Abstract
Background and Objectives
To evaluate the adoption and perceived utility of video visits for new and return patient encounters in ambulatory neurology subspecialties.
Methods
Video visits were launched in an academic, multi-subspecialty, ambulatory neurology clinic in March 2020. Adoption of video visits for new and return patient visits was assessed using clinician-level scheduling data from March 22 to May 16, 2020. Perceived utility of video visits was explored via a clinician survey and semistructured interviews with clinicians and patients/caregivers. Findings were compared across 5 subspecialties and 2 visit types (new vs return).
Results
Video visits were adopted rapidly; all clinicians (n = 65) integrated video visits into their workflow within the first 6 weeks, and 92% of visits were conducted via video, although this varied by subspecialty. Utility of video visits was higher for return than new patient visits, as indicated by surveyed (n = 48) and interviewed clinicians (n = 30), aligning with adoption patterns. Compared with in-person visits, clinicians believed that it was easier to achieve a similar physical examination, patient-clinician rapport, and perceived quality of care over video for return rather than new patient visits. Of the 25 patients/caregivers interviewed, most were satisfied with the care provided via video, regardless of visit type, with the main limitation being the physical examination.
Discussion
Teleneurology was robustly adopted for both new and return ambulatory neurology patients during the COVID-19 pandemic. Return patient visits were preferred over new patient visits, but both were feasible. These results provide a foundation for developing targeted guidelines for sustaining teleneurology in ambulatory care.

Teleneurology was first used for care of Parkinson disease in the early 1990s, and within a decade, expanded to telestroke, where it improved access and quality of care.1-4 Despite the benefits and advancements in technology, many neurologists have been hesitant to adopt telemedicine across ambulatory subspecialties for numerous reasons: restrictive policies, limited reimbursement, technical and connectivity difficulties, clinician credentialing, liability requirements, and required in-person evaluations before virtual care.1-3,5-11 The severe acute respiratory syndrome coronavirus 2 (COVID-19) pandemic prompted widespread telemedicine usage to protect patients and health care workers.12-17 Many barriers were lifted with the loosening of US federal regulations on reimbursements, licensing, and Health Insurance Portability and Accountability Act compliance, as well as health care systems increasing institutional and financial support of telemedicine during the pandemic.18,19
Well-established patients with chronic conditions have generally been deemed the best-case use for ambulatory teleneurology.20 Although follow-up visits have been the mainstay of ambulatory teleneurology care, studies have demonstrated that it is also feasible for new patient visits.3,5,6,21,22 Neurology patients are interested in and satisfied with video visits for follow-up care,20,23,24 but less is known about perceptions of video for new patient consultations, which were uncommon prepandemic.3,25 Furthermore, ambulatory neurology subspecialties and patient needs are diverse.2,7,26 Therefore, the compelled widespread implementation of video visits presented a unique opportunity to pragmatically evaluate the adoption and perceived utility of video for new and return patient encounters among multiple ambulatory neurology subspecialties. Our study provides insights on how to use this technology for different visit types, set expectations, and plan for the postpandemic standard of care.
Methods
Setting and Video Visit Implementation
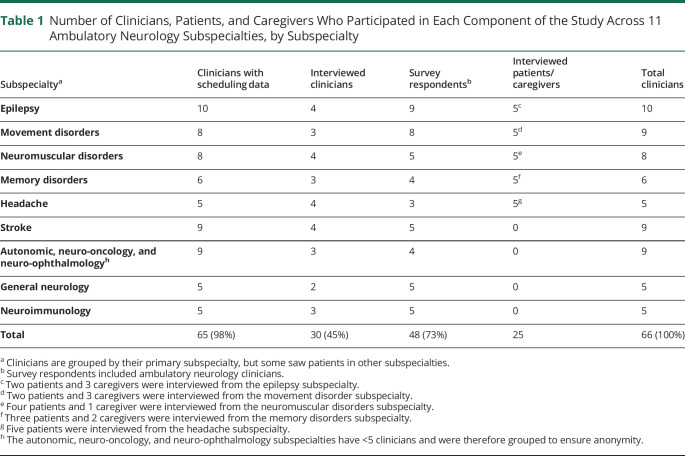
In response to the COVID-19 pandemic stay-at-home orders, Stanford University's Department of Neurology and Neurological Sciences (Stanford, CA) accelerated the implementation of a telemedicine quality improvement initiative across all its ambulatory clinics.16,17 The department includes 68 clinicians (60 physicians and 8 nurse practitioners) in 11 ambulatory subspecialties (Table 1). Stanford's Neurology clinics provide general and subspecialized neurology care in the Bay Area and Northern California with over 60,000 outpatient visits annually. The clinics also serve as one of the largest referral centers for highly subspecialized neurologic care in the United States. The rapid video visit implementation process, rapid adaptations, and clinicians' perceptions of acceptability, appropriateness, and sustainability of telemedicine across the clinic have been previously described.16,17 In brief, all clinicians were given access to video visit–enabled hardware to facilitate conversion of as many in-person visits to video visits as possible. Although voluntary, the clinic encouraged reserving in-person visits for procedures, such as botulinum injections, programming of implanted stimulators, autonomic testing, EMG, and EEGs, or patients deemed to require in-person assessment (e.g., after an initial video visit or as requested by the clinician or patient).
Table 1.
