Abstract
Objectives:
Determine the relationship of patellofemoral osteoarthritis (OA) to changes in performance-based function over 7 years.
Methods:
2666 participants (62.2±8.0 years, BMI 30.6±5.9kg/m2; 60% female) from the Multicenter Osteoarthritis Study with knee radiographs at baseline and who completed repeated chair stands and 20-meter walk test at baseline, 2.5, 5, and 7 years were included. Generalized linear models assessed the relation of radiographic patellofemoral OA and radiographic patellofemoral OA with frequent knee pain to longitudinal changes in performance-based function. Analyses were adjusted for age, sex, BMI, tibiofemoral OA, and injury/surgery.
Results:
Linear models demonstrated a significant group by time interaction for the repeated chair stands (p=0.04) and the 20-meter walk test (p<0.0001). Those with radiographic patellofemoral OA took 1.01seconds longer on the repeated chair stands (p=0.02) and 1.69seconds longer on the 20-meter walk test (p<0.0001) at 7 years compared with baseline. When examining the relation of radiographic patellofemoral OA with frequent knee pain to performance-based function there was a significant group by time interaction for repeated chair stands (p=0.05) and the 20-meter walk test (p<0.0001). Those with radiographic patellofemoral OA with frequent knee pain increased their time on the repeated chair stands by 1.12seconds (p=0.04) and 1.91seconds (p<0.0001) on the 20-meter walk test over 7 years.
Conclusion:
Individuals with radiographic patellofemoral OA and those with radiographic patellofemoral OA with frequent knee pain have worsening of performance-based function over time. This knowledge may present opportunities to plan for early treatment strategies for patellofemoral OA to limit functional decline over time.
KEY INDEXING TERMS: Osteoarthritis, Function, Rehabilitation, Patellofemoral
INTRODUCTION
Pain and functional limitations (e.g., difficulty with walking and rising from a chair) associated with knee osteoarthritis (OA)[1] are important barriers to physical activity in individuals with knee OA[2]. This reduced mobility may contribute to development of comorbidities such as cardiovascular disease associated with physical inactivity[3]. Thus, it is important to understand and address functional limitations associated with knee OA.
Knee OA can occur either in the tibiofemoral joint, patellofemoral joint, or both. Tibiofemoral OA is associated with poorer performance during walking and sit-to-stand activities relative to those without OA[4]. It is also associated with a decline in self-reported and performance-based function over time[5, 6]. The patellofemoral joint is frequently affected in knee OA[7]. Patellofemoral OA is more prevalent than previously thought—half of individuals with knee pain or radiographic knee OA have patellofemoral involvement[8]. It is associated with substantial knee pain[7, 9] and reduced quality of life[10].
Patellofemoral OA is associated with poor self-reported functional ability [7, 11] and performance-based function (assessed by Timed Up and Go, timed stairs, and one-leg rise tasks)[12, 13], however, the extent of longitudinal changes in performance-based function in those with patellofemoral OA is unknown. Considering the progressive nature of patellofemoral OA[14, 15], the knowledge about the course of decline in functional ability associated with patellofemoral OA is of clinical importance. In addition, symptomatic knee OA (defined as radiographic OA with knee pain) has been associated with lower self-reported function than radiographic knee OA without pain[16]. Therefore, it is important to investigate the association of radiographic and symptomatic patellofemoral OA with performance-based function over-time. Treatment strategies targeting functional limitations associated with patellofemoral OA early in the disease process may improve outcomes. Therefore, we aimed to determine the relationship of radiographic patellofemoral OA and radiographic patellofemoral OA with frequent knee pain to changes in performance-based function (assessed using repeated chair test and 20-meter walk test) over 7 years. We hypothesized that individuals with patellofemoral OA will have greater decrease in performance-based function over 7 years than those without patellofemoral OA.
METHODS
Study population
The Multicenter Osteoarthritis (MOST) Study is an NIH-funded prospective cohort study of 3,026 older adults, who were aged 50 to 79 years and had knee OA or were at risk of knee OA at the time of recruitment. Participants were recruited from two communities in the US: Birmingham, Alabama, and Iowa City, Iowa. Ethical approval was obtained from the institutional review boards of the University of Iowa (#201511711), University of Alabama at Birmingham (#000329007), University of California San Francisco (#10–00500), and Boston University Medical Center (#H-32956). Participants enrolled in the MOST Study provided written informed consent. Details of the study population have been previously published[17]. Participants who had knee radiographs assessed at baseline and who completed the repeated chair stand test and the 20-meter walk test at baseline, 2.5-, 5- and 7-year study visits were included in the present study. Participants who had a total knee/hip replacement baseline were excluded from the analyses (n=71), as function after these surgeries is highly variable and unlikely due to baseline OA status. Participants who had total knee or hip knee replacement at 2.5, 5- or 7- years study visits, their performance-based function data were included in the analyses from study visits before their surgery.
