Abstract
Introduction
Corona virus disease (Covid-19) affects the airways and induces pulmonary lesions, patients with this disease require oxygen therapy as the disease progresses. Several oxygenation options have been used, l’HFNO had showed beneficial effects
The objective of this study
To evaluate the efficacy of high-flow nasal oxygen HFNO versus non-invasive ventilation in COVID-19.
Methods
This is a retrospective and comparative study conducted over a period of 10 months from March 2020 to December 2020 and involving 600 patients hospitalized in the intensive care unit of the CHU Mohammed VI of Oujda for the management of acute respiratory failure caused by COVID-19.
Results
Out of 600 patients with acute respiratory failure, 265 patients were included in the analyses. 162 (61.10%) patients were treated with HFNO, the intubation rate was 49.7% (80 patients out of 162) of which 63 died intubated (78.8%). Concerning the 82 non-intubated patients, only 16 died (19.8%).
The total number of patients who received NIV was 71 (26.8%), 33 (46.5%) required mechanical ventilation. In-hospital mortality in patients treated with NIV was 100%.
The difference in mortality outcome between the two groups was significantly (P < 0.0001) reduced in HFNO.
Conclusions
Treatment with high-flow oxygen improved survival in patients with acute hypoxemic respiratory failure compared with noninvasive ventilation, although no difference was observed in intubation rate
Keywords: COVID-19, High-flow nasal oxygen therapy, Non-invasive ventilation, Acute respiratory failure, Intensive care unit
1. Introduction
SARS-CoV-2 pneumonia manifests as acute respiratory failure, which most often requires oxygen supplementation. In severely affected patients, the need for oxygen is sometimes so great that it can lead to invasive mechanical ventilation, a procedure that is associated with a high mortality rate [1].
At the beginning of the pandemic, the indications for intubation of patients with COVID-19 were broad [1]. However, as more experience was gained, practitioners began to use high-flow nasal oxygen therapy as an alternative to too early intubation. This method provides humidified and heated oxygen with a FiO2 of up to 100% and a flow rate of up to 80L/min. This would decrease the work of breathing, decrease dead space, improve mucociliary clearance and give a PEEP effect of 2–7 mmHg [2].
This technique of high flow nasal oxygen therapy was at the beginning of the pandemic limited to a flow of 30L/min [3] because the learned societies feared a high contamination of the nursing staff through the aerosol droplets. Today, this hypothetical risk is questioned, and this means of oxygen supplementation has become widespread in intensive care units, as it would reduce the rate of mechanical ventilation in patients with hypoxemic respiratory failure [4].
This work is a retrospective observational study that aims to evaluate mortality in patients on high-flow nasal oxygen therapy and the possible risk of resorting to invasive mechanical ventilation in these patients.
2. Materials and methods
This is a monocentric retrospective observational study conducted in the Intensive Care Unit of the Mohammed VI Public University Hospital of Oujda.
It includes all patients (600 patients) hospitalized in intensive care infected with COVID-19 from March 1st, 2020, to December 31st, 2021.
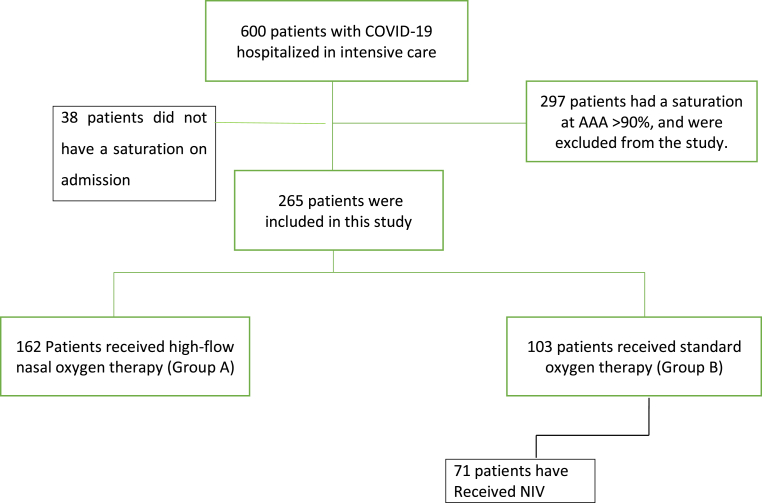
These 600 patients were divided into 2 groups: group A which includes the 162 patients who were put on high flow nasal oxygen therapy and group B including the remaining 103 patients who received standard oxygen therapy (SO).
Patients with room air saturation >90% or did not have saturation at admission were excluded from the study (335 patients) (see Fig. 1).
Fig. 1.
Patient inclusion criteria in our study.