Number of Clinicians, Patients, and Caregivers Who Participated in Each Component of the Study Across 11 Ambulatory Neurology Subspecialties, by Subspecialty
Primary Aims and Evaluation Design
The primary aim of this evaluation is to investigate the adoption and perceived utility (by clinicians and patients/caregivers) of video visits for new and return patient encounters across ambulatory neurology subspecialties using scheduling data. Furthermore, we compare adoption across 5 subspecialties with large outpatient volumes and wide variation in the degree of reliance on the physical examination. We also explore patients', caregivers' and clinicians' perspectives on the acceptability and perceived utility of video visits with a clinician survey and interviews with clinicians and patients/caregivers. Surveys and interviews were conducted with clinicians across all subspecialties. Interviews were conducted with patients/caregivers in 5 subspecialties: epilepsy, headache, memory disorders, movement disorders, and neuromuscular disorders. We limited patient/caregiver interviews to these subspecialties to balance time and resources while purposefully aiming to capture a breadth of neurologic conditions that have variable dependence on the physical examination.
Scheduling Data Inclusion Criteria and Analysis
Clinician-level scheduling data were used to assess early adoption of video visits in the 8-week period: March 22, 2020, through May 16, 2020. The week of March 15, 2020, was the first week of the regional stay-at-home orders and was thus excluded as a transition period. Data were extracted for all clinicians who conducted at least 1 patient visit via video during the 8-week study period. Visit types that required the patient to attend the clinic in-person and could not be converted to video (e.g., procedures) were excluded. Included visit types, herein referred to as “All Patient Visits,” were further categorized into “New Patient Visits” or “Return Patient Visits.”
Adoption was assessed in 2 ways: (1) the proportion of visits completed via video during the COVID-19 pandemic and (2) the proportion of all “expected” visits completed via video. Expected visits volume was the estimated number of visits completed had COVID-19 not occurred and was based on data from an analogous 8-week period in 2019, specifically March 24 through May 18. This estimate of expected visit volume was used as the denominator to evaluate the proportion of visits that were saved or recuperated by telemedicine in the context of the COVID-19 pandemic and stay-at-home orders. The proportion of expected visits completed in person and lost potential visits was also reported. We calculated the proportion of expected visits overall and separately for the 5 subspecialties of interest.
Clinician Survey and Analysis
We developed a novel survey to assess clinicians' perspectives of the perceived utility of video visits in the context of new and return patient visits, the pandemic, and the clinical setting.17 The survey was administered to all neurology clinicians via Stanford's REDCap platform.27 A pair of questions asked clinicians to identify the percentage of new and return patient visits, respectively, that they thought were appropriate for video visits using a visual analogue scale with anchors of 0% of the time and 100% of the time (Table 2). Five additional question pairs (10 questions) addressed the utility of video visits for new and return patient visits with regard to the (1) physical examination, (2) patient history, (3) patient-clinician rapport, (4) visit time, and (5) quality of care, using a 5-point Likert scale (Table 2).
Table 2.
Select Questions From the 20-Item Neurology Video Visit Survey Administered to Clinicians Electronically via the REDCap Survey Tool
Clinicians indicating that they did not use video visits were excluded from survey analyses. Mean percentage ± SDs were calculated for visual analogue scale questions, and p values were calculated using t tests assuming unequal variance. Responses to Likert scale questions were recoded to differentiate 2 levels of agreement: (1) “Never,” “Rarely,” or “Sometimes” and (2) “Often” or “Always.” The percentage of participants indicating “Often” or “Always” for each question was calculated; χ2 tests or Fisher exact tests (if expected cell size ≤5) were conducted for each question pair to calculate p values comparing the percentage of “Often”/“Always” responses for new vs return patient visits. All quantitative analyses were conducted using SAS (version 9.4; SAS Institute, Inc., Cary, NC) and/or R (version 4.0.2).28-32
Clinician and Patient/Caregiver Interviews and Analysis
Semistructured interview guides were designed to capture perceived utility of video visits.33 A purposive sample of 47 clinicians who completed at least 1 video visit were selected and sent an email invitation (and 2 reminders) to participate in 15- to 30-minute qualitative, semistructured phone interviews. Clinicians who responded to the email were interviewed in March and April 2020.
Qualitative semistructured phone interviews were also held with a stratified random sample of patients/caregivers within the 5 subspecialties of interest between March and July 2020. Patients who completed a neurology video visit during the weeks of April 13 and 24, 2020, were identified from managerial reporting tools and included in a stratified randomized patient calling list. Patients were stratified by subspecialty and randomized. The 229 neurology patients (headache [n = 50], memory disorders [n = 29], movement disorders [n = 50], neuromuscular disorders [n = 50], and epilepsy [n = 50]) on the list were called once at random. If the participant answered the phone, they were invited to participate in a 15-minute phone interview. Whenever the patient did not answer the phone, the next patient on the list was called. When the predetermined goal of between 25 and 30 patients/caregivers was reached, data collection ended. A caregiver or family member was interviewed if the patient had severely impaired cognition or speech.
Data from interview transcripts and notes were analyzed using a deductive and inductive approach to derive codes informed by the implementation outcomes of interest.33 Other barriers, facilitators, and emergent themes were identified and coded as appropriate throughout analysis. Interview summaries were used to support a multiphase analysis approach leveraging rapid analytic procedures to extract early themes, consensus coding of transcripts, and a matrix analysis.34 Initially, individual interview transcripts were summarized independently by 3 team members. After review and consensus discussion, transcript summaries were consolidated into a matrix to identify themes and allow comparison across participants and subspecialties. To ensure clinician and patient anonymity in reporting results, identifiable information was removed from all transcripts, and subspecialties with <5 clinicians were grouped.