Radiographic knee OA
Participants were classified by the presence of OA at baseline. We considered two definitions of patellofemoral OA: radiographic OA defined by the presence of radiographic features; and symptomatic OA, which was defined by both radiographic features and the presence of knee pain. Bilateral knee radiographs were obtained at baseline. Radiographs included standing fixed-flexed posterior-anterior view as well as weight-bearing lateral view. The posterior-anterior views were scored on a scale 0–3 based on the atlas of the Osteoarthritis Research Society International[18], and the lateral views were scored on a scale 0–3 based on the atlas of the Framingham Osteoarthritis Study[19]. Radiographic tibiofemoral OA was defined as a Kellgren and Lawrence grade ≥2 on posterior-anterior radiographs[20, 21]. Radiographic patellofemoral OA was defined as grade ≥2 osteophytes or grade ≥2 joint space narrowing plus grade ≥1 osteophytes, sclerosis, or cyst on lateral views[18, 21]. Two raters independently scored all knee radiographs, and discrepancies were resolved by a panel of three adjudicators[22].
Knee pain
At baseline, frequent knee pain was assessed in each knee by asking participants, “Do you have knee pain, aching, or stiffness on most days of the month?”.
Performance-based function
The repeated chair stand test[23] and the 20-meter walk test[24] were used to assess performance-based function. For the repeated chair stand participants were asked to stand up from a sitting position and sit down, with both arms crossed against the chest, five times as quickly as possible. The time required to complete five repetitions was recorded in seconds. The repeated chair stand test is a measure of functional performance related to thigh strength[25]. For the 20-meter walk test, participants were asked to walk 20 meters in an unobstructed hallway at their usual walking pace and the time needed to perform the test was recorded in seconds. The 20-meter walk test is a commonly used performance measure to assess the walking speed and monitor physical functioning over time. As the repeated chair stand and 20-meter walk test provide different information, these performance-based functional tests were studied independently. Those who were not able to perform the repeated chair stands and/or 20-meter walk were not excluded from the analysis.
Statistical analyses
Since our two measures of performance-based function were person specific (not knee specific) measures, a person was considered to have patellofemoral OA if either knee had patellofemoral OA at baseline. We used generalized estimating equations (GEE) linear regression models to assess the effects of patellofemoral OA on changes in performance-based function over 7 years. Tukey-Kramer adjustments were used for multiple comparisons. Group (radiographic patellofemoral OA vs no radiographic patellofemoral OA) was included along with assessment visit (4-level categorical variable representing each clinic visit) and their interaction as the main predictors of performance-based function at each time point. We performed additional analyses to determine the relation of radiographic patellofemoral OA plus presence of frequent knee pain to changes in performance-based function. Analyses were adjusted for age, sex, BMI, history of injury/surgery, and baseline radiographic tibiofemoral OA. Analyses were conducted using SAS 9.4 (Cary, NC).
RESULTS
Participant characteristics
Of the 2,737 participants who had radiographs assessed at baseline, 71 participants had a total hip or knee replacement in either knee at baseline, leaving 2,666 participants eligible for the current study (Table 1). In total, 2,623 and 2,664 participants had at least one visit where the repeated chair stands and 20-meter walk were assessed, respectively. For repeated chair stands, 1697 (64.7%) participants had data for all study visits and 446 (17.0%), 402 (15.3%), and 86 (3.3%) had data for three, two, and one study visit. For 20-meter walk, 1531 (57.5%) participants had data for all study visits and 428 (16.0%), 545 (20.5%), and 160 (6.0%) had data for three, two, and one study visit (Figure 1).
Table 1.
Baseline characteristics
| Overall (n=2666) | Radiographic patellofemoral OA (n=607) | No radiographic patellofemoral OA (n=2059) | Radiographic patellofemoral OA with frequent knee pain (n=533) | No radiographic patellofemoral OA and frequent knee pain (n=2131) | |
|---|---|---|---|---|---|
| Age, years | 62.2±8.0 | 63.6±8.0 | 61.8±8.0 | 63.6±8.0 | 61.8±7.9 |
| Body mass index, kg/m2 | 30.6±5.9 | 32.8±6.7 | 29.9±5.4 | 33.2±6.9 | 29.9±5.4 |
| Sex,Female, % | 60 | 65 | 42 | 68 | 58 |
| Radiographic tibiofemoral OA, % | 51 | 85 | 41 | 87 | 42 |
| History of injury/surgery, % | 31 | 37 | 29 | 37 | 29 |
Note. Data are presented as mean±standard deviation, unless otherwise stated. Abbreviations as follows: OA, osteoarthritis
Figure 1.
