Abstract
Pyroptosis is a recently identified mechanism of programmed cell death related to Caspase-1 that triggers a series of inflammatory reactions by releasing several proinflammatory factors such as IL-1β and IL-18. The process is characterised by the rupture of cell membranes and the release of cell contents through the mediation of gasdermin (GSDM) proteins. GSDMD is an important member of the GSDM family and plays a critical role in the two pathways of pyroptosis. Diabetic nephropathy (DN) is a microvascular complication of diabetes and a major cause of end-stage renal disease. Recently, it was revealed that GSDMD-mediated pyroptosis plays an important role in the occurrence and development of DN. In this review, we focus on two types of kidney cells, tubular epithelial cells and renal podocytes, to illustrate the mechanism of pyroptosis in DN and provide new ideas for the prevention, early diagnosis and molecular therapy of DN.
Keywords: Diabetic nephropathy, GSDMD, podocytes, pyroptosis, tubular epithelial cells
Introduction
Diabetic nephropathy (DN), one of the main complications of diabetes mellitus (DM), is also the main cause of end-stage renal disease (ESRD) (Ref. 1).
So far, it has been found that cell death exists in the process of DN, such as apoptosis, necrosis, autophagy, pyroptosis, ferroptosis and so on (Refs 2–6). Apoptosis and necrosis were first discovered to be involved in the exploration of the mechanism of DN, whose occurrence is closely related to tumour necrosis factor-α (TNF-α) (Refs 7–13). TNF is a cytokine from the proinflammatory cytokine family (Refs 10, 11). TNF-α, IL-1 and IL-6 are all inflammatory factors released during cell death (Ref. 14). TNF-α, the transmembrane protein, is not only expressed by immune cells, such as monocytes/macrophages (including microglia in the nervous system), B cells, activated T and NK cells, but also by a diverse array of non-immune cells, such as fibroblasts, endothelial cells, epithelial cells and tumour cells (Ref. 15). Transmembrane TNF-α assembles into homotrimers, which are cleaved by matrix metalloproteinase TNF-α converting enzyme (TACE/ADAM17), leading to the releasing of TNF-α homotrimers, which is responsible for the endocrine function of TNF-α (Refs 16, 17). Both forms bind to structurally related but functionally distinct receptors: TNF receptor 1 (TNFR1), which is ubiquitously expressed in almost any cell type at a low level (Refs 18, 19). From the mechanism perspective, TNFR1 is involved in mediating extrinsic apoptosis (Ref. 20). After binding to the ligand TNF, the TNFR1 signalling complex separates from the plasma membrane. In the cytoplasm, the FAS-associated death domain protein (FADD)-bound initiator caspase-8 is recruited to the complex and interacts with receptor-interacting protein kinase 1 (RIPK1) (Refs 21, 22). After caspase-8 is activated, RIPK1 activity is blocked by proteolytic cleavage of RIPK1 by caspase-8 (Ref. 23). Caspase-8 with proteolytic activity is involved in the activation of apoptosis and pyroptosis pathways (Ref. 9).
Pyroptosis, which is a newly discovered type of programmed cell death, has received increasing attention in recent years. Upon the recognition of ‘danger signals’ when the body is exposed to infection, the innate immune system initiates a response that may trigger cell necrosis, apoptosis or pyroptosis to kill the invading microorganisms. As a lytic and inflammatory death that depends on inflammasomes and caspases, pyroptosis is characterised by the rupture of the plasma membrane, swelling and dissolution of cells, which is mediated by the gasdermin (GSDM) protein family. Finally, it leads to the delivery of proinflammatory factors such as IL-1β and IL-18, and the release of cell contents. GSDMD plays a critical role in pyroptosis; therefore, pyroptosis is also defined as GSDM-mediated programmed necrotic cell death (Ref. 24).
Relevant studies have reported that pyroptosis is involved in the occurrence and development of DN (Refs 25–27). To a certain extent, inhibiting the occurrence of pyroptosis equals to alleviating the damage to the kidney in DN. Currently, the pyroptosis signalling pathways involved in the pathogenesis of DN constitute a hot topic. In this review, we summarise the mechanisms of pyroptosis in two types of intrinsic renal cells, tubular epithelial cells (TECs) and renal podocytes, during DN.
The role of GSDMD in pyroptosis
GSDM family
The GSDM family, a protein family with sequence homology, mainly includes GSDM A, B, C, D, E, DFNB59 (Refs 28–30). Most of them can form oligomer and insert into the cellular or mitochondrial membranes to form a hole, except DFNB59, which does not have a domain within a pore-forming activity (Ref. 31).
Both GSDMA and GSDMB are located at human chromosome 17q21.1, while GSDMC and GSDMD at chromosome 8q24. Mice lack Gsdmb, but carry genes encoding three homologs of GSDMA (Gsdma1–3) clustered on chromosome 11, and four homologs of GASDMC (Gsdmc1–4) clustered on chromosome 15 (Ref. 32).
Gsdma3/GSDMA participates in the regulation of cellular apoptosis, autophagy and oxidative stress (OS) (Ref. 32). Lei et al (Ref. 33). found that TNF-α directly leads to the release of Gsdma3, enhancing caspase-3 expression and causing apoptosis. GSDMA, a downstream protein in transforming growth factor-β (TGF-β)-dependent apoptosis, is a potential suppressor of gastric cancer, indicating that GSDMA suppression is required for tumorigenesis in gastric tissue (Ref. 34). LMO1 (LIM domain only 1), a member of the LMO protein family, is a transcriptional regulator. It has different expression patterns in embryonic and adult tissues, indicating that it plays a vital role in expressing different cellular biological functions (Ref. 35). Without the ability of DNA binding, it is believed to interact with other molecules through its LIM domain when playing a role in transcriptional regulation. LMO1 has been confirmed to regulate the expression of GSDM family proteins (Ref. 36). LMO1 targets GSDMA through Runt-related transcription factor 3 and participates in the apoptosis induced by TGF-β, which is accompanied by the release of caspase-3/7 (Ref. 36). In addition, autophagy can be induced by mutations in the Gsdma3 C-terminal domain (Ref. 37). The loss or mutation of the C-terminal domain results in the release of the intrinsic pro-autophagic capability of the N-terminal domain. The N-terminal domain associates with Hsp90 and migrates to mitochondria through the mitochondrial importer receptor Tom70, where it interacts with the mitochondrial chaperone Trap1 and causes an increase in the production of reactive oxygen species (ROS) and in mitochondrial permeability transition (Ref. 38). The specific regulation process of GSDMA is shown in Figure 1.
Fig. 1.
GSDMA is involved in the process of regulating apoptosis and autophagy: TNF-α or TGF-β, LMO1 target to Gsdma3, accompanied by the release of Caspase3/7, leading to the occurrence of apoptosis. The cleavage of Gsdma3 promotes the release of N-terminal and C-terminal. The deletion or mutation of C-terminal makes N-terminal have the ability to participate in the regulation of autophagy. N-terminal interacts with HSP90 and translocates to mitochondria through Tom70, and then associates with Trap1, which results in the massive release of ROS and mitochondrial permeability transition.
GSDMB, which is known as gasdermin-like protein, is composed of 411 amino acids and may cover genes that influence diseases associated with aberrant immune responses (Refs 39, 40). Human GSDMB has six splicing variants, each of which encodes a protein with a molecular weight ranging from 35 to 50 kDa that has different expression profiles and subcellular localization patterns in different cell types. Compared with other gasdermins, these isoforms are weaker and more unstable in terms of their functions and structures (Refs 41, 42). A recent study found that GSDMB can induce pyroptosis-like characteristics, but the mechanism whereby GSDMB activity leads to pyroptosis and participates in the regulation of inflammation needs to be further explored (Ref. 43). Chao et al (Ref. 41). found that GSDMB is not a substrate for inflammatory caspases 1 and 4/5/11 because of its lack of a specific interdomain linker region site. In addition, based on the phospholipid-binding activities of GSDMB and the cleavage profile of caspases, they confirmed that GSDMB proteins are substrates of the executioner caspases-3, -6 and -7, which activate apoptosis, not inflammatory caspases. Panganiban et al (Ref. 44) found that the expression of GSDMB alone does not stimulate pyroptosis. Further experiments indicated that GSDMB is cleaved by caspase-1 at site 236. One of the cleaved forms is the N-terminus of the GSDMB protein, which induces pyroptosis. Chen et al (Ref. 45) reported that the N-terminus of GSDMB does not cause pyroptosis by itself. The binding of full-length GSDMB to the CARD domain of caspase-4 may lead to the oligomerization of caspase-4, which in turn causes conformational changes in caspase-4, thus increasing its enzymatic activity and promoting the cleavage of GSDMD. They also proposed that in non-canonical pyroptosis, the effect of GSDMB on caspase-4 can be halted through a negative feedback mechanism, which may be an essential protective function during immune overreaction to infectious pathogens. Therefore, they believe that the N-terminus of GSDMB does not cause the formation of pores, and that GSDMB causes cell death by enhancing the enzymatic activity of caspase-4. The mechanism whereby GSDMB causes pyroptosis remains, however, to be elucidated. Different studies have reached different conclusions regarding the role of caspases in the cleavage of GSDMB in pyroptosis. Different cell lines and conditions may affect the cleavage site of caspases. However, only the cleavage of GSDMB by a specific caspase at a particular site can produce a pore-forming N-terminus, which may be the reason for the different conclusions. The specific process is shown in Figure 2.
