifart C, Hofmann M, Bär T, Riera Knorrenschild J, Seifart U, Rief W. Breaking bad news-what patients want and what they get: evaluating the SPIKES protocol in Germany. Ann Oncol 2014;25:707–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rabow MW, McPhee SJ. Beyond breaking bad news: how to help patients who suffer. West J Med 1999;171:260–263. [PMC free article] [PubMed] [Google Scholar]
- 43.Narayanan V, Bista B, Koshy C. “BREAKS” protocol for breaking bad news. Indian J Palliat Care 2010;16:61–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Clayton JM, Hancock K, Parker S, et al. Sustaining hope when communicating with terminally ill patients and their families: a systematic review. Psychooncology 2008;17:641–659. [DOI] [PubMed] [Google Scholar]
- 45.Daneault S, Lussier V, Mongeau S, et al. Ultimate journey of the terminally ill: ways and pathways of hope. Can Fam Physician 2016;62:648–656. [PMC free article] [PubMed] [Google Scholar]
- 46.Clayton JM, Hancock KM, Butow PN, et al. Clinical practice guidelines for communicating prognosis and end-of-life issues with adults in the advanced stages of a life-limiting illness, and their caregivers. Med J Aust 2007;186:S77–S105. [DOI] [PubMed] [Google Scholar]
- 47.Taylor JP, Brown RH Jr, Cleveland DW. Decoding ALS: from genes to mechanism. Nature 2016;539:197–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mancuso R, Navarro X. Amyotrophic lateral sclerosis: current perspectives from basic research to the clinic. Prog Neurobiol 2015;133:1–26. [DOI] [PubMed] [Google Scholar]
- 49.Moujalled D, White AR. Advances in the development of disease-modifying treatments for amyotrophic lateral sclerosis. CNS Drugs 2016;30:227–243. [DOI] [PubMed] [Google Scholar]
- 50.Nardo G, Trolese MC, Tortarolo M, et al. New insights on the mechanisms of disease course variability in ALS from mutant SOD1 mouse models. Brain Pathol 2016;26:237–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chiò A, Lauria G. Degenerative neuromuscular diseases: crucial gene and cell machinery discoveries. Lancet Neurol 2016;15:12–13. [DOI] [PubMed] [Google Scholar]
- 52.Petrov D, Mansfield C, Moussy A, Hermine O. ALS clinical trials review: 20 years of failure. Are we any closer to registering a new treatment? Front Aging Neuroscience 2017;9:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kumar V, Islam A, Hassan MI, Ahmad F. Therapeutic progress in amyotrophic lateral sclerosis-beginning to learning. Eur J Med Chem 2016;121:903–917. [DOI] [PubMed] [Google Scholar]
- 54.Aoun SM, Breen LJ, Howting D, et al. Receiving the news of a diagnosis of motor neuron disease: what does it take to make it better? Amyotroph Lateral Scler Front Degener 2016;17:168–178. [DOI] [PubMed] [Google Scholar]