Flowchart of participants selection
Relation of radiographic patellofemoral OA to changes in performance-based function
When comparing individuals with and without radiographic patellofemoral OA, there were no significant differences in the time to complete the repeated chair stands test (mean difference [95% confidence interval]: 0.09 seconds [−0.28 to 0.47]; p=0.99) and the 20-meter walk test (0.25 seconds [−0.14 to 0.64]; p=0.91) at baseline. There were also no significant differences at 2.5 years between individuals with and without radiographic patellofemoral OA (repeated chair stands: 0.56 seconds [0.06 to 1.06]; p=0.36; 20-meter walk: 0.56 seconds [0.16 to 0.96]; p=0.11). There were no significant differences in time to complete the repeated chair stands test at 5 years (0.54 seconds [0.04 to 1.03]; p=0.41) and 7 years (0.90 seconds [0.26 to 1.54]; p=0.10) between those with and without radiographic patellofemoral OA; however, those with radiographic patellofemoral OA took significantly longer to complete the 20-meter walk test at 5 years (1.08 seconds [0.60 to 1.55]; p=0.0002) and 7 years (1.57 seconds [1.00 to 2.13]; p<0.0001).
Individuals with radiographic patellofemoral OA had worsening performance over time on the repeated chair stands (Figure 2A) and 20-meter walk (Figure 2B). There was a significant group by time interaction for the repeated chair stands (p=0.04) and the 20-meter walk test (p<0.0001). From baseline to 7 years, those with radiographic patellofemoral OA took 1.01 seconds (95% CI: 0.42 to 1.60; p=0.02) longer on the repeated chair stands and 1.69 seconds (95% CI: 1.18 to 2.20; p<0.0001) on the 20-meter walk test. While individuals without radiographic patellofemoral OA took 0.21 seconds (95% CI: 0.01 to 0.40; p=0.43) longer on the repeated chair stands and 0.37 seconds (95% CI: 0.23 to 0.52; p<0.0001) longer on the 20-meter walk test from baseline to 7 years.
Figure 2.
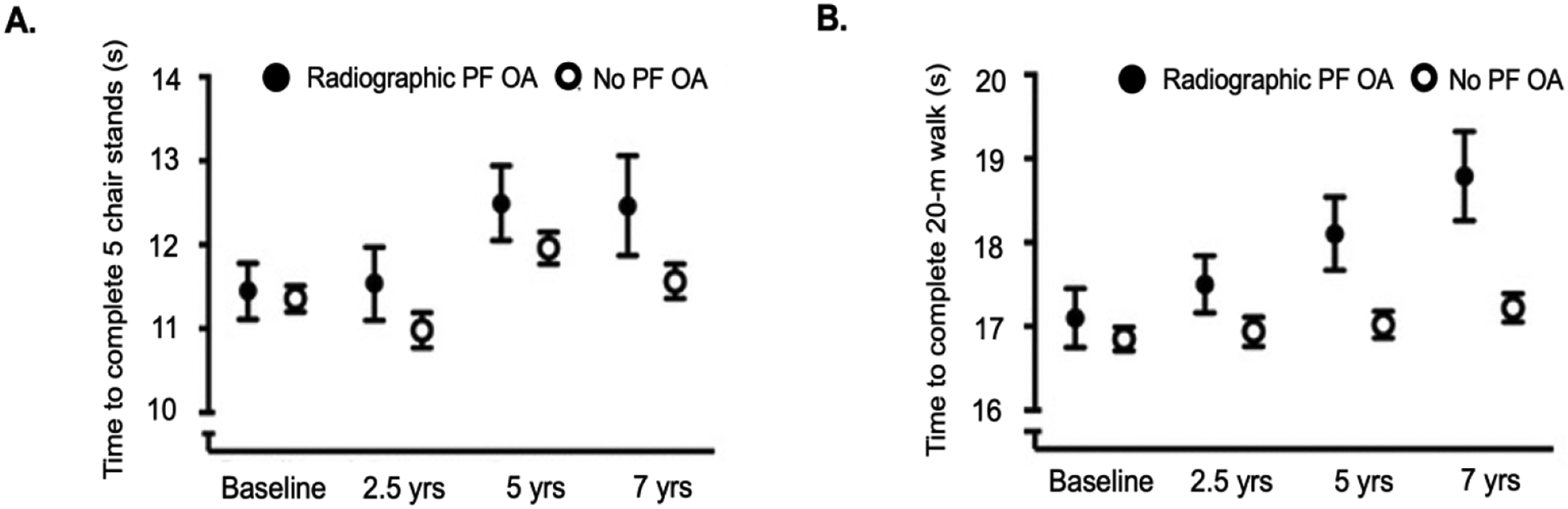
Mean time (seconds) to complete five chair stands (panel A.) and time to complete 20 meters walk (panel B.) in those with and without radiographic PF OA from baseline to 7 years
Relation of radiographic patellofemoral OA with frequent knee pain to changes in performance-based function
Between individuals with and without radiographic patellofemoral OA with frequent knee pain, there were no significant differences in the time to complete the repeated chair stands (0.43 seconds [0.03 to 0.84]; p=0.42) or the 20-meter walk test (0.42 seconds [−0.001 to 0.84]; p=0.51) at baseline. At 2.5 years, those with radiographic patellofemoral OA with frequent knee pain took significantly longer to complete the repeated chair