Fig. 2.
GSDMB causes pyroptosis: GSDMB is a substrate of Caspase-3/6/7 and could be cleaved into N-terminal and C-terminal. GSDMB could be cleaved by Caspase-1 at position 236. N-terminal of GSDMB may lead to pyroptosis. Relevent studies suggest that N-terminal of GSDMB cannot form pores, and that the cell death associated with GSDMB is caused by Caspase-4. The combination of GSDMB and the CARD domain of Caspase-4 changes the conformation of Caspase-4, which in turn promotes the lysis of GSDMD, resulting in the occurrence of pyroptosis.
GSDMC, which is expressed in the epithelial cells of many tissues, is involved in controlling various cellular processes, including cell growth and death (Refs 37, 46–50). As illustrated in Figure 3, Hou et al (Ref. 51) demonstrated that the N-terminal domain of GSDMC can induce pyroptosis, and 362LELD365 is the site where caspase-8 cleaves GSDMC. Due to the presence of GSDMC and nuclear programmed death ligand 1 (nPD-L1), TNF-α activates caspase-8 and switches from apoptosis to pyroptosis, leading to tumour necrosis in hypoxic areas. Current research on GSDMC mainly focuses on lumbar spinal stenosis, melanoma, breast cancer, lumbar disc herniation, lung adenocarcinoma, chronic back pain and ultraviolet radiation (Refs 47–54).
Fig. 3.
GSDMC is involved in the regulation of pyroptosis: In the presence of PD-L1, TNF-α induces Caspase-8 to cleave GSDMC at the site of 362LELD365 to generate N-terminal and C-terminal, which further leads to pyroptosis.
GSDME, which is also known as DFNA5, has an apoptosis-inducing activity that depends on the domain structure (Refs 32, 55). A relevant study has illustrated that mutations in DFNA5 significantly enhance ROS production and upregulate several cytochrome c oxidase genes involved in OS (Ref. 56). Moreover, endoplasmic reticulum stress, mitochondrial damage and the MAPK pathway are involved in DFNA5-induced cell death (Refs 57, 58). Further studies have revealed that the DFNA5-NT domain is associated with apoptosis and pyroptosis, which is shown in Figure 4. Caspase-3 is involved in cell apoptosis; however, Wang et al (Ref. 29) found that either TNF-α or chemotherapeutic drugs facilitate the cleavage of DFNA5, leading to the conversion of cell apoptosis to pyroptosis. DFNA5 can be specifically cleaved at its junction by caspase-3 to generate a DFNA5-NT fragment that penetrates the membrane and induces pyroptosis, which suggests that excessive apoptosis with caspase-3 activity can further lead to pyroptosis. Rogers et al (Ref. 30) also confirmed that DFNA5 mutation causes the mitochondria to release cytochrome C, activate caspase-3, and form pores in the plasma membrane. This means that regardless of whether caspase-1 is absent or non-functional, cells will continue undergoing pyroptosis even without GSDMD activation (Ref. 59).
Fig. 4.
DFNA5 is involved in the regulation of apoptosis and pyroptosis: (1) Caspase-8 and Caspase-3 promote the cleavage of DFNA5 into N-terminal and C-terminal, leading to increasing levels of ROS and COX, mitochondrial damages, further causing generation of Cyct and apoptosome, and ultimately leading to apoptosis. (2) TNF or chemotherapeutic drugs induce Caspase-3 to cleave DFNA5 to generate N-terminal and C-terminal, resulting in the pore formation of cell membrane and pyroptosis.
GSDMD is a key factor regulating pyroptosis (Refs 60–62). GSDMD is composed of a 242-amino acid N-terminal domain (GSDMD-NT) and a 199-amino acid C-terminal domain (GSDMD-CT) connected via a 43-amino acid linker. GSDMD-NT can bind to lipids, insert into the cellular membrane, and form pores (Ref. 61), GSDMD-NT is also known as the pore-forming domain. However, under non-stimulating conditions, its pore-forming activity is inhibited by GSDMD-CT; therefore, GSDMD-CT is also known as the repressing domain. In resting cells, the two aromatic amino acids Phe and Trp on the 1–2 loop of GSDMD-NT are bound to the same hydrophobic pocket located on the surface of its C-terminal domain and form autoinhibition structures. In such conditions, GSDMD is in a self-inhibiting state (Ref. 63). When pathogen-associated molecular pattern (PAMP) receptors, such as Toll-like receptors, recognise their ligands, inflammasomes are activated and GSDMD is cleaved by activated caspase-1. The N-terminal and C-terminal regions of GSDMD are dissociated, and the self-inhibiting structure disappears. Consequently, the N-terminus of GSDMD binds to membrane lipids and forms micropores with a diameter of 10–14 nm, resulting in cell rupture and the occurrence of an inflammatory cascade (Ref. 64). GSDMA, GSDMC and GSDMD are all capable of suppressing tumours, whereas GSDMB is considered an oncogene associated with immune diseases, such as childhood-onset asthma (Refs 65, 66). The molecular mechanism of GSDMD regulating the process of pyroptosis is illustrated in Figure 5.
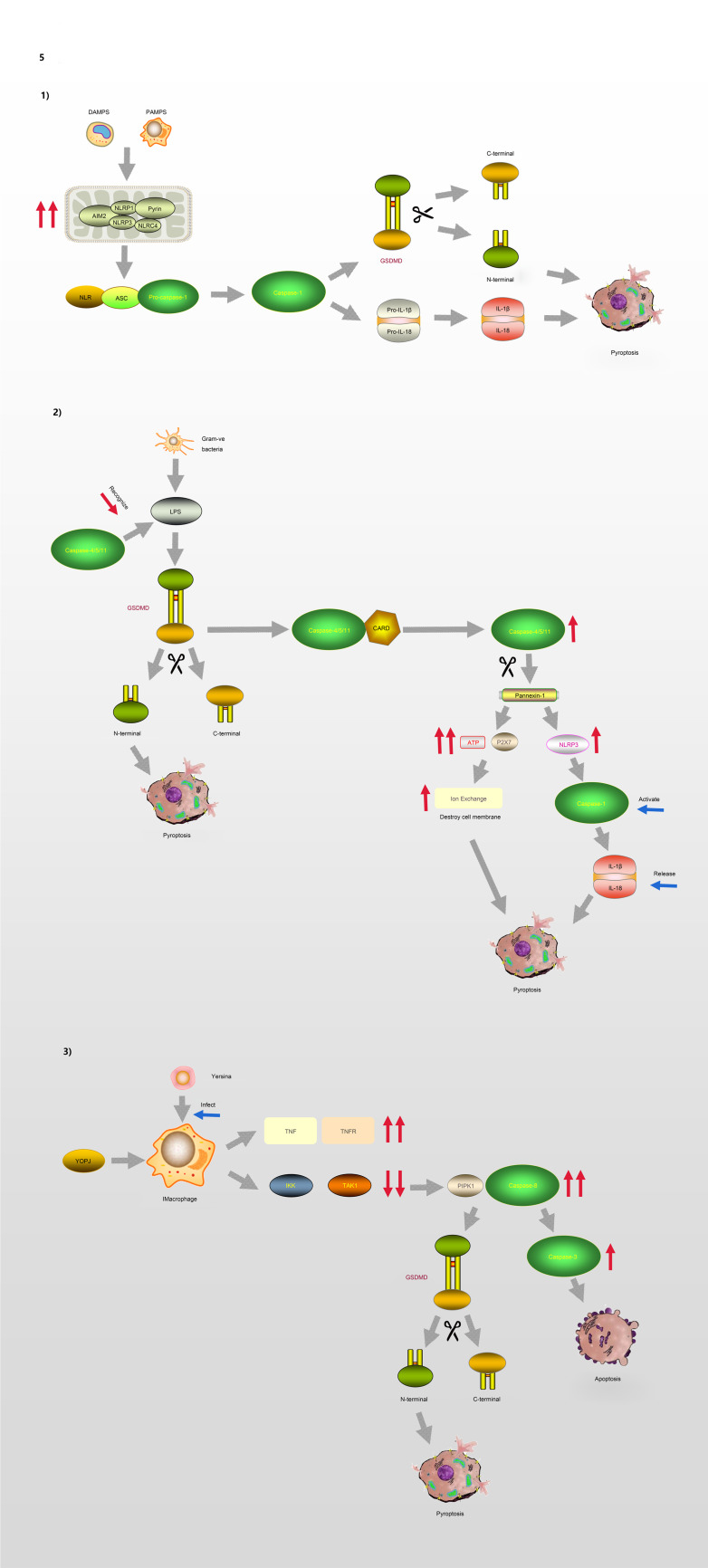
Fig. 5.