Mixed Methods Analysis
To comprehensively understand converging and diverging issues regarding the utility of video visits in ambulatory neurology, scheduling data, clinician survey data, and qualitative interview data were consolidated throughout analysis and interpreted in parallel. This approach harnesses the strengths and offsets the weaknesses of each methodology.35,36
Standard Protocol Approvals, Registrations, and Patient Consents
The project was given a human subjects nonresearch determination by Stanford University's Institutional Review Board (IRB-55644). Nevertheless, all interviewees were informed about the interview's purpose and asked to provide verbal consent to participate and be recorded. They were assured that their responses would remain confidential and that any identifiable information would be removed during analysis and reporting. Whenever interviewees did not consent to the recording, detailed interview notes were taken instead.
Data Availability
The data that support the findings of this study are available from the corresponding author on reasonable request.
Results
Of the 68 clinicians in the department's 11 ambulatory subspecialties, 2 clinicians did not conduct any patient visits during the 8-week study period, and 1 clinician lacked scheduling data from 2019. Thus, 65 clinicians were included in the analyses of scheduling data (Table 1). Forty-eight clinicians responded to the survey, and 30 clinicians were interviewed, with interviews lasting an average of 25 minutes. Twenty-five patients/caregivers (5 per subspecialty) were interviewed, and interviews lasted an average of 17 minutes. Interviews were conducted an average of 32 days (SD = 20, range = 15–76 days) after their video visit with an ambulatory neurology provider. Nine patient/caregiver interviews were based on their experience as a new patient, and 16 were return patient visits.
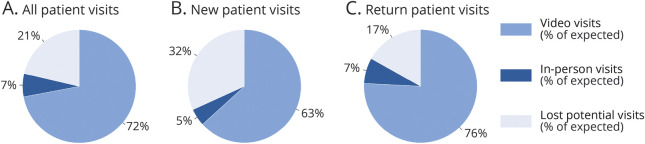
Adoption of Video Visits
During the stay-at-home orders, ambulatory neurology clinicians (n = 65) were able to recuperate most of expected visit volume based on 2019 data (Figure 1A) through widespread utilization of video visits (72% of expected visits) and parsimonious use of in-person visits (7% of expected visits). Of the visits completed during the stay-at-home orders, 92% were completed via video. Across all subspecialties, video visit adoption was high for both new and return patient visits (93% and 91% of completed visits, respectively). Compared with 2019, however, clinicians completed a smaller proportion of expected volume of total new patient visits (Figure 1B) than return patient visits (Figure 1C), 68% vs 83%, respectively.
Figure 1. Percent of Completed Video and In-Person Visits and Lost Potential Visits Across 11 Ambulatory Neurology Subspecialties Is Shown for All Patient Visits, New Patient Visits, and Return Patient Visits.
The percent of video and in-person visits completed by ambulatory neurology providers (n = 65) and their patients during the 2020 stay-at-home orders is based on the expected visit volume, which was derived from visit volume during the corresponding time period in 2019. Each pie chart (100%) represents the expected visit volume based on the 2019 data. The medium blue slice shows the percentage of visits completed via video in 2020 of the expected visit volume. The dark blue slice shows the percentage of visits completed in-person in 2020 of the expected visit volume. The light blue slice shows the percentage of visits that occurred in 2019 but not in 2020 (i.e., percent lost potential visits). Video visits were completed on the EPIC Hyperspace Platform. Figure 1 was previously published and can be reproduced under the terms of Creative Commons Attribution 4.0 license.17
Video visit adoption, however, varied between the 5 subspecialties investigated in greater detail (Figure 2, A–O). Movement disorders and epilepsy had the lowest adoption of video visits overall (61% and 62% of expected visits, respectively), whereas headache and memory disorders had ≥95% video utilization. For new patient visits, neuromuscular disorders had the lowest adoption, with 33% of expected new patient visits completed via video, whereas headache had the highest adoption, with 99% of new patient visits conducted via video. In comparison, for return patient visits, movement disorders had the lowest adoption of video at 60% of expected visits compared with headache and memory disorders with 93% and 96% of return patient visits conducted via video, respectively.
Figure 2. Percent of Completed Video and In-Person Visits and Lost Potential Visits for All Patient Visits, New Patient Visits, and Return Patient Visits Is Presented for the 5 Ambulatory Neurology Subspecialties: Headache (n = 5), Memory Disorders (n = 8), Movement Disorders (n = 8), Neuromuscular Disorders (n = 8), and Epilepsy (n = 10).
The percent of video and in-person visits completed by providers in patients in 5 ambulatory neurology subspecialties during the 2020 stay-at-home orders based on expected visit volume. Expected visit volume was derived from visit volume during the corresponding time period in 2019. Each pie chart (100%) represents the expected visit volume. The medium blue slice shows the percentage of visits completed via video in 2020 of the expected visit volume. The dark blue slice shows the percentage of visits completed in-person in 2020 of the expected visit volume. The light blue slice shows the percentage of visits that occurred in 2019 but not in 2020 (i.e., percent lost potential visits). An “*” indicates that 2020 visit volume was greater than the expected visit volume derived from 2019. For all patient visits, headache achieved 120% of the expected patient visit volume, and memory achieved 110% of expected visits.