stands (0.93 seconds [0.39 to 1.48]; p=0.02) and the 20-meter walk test (0.89 seconds, [0.46 to 1.32]; p=0.001) when compared with those without radiographic patellofemoral OA or knee pain. Individuals with radiographic patellofemoral OA with frequent knee pain also took significantly longer to complete the performance-based function tests at 5 years (repeated chair stands: 0.87 seconds [0.32 to 1.43]; p=0.04; 20-meter walk test: 1.39 seconds [0.86 to 1.93]; p<0.0001) and 7 years (repeated chair stands: 1.33 seconds [0.59 to 2.08]; p=0.009; 20-meter walk test: 1.96 seconds [1.31 to 2.60]; p<0.0001) when compared with those without radiographic patellofemoral OA or knee pain.
When examining the relation of radiographic patellofemoral OA with frequent knee pain to performance-based function there was a significant group by time interaction for the repeated chair stands (p=0.05) (Figure 3A) and the 20-meter walk test (p<0.0001) (Figure 3B). From baseline to 7 years, individuals with radiographic patellofemoral OA with frequent knee pain increased their time on the repeated chair stands and 20-meter walk test by 1.12 seconds (95% CI: 0.42 to 1.82, p=0.04) and 1.91 seconds (95% CI: 1.31 to 2.52; p<0.0001), respectively. In those without radiographic patellofemoral OA with frequent knee pain, the time to complete the repeated chair stands (0.23 seconds [0.04 to 0.42]; p=0.28) did not significantly increase from baseline to 7 years, but the time to complete the 20-meter walk test increased (0.38 seconds [0.23 to 0.52]; p<0.0001) from baseline to 7 years.
Figure 3.
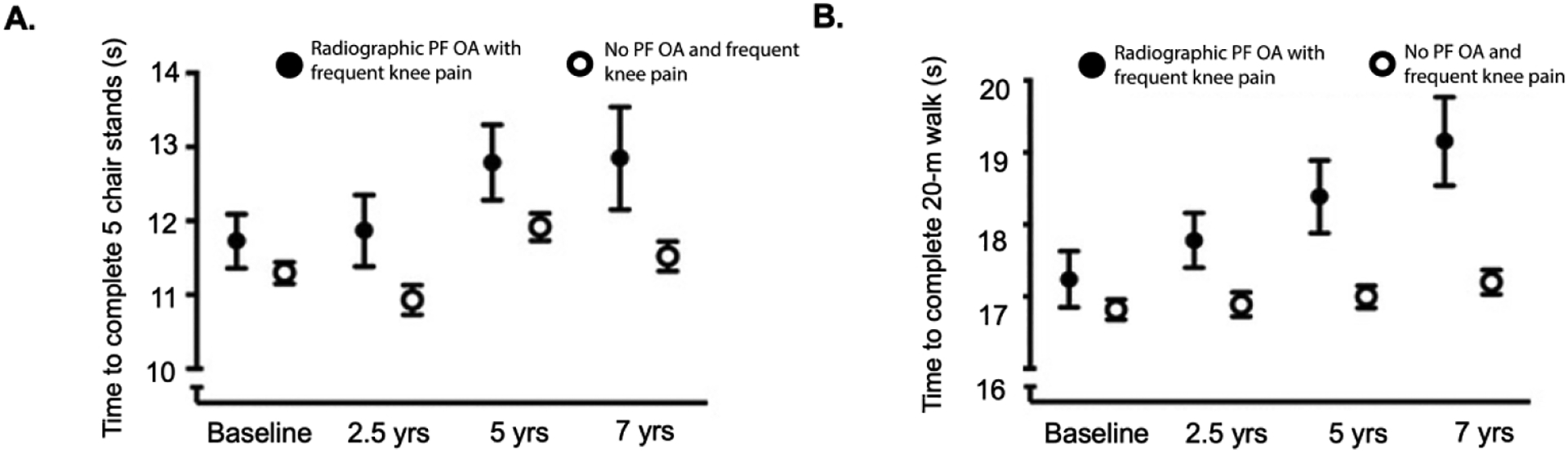
Mean time (seconds) to complete five chair stands (panel A.) and time to complete 20 meters walk (panel B.) in those with and without symptomatic PF OA from baseline to 7 years
DISCUSSION
Our study revealed that participants with radiographic patellofemoral OA and those with radiographic patellofemoral OA with frequent knee pain had worsening of performance-based function over-time. It has been reported that taking longer than 12 seconds to complete the repeated chair stand test and walking slower than 1.22m/s to complete 20-meter walk test may indicate inadequate physical ability to walk at least 6000 steps per day[26]—daily step count threshold associated with risk of incident functional limitation in individuals with knee OA[27]. Our results showed that individuals with patellofemoral OA (radiographic with or without frequent knee pain) took on average longer than 12 seconds to complete the repeated chair stands at 5 and 7 years. Those with patellofemoral OA on average walked with a gait speed of less than 1.22m/s at baseline and each study follow-up.