Pyroptosis and GSDMD. (1) Canonical pathway: The formation of classic inflammasome containing Caspase-1 on the one hand accelerates the release of IL-18 and IL-1β; on the other hand, it also directly lyses GSDMD, leading to cell membrane pore formation and pyroptosis. (2) Non-canonical pathway: Caspase-4/5/11 cleaves GSDMD and causes pyroptosis. The activation of Caspase-11 cleaves Pannexin-1, thereby destroying the integrity of the cell membrane. In addition, Pannexin-1 activates NLRP3 and participates in the formation of Caspase-1. (3) Model of macrophages infected by Yersina: After activated by Yersina, Caspase-8 cleaves GSDMD at the site of D276, which leads to pyroptosis or apoptosis by activating Caspase-3.
Process and signal transduction of pyroptosis
Currently, two pathways are known to be involved in the regulation of pyroptosis, including the conventional pathway mediated by caspase-1 and a non-canonical pathway regulated by caspase-4/5 (human) and caspase-11 (mouse), which senses intracellular bacterial lipopolysaccharide (LPS) (Refs 67, 68). In response to different types of stimulation, cells initiate pyroptosis through different pathways.
The process of pyroptosis begins with the assembly and integration of inflammasomes. The canonical pathway, which relies on caspase-1, is initiated by PAMP recognition and the activation of inflammasome sensors such as NLRP1b, NLRP3, NLRC4, AIM2 and pyrin (Ref. 69). Thus, inflammasome complexes are generated in immune cells, including macrophages and dendritic cells, under the stimulation of various signals. The complexes are composed of NOD-like receptor proteins (NLRPs) and a framework protein – apoptosis-associated speck-like protein containing a CARD (ASC), precursory caspase-1 (pro-caspase-1) and other related proteins. The framework protein ASC acts as a linker protein that can tightly connect NLRs and pro-caspase-1 via its N-terminal PYD and C-terminal CARD domains, respectively. Subsequently, pro-caspase-1 is activated and cleaved into two subunits, P20 and P10, forming the classic inflammasome containing caspase-1 (Refs 70, 71). On the one hand, upon meeting the inflammasomes, pro-caspase-1 self-cleaves into caspase-1, and because of its catalytic activity, pro-interleukin-1β (Pro-IL-1β) and pro-interleukin-18 (Pro-IL-18) are cleaved, resulting in the inflammatory factors interleukin-1β (IL-1β) and interleukin-18 (IL-18). On the other hand, activated caspase-1 can directly cleave GSDMD, causing the release of GSDMD-NT and consequently, leading to cell membrane pore formation and pyroptosis.
In the non-canonical signalling pathway, caspases-4 and -5 (human) or caspase-11 (mouse) can directly recognise LPS in the cytoplasm and cleave the GSDMD protein, resulting in pyroptosis (Ref. 72). After LPS-induced activation, caspase-11 cleaves pannexin-1, which controls the entry and exit of small molecules, leading to the release of ATP and the opening of the membrane channel P2X7, thereby mediating intracellular potassium efflux and the activation of the NLRP3 inflammasome (Refs 73, 74). In addition, pannesin-1 stimulates NLRP3 in apoptotic cells, promoting the release of IL-1β and the activation of caspase-1 (Refs 75, 76).
Moreover, caspase-8 is involved in the regulation of some infection-related immune pathways (Refs 77–80). A macrophage model of Yersinia infection demonstrated that the induction of pyroptosis by caspase-8 occurs via the hydrolysis and activation of gasdermin (Refs 81, 82). Orning et al (Ref. 81) confirmed that caspase-8 cleaves GSDMD at site D276, and suggested that after Yersinia activates caspase-8, GSDMD may not be the only downstream effector of caspase-8. These findings indicate that there is no strict boundary between the regulation of caspases and their downstream molecules, and that cross-pathway regulation exists in the face of different types of stimuli.
GSDMD governed the pyroptosis involving in the development of DN
DN is an abnormality in the structure and function of the kidneys caused by diabetic chronic microvascular disease, which eventually leads to renal failure and ESRD. High glucose (HG) induces mitochondrial dysfunction, such as mitochondrial dynamics disorder, abnormal biosynthesis and DNA mutations. Various pathophysiological changes act on kidney cells, causing a series of inflammatory reactions. Intrinsic renal cells mainly include TECs and podocytes. The relationships between pyroptosis and DN in these two types of renal cells are described below.
Tubular epithelial cell pyroptosis in DN
To maintain homeostasis, TECs are responsible for reabsorption of the kidneys, transferring some or all the water and several solutes from the tubules to the blood, retaining useful substances, and effectively removing harmful and excess substances. Under HG conditions, TECs are more susceptible to metabolic disorder, inflammation and haemodynamic changes, leading to the release of ROS and a variety of inflammatory factors, which results in renal interstitial inflammation and fibrosis. Relevant studies have reported that the pyroptosis of TECs occurs in the process of acute kidney injury and renal function damage caused by a contrast agent (Ref. 83), which suggests that pyroptosis participates in the occurrence and development of renal tubular damage in kidney disease.
Long non-coding RNAs (lncRNAs) are more than 200 nucleotides in length and only encode a small number of functional short peptides found in eukaryotes. They are important regulatory factors in the development of various diseases, and have been shown to be related to pyroptosis (Refs 84–86). MicroRNAs (miRNAs) are small endogenous non-coding RNAs with a length of approximately 22 nt, which are involved in cell proliferation and differentiation, programmed death, OS and the regulation of inflammation (Ref. 87). They are also recognised as important molecular regulators (Refs 88, 89). LncRNA combine with miRNA through the 3′-UTR region to form a ceRNA structure and participate in the regulation of related pathways. Previous studies have confirmed that lncRNA GAS5 expression is elevated in the serum of DM patients (Ref. 90). Xie et al. investigated the expression and relation of GAS5 and miR-452-5p in HG-induced HK-2 cells, and their effect on inflammation, OS and the pyroptosis of these cells (Ref. 91). They found that after HG treatment, GAS5 expression is reduced in HK-2 cells, while that of miR-452-5p is increased, and that GAS5 may directly target miR-452-5p. In addition, GAS5 overexpression was found to inhibit HG-induced inflammation, OS and pyroptosis through miR-452-5p interference. In this process, GSDMD-NT expression was shown to be upregulated in HG-induced HK-2 cells, which promoted pyroptosis. Moreover, the expression of lncRNA KCNQ1OT1 is increased in patients with diabetic cardiomyopathy, and its inhibition reduces the damage to cardiomyocytes (Ref. 92). On the other hand, it was found that miR-506-3p participates in the regulation of OS (Ref. 93). Zhu et al (Ref. 94) found that the expression of KCNQ1OT1 is increased in HG-induced HK-2 cells and in the plasma of DN patients. In addition, they confirmed that KCNQ1OT1 directly targets miR-506-3p using a luciferase assay. They showed that the expression of miR-506-3p is downregulated in HG-treated HK-2 cells and in the plasma of patients with DN, and that KCNQ1OT1 interference could reduce the levels of caspase-1, NLRP3 and GSDMD-NT by upregulating the expression of miR-506-3p, thereby alleviating inflammation, OS and the pyroptosis of HG-induced HK-2 cells. Therefore, KCNQ1OT1 may be a novel target for the treatment of DN. Metastasis-associated lung adenocarcinoma transcript 1 (MALAT1) is a lncRNA that is widely expressed in mammalian kidney tissues and increased in cancer cells (Ref. 95), and it is related to DM-related pyroptosis. Li et al (Ref. 96) found that MALAT1 expression is significantly increased, while that of miR-23c is decreased, in STZ-induced diabetic rats and HG-induced HK-2 cells. Downregulating the expression of MALAT1 or upregulating that of miR-23c can inhibit pyroptosis in HK-2 cells, and decrease the levels of NLRP3, caspase-1 and the inflammatory factor IL-1β, suggesting that the inhibition of MALAT1 can suppress HG-induced pyroptosis.