Epidemiological, clinical, paraclinical, therapeutic and evolutionary data were collected thanks to an exploitation form including the different variables collected from the patients' medical files. The data were then computerized and analyzed using SPSS software.
Access to patient data was authorized by the Mohammed VI University Hospital, given the retrospective design of this study, the requirement for patient consent was waived. Data anonymity was respected in accordance with national and international guidelines.
The aim of our work is to describe the use of high flow oxygen therapy in the initial management of patients admitted to the intensive care unit on admission, to study their mortality and the possible use of invasive mechanical ventilation in these patients.
This case series has been reported in line with the PROCESS Guideline [5].
Research registry 6573.
3. Results
Between March 1 and December 31, 600 patients were admitted to the ICU for management of acute respiratory failure due to COVID-19 pneumonia.
Of these, 162 (61.1%) patients were placed on high-flow nasal oxygen therapy (HFNO) on admission (group A), while 103 patients received other means of oxygen supplementation (group B) such as oxygen spectacles, high-concentration masks, non-invasive ventilation or invasive mechanical ventilation.
In group A (HFNO), there were 117 men (72.2%) and 45 women (27.8%). The mean age was 66.3 years (±12.8) and the mean BMI was 27.5 kg/m2 (±4).
The pathological history was dominated by hypertension (43.2%), diabetes (30.9%), and heart disease (12.3%).
On admission, the average saturation of the patients was 82.3% (±7) at AAA and their PaO2 was on average 53.03 (±17).
Concerning the degree of pulmonary lesions on the CT scan, 8 patients (5.1%) had degree of lesions between 10 and 25%, 19 patients (11.4%) had between 25 and 50%, 66 (41.1%) patients had between 50 and 75% and 69 (42.4%) had >75%.
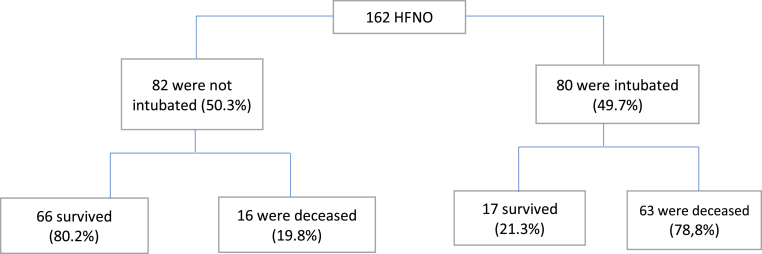
Among these 162 patients who benefited from HFNO, we had recourse to invasive mechanical ventilation in 80 patients (49.7%) of whom 63 died intubated (78.8%).
Concerning the 82 non-intubated patients of group A (50.3%) only 16 died (19.8%).
In addition, in the 71 patients who benefited from NIV in group B, there were 49 men (69.0%) and 22 women (31%). Their mean age was 64.66 years (±14.97) and their BMI was 27.49 kg/m2 (±4.93).
They were hypertensive in 33.8%, diabetic in 26.8%, and had underlying heart disease in 7.0%.
Their initial saturation was on average 81.84% (±7.96) at AAA and their mean PaO2 was 52.53 (±11.95).
The degree of parenchymal involvement was in 4 patients (5.8%) 10–25%, in 9 patients (13.0%) 25–50%, in 26 patients (37.7%) 50–75% and in 32 patients (43.5%) it was >75%.
The total number of patients who received NIV was 71 (26.8%), 33 (46.5%) required mechanical ventilation. The evolution of these intubated patients was marked by death in 27 cases (81.8%) (see Fig. 2).
| Groupe A (N = 162) | Groupe B with NIV (N = 71) | |
|---|---|---|
| Gender -nb (%) | ||
| -male (%) | 117 (72,2%) | 49 (69,00%) |
| -Female (%) | 45 (27,8%) | 22 (31,0%) |
| Age-years (SD) | 66,32 (±12,8) | 64,66 (±14,97) |
| BMI-kg/m2 (SD) | 27,59 (±4,67) | 27,49 (±4,93) |
| Antecedents -nb (%) | ||
| -HTA | 70 (43,2%) | 24 (33,8%) |
| -Diabetes | 50 (30.9%) | 19 (26,8%) |
| -Heart disease | 20 (13.3%) | 5 (7.0%) |
| Saturation at admission -% (SD) | 82,34% (±7,07) | 81,48 (±7,96) |
| Initial PaO2 (SD) | 53,03 (±17,03) | 81,48 (±7,96) |
| Thoracic CT -nb (%) | ||
| −10–25% | 8 (5,1%) | 4 (5,8%) |
| −25–50% | 19 (11,4%) | 9 (13,0%) |
| −50–75% | 66 (41,1%) | 26 (37,7%) |
| ->75% | 69 (42.4%) | 32 (43,5) |
| Use of intubation | 80 (49,7%) | 33 (46.5%) | pValue = 0.08 |
|---|---|---|---|
| Mortality: | |||
| - Total: | 79 (98.6%) | 34 (100%) | pValue <.0001 |
| Intubated patients | 63 (78.8%) | 27 (81.6%) | |
| Non-intubated patients | 16 (19.8%) | 17 (18.4) | |
Fig. 2.