Patellofemoral OA is associated with poor self-reported function[7, 11] and performance-based function[12]. In the present study, individuals with patellofemoral OA at the study baseline took longer to complete the repeated chair stands and walked more slowly during the 20-meter walk test during follow-up than those without patellofemoral OA at 7 years. The differences between individuals with and without radiographic patellofemoral OA with frequent knee pain were evident at 2.5 year follow-up for the repeated chair stand test and the 20-meter walk test. The repeated chair stand test is a measure of functional performance related to thigh strength[25] and previous research has reported that individuals with patellofemoral OA have reduced quadriceps volume and strength[28]. Further, activities that load the patellofemoral joint during weight bearing on a flexed knee can be more demanding for individuals with patellofemoral OA than level walking. Interestingly, the decline in performance appeared to more prominent on the 20-meter walk test than the repeated chair stands between those with and without radiographic patellofemoral OA with frequent knee pain at 5 and 7 year follow-up. These findings highlight the importance of using a variety of performance-based functional tasks as different tests measure different aspects of physical health.
Walking speed has been identified as a functional sixth ‘vital sign’ and it is an indicator of future health status and quality of life[29]. For example, slower walking speed has been associated with incident radiographic and symptomatic knee OA[30]. A change in 20-meter walk test time between −1.59 seconds (walking slower) and 0.15 seconds (walking faster) among individuals with knee OA is considered within the range of normal variability[24]. Individuals with radiographic patellofemoral OA increased the time to complete the 20-meter walk test by 1.69 seconds from baseline to 7-year follow-up, and individuals with symptomatic patellofemoral OA increased the time to complete the 20-meter walk test by 1.91 seconds, which is outside the normal variability for the 20-meter test. This is of importance, as walking 0.2m/s slower over-time during 20-meter walk test has been associated with increased mortality in individuals with knee OA[31]. Individuals without patellofemoral OA also took 0.38 seconds longer to complete the 20-meter walk test at 7 years than at baseline; however, this is within the normal variability for the test. We are unaware of validated minimal clinically important difference for the increases in repeated chair stand test in individuals with knee OA. The minimal detectable change for the repeated chair stands is 4.52 seconds based on community-dwelling adults aged ≥50 years (median age 66 years, range 51–89 years)[32]. At all-time points, except one, we observed significant differences in individuals with radiographic patellofemoral OA (with or without frequent pain) and those without patellofemoral OA. These differences, however, were within the minimal detectable change for the repeated chair stands. In individuals without patellofemoral OA, there were significant fluctuations in time to complete the repeated chair stands over the 7 years, however, these were within the minimal detectable change value. When compared to baseline, there were no significant differences in time to complete the repeated chair stands at 7 years in individuals without patellofemoral OA.