In addition to ceRNA, relative research has begun on the regulatory pathway mediated by Toll-like receptor 4 (TLR4). TLR4, a member of the TLR family, plays an important role in activating immune responses. It typically activates the nuclear factor-κB (NF-κB) pathway through MyD88, leading to the release of ROS – which causes OS – and cytokines. TLR4 induces the activation of caspase-1 and the expression of caspase-11, resulting in pyroptosis and the release of pro-inflammatory factors (Ref. 97). Wang et al (Ref. 98) examined TLR4 expression in DN patients and renal tubular cells, and found that increased TLR4 expression was related to renal tubular damage. They found that HG induces increased TLR4 expression, GSDMD cleavage and IL-1β release in vivo and in vitro, and that these effects can be reversed with TLR4 and NF-κB inhibitors. These results indicate that the TLR4/NF-κB signalling pathway is involved in regulating the pyroptosis of TECs in DN. In addition, Pang et al (Ref. 99) confirmed that nuclear factor erythroid-2 related factor 2 (Nrf2)/NLRP3 signalling is involved in the regulation of caspase-1-GSDMD-mediated pyrolysis in HK-2 cells. In addition, Nrf2, a protective factor in DN, attenuates ROS and regulates the redox balance under OS (Refs 100–102). It has been considered as a potential therapeutic target to prevent and reverse the progression of DN (Ref. 103).
Besides the above mechanisms, thioredoxin-interacting protein (TXNIP) regulating the level of ROS to mediate the process of pyroptosis is also an interesting direction. TXNIP is a negative regulator of thioredoxin (TRX). TXNIP–TRX interaction accelerates the generation of intracellular ROS and regulates redox reactions, which are closely related to the OS of the glomeruli (Refs 104, 105) and renal tubules (Ref. 106), and these processes are involved in the progression of DN (Ref. 107). Ke et al (Ref. 108) found that rat renal tubular epithelial NRK-52E cells are activated by the HG-induced TXNIP/NLRP3 axis, thereby inducing inflammation and pyroptosis. After inhibiting endoplasmic reticulum stress-related factors such as inositol-requiring enzyme 1 (IRE1), the expression of miR-200a increased and the expression of TXNIP decreased. Thus, IRE1 may mediate the pyroptosis and renal damage caused by the TXINP/NLRP3 pathway through the degradation of miR-200a. TXNIP also regulates the level of pyroptosis in DN by co-acting with ceRNA. Song et al (Ref. 109) confirmed that elevated levels of lncRNA ANRIL could induce vascular cell apoptosis, aggravate cell inflammation and lead to endothelial cell dysfunction in atherosclerosis. ANRIL and TXINP expression increases, and that of miR-497 decreases, after the induction of HG (Ref. 110). MiR-497, which binds to ANRIL and directly targets TXINP, was found to inhibit the expression of ANRIL, thereby suppressing the activation of TXNIP/NLRP3/caspase-1 and the release of IL-1β and IL-18. By restraining miR-497 or overexpressing TXNIP, the effects that ANRIL knockdown and inhibition of the pyroptosis were reversed (Ref. 110).
Podocyte pyroptosis in DN
Podocytes – terminally differentiated cells located in the outer layer of glomerular capillaries – are composed of a cytoskeleton structure, joint connections and branched foot processes surrounding the glomerular capillaries. Once damaged, they cannot be regenerated. The basal, basolateral and parietal areas together constitute the foot process that adheres to the glomerular filtration barrier through the podoplanin protein. The reticular structure formed by the slit diaphragm between the foot process and the podocytes is involved in various signal transduction pathways in podocytes, which are essential for maintaining the structure of the glomerulus and the filtration function. Abnormal glomerular filtration and damage to podocytes are the core reasons for the development of proteinuria and glomerular sclerosis in DN (Ref. 111). Cheng et al (Ref. 112) found that HG intervention promoted caspase-11 and caspase-4 expression, and the decomposition of GSDMD. The knockout of caspase-11 or GSDMD could significantly improve the deterioration of renal function and the morphological changes of glomeruli and podocytes and alleviate the surging of inflammatory factors.
Mammalian target of rapamycin (mTOR), which is a highly conserved serine/threonine kinase that has been shown to regulate cell growth and proliferation in various in vivo and in vitro models, can combine with NLRP3 to regulate the level of inflammation (Refs 113–115). Studies have confirmed that the expression of NF-κB is highly correlated with the mTOR signalling pathway (Ref. 116), the inhibition of which could protect podocytes and reverse DN by blocking the transdermal differentiation of glomerular mesangium (Ref. 117). Wang et al (Ref. 118) treated podocytes with an mTOR activator/inhibitor and an NF-κB inhibitor, confirming that the mTOR/NLRP3/IL-1β axis is able to suppress podocyte damage in DN.
In addition to the mTOR/NLRP3 signalling pathway, mitochondrial function can also affect the level of inflammation and pyroptosis. SIRT1, a member of the mammalian silent information regulator (SIRT) protein family, is an important deacetylase in the mitochondria and participates in a variety of metabolic processes. Mitochondria can regulate the activation of the inflammasomes involved in pyroptosis (Refs 119, 120). Adenosine 5′-monophosphate (AMP)-activated protein kinase (AMPK) is involved in the regulation of energy metabolism. Activation of the AMPK/SIRT1 pathway can play a protective role in various inflammation-related diseases by inhibiting OS and apoptosis (Refs 121–123). AMPK has been reported to inhibit the expression of NF-κB by increasing SIRT1 levels, thereby reducing inflammation (Ref. 124). Relevant studies have confirmed that AMPK, p-AMPK and SIRT1 levels are significantly reduced in HG-induced podocytes, and that the occurrence of DN may be related to the APMK/SIRT1/NF-κB pathway (Refs 125, 126).
TNF-α-induced protein 3, also known as A20, is a protein encoded by the gene TNFAIP3 that participates in the regulation of inflammatory signals by inhibiting NF-κB, thereby exerting anti-inflammatory effects and protecting tissue cells (Ref. 127), and suppressing the activation of NLRP3 (Ref. 128). Many studies have shown that miR-21-5p promotes the development of inflammation (Refs 129, 130). In addition, miRNA transferred through extracellular vesicles can regulate mRNA levels after entering the cell, thereby influencing a variety of diseases (Refs 131, 132). Ding et al (Ref. 133) proved that miR-21-5p in macrophage-derived extracellular vesicles can regulate podocyte pyroptosis through A20.
The sponge structure formed by lncRNA and miRNA can also be involved in the regulation of podocyte pyroptosis. The lncRNA NEAT1 plays a vital role in the occurrence and development of DN; lncRNA NEAT1 expression is upregulated in both in vivo and in vitro models of DN (Ref. 134), and promotes epithelial-to-mesenchymal transition and kidney fibrosis in DN (Ref. 135). A meta-analysis of miRNA expression profiles in DN showed that at least two studies revealed the downregulation of miR-34c (Ref. 136). Recently, Liu et al (Ref. 137) found that miR-34c inhibits cell death in HG-induced podocytes. Zhan et al (Ref. 138) found that NEAT1 promotes podocyte pyroptosis by regulating miR-34c, whose target was shown to be NLRP3, thus regulating the expression of NLRP3, caspase-1 and IL-1β. These findings highlight the role of the NLRP3/caspase-1/IL-1β axis in DN. Zuo et al (Ref. 139) found that the level of MALAT1 and miR-200c increased, while the level of NRF2 decreased in the mouse podocytes treated with HG. MALAT1, as an upstream factor, affected the expression of miR-200c and NRF2. In addition, the level of OS also changed respectively by interfering with the expression of the three above. They confirmed that MALAT1/miR-200c/NRF2 axis is relative to regulating the pyroptosis and OS of podocyte treated with HG.