Perceived Utility of Video Visits
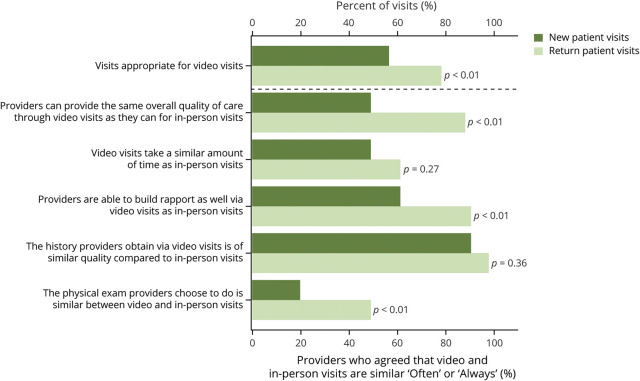
Forty-eight clinicians (73%) responded to the survey. Seven of these respondents, however, indicated that they had not seen new patients via video and were, therefore, excluded from survey analyses comparing perspectives on new and return patient visits. Figure 3 illustrates the findings from the clinician survey. On average, surveyed clinicians perceived that a larger proportion of return patient visits were more conducive for video visits than new patient visits (78% ± 18% vs 56% ± 33%, p < 0.01).
Figure 3. Perceptions of Ambulatory Neurology Clinicians (n = 65) Were Assessed via Survey That Captured the Percent of Video Visits Appropriate for New and Return Patients and Perceived Utility of Video Visits for New vs Return Patient Visits Compared With In-Person, Clinic Visits.
The survey assessed 5 areas of utility: perceived quality of care, visit time, clinician-patient rapport, patient history, and physical examination. Differences in the percentage of visits appropriate for video between new and return patient visits were determined with a t test. Clinician responses to questions on a 5-point Likert scale were recoded to 2 levels of agreement: (1) “Never,” “Rarely,” or “Sometimes” and (2) “Often” or “Always,” and the percent of clinicians reporting the latter is reported. Differences between new and return visits on the 5 utility aspects were tested with χ2 tests or Fisher exact tests (if expected cell size ≤5).
Similarly, just over half of interviewed providers indicated that return patient encounters are more suited for video visits than new patients, and they would prefer to see new patients in-person if possible before determining whether further follow-up care could be provided over video. Nevertheless, some believed it possible to deliver care to both new and follow-up patients via video. Clinician 9 noted that:
[Video visits are] good for a lot of people for follow-up visits. New visits are a little harder … because we can't examine people. … Although a lot of times, that doesn't really matter either. We can still manage their care.
In contrast, patients/caregivers were generally in favor of video visits and rarely expressed a specific preference for an in-person visit, even when meeting a clinician for the first time. Many patients/caregivers wished to be offered a hybrid of in-person and video visits, depending on their needs at the time of the visit. Patient/caregiver 23 (a caregiver to a 20-year-old patient who had an epilepsy new visit) emphasized that:
[A]ccess to health care, especially for populations that are special needs like my son, is so important. So, having that [video visits] as an option was amazing. … you don't have to be seen in person all the time and sometimes video can be just as effective.
Clinicians' and patients' views on the utility of video visits for new and return visits are presented below over the same 5 domains as the survey questions: (1) quality of care, (2) visit time, (3) patient-provider rapport, (4) patient history, and (5) physical examination. Exemplar quotes have been extracted to support our findings and are presented in Table 3.
Table 3.
Additional Exemplary Quotes From Clinician (n = 30) and Patient/Caregiver Interviews (n = 25) by Domains for Utility of Teleneurology for New and Return Patient Visits in Ambulatory Neurology
Quality of Care
The percentage of clinicians who agreed (“Often” or “Always” in the survey) that the perceived quality of care delivered via video was similar to that of an in-person visit was higher for return patient visits (88%) than new patient visits (49%) (p < 0.01; Figure 3). Similarly, interviewed clinicians also indicated that perceived quality of care was similar between video and in-person, more frequently for return than new patient visits. The limiting factors were the ability to build patient-clinician rapport and perform a standard physical examination, although much of the examination could be completed on video. Patients and caregivers, however, were generally satisfied with the quality of care received via video, regardless of visit type. According to patient/caregiver 21 (a 24-year-old, female patient who had an epilepsy return visit):
It was still really good quality… she was definitely making sure it was as much like an in person [visit] as possible.
Visit Length
Of the surveyed clinicians, the percent of those who agreed that video visits took a similar amount of time to in-person visit did not differ between new (61%) and new (49%) patient visit types (p = 0.27; Figure 3). Yet, the views of interviewed clinicians were mixed. Although some clinicians found that not having to room patients and the focused nature of video was more time efficient, others dealt with connectivity issues dividing their focus and thus lengthening the visit time. Patients, however, found video visits to be considerably more time efficient than in-person visits, saving time commuting and in the waiting room. Many also noted that clinicians had fewer competing priorities and could devote their full attention to the visit. They felt that the visit was not rushed and the clinician gave them sufficient time to address queries, which increased their satisfaction with the quality of care received. Patient/caregiver 11 (a 77-year-old patient who had a memory disorders new patient visit) remarked that:
…what's good about a video visit is that providers really slotted for this time to see you. …there's no beepers going off …no knocking on the door, getting the physician to help with some other problem happening in the clinic.