Individuals with patellofemoral OA have a decline in performance-based function over time. Thus, clinicians should monitor function in individuals with patellofemoral OA and target modifiable risk factors of physical function (such as quadriceps strength) to aid in reducing functional decline over time[33]. Further to this, researchers and clinicians should consider using a battery of functional tests. Different performance-based functional tests assess discrete and specific components of the performance on specific tasks, and thus functional limitations may be more evident or evident earlier on some performance-based functional tasks than others. The Osteoarthritis Research Society International recommended set of performance-based tests of physical function for individuals with knee OA include the minimum core set (i.e., 30 seconds Chair Stand test, 40-meter Fast-paced Walk test, Stair Climb test) and the recommended set (minimum core set, timed up & Go test and 6 Minute Walk test)[34]. The Multicenter Osteoarthritis Study was established prior to the Osteoarthritis Research Society International recommendations regarding performance-based tests, and it does not include the entire minimum core set. Although, we were unable gain insights into stair climbing function over time, we were able to determine how performance-based function over time based on a walking task (20-meter walk test) and a chair task (five-repeated chair stand).
Our study has several strengths and clinical implications. We used data from a large cohort of individuals with or at risk of knee OA to investigate longitudinal changes in performance-based function. Individuals with patellofemoral OA have self-reported functional limitations; however, this is the first study to describe that individuals with patellofemoral OA are more likely to experience decline in performance-based function decline over time. The MOST study included individuals who were aged 50–79 years with or at risk of knee OA. Patellofemoral OA is common in young and middle-aged adults[35, 36], who have higher physical demands due to work and child-care related activities; any decline in function may adversely impact work participation and quality of life. Thus, it is important to investigate performance-based function over-time in a younger cohort of individuals with patellofemoral OA. This could have important implications, as early rehabilitative treatments focusing on improving pain and functional limitations in younger and middle-aged individuals with patellofemoral OA may mitigate worsening over time. There are several other limitations that we encourage the readers to consider when interpreting the results. We focused on the presence of patellofemoral OA at baseline and its association with performance-based function. However, radiographic patellofemoral OA disease severity may influence patterns of performance-based function. Unfortunately, there were not enough numbers to analyze mild, moderate, and severe OA separately. We defined patellofemoral OA using only the lateral radiographs, which likely lead us to miss cases of patellofemoral OA. Repeating our analysis in a cohort that also has a skyline view may lead to different results. We relied on the baseline assessment of OA in this study, although some participants without OA at baseline could develop OA during the follow-up period, which may have reduced the observed group differences at later exams. Further to this, we accounted for age, sex, body mass index, history of injury/surgery and radiographic tibiofemoral OA in the models, However, there are several other factors such as comorbidities, depression and physical activity that may contribute performance-based function over time. Lastly, 35% and 43% of participants did not have complete data for all study visits for the repeated chair stands and 20-meter walk tests, respectively. This may have influenced the results of our study, especially the precision of the estimates. However, the repeated measures linear regression analyses are valid under the same ‘missing at random’ assumption that other approaches such as multiple imputation would require. The GEE analyses of longitudinal data allow inclusion of participants with some missing outcome values due to dropout from the study. If the dropout from the study is completely at random then the estimates will be unbiased. If the dropout rate is low and variables predictive of dropout included as independent variables, then any bias should be minimal. In addition, we found no differences in baseline participants characteristics with individuals with complete data and those with missing data.
CONCLUSION
Individuals with patellofemoral OA demonstrated worsening of performance-based function over 7 years. This information may present opportunities to plan for early treatment strategies for patellofemoral OA to limit functional decline over time.
SOURCE OF SUPPORT:
Funding:
The Multicenter Osteoarthritis Study was funded by the NIH/NIA UO1 AG18820, UO1 AG18832, UO1 AG18947, and UO1 AG19069. Dr. Hart is funded by a Canadian Institutes of Health Research Fellowship. Dr. Stefanik is supported by NIH/NIAMS K23 AR070913. Dr. Neogi was supported by NIH/NIAMS K24AR070892. This work was also supported by NIH/NIAMS P30AR072571. Funding sources had no role in the study design, collection, analysis, and interpretation of the data or the decision to submit the manuscript for publication.
Footnotes
CONFLICT OF INTEREST: The authors have declared no conflicts of interest.