Current clinical drugs and potential treatments for DN
The present treatment principles for DN are mainly to control blood sugar and blood pressure, protect kidney function, increase high-quality protein intake, reduce cardiovascular and cerebrovascular and peripheral vascular complications, etc. When it progresses to chronic renal failure, dialysis replacement therapy is needed, whose purpose is to delay its progress. At present, domestic and foreign studies on the clinical hypoglycaemic drugs to reverse the process of DN by inhibiting renal pyroptosis have not yet been fully established, which indicates that the pathogenesis of DN and the exploration of the drug mechanism are incomplete.
At the moment, it has been confirmed that dipeptidyl-peptidase-4 inhibitors saxagliptin inhibits the activation of NLRP3 inflammasomes, downregulates the expression of IL-18 and IL-1β, and avoids inflammation and renal fibrosis (Refs 140, 141). Although it was found that saxagliptin downregulates the level of pyroptotic factors in the process of inhibiting inflammation, whether it protects renal function by inhibiting pyroptosis still needs to be further explored.
Although the mechanism of clinical drugs in inhibiting pyroptosis has not yet been elucidated, potential therapeutic methods regarding their important role in controlling the level of pyroptosis have emerged. Necrosulfonamide (NSA), a pyroptosis inhibitor, has been proved to reduce the level of inflammation through various signalling pathways to inhibit the level of pyroptosis in many diseases such as non-small-cell lung cancer, gastric cancer, pulmonary fibrosis and coronary artery disease (Refs 142–145). It has great prospects, but whether it inhibits the level of renal pyroptosis and delays the deterioration of renal function has not yet been studied. Relative studies might be established to explore whether it plays a reversal role in renal pyroptosis caused by DN. It may become a new hope for the treatment of DN.
Conclusion and outlook
Pyroptosis is one type of cell death that is associated with caspase-1 and accompanied by the releasing of inflammasomes. Under the action of different external stimuli, the cell membrane is punctured via the GSDMD protein through different channels, which leads to cell rupture, necrosis and the flowing out of cell contents. GSDMD-mediated pyroptosis is related to the occurrence and development of DN. This review summarises the relationships between the signalling pathways induced by HG in TECs and renal podocytes, and the process of GSDMD-mediated pyroptosis. However, the pathogenesis of DN is complicated, and many mechanisms are involved in pyroptosis. The specific regulatory network requires further investigation. Currently, the signalling pathways involved in the pyroptosis of other kidney cells, such as glomerular endothelial cells and glomerular mesangial cells, during DN are still unknown. With the gradual improvement of genetic research technology and the continuous expansion of our understanding of in vivo and in vitro functions, we may eventually gain a comprehensive understanding of the pathogenesis of DN caused by pyroptosis, which will result in a new breakthrough in its clinical treatment.
Acknowledgements
This project was supported by the grant from the National Nature Foundation of China (81860156), Science and Technology Project Foundation of Huaian City (No.HABZ201927) and Traditional Chinese Medicine Science and Technology Project Foundation of Jiangsu Province (No.YB2017070). Yi Zuo, Xiaoyun He, Qixiang Shao and Caiping Xue conceived and designed this study. Yi Zuo, Li Chen and Huiping Gu participated in manuscript writing. All authors made a significant contribution to the work and approved the submitted version.
Conflict of interest
None.
References
- 1.Ayinde KS et al. (2020) AMPK allostery: a therapeutic target for the management/treatment of diabetic nephropathy. Life Sciences 261, 118455. [DOI] [PubMed] [Google Scholar]
- 2.Chen XC et al. (2021) Lysosome depletion-triggered autophagy impairment in progressive kidney injury. Kidney Dis (Basel) 7, 254–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Duan JY et al. (2021) Ferroptosis and its potential role in metabolic diseases: a curse or revitalization? Frontiers in Cell and Developmental Biology 9, 701788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al Mamun A et al. (2021) Pyroptosis in diabetic nephropathy. Clinica Chimica Acta 523, 131–143. [DOI] [PubMed] [Google Scholar]
- 5.Sifuentes-Franco S et al. (2018) Oxidative stress, apoptosis, and mitochondrial function in diabetic nephropathy. International Journal of Endocrinology 2018, 1875870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hu H et al. (2020) C1q/tumor necrosis factor-related protein-9 attenuates diabetic nephropathy and kidney fibrosis in db/db mice. DNA and Cell Biology 39, 938–948. [DOI] [PubMed] [Google Scholar]
- 7.Obeng E (2021) Apoptosis (programmed cell death) and its signals – a review. Brazilian Journal of Biology 81, 1133–1143. [DOI] [PubMed] [Google Scholar]
- 8.Vanden Berghe T et al. (2013) Determination of apoptotic and necrotic cell death in vitro and in vivo. Methods 61, 117–129. [DOI] [PubMed] [Google Scholar]
- 9.Tonnus W et al. (2021) The role of regulated necrosis in endocrine diseases. Nature Reviews. Endocrinology 17, 497–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jurisic V et al. (2011) TNF-alpha induced apoptosis is accompanied with rapid CD30 and slower CD45 shedding from K-562 cells. Journal of Membrane Biology 239, 115–122. [DOI] [PubMed] [Google Scholar]
- 11.Jurisic V et al. (2006) Effect of TNF-alpha on Raji cells at different cellular levels estimated by various methods. Annals of Hematology 85, 86–94. [DOI] [PubMed] [Google Scholar]
- 12.Jurisic V et al. (2004) Modulation of TNF-alpha activity in tumor PC cells using anti-CD45 and anti-CD95 monoclonal antibodies. Cancer Letters 214, 55–61. [DOI] [PubMed] [Google Scholar]
- 13.Jurisic V et al. (2004) TNF-alpha induces changes in LDH isotype profile following triggering of apoptosis in PBL of non-Hodgkin's lymphomas. Annals of Hematology 83, 84–91. [DOI] [PubMed] [Google Scholar]
- 14.Jurisic V (2020) Multiomic analysis of cytokines in immuno-oncology. Expert Review of Proteomics 17, 663–674. [DOI] [PubMed] [Google Scholar]
- 15.Sedger LM and McDermott MF (2014) TNF and TNF-receptors: from mediators of cell death and inflammation to therapeutic giants – past, present and future. Cytokine & Growth Factor Reviews 25, 453–472. [DOI] [PubMed] [Google Scholar]
- 16.Black RA et al. (1997) A metalloproteinase disintegrin that releases tumour-necrosis factor-alpha from cells. Nature 385, 729–733. [DOI] [PubMed] [Google Scholar]
- 17.Moatti A and Cohen JL (2021) The TNF-alpha/TNFR2 pathway: targeting a brake to release the anti-tumor immune response. Frontiers in Cell and Developmental Biology 9, 725473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Puimege L, Libert C and Van Hauwermeiren F (2014) Regulation and dysregulation of tumor necrosis factor receptor-1. Cytokine & Growth Factor Reviews 25, 285–300. [DOI] [PubMed] [Google Scholar]
- 19.Pegoretti V et al. (2018) Selective modulation of TNF-TNFRs signaling: insights for multiple sclerosis treatment. Frontiers in Immunology 9, 925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krammer PH, Arnold R and Lavrik IN (2007) Life and death in peripheral T cells. Nature Reviews Immunology 7, 532–542. [DOI] [PubMed] [Google Scholar]
- 21.Ofengeim D and Yuan J (2013) Regulation of RIP1 kinase signalling at the crossroads of inflammation and cell death. Nature Reviews Molecular Cell Biology 14, 727–736. [DOI] [PubMed] [Google Scholar]
- 22.Vanden Berghe T et al. (2014) Regulated necrosis: the expanding network of non-apoptotic cell death pathways. Nature Reviews Molecular Cell Biology 15, 135–147. [DOI] [PubMed] [Google Scholar]
- 23.Newton K et al. (2019) Cleavage of RIPK1 by caspase-8 is crucial for limiting apoptosis and necroptosis. Nature 574, 428–431. [DOI] [PubMed] [Google Scholar]
- 24.Shi J, Gao W and Shao F (2017) Pyroptosis: gasdermin-mediated programmed necrotic cell death. Trends in Biochemical Sciences 42, 245–254. [DOI] [PubMed] [Google Scholar]
- 25.Zhao W, He C and Wang F (2020) [Screening potential Chinese materia medica and their monomers for treatment diabetic nephropathy based on caspase-1-mediated pyroptosis]. Nan Fang Yi Ke Da Xue Xue Bao 40, 1280–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tian D et al. (2019) The effect of A1 adenosine receptor in diabetic megalin loss with caspase-1/IL18 signaling. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy 12, 1583–1596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gu J et al. (2019) Sodium butyrate alleviates high-glucose-induced renal glomerular endothelial cells damage via inhibiting pyroptosis. International Immunopharmacology 75, 105832. [DOI] [PubMed] [Google Scholar]