Patient-Clinician Rapport
The percentage of clinicians surveyed who agreed that the ability to build patient-clinician rapport during a video visit was similar to that of an in-person visit was higher for return visits (90%) than new patient visits (61%) (p < 0.01; Figure 3). Interviewed clinicians generally believed that video (vs phone) allowed for better communication and patient experience, but they noted that it is harder to build rapport with new patients than patients with whom they have an established relationship. Connecting with patients on an emotional level was considered more taxing over video. According to Clinician 25:
…it's a lot easier to do the video visit with return patients because we already have a really well-established rapport. There's already a lot of trust built and you don't have to spend your effort trying to do that over a video. … Whereas newer patients … they haven't really connected with the doctor. … Having the in-person ability to make that connection and build that physician-patient trust … it's just harder to do on video and I think those people are better served in person.
Conversely, few new patients struggled to develop a relationship with their clinician. Both new and follow-up patients were often satisfied with the interaction and pleased by the level of engagement and professionalism that clinicians exhibited. A few patients, however, yearned for human and physical connection that was not possible over video. The biggest deterrents were the inability to maintain eye contact and read nonverbal cues, which made the visit impersonal. Patient/caregiver 15 (a 71-year-old female patient who had a memory disorders return visit) expressed that:
Virtual things can only go so far. After a while you want to hug somebody or shake somebody's hand and say thank you while having eye contact.
Patient History
The percentage of clinicians surveyed who agreed that their ability to obtain a patient history in video visits was similar to that of an in-person visit did not differ between return (98%) and new (90%) patient visits (p = 0.36; Figure 3). In fact, interviewed clinicians indicated that video visits were ideal to obtain a medical history across all visit types and subspecialties. For new patient visits, obtaining a superior medical history was a means by which clinicians attempted to compensate for the limitations of the virtual physical examination. Clinician 15 described how:
…what I'm doing is really mostly history. …I'm asking them when their last seizures were, how often they were, how often they're having them, how the meds are working, whether they are having side effects. Even in clinic, I frequently do a limited exam on the follow-ups, and so those patients are perfect for it.
Physical Examination
The percentage of clinicians surveyed who agreed that the virtual physical examination was similar to the in-person examination was higher when asked about return visits (49%) than new patient visits (20%; p < 0.01; Figure 3). Similarly, interviewed clinicians generally agreed that video visits are better suited for stable, uncomplicated, and established patients and visits that require a quick checkup without extensive examination or testing. For new patient visits, acute cases, patients with declining health, or persons in need of periodic procedures or extensive physical examinations, most interviewed clinicians agreed that the limited physical examination made them less suited for video. Nonetheless, several epilepsy and memory disorders clinicians felt that both new and return patients can be seen over video without impacting care. Clinician 8 mentioned how fortunate they are:
I'm fortunate in that usually the physical exam is normal in epilepsy, and when it isn't normal, it's in the area of mental status with memory and confusion problems that can be easily assessed in a video visit. Or in shakiness or unsteady gait or eye movement abnormalities, which also were observable.
Patients and caregivers also voiced that the main drawback to video visits is the physical examination limitations. This was more prevalent among neuromuscular and movement disorders patients and caregivers (almost all of whom were follow-up visits) who expressed that they did not want video visits to replace in-person visits completely. Patient/caregiver 4 (a 63-year-old male patient who a neuromuscular disorders return visit) reflected that:
The only thing that's really missing is the ability to touch and feel, and see. … Being able to test reflexes, being able to test motion in arm, legs, foot… things that … only happen if somebody's actually doing it versus just describing it.
Nevertheless, both new and follow-up patients appreciated being offered video visits should there be no need to attend the clinic in person. Like clinicians, many patients with memory disorders and epilepsy conveyed less need for in-person physical examinations because their consultations are typically mainly discursive.
Discussion
Video visits were rapidly adopted and used for both new and return patients by ambulatory neurology clinicians during the COVID-19 pandemic, which allowed clinicians to recuperate most of the expected visit volume and maintain access to care for neurology patients, a high-risk patient population.37 However, video visit utilization varied across subspecialties. Headache and memory had the highest adoption of video visits for both return and new patient visits, whereas neuromuscular disorders had the lowest adoption of video for new patient visits and movement disorders for return patient visits. Clinicians thought video had more utility for return than new patient visits, whereas patients and caregivers were generally satisfied with video regardless of visit type. The physical examination, patient-clinician rapport, and perceived quality of care were considered harder to achieve over video for new patient visits. Visit time and the ability to obtain a patient history did not differ between the 2 visit types. This rapid implementation of teleneurology demonstrates that widespread use of video visits in ambulatory neurology is feasible,17 but also suggests that their potential utility differs between new and return visits and by subspecialties.
Video visits, overall, were adopted at higher rates for return patients than new patients across the ambulatory neurology clinics as well as in 4 of the 5 subspecialties of interest. Thus, clinicians recuperated a higher proportion of expected return than new patient visits. Previous studies have shown that teleneurology is acceptable for return patients but have focused on rural populations with limited access to neurologists and chronic populations with specific diseases prohibiting traveling, such as Parkinson.3,6,17,20,21,23,24,38 Our results support and expand on this, as we demonstrate that video visits can be widely adopted and are perceived to have utility for most return patient visits in an academic, multi-subspecialty ambulatory clinic in a urban/suburban setting. Moreover, although video was adopted less and perceived to have lower utility for new than return patient visits, over 800 new patient visits were successfully completed in the 8-week implementation period. Furthermore, clinicians perceived that half of their new patients would be appropriate for video in the future, and patients and caregivers generally approve of video visits and trust in their physician's recommendation on visit format.