REFERENCES
- 1.Guccione AA, Felson DT, Anderson JJ, Anthony JM, Zhang Y, Wilson PW, Kelly-Hayes M, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health 1994; 84:351–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kanavaki AM, Rushton A, Efstathiou N, Alrushud A, Klocke R, Abhishek A, Duda JL. Barriers and facilitators of physical activity in knee and hip osteoarthritis: a systematic review of qualitative evidence. BMJ Open 2017; 7:e017042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van Dijk GM, Veenhof C, Schellevis F, Hulsmans H, Bakker JP, Arwert H, et al. Comorbidity, limitations in activities and pain in patients with osteoarthritis of the hip or knee. BMC Musculoskelet Disord 2008; 9:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim I, Kim HA, Seo YI, Song YW, Hunter DJ, Jeong JY, Kim DH. Tibiofemoral osteoarthritis affects quality of life and function in elderly Koreans, with women more adversely affected than men. BMC Musculoskelet Disord 2010; 11:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miller ME, Rejeski WJ, Messier SP, Loeser RF. Modifiers of change in physical functioning in older adults with knee pain: the Observational Arthritis Study in Seniors (OASIS). Arthritis Rheum 2001; 45:331–339. [DOI] [PubMed] [Google Scholar]
- 6.White DK, Neogi T, Nguyen U-SDT, Niu J, Zhang Y. Trajectories of functional decline in knee osteoarthritis: the Osteoarthritis Initiative. Rheumatology (Oxford, England) 2016; 55:801–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duncan R, Peat G, Thomas E, Wood L, Hay E, Croft P. How do pain and function vary with compartmental distribution and severity of radiographic knee osteoarthritis? Rheumatology (Oxford) 2008; 47:1704–1707. [DOI] [PubMed] [Google Scholar]
- 8.Hart HF, Stefanik JJ, Wyndow N, Machotka Z, Crossley KM. The prevalence of radiographic and MRI-defined patellofemoral osteoarthritis and structural pathology: a systematic review and meta-analysis. Brit J Sports Med 2017; 51:1195–1208. [DOI] [PubMed] [Google Scholar]
- 9.Hart HF, Crossley KM, Hunt MA. Gait patterns, symptoms, and function in patients with isolated tibiofemoral osteoarthritis and combined tibiofemoral and patellofemoral osteoarthritis. J Orthop Res 2018; 36:1666–72. [DOI] [PubMed] [Google Scholar]
- 10.Hart HF, Filbay SR, Coburn S, Charlton JM, Sritharan P, Crossley KM. Is quality of life reduced in people with patellofemoral osteoarthritis and does it improve with treatment? A systematic review, meta-analysis and regression. Disabil Rehab 2019; 41:2979–93. [DOI] [PubMed] [Google Scholar]
- 11.Stefanik JJ, Guermazi A, Roemer FW, Peat G, Niu J, Segal NA, et al. Changes in patellofemoral and tibiofemoral joint cartilage damage and bone marrow lesions over 7 years: the Multicenter Osteoarthritis Study. Osteoarthritis Cartilage 2016; 24:1160–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lankhorst NE, Damen J, Oei EH, Verhaar JAN, Kloppenburg M, Bierma-Zeinstra SMA, van Middelkoop M. Incidence, prevalence, natural course and prognosis of patellofemoral osteoarthritis: the Cohort Hip and Cohort Knee study. Osteoarthritis Cartilage 2017; 25:647–53. [DOI] [PubMed] [Google Scholar]
- 13.Duncan R, Peat G, Thomas E, Wood L, Hay E, Croft P. Does isolated patellofemoral osteoarthritis matter? Osteoarthritis Cartilage 2009; 17:1151–55. [DOI] [PubMed] [Google Scholar]
- 14.Hoglund LT, Lockard MA, Barbe MF, Hillstrom HJ, Song J, Reinus WR, Barr-Gillespie AE. Physical performance measurement in persons with patellofemoral osteoarthritis: A pilot study. J Back Musculoskelet Rehabil 2015; 28:335–42. [DOI] [PubMed] [Google Scholar]
- 15.Macri EM, Crossley KM, Hart HF, d’Entremont AG, Forster BB, Ratzlaff CR, et al. Clinical findings in patellofemoral osteoarthritis compared to individually-matched controls: a pilot study. BMJ Open Sport 2020; 6:e000877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muraki S, Akune T, Oka H, En-yo Y, Yoshida M, Saika A, et al. : Association of radiographic and symptomatic knee osteoarthritis with health-related quality of life in a population-based cohort study in Japan: the ROAD study. Osteoarthritis and Cartilage 2010, 18:1227–34. [DOI] [PubMed] [Google Scholar]
- 17.Segal NA, Nevitt MC, Gross KD, Hietpas J, Glass NA, Lewis CE, Torner JC. The Multicenter Osteoarthritis Study: opportunities for rehabilitation research. PM & R 2013; 5:647–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Felson DT, McAlindon TE, Anderson JJ, Naimark A, Weissman BW, Aliabadi P, et al. Defining radiographic osteoarthritis for the whole knee. Osteoarthritis Cartilage 1997; 5:241–50. [DOI] [PubMed] [Google Scholar]