- 28.Rogers C et al. (2017) Cleavage of DFNA5 by caspase-3 during apoptosis mediates progression to secondary necrotic/pyroptotic cell death. Nature Communications 8, 14128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang Y et al. (2017) Chemotherapy drugs induce pyroptosis through caspase-3 cleavage of a gasdermin. Nature 547, 99–103. [DOI] [PubMed] [Google Scholar]
- 30.Rogers C et al. (2019) Gasdermin pores permeabilize mitochondria to augment caspase-3 activation during apoptosis and inflammasome activation. Nature Communications 10, 1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shi J et al. (2015) Cleavage of GSDMD by inflammatory caspases determines pyroptotic cell death. Nature 526, 660–665. [DOI] [PubMed] [Google Scholar]
- 32.Qiu S, Liu J and Xing F (2017) ‘Hints’ in the killer protein gasdermin D: unveiling the secrets of gasdermins driving cell death. Cell Death & Differentiation 24, 588–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lei M et al. (2012) Gsdma3 is a new factor needed for TNF-alpha-mediated apoptosis signal pathway in mouse skin keratinocytes. Histochemistry and Cell Biology 138, 385–396. [DOI] [PubMed] [Google Scholar]
- 34.Zheng Z et al. (2020) Gasdermins: pore-forming activities and beyond. Acta Biochim Biophys Sin (Shanghai) 52, 467–474. [DOI] [PubMed] [Google Scholar]
- 35.Kenny DA et al. (1998) Identification and characterization of LMO4, an LMO gene with a novel pattern of expression during embryogenesis. Proceedings of the National Academy of Sciences of the USA 95, 11257–11262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Saeki N et al. (2007) GASDERMIN, suppressed frequently in gastric cancer, is a target of LMO1 in TGF-beta-dependent apoptotic signalling. Oncogene 26, 6488–6498. [DOI] [PubMed] [Google Scholar]
- 37.Shi P et al. (2015) Loss of conserved Gsdma3 self-regulation causes autophagy and cell death. Biochemical Journal 468, 325–336. [DOI] [PubMed] [Google Scholar]
- 38.Lin PH et al. (2015) N-terminal functional domain of Gasdermin A3 regulates mitochondrial homeostasis via mitochondrial targeting. Journal of Biomedical Science 22, 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Das S, Miller M and Broide DH (2017) Chromosome 17q21 genes ORMDL3 and GSDMB in asthma and immune diseases. Advances in Immunology 135, 1–52. [DOI] [PubMed] [Google Scholar]
- 40.Li L, Li Y and Bai Y (2020) Role of GSDMB in pyroptosis and cancer. Cancer Management and Research 12, 3033–3043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chao KL, Kulakova L and Herzberg O (2017) Gene polymorphism linked to increased asthma and IBD risk alters gasdermin-B structure, a sulfatide and phosphoinositide binding protein. Proceedings of the National Academy of Sciences of the USA 114, E1128–E1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ruan J (2019) Structural insight of gasdermin family driving pyroptotic cell death. Advances in Experimental Medicine and Biology 1172, 189–205. [DOI] [PubMed] [Google Scholar]
- 43.Feng S, Fox D and Man SM (2018) Mechanisms of gasdermin family members in inflammasome signaling and cell death. Journal of Molecular Biology 430, 3068–3080. [DOI] [PubMed] [Google Scholar]
- 44.Panganiban RA et al. (2018) A functional splice variant associated with decreased asthma risk abolishes the ability of gasdermin B to induce epithelial cell pyroptosis. Journal of Allergy and Clinical Immunology 142, 1469–1478.e1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen Q et al. (2019) GSDMB promotes non-canonical pyroptosis by enhancing caspase-4 activity. Journal of Molecular Cell Biology 11, 496–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tamura M and Shiroishi T (2015) GSDM family genes meet autophagy. Biochemical Journal 469, e5–e7. [DOI] [PubMed] [Google Scholar]
- 47.Jiang H et al. (2020) Two GWAS-identified variants are associated with lumbar spinal stenosis and Gasdermin-C expression in Chinese population. Scientific Reports 10, 21069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kusumaningrum N et al. (2018) Gasdermin C is induced by ultraviolet light and contributes to MMP-1 expression via activation of ERK and JNK pathways. Journal of Dermatological Science 90, 180–189. [DOI] [PubMed] [Google Scholar]
- 49.Kusumaningrum N et al. (2018) Ultraviolet light-induced gasdermin C expression is mediated via TRPV1/calcium/calcineurin/NFATc1 signaling. International Journal of Molecular Medicine 42, 2859–2866. [DOI] [PubMed] [Google Scholar]
- 50.Wu J et al. (2020) Association of GSDMC polymorphisms with lumbar disc herniation among Chinese Han population. International Journal of Immunogenetics 47, 546–553. [DOI] [PubMed] [Google Scholar]
- 51.Hou J et al. (2020) PD-L1-mediated gasdermin C expression switches apoptosis to pyroptosis in cancer cells and facilitates tumour necrosis. Nature Cell Biology 22, 1264–1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shou Y et al. (2020) Identification of signatures of prognosis prediction for melanoma using a hypoxia score. Frontiers in Genetics 11, 570530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wei J et al. (2020) Overexpression of GSDMC is a prognostic factor for predicting a poor outcome in lung adenocarcinoma. Molecular Medicine Reports 21, 360–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Suri P et al. (2018) Genome-wide meta-analysis of 158,000 individuals of European ancestry identifies three loci associated with chronic back pain. PLoS Genetics 14, e1007601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Op de Beeck K et al. (2011) The DFNA5 gene, responsible for hearing loss and involved in cancer, encodes a novel apoptosis-inducing protein. European Journal of Human Genetics 19, 965–973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Van Rossom S et al. (2012) The splicing mutant of the human tumor suppressor protein DFNA5 induces programmed cell death when expressed in the yeast Saccharomyces cerevisiae. Frontiers in Oncology 2, 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Van Rossom S et al. (2015) The deafness gene DFNA5 induces programmed cell death through mitochondria and MAPK-related pathways. Frontiers in Cellular Neuroscience 9, 231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wu J et al. (2020) Programmed cell death pathways in hearing loss: a review of apoptosis, autophagy and programmed necrosis. Cell Proliferation 53, e12915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schneider KS et al. (2017) The inflammasome drives GSDMD-independent secondary pyroptosis and IL-1 release in the absence of caspase-1 protease activity. Cell Reports 21, 3846–3859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chen X et al. (2016) Pyroptosis is driven by non-selective gasdermin-D pore and its morphology is different from MLKL channel-mediated necroptosis. Cell Research 26, 1007–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Liu X et al. (2016) Inflammasome-activated gasdermin D causes pyroptosis by forming membrane pores. Nature 535, 153–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.He WT et al. (2015) Gasdermin D is an executor of pyroptosis and required for interleukin-1beta secretion. Cell Research 25, 1285–1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liu Z et al. (2019) Crystal structures of the full-length murine and human gasdermin D reveal mechanisms of autoinhibition, lipid binding, and oligomerization. Immunity 51, 43–49.e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ding J et al. (2016) Pore-forming activity and structural autoinhibition of the gasdermin family. Nature 535, 111–116. [DOI] [PubMed] [Google Scholar]
- 65.Zihlif M et al. (2016) Association between gasdermin A and gasdermin B polymorphisms and susceptibility to adult and childhood asthma among Jordanians. Genetic Testing and Molecular Biomarkers 20, 143–148. [DOI] [PubMed] [Google Scholar]
- 66.Acevedo N et al. (2015) Risk of childhood asthma is associated with CpG-site polymorphisms, regional DNA methylation and mRNA levels at the GSDMB/ORMDL3 locus. Human Molecular Genetics 24, 875–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lin J et al. (2020) New insights into the mechanisms of pyroptosis and implications for diabetic kidney disease. International Journal of Molecular Sciences 21, 7057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Al Mamun A et al. (2021) Role of pyroptosis in spinal cord injury and its therapeutic implications. Journal of Advanced Research 28, 97–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Aglietti RA and Dueber EC (2017) Recent insights into the molecular mechanisms underlying pyroptosis and gasdermin family functions. Trends in Immunology 38, 261–271. [DOI] [PubMed] [Google Scholar]