Within the 5 subspecialties investigated, headache and memory disorders completed almost all their new and return patients via video. Adoption was lower and more variable for epilepsy, movement disorders, and neuromuscular disorders subspecialties, but these subspecialties completed over half of new and return visits on video, except for neuromuscular disorders with 33% of new patient visits completed via video. Before the pandemic and the resulting widespread use of telemedicine, Ross et al.26 similarly showed that headache was the leading adopter of video visits in a multi-subspecialty neurology clinic, followed by epilepsy. Movement disorders was a moderate adopter and neuromuscular disorders conducted a negligible number of video visits.26 The 4 adopting subspecialties from this previous study, however, conducted 11%–22% of their visits on video, which is lower than the adoption rates seen in our study for both return (60%–96%) and new (33%–99%) patient visits.26 Our study further supports the particular utility of video visits for headache, memory disorders, and epilepsy, and it adds that for movement disorders and neuromuscular disorders, there is still a place for video visits, just likely at a lower percentage of visits.
Differences in key attributes of visits could explain the discrepancy in the adoption of video between new and return patient visits. Survey results showed that the physical examination, patient-clinician rapport, and perceived quality of care were easier to achieve over video for return vs new patient visits. This is not surprising as clinicians have already established a baseline examination, rapport, and care plan with return patients. For new patients, about half of clinicians believed that they could achieve a similar perceived quality of care and rapport as they could in an in-person visit; whereas only about 20% of clinicians indicated that they could perform a similar physical examination in-person and via video. Video may be most appropriate, accepted, and potentially sustained for new patient visits that primarily focus on patient history, as participating clinicians indicated that video had less impact on this aspect of the visit. For subspecialties that heavily rely on the physical examination, additional clinician training and patient education may be helpful and may impact clinicians' perspectives on the use of telemedicine within their practice. After the study period, the neurology department created and offered professional development webinars on optimal physical examination techniques for video visits and developed internal guidance based on previous research.2,11,13,16,17,39-42 In addition, providing patients with previsit guidance on optimizing the video visit by involving a caregiver and selecting an appropriate space may also improve both clinician's and patients' experience with the virtual physical examination.43,44 Whether this additional training and guidance improves visits has not been investigated, but is an area that could be explored in future research.
Video visits have utility for new and return patient visits in several ambulatory neurology subspecialties.3,6,17,20,21,23,24,26,38 Clinicians and patients generally support use of telemedicine for return patient visits, especially if care is well established and if patient travel is difficult.16,17 New patients with headache, memory disorder, and epilepsy may be good candidates for video visits as their visits focus predominantly on obtaining patient history and discussion of diagnostic implications and management. For patients unable to travel to the clinic, video visits could also be an acceptable option to provide access for new patients and continuity of care for return patients, even if an in-person physical examination would be preferable. Future work is needed to identify and/or assess whether there is an optimal proportion of visits to schedule and complete in video format for each subspecialty. Nonetheless, the strong adoption during the COVID-19 pandemic and positive perceptions of the utility of video visits by both clinicians and patients likely make teleneurology a permanent fixture for ambulatory care.
The main strengths of the study are the utilization of mixed methods to capture the behavior, experience, and perceptions of both clinicians and patients/caregivers in real time and the large-scale implementation across all patient visits in ambulatory neurology. This pragmatic, real-world evaluation has limitations. First, scheduling data did not capture the minority of video visits conducted using a secondary video software platform and visits that reverted to phone calls. As a result, patients interviewed only included those who had successfully completed a video visit. Interviews do not capture the perceptions of those patients/caregivers who completed their visit using different software platforms or whose visit reverted to a phone call due to technical difficulties. Furthermore, given the gap in the time from encounter to interview, it is possible that interviewees were unable to recall all details about their video visit. To mitigate this, the interviewer clarified what visit and provider the interview pertained to before its initiation. In addition, in-depth comparisons across subspecialties were limited by the low number of clinicians per subspecialty. Finally, views of residents and other healthcare staff, such as patient care coordinators and medical assistants, were not included.
The COVID-19 pandemic led to a surge in teleneurology, overcoming previous barriers and hesitancy to broad implementation across patient visit types and neurologic subspecialties.3,6,20,23,24 Clinicians and patients rapidly adopted video visits; the majority of visits conducted during the stay-in-place orders were via video, but more so for return than new patient visits. Adoption, however, varied by subspecialty; headache and memory had the highest levels of adoption between visit types potentially related to less dependence on physical examinations. In general, clinicians and patients indicated that video visits have utility for both new and return patient visits, but clinicians reported that it was easier to achieve usual standards via video for return patients for the physical examination, patient-clinician rapport, and perceived quality of care than for new patient video visits. Thus, video may have the most utility for return patients and new patients with history-focused visits. As pandemic-related restrictions subside, the regression in video visit volume as well as targeted use of video visits should be investigated to understand how clinicians sustain video visits in their practice, especially given the uncertainties of the permanence of pandemic-related expansions in reimbursements.18,19 In addition, future research efforts are needed to better understand the impact of teleneurology on patients' ability to access care as related to the technology, socioeconomic status, and culture and languages. This study, however, does demonstrate that conducting new and return patient visits via video is feasible and provides a foundation for developing targeted guidelines for sustaining teleneurology in ambulatory care.