Progression of patients on high-flow nasal oxygen therapy.
4. Discussion
This retrospective study of 233 cases shows, in a population of severe COVID-19 patients with acute respiratory distress syndrome, that an initial oxygenation strategy including the use of high-flow nasal oxygen therapy is associated with a lower mortality rate (98.6% in the HFNO group versus 100% in the NIV group; p < 0.0001).
In addition, neither non-invasive ventilation nor high-flow oxygen decreased the rate of invasive mechanical ventilation in these patients (49.7% in the ONHD group versus 46.5% in the NIV group; p = 0.08).
In a multicenter, randomized, open-label trial of COVIDS patients hospitalized in an intensive care unit (ICU), the rate of intubation was 38% in the high oxygen flow group (80 or 49.7% in our study), compared with 50% in the non-invasive ventilation group (33 or 46.5% in our study). The use of mechanical ventilation was therefore not significant for our two studies (p = 0.18 for this trial, and p = 0.08 for our study) [6].
In contrast, in a recent large French retrospective observational study, 74% of patients receiving standard oxygen therapy were eventually intubated, compared with 51% in the HFNO group. The use of mechanical ventilation was therefore significant in their study (p = 0.007) [7].
Concerning mortality, it was not significant in their study (12% in the HFNO group vs 16% in the OS group, p = 0.017), whereas it was significant in our study 98.6% vs 100% (p<. 0001), and also in the above trial with a relative risk of death was 2.50 (95% CI, 1.31 to 4.78) in the noninvasive ventilation group vs the high oxygen flow group (P = 0.006; P = 0.02 by log-rank test).
Administration of high-flow nasal oxygen therapy was not available in our department before the first wave of COVID-19 in our country in March 2020. At the request of the health care team, the resuscitation department of the university hospital has acquired several HFNO devices of the Ergo, Philips and Hamilton type (Hamilton reaching 80L/min) that can deliver heated and humidified air through an intranasal cannula. This delivers a flow rate ranging from 60 to 80L/min. The FiO2 was adjusted to achieve an O2 saturation greater than 92%.
HFNO appeared to have a protective effect, suggesting that avoiding intubation reduced the risk of transmission. More recently, some have recommended the use of HFNO in patients with moderately severe hypoxemia, which may obviate the need for intubation, or at least delay it [8].
HFNO allows patients to feed more easily than other forms of oxygen supplementation, including NIV, and facilitates respiratory/bronchial physical therapy, patients can do prone easily and can continue to talk and interact with family and health care personnel. This is psychologically very important for everyone involved.
Our study has several limitations. First, the analysis of ventilator-free days must be viewed with caution. Indeed, because of an anomalous distribution, the ventilator-free days were not adjusted for potential confounders. Second, this is not a randomized controlled trial. And some data were unavailable and missing during chart collection because this study was retrospective. Therefore, it is important to conduct a more complete and thorough investigation in the future in a prospective sense.
5. Conclusion
In patients with acute respiratory failure caused by COVID19, high flow oxygen is a simple ventilatory support to use, better tolerated and improves survival rate compared to non-invasive ventilation, although no difference was observed in the intubation rate.
Ethical approval
This study was approved by the ethics committee for biomedical research of Oujda of the faculty of medicine and pharmacy of Oujda. informed consent was obtained from the participants.
Sources of funding
None.
Author contribution
Alkouh Rajae: study concept, Data collection; data analysis; writing review & editing. Abdelilah El Rhalete: Study conception, writing review. Merbouh Manal: contributor. Elaidouni Ghizlane: contributor. Berrichi Samia: contributor. Taouihar Salma: contributor. Fatima Zahra Aftiss:contributor. Bkiyar Houssam: supervision and data validation. Abda Naima: Data analysis, supervision and data validation. Housni Brahim: supervision and data validation.
Registration of research studies
This research is registered with the number: Researchregistry6573.
Guarantor
Alkouh Rajae Abdelilah El Rhalete.
Consent
Obtained.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
None.
Acknowledgments
We would like to thank the medical and nursing teams of Mohammed VI University Hospital for their significant involvement in the management of the patients included in our study. Particular thanks to the director of Mohammed VI University Hospital Prof. Abdelkarim Daoudi for his successful management of this outbreak.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2021.103230.