- 70.Hu Z and Chai J (2016) Structural mechanisms in NLR inflammasome assembly and signaling. Current Topics in Microbiology and Immunology 397, 23–42. [DOI] [PubMed] [Google Scholar]
- 71.Lu A and Wu H (2015) Structural mechanisms of inflammasome assembly. FEBS Journal 282, 435–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ding J and Shao F (2017) SnapShot: the noncanonical inflammasome. Cell 168, 544–544.e541. [DOI] [PubMed] [Google Scholar]
- 73.Yang D et al. (2015) Caspase-11 requires the pannexin-1 channel and the purinergic P2X7 pore to mediate pyroptosis and endotoxic shock. Immunity 43, 923–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Xu Z et al. (2020) Distinct molecular mechanisms underlying potassium efflux for NLRP3 inflammasome activation. Frontiers in Immunology 11, 609441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chen KW, Demarco B and Broz P (2020) Pannexin-1 promotes NLRP3 activation during apoptosis but is dispensable for canonical or noncanonical inflammasome activation. European Journal of Immunology 50, 170–177. [DOI] [PubMed] [Google Scholar]
- 76.Chen KW et al. (2019) Extrinsic and intrinsic apoptosis activate pannexin-1 to drive NLRP3 inflammasome assembly. EMBO Journal 38, e101638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mascarenhas DPA et al. (2017) Inhibition of caspase-1 or gasdermin-D enable caspase-8 activation in the Naip5/NLRC4/ASC inflammasome. PLoS Pathogens 13, e1006502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rauch I et al. (2017) NAIP-NLRC4 inflammasomes coordinate intestinal epithelial cell expulsion with eicosanoid and IL-18 release via activation of caspase-1 and -8. Immunity 46, 649–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Philip NH et al. (2014) Caspase-8 mediates caspase-1 processing and innate immune defense in response to bacterial blockade of NF-kappaB and MAPK signaling. Proceedings of the National Academy of Sciences of the USA 111, 7385–7390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Weng D et al. (2014) Caspase-8 and RIP kinases regulate bacteria-induced innate immune responses and cell death. Proceedings of the National Academy of Sciences of the USA 111, 7391–7396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Orning P et al. (2018) Pathogen blockade of TAK1 triggers caspase-8-dependent cleavage of gasdermin D and cell death. Science (New York, N.Y.) 362, 1064–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sarhan J et al. (2018) Caspase-8 induces cleavage of gasdermin D to elicit pyroptosis during Yersinia infection. Proceedings of the National Academy of Sciences of the USA 115, E10888–E10897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zhang Z et al. (2018) Caspase-11-mediated tubular epithelial pyroptosis underlies contrast-induced acute kidney injury. Cell Death & Disease 9, 983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Li J et al. (2018) LncRNA GAS5 suppresses ovarian cancer by inducing inflammasome formation. Bioscience Reports 38, BSR20171150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zhang Y et al. (2018) Melatonin prevents endothelial cell pyroptosis via regulation of long noncoding RNA MEG3/miR-223/NLRP3 axis. Journal of Pineal Research 64. [DOI] [PubMed] [Google Scholar]
- 86.Han Y et al. (2018) Low-dose sinapic acid abates the pyroptosis of macrophages by downregulation of lncRNA-MALAT1 in rats with diabetic atherosclerosis. Journal of Cardiovascular Pharmacology 71, 104–112. [DOI] [PubMed] [Google Scholar]
- 87.Hata A and Lieberman J (2015) Dysregulation of microRNA biogenesis and gene silencing in cancer. Science Signaling 8, re3. [DOI] [PubMed] [Google Scholar]
- 88.Trionfini P, Benigni A and Remuzzi G (2015) MicroRNAs in kidney physiology and disease. Nature Reviews. Nephrology 11, 23–33. [DOI] [PubMed] [Google Scholar]
- 89.Li R et al. (2014) MicroRNAs in diabetic kidney disease. International Journal of Endocrinology 2014, 593956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Carter G et al. (2015) Circulating long noncoding RNA GAS5 levels are correlated to prevalence of type 2 diabetes mellitus. BBA Clinical 4, 102–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Xie C et al. (2019) lncRNA GAS5/miR-452-5p reduces oxidative stress and pyroptosis of high-glucose-stimulated renal tubular cells. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy 12, 2609–2617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yang F et al. (2018) LncRNA KCNQ1OT1 mediates pyroptosis in diabetic cardiomyopathy. Cellular Physiology and Biochemistry 50, 1230–1244. [DOI] [PubMed] [Google Scholar]
- 93.Yin M et al. (2015) Selective killing of lung cancer cells by miRNA-506 molecule through inhibiting NF-kappaB p65 to evoke reactive oxygen species generation and p53 activation. Oncogene 34, 691–703. [DOI] [PubMed] [Google Scholar]
- 94.Zhu B et al. (2020) Silencing of KCNQ1OT1 decreases oxidative stress and pyroptosis of renal tubular epithelial cells. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy 13, 365–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Yoshimoto R et al. (2016) MALAT1 long non-coding RNA in cancer. Biochimica et Biophysica Acta 1859, 192–199. [DOI] [PubMed] [Google Scholar]
- 96.Li X et al. (2017) Long noncoding RNA MALAT1 regulates renal tubular epithelial pyroptosis by modulated miR-23c targeting of ELAVL1 in diabetic nephropathy. Experimental Cell Research 350, 327–335. [DOI] [PubMed] [Google Scholar]
- 97.Napier BA et al. (2016) Complement pathway amplifies caspase-11-dependent cell death and endotoxin-induced sepsis severity. Journal of Experimental Medicine 213, 2365–2382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wang Y et al. (2019) TLR4/NF-kappaB signaling induces GSDMD-related pyroptosis in tubular cells in diabetic kidney disease. Frontiers in Endocrinology (Lausanne) 10, 603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Pang Y et al. (2020) Andrade-Oliveira salvianolic acid B modulates caspase-1-mediated pyroptosis in renal ischemia-reperfusion injury via Nrf2 pathway. Frontiers in Pharmacology 11, 541426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Chen Q et al. (2018) Astragalosides IV protected the renal tubular epithelial cells from free fatty acids-induced injury by reducing oxidative stress and apoptosis. Biomedicine & Pharmacotherapy 108, 679–686. [DOI] [PubMed] [Google Scholar]
- 101.Su S et al. (2018) Hordenine protects against hyperglycemia-associated renal complications in streptozotocin-induced diabetic mice. Biomedicine & Pharmacotherapy 104, 315–324. [DOI] [PubMed] [Google Scholar]
- 102.Yang WJ et al. (2018) Protective effect of the ethanol extract from Ligusticum chuanxiong rhizome against streptozotocin-induced diabetic nephropathy in mice. Journal of Ethnopharmacology 227, 166–175. [DOI] [PubMed] [Google Scholar]
- 103.Tong Y et al. (2019) Ethyl vanillin protects against kidney injury in diabetic nephropathy by inhibiting oxidative stress and apoptosis. Oxidative Medicine and Cellular Longevity 2019, 2129350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hou Y et al. (2016) Mitochondria-targeted peptide SS-31 attenuates renal injury via an antioxidant effect in diabetic nephropathy. American Journal of Physiology. Renal Physiology 310, F547–F559. [DOI] [PubMed] [Google Scholar]
- 105.Shah A et al. (2015) Thioredoxin-interacting protein deficiency protects against diabetic nephropathy. Journal of the American Society of Nephrology 26, 2963–2977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Du C et al. (2016) Thioredoxin-interacting protein regulates lipid metabolism via Akt/mTOR pathway in diabetic kidney disease. International Journal of Biochemistry & Cell Biology 79, 1–13. [DOI] [PubMed] [Google Scholar]
- 107.Ji L et al. (2019) FOXO1 overexpression attenuates tubulointerstitial fibrosis and apoptosis in diabetic kidneys by ameliorating oxidative injury via TXNIP-TRX. Oxidative Medicine and Cellular Longevity 2019, 3286928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ke R et al. (2020) Endoplasmic reticulum stress related factor IRE1alpha regulates TXNIP/NLRP3-mediated pyroptosis in diabetic nephropathy. Experimental Cell Research 396, 112293. [DOI] [PubMed] [Google Scholar]