Acknowledgment
The authors thank Dr. Frank Longo, Dr. Yuen So, Alison Kerr, Sophia Loo, and Dana Gonzales for their support of this clinical innovation. They also thank Dr. David Larson and the leadership of the Improvement Capability Development Program for arranging the partnership between the Department of Neurology & Neurological Sciences and the Evaluation Sciences Unit; They greatly appreciate the efforts of Anna Sophia Lestoquoy and Mae-Richelle Verano interviewing patients.
Appendix. Authors

Study Funding
This project was supported by Stanford Healthcare as part of the Improvement Capability Development Program. The Stanford REDCap platform was used for quantitative survey data collection. The Stanford REDCap platform (redcap.stanford.edu) is developed and operated by Stanford Medicine Research IT team. The REDCap platform services at Stanford are subsidized by (1) Stanford School of Medicine Research Office and (2) the National Center for Research Resources and the National Center for Advancing Translational Sciences, NIH, through grant UL1 TR001085.
Disclosure
The authors report no disclosures relevant to the manuscript. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Hatcher-Martin JM, Adams JL, Anderson ER, et al. Telemedicine in neurology: Telemedicine Work Group of the American Academy of Neurology update. Neurology. 2020;94:30-38. [DOI] [PubMed] [Google Scholar]
- 2.Dorsey ER, Glidden AM, Holloway MR, Birbeck GL, Schwamm LH. Teleneurology and mobile technologies: the future of neurological care. Nat Rev Neurol. 2018;14:285-297. [DOI] [PubMed] [Google Scholar]
- 3.Patel UK, Malik P, DeMasi M, Lunagariya A, Jani VB. Multidisciplinary approach and outcomes of tele-neurology: a review. Cureus. 2019;11:e4410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hubble JP, Pahwa R, Michalek DK, Thomas C, Koller WC. Interactive video conferencing: a means of providing interim care to Parkinson's disease patients. Mov Disord. 1993;8:380-382. [DOI] [PubMed] [Google Scholar]
- 5.Schneider RB, Biglan KM. The promise of telemedicine for chronic neurological disorders: the example of Parkinson's disease. Lancet Neurol. 2017;16:541-551. [DOI] [PubMed] [Google Scholar]
- 6.Hassan A, Dorsey ER, Goetz CG, et al. Telemedicine use for movement disorders: a global survey. Telemed J E Health. 2018;24:979-992. [DOI] [PubMed] [Google Scholar]
- 7.George BP, Scoglio NJ, Reminick JI, et al. Telemedicine in leading US neurology departments. Neurohospitalist. 2012;2:123-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Achey M, Aldred JL, Aljehani N, et al. The past, present, and future of telemedicine for Parkinson's disease. Mov Disord. 2014;29:871-883. [DOI] [PubMed] [Google Scholar]
- 9.Wechsler LR. Advantages and limitations of teleneurology. JAMA Neurol. 2015;72:349-354. [DOI] [PubMed] [Google Scholar]
- 10.Reider-Demer MM, Eliashiv D. Expanding the use of telemedicine in neurology: a pilot study. J Mob Technol Med. 2018;7:46-50. [Google Scholar]
- 11.Bashshur R, Doarn CR, Frenk JM, Kvedar JC, Woolliscroft JO. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemed J E Health. 2020;26:571-573. [DOI] [PubMed] [Google Scholar]
- 12.Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382:1679-1681. [DOI] [PubMed] [Google Scholar]
- 13.Grossman SN, Han SC, Balcer LJ, et al. Rapid implementation of virtual neurology in response to the COVID-19 pandemic. Neurology. 2020;94:1077-1087. [DOI] [PubMed] [Google Scholar]
- 14.Reeves JJ, Hollandsworth HM, Torriani FJ, et al. Rapid response to COVID-19: health informatics support for outbreak management in an academic health system. J Am Med Inform Assoc. 2020;27:853-859. Accessed May 5, 2020. academic-oup-com.stanford.idm.oclc.org/jamia/advance-article/doi/10.1093/jamia/ocaa037/5811358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020 [online]. Geneva: World Health Organization; 2020. Accessed April 23, 2020. who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 [Google Scholar]
- 16.Yang L, Brown-Johnson CG, Miller-Kuhlmann R, et al. Accelerated launch of video visits in ambulatory neurology during COVID-19: key lessons from the Stanford experience. Neurology. 2020;95:305-311. [DOI] [PubMed] [Google Scholar]
- 17.Saliba-Gustafsson EA, Miller-Kuhlmann R, Kling SMR, et al. Rapid implementation of video visits in neurology during COVID-19: a mixed methods evaluation. J Med Internet Res. 2020;22:e24328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Waldman G, Mayeux R, Claassen J, et al. Preparing a neurology department for SARS-CoV-2 (COVID-19): early experiences at Columbia University Irving Medical Center and the New York Presbyterian Hospital in New York City. Neurology. 2020;94:886-891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guidon AC, Amato AA. COVID-19 and neuromuscular disorders. Neurology. 2020;94:959-969. [DOI] [PubMed] [Google Scholar]