Contributor Information
Rajae Alkouh, Email: akouhrajae1993@gmail.com.
Abdelilah El Rhalete, Email: elrhaleteabdelilah@yahoo.fr.
Merbouh Manal, Email: manal.mrb@gmail.com.
El Aidouni Ghizlane, Email: elaidounighizlane@gmail.com.
Berrichi Samia, Email: sammia9@gmail.com.
Taouihar Salma, Email: salma.taouihar@gmail.com.
Fatima Zahra Aftiss, Email: fatimaaf-13@hotmail.com.
Bkiyar Houssam, Email: 7b.houssam@gmail.com.
Abda Naima, Email: abda.naima@yahoo.com.
Housni Brahim, Email: brahimhousni@yahoo.fr.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Goyal P., Choi J.J., Pinheiro L.C., Schenck E.J., Chen R., Jabri A., Satlin M.J., Campion T.R., Jr., Nahid M., Ringel J.B., Hoffman K.L., Alshak M.N., Li H.A., Wehmeyer G.T., Rajan M., Reshetnyak E., Hupert N., Horn E.M., Martinez F.J., Gulick R.M. Clinical characteristics of covid-19 in New York city. Safford MM N Engl J Med. 2020 Jun 11;382(24):2372–2374. doi: 10.1056/NEJMc2010419. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Frat J.-P., Thille A.W., Mercat A., Girault C., Ragot S., Perbet S., et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N. Engl. J. Med. 2015;372:2185–2196. doi: 10.1056/NEJMoa1503326. ([PubMed]) [DOI] [PubMed] [Google Scholar]
- 3.Staff Safety during Emergency Airway Management for COVID-19 in Hong Kong Jonathan Chun-Hei Cheung 1, Lap Tin Ho 2, Justin Vincent Cheng 2, Esther Yin Kwan Cham 2, Koon Ngai Lam 2, Affiliations expand PMID: 32105633 PMCID: PMC7128208, DOI: 10.1016/S2213-2600(20)30084-9. [DOI] [PMC free article] [PubMed]
- 4.Leung C.C.H., Joynt G.M., Gomersall C.D., Wong W.T., Lee A., Ling L., Chan P.K.S., Lui P.C.W., Tsoi P.C.Y., Ling C.M., Hui M. Comparison of high-flow nasal cannula versus oxygen face mask for environmental bacterial contamination in critically ill pneumonia patients: a randomized controlled crossover trial. J. Hosp. Infect. 2019 Jan;101(1):84–87. doi: 10.1016/j.jhin.2018.10.007. ([PubMed]) [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Sohrabi C., Mathew G., Franchi T., Kerwan A., O'Neill, N for the Process Group The PROCESS 2020 guideline: updating consensus preferred reporting of CasE series in surgery (PROCESS) guidelines. Int. J. Surg. 2020;84:231–235. doi: 10.1016/j.ijsu.2020.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Frat J.P., Thille A.W., Mercat A., Girault C., Ragot S., Perbet S., Prat G., Boulain T., Morawiec E., Cottereau A., Devaquet J., Nseir S., Razazi K., Mira J.P., Argaud L., Chakarian J.C., Ricard J.D., Wittebole X., Chevalier S., Herbland A., Fartoukh M., Constantin J.M., Tonnelier J.M., Pierrot M., Mathonnet A., Béduneau G., Delétage-Métreau C., Richard J.C., Brochard L., Robert R., FLORALI Study Group REVA network. N. Engl. J. Med. 2015 Jun 4;372(23):2185–2196. doi: 10.1056/nejmoa1503326. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. [DOI] [PubMed] [Google Scholar]
- 7.Bonnet N., Martin O., Boubaya M., Levy V., Ebstein N., Karoubi P., Tandjaoui-Lambiotte Y., Van Der Meersch G., Oziel J., Soulie M., Ghalayini M., Winchenne A., Zahar J.R., Ahmed P., Gaudry S., Cohen Y. High flow nasal oxygen therapy to avoid invasive mechanical ventilation in SARS-CoV-2 pneumonia: a retrospective study. Ann. Intensive Care. 2021 Feb 27;11(1):37. doi: 10.1186/s13613-021-00825-5. PMID: 33638752; PMCID: PMC7910764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Créac'hcadec A., Ricordel C., Salé A., Arnouat B., Bizec J.L., Langelot M., Lineau C., Marquette D., Martin F., Lederlin M., Jouneau S. High-flow nasal oxygen: a safe, efficient treatment for COVID-19 patients not in an ICU. Guy T. Eur. Respir. J. 2020 Nov 12;56(5) doi: 10.1183/13993003.01154-2020. 10.1183/13993003.01154-2020. Print 2020 Nov.PMID: 32859678. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.