- 19.Chaisson CE, Gale DR, Gale E, Kazis L, Skinner K, Felson DT. Detecting radiographic knee osteoarthritis: what combination of views is optimal? Rheumatology (Oxford) 2000; 39:1218–21. [DOI] [PubMed] [Google Scholar]
- 20.Kellgren JH, Lawrence JS: Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957; 16:494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Felson DT, Zhang Y, Hannan MT, Naimark A, Weissman B, Aliabadi P, Levy D. Risk factors for incident radiographic knee osteoarthritis in the elderly. The framingham study. Arthritis Rheum 1997; 40:728–33. [DOI] [PubMed] [Google Scholar]
- 22.Roemer FW, Guermazi A, Hunter DJ, Niu J, Zhang Y, Englund M, et al. : The association of meniscal damage with joint effusion in persons without radiographic osteoarthritis: the Framingham and MOST osteoarthritis studies. Osteoarthritis Cartilage 2009; 17:748–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lin YC, Davey RC, Cochrane T. Tests for physical function of the elderly with knee and hip osteoarthritis. Scan J Med Sci Sports 2001; 11:280–86. [DOI] [PubMed] [Google Scholar]
- 24.Motyl JM, Driban JB, McAdams E, Price LL, McAlindon TE:.Test-retest reliability and sensitivity of the 20-meter walk test among patients with knee osteoarthritis. BMC Musculoskelet Disord 2013; 14:166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bohannon RW. Test-retest reliability of the five-repetition sit-to-stand test: a systematic review of the literature involving adults. J Strength Cond Res 2011; 25:3205–07. [DOI] [PubMed] [Google Scholar]
- 26.Master H, Thoma LM, Christiansen MB, Polakowski E, Schmitt LA, White DK. Minimum Performance on clinical tests of physical function to predict walking 6,000 steps/day in knee osteoarthritis: An Observational Study. Arthritis Care Res 2018, 70:1005–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.White DK, Tudor-Locke C, Zhang Y, Fielding R, LaValley M, Felson DT, et al. Daily walking and the risk of incident functional limitation in knee osteoarthritis: an observational study. Arthritis Care Res 2014; 66:1328–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hart HF, Ackland DC, Pandy MG, Crossley KM. Quadriceps volumes are reduced in people with patellofemoral joint osteoarthritis. Osteoarthritis Cartilage 2012, 20:863–68. [DOI] [PubMed] [Google Scholar]
- 29.Fritz S, Lusardi M. White Paper: “Walking Speed: the Sixth Vital Sign”. J Geriatric Phys Ther 2009; 32:2–5. [PubMed] [Google Scholar]
- 30.Purser JL, Golightly YM, Feng Q, Helmick CG, Renner JB, Jordan JM. Association of slower walking speed with incident knee osteoarthritis-related outcomes. Arthritis Care Res 2012, 64:1028–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Master H, Neogi T, Callahan LF, Nelson AE, LaValley M, Cleveland RJ, et al. The association between walking speed from short- and standard-distance tests with the risk of all-cause mortality among adults with radiographic knee osteoarthritis: data from three large United States cohort studies. Osteoarthritis Cartilage 2020, 28:1551–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Donoghue OA, Savva GM, Börsch-Supan A, Kenny RA. Reliability, measurement error and minimum detectable change in mobility measures: a cohort study of community-dwelling adults aged 50 years and over in Ireland. BMJ Open 2019, 9:e030475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Collins NJ, Barton CJ, van Middelkoop M, Callaghan MJ, Rathleff MS, Vicenzino BT, et al. 2018 Consensus statement on exercise therapy and physical interventions (orthoses, taping and manual therapy) to treat patellofemoral pain: recommendations from the 5th International Patellofemoral Pain Research Retreat, Gold Coast, Australia, 2017. Brit J Sport Med 2018, 52:1170–78. [DOI] [PubMed] [Google Scholar]
- 34.Dobson F, Hinman RS, Roos EM, Abbott JH, Stratford P, Davis AM, et al. OARSI recommended performance-based tests to assess physical function in people diagnosed with hip or knee osteoarthritis. Osteoarthritis Cartilage 2013, 21:1042–52. [DOI] [PubMed] [Google Scholar]
- 35.Collins NJ, Oei EHG, de Kanter JL, Vicenzino B, Crossley KM. Prevalence of Radiographic and Magnetic Resonance Imaging Features of Patellofemoral Osteoarthritis in Young and Middle-Aged Adults With Persistent Patellofemoral Pain. Arthritis Care Res 2019, 71:1068–73. [DOI] [PubMed] [Google Scholar]
- 36.Hinman RS, Lentzos J, Vicenzino B, Crossley KM. Is patellofemoral osteoarthritis common in middle-aged people with chronic patellofemoral pain? Arthritis Care Res 2014, 66:1252–57. [DOI] [PubMed] [Google Scholar]