- 20.Davis LE, Harnar J, LaChey-Barbee LA, Pirio Richardson S, Fraser A, King MK. Using teleneurology to deliver chronic neurologic care to rural veterans: analysis of the first 1,100 patient visits. Telemed J E Health. 2019;25:274-278. [DOI] [PubMed] [Google Scholar]
- 21.Chua R, Craig J, Wootton R, Patterson V. Randomised controlled trial of telemedicine for new neurological outpatient referrals. J Neurol Neurosurg Psychiatry. 2001;71:63-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Agarwal S, Warburton EA. Teleneurology: is it really at a distance? J Neurol. 2011;258:971-981. [DOI] [PubMed] [Google Scholar]
- 23.Cheung L, Norden J, Harrington RA, Desai SA. New delivery model for rising-risk patients: the forgotten lot? Telemed J E Health. 2017;23:649-653. [DOI] [PubMed] [Google Scholar]
- 24.Davis LE, Coleman J, Harnar J, King MK. Teleneurology: successful delivery of chronic neurologic care to 354 patients living remotely in a rural state. Telemed J E Health. 2014;20:473-477. [DOI] [PubMed] [Google Scholar]
- 25.Bashiri M, Greenfield LJ, Oliveto A. Telemedicine interest for routine follow-up care among neurology patients in Arkansas. Telemed J E Health. 2016;22:514-518. [DOI] [PubMed] [Google Scholar]
- 26.Ross L, Bena J, Bermel R, et al. Implementation and patient experience of outpatient teleneurology. Telemed J E Health. Epub 2020 Jun 23. [DOI] [PMC free article] [PubMed]
- 27.REDCap Home Page [online]. Google Data Studio. Accessed June 5, 2020. datastudio.google.com/reporting/17evFt8UqrGNAmLlB4i5PScKrAXDiPWDb/page/TDxq?feature=opengraph [Google Scholar]
- 28.R: The R Project for Statistical Computing [online]. Accessed June 25, 2020. r-project.org/ [Google Scholar]
- 29.Auguie B, Antonov A. gridExtra: Miscellaneous Functions for “Grid” Graphics [online]. 2017. Accessed June 25, 2020. CRAN.R-project.org/package=gridExtra [Google Scholar]
- 30.Wickham H, Pedersen TL, RStudio. gtable: Arrange “Grobs” in Tables [online]. 2019. Accessed June 25, 2020. CRAN.R-project.org/package=gtable [Google Scholar]
- 31.Urbanek S, Horner J. Cairo: R Graphics Device Using Cairo Graphics Library for Creating High-Quality Bitmap (PNG, JPEG, TIFF), Vector (PDF, SVG, PostScript) and Display (X11 and Win32) Output [online]. 2020. Accessed June 25, 2020. CRAN.R-project.org/package=Cairo [Google Scholar]
- 32.Barthelme S, Tschumperle D, Wijffels J, Assemlal HE, Ochi S. imager: Image Processing Library Based on “CImg” [online]. 2020. Accessed June 25, 2020. CRAN.R-project.org/package=imager [Google Scholar]
- 33.Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38:65-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Averill JB. Matrix analysis as a complementary analytic strategy in qualitative inquiry. Qual Health Res. 2002;12:855-866. [DOI] [PubMed] [Google Scholar]
- 35.Tariq S, Woodman J. Using mixed methods in health research. JRSM Short Rep. 2013;4:2042533313479197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bekhet AK, Zauszniewski JA. Methodological triangulation: an approach to understanding data. Nurse Res. 2012;20:40-43. [DOI] [PubMed] [Google Scholar]
- 37.GBD 2015 Neurological Disorders Collaborator Group. Global, regional, and national burden of neurological disorders during 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 2017;16:877-897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dorsey ER, Deuel LM, Voss TS, et al. Increasing access to specialty care: a pilot, randomized controlled trial of telemedicine for Parkinson's disease. Mov Disord. 2010;25:1652-1659. [DOI] [PubMed] [Google Scholar]
- 39.Craig JJ, McConville JP, Patterson VH, Wootton R. Neurological examination is possible using telemedicine. J Telemed Telecare. 1999;5:177-181. [DOI] [PubMed] [Google Scholar]
- 40.Ansary AM, Martinez JN, Scott JD. The virtual physical exam in the 21st century. J Telemed Telecare. Epub 2019 Nov 6. doi: 10.1177/1357633X19878330. [DOI] [PubMed]
- 41.Awadallah M, Janssen F, Körber B, Breuer L, Scibor M, Handschu R. Telemedicine in general neurology: interrater reliability of clinical neurological examination via audio-visual telemedicine. Eur Neurol 2018;80:289-294. [DOI] [PubMed] [Google Scholar]
- 42.Blue R, Yang AI, Zhou C, et al. Telemedicine in the era of coronavirus disease 2019 (COVID-19): a neurosurgical perspective. World Neurosurg. 2020;139:549-557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Boes CJ, Leep Hunderfund AN, Martinez-Thompson JM, et al. A primer on the in-home teleneurologic examination: a COVID-19 pandemic imperative. Neurol Clin Pract. 2021;11(2):e157-e164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.American Academy of Neurology. Telemedicine and COVID-19 Implementation Guide. Minneapolis: American Academy of Neurology; 2020:1-9. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author on reasonable request.