- 109.Song CL et al. (2017) Effect of circular ANRIL on the inflammatory response of vascular endothelial cells in a Rat model of coronary atherosclerosis. Cellular Physiology and Biochemistry 42, 1202–1212. [DOI] [PubMed] [Google Scholar]
- 110.Wang J and Zhao SM (2021) LncRNA-antisense non-coding RNA in the INK4 locus promotes pyroptosis via miR-497/thioredoxin-interacting protein axis in diabetic nephropathy. Life Sciences 264, 118728. [DOI] [PubMed] [Google Scholar]
- 111.Nagata M (2016) Podocyte injury and its consequences. Kidney International 89, 1221–1230. [DOI] [PubMed] [Google Scholar]
- 112.Cheng Q et al. (2020) Caspase-11/4 and gasdermin D-mediated pyroptosis contributes to podocyte injury in mouse diabetic nephropathy. Acta Pharmacologica Sinica 42, 954–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Yoon MS (2017) The role of mammalian target of rapamycin (mTOR) in insulin signaling. Nutrients 9, 1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Cosin-Roger J et al. (2017) Hypoxia ameliorates intestinal inflammation through NLRP3/mTOR downregulation and autophagy activation. Nature Communications 8, 98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Jia X et al. (2018) Delayed oseltamivir plus sirolimus treatment attenuates H1N1 virus-induced severe lung injury correlated with repressed NLRP3 inflammasome activation and inflammatory cell infiltration. PLoS Pathogens 14, e1007428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sahan-Firat S et al. (2018) Protection by mTOR inhibition on zymosan-induced systemic inflammatory response and oxidative/nitrosative stress: contribution of mTOR/MEK1/ERK1/2/IKKbeta/IkappaB-alpha/NF-kappaB signalling pathway. Inflammation 41, 276–298. [DOI] [PubMed] [Google Scholar]
- 117.Wang X et al. (2018) Astragaloside IV represses high glucose-induced mesangial cells activation by enhancing autophagy via SIRT1 deacetylation of NF-kappaB p65 subunit. Drug Design, Development and Therapy 12, 2971–2980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wang T et al. (2020) Ginsenoside Rg1 alleviates podocyte injury induced by hyperlipidemia via targeting the mTOR/NF-kappaB/NLRP3 axis. Evidence-Based Complementary and Alternative Medicine: ECAM 2020, 2735714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Gurung P, Lukens JR and Kanneganti TD (2015) Mitochondria: diversity in the regulation of the NLRP3 inflammasome. Trends in Molecular Medicine 21, 193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Traba J et al. (2015) Fasting and refeeding differentially regulate NLRP3 inflammasome activation in human subjects. Journal of Clinical Investigation 125, 4592–4600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Chan SH et al. (2018) Exercise intervention attenuates hyperhomocysteinemia-induced aortic endothelial oxidative injury by regulating SIRT1 through mitigating NADPH oxidase/LOX-1 signaling. Redox Biology 14, 116–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Thornton CC et al. (2016) Methotrexate-mediated activation of an AMPK-CREB-dependent pathway: a novel mechanism for vascular protection in chronic systemic inflammation. Annals of the Rheumatic Diseases 75, 439–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Yang M et al. (2020) Colchicine alleviates cholesterol crystal-induced endothelial cell pyroptosis through activating AMPK/SIRT1 pathway. Oxidative Medicine and Cellular Longevity 2020, 9173530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chen B, Li J and Zhu H (2016) AMP-activated protein kinase attenuates oxLDL uptake in macrophages through PP2A/NF-kappaB/LOX-1 pathway. Vascular Pharmacology 85, 1–10. [DOI] [PubMed] [Google Scholar]
- 125.Li F et al. (2020) Geniposide alleviates diabetic nephropathy of mice through AMPK/SIRT1/NF-kappaB pathway. European Journal of Pharmacology 886, 173449. [DOI] [PubMed] [Google Scholar]
- 126.Chen J et al. (2020) Study on the inhibitive effect of Catalpol on diabetic nephropathy. Life Sciences 257, 118120. [DOI] [PubMed] [Google Scholar]
- 127.Rajamaki K et al. (2018) Haploinsufficiency of A20 impairs protein-protein interactome and leads into caspase-8-dependent enhancement of NLRP3 inflammasome activation. RMD Open 4, e000740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Xue Z et al. (2019) miR-21 promotes NLRP3 inflammasome activation to mediate pyroptosis and endotoxic shock. Cell Death & Disease 10, 461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ge X et al. (2016) miR-21-5p alleviates leakage of injured brain microvascular endothelial barrier in vitro through suppressing inflammation and apoptosis. Brain Research 1650, 31–40. [DOI] [PubMed] [Google Scholar]
- 130.Voet S et al. (2018) A20 critically controls microglia activation and inhibits inflammasome-dependent neuroinflammation. Nature Communications 9, 2036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.O'Brien K et al. (2020) RNA delivery by extracellular vesicles in mammalian cells and its applications. Nature Reviews Molecular Cell Biology 21, 585–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kosaka N et al. (2016) Versatile roles of extracellular vesicles in cancer. Journal of Clinical Investigation 126, 1163–1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Ding X et al. (2020) MiR-21-5p in macrophage-derived extracellular vesicles affects podocyte pyroptosis in diabetic nephropathy by regulating A20. Journal of Endocrinological Investigation 44, 1175–1184. [DOI] [PubMed] [Google Scholar]
- 134.Huang S et al. (2019) Long noncoding RNA NEAT1 accelerates the proliferation and fibrosis in diabetic nephropathy through activating Akt/mTOR signaling pathway. Journal of Cellular Physiology 234, 11200–11207. [DOI] [PubMed] [Google Scholar]
- 135.Wang X et al. (2019) LncRNA NEAT1 promotes extracellular matrix accumulation and epithelial-to-mesenchymal transition by targeting miR-27b-3p and ZEB1 in diabetic nephropathy. Journal of Cellular Physiology 234, 12926–12933. [DOI] [PubMed] [Google Scholar]
- 136.Gholaminejad A, Abdul Tehrani H and Gholami Fesharaki M (2018) Identification of candidate microRNA biomarkers in diabetic nephropathy: a meta-analysis of profiling studies. Journal of Nephrology 31, 813–831. [DOI] [PubMed] [Google Scholar]
- 137.Liu XD et al. (2015) Overexpression of miR-34c inhibits high glucose-induced apoptosis in podocytes by targeting Notch signaling pathways. International Journal of Clinical and Experimental Pathology 8, 4525–4534. [PMC free article] [PubMed] [Google Scholar]
- 138.Zhan JF et al. (2020) Long non-coding RNA NEAT1 regulates pyroptosis in diabetic nephropathy via mediating the miR-34c/NLRP3 axis. Kidney & Blood Pressure Research 45, 589–602. [DOI] [PubMed] [Google Scholar]
- 139.Zuo Y et al. (2021) Atorvastatin regulates MALAT1/miR-200c/NRF2 activity to protect against podocyte pyroptosis induced by high glucose. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy 14, 1631–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Birnbaum Y et al. (2018) Combined SGLT2 and DPP4 inhibition reduces the activation of the Nlrp3/ASC inflammasome and attenuates the development of diabetic nephropathy in mice with type 2 diabetes. Cardiovascular Drugs and Therapy 32, 135–145. [DOI] [PubMed] [Google Scholar]
- 141.Birnbaum Y et al. (2016) Dipeptidyl peptidase-4 inhibition by saxagliptin prevents inflammation and renal injury by targeting the Nlrp3/ASC inflammasome. BMJ Open Diabetes Research & Care 4, e000227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Liu J et al. (2019) Downregulation of LncRNA-XIST inhibited development of non-small cell lung cancer by activating miR-335/SOD2/ROS signal pathway mediated pyroptotic cell death. Aging (Albany NY) 11, 7830–7846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Ren N et al. (2020) LncRNA ADAMTS9-AS2 inhibits gastric cancer (GC) development and sensitizes chemoresistant GC cells to cisplatin by regulating miR-223-3p/NLRP3 axis. Aging (Albany NY) 12, 11025–11041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Li Y et al. (2019) Diazepam inhibited lipopolysaccharide (LPS)-induced pyroptotic cell death and alleviated pulmonary fibrosis in mice by specifically activating GABAA receptor alpha4-subunit. Biomedicine & Pharmacotherapy 118, 109239. [DOI] [PubMed] [Google Scholar]
- 145.Wang X et al. (2020) Upregulation of miR-223 abrogates NLRP3 inflammasome-mediated pyroptosis to attenuate oxidized low-density lipoprotein (ox-LDL)-induced cell death in human vascular endothelial cells (ECs). In Vitro Cellular & Developmental Biology Animal 56, 670–679. [DOI] [PubMed] [Google Scholar]