Abstract
Objective
We hypothesised that videolaryngoscopy modifies practice of tracheal intubation.
Design
Randomised single-blinded study (video and no-video groups).
Setting
Three institutions: one academic, one non-profit and one profit.
Participants
Patients >18 years, requiring orotracheal intubation, without predicted difficult intubation. Non-inclusion criterion was patients requiring a rapid-sequence intubation. 300 patients were included, 271 randomised, 256 analysed: 123 in the no-video and 133 in the video groups.
Intervention
Tracheal intubation using a McGrath Mac videolaryngoscope, the sequence being video recorded.
Primary and secondary outcome measures
The primary outcome was the proportion of intubations where assistance is necessary on request of the operator. Secondary outcomes included intraoperative variables (intubation difficulty scale and its components, percentage of glottic opening score, oesophageal Intubation, duration of intubation, removal of the screen cover in the no-video group, global evaluation of the ease of intubation, bispectral index, heart rate and blood pressure), intraoperative and postoperative complications (hoarseness or sore throat) and cooperation of the anaesthesiology team.
Results
Requirement for assistance was not decreased in the Video group: 36.1% (95% CI 27.9 to 44.9) vs 45.5% (95% CI 36.5 to 54.7) in the no-video group, p=0.74; OR: 0.7 (95% CI 0.4 to 1.1) and absolute risk: 0.10 (95% CI −0.03 to 0.22). Intubation difficulty scale was similar in both groups (p=0.05). Percentage of glottic opening score was better in the Video group (median of 100 (95% CI (100 to 100) and 80 (95%CI (80 to 90) in the no-video group; p<0.001) as Cormack and Lehane grade (p=0001). Ease of intubation was considered better in the video group (p<0.001). Other secondary outcomes were similar between groups. Screen cover was removed in 7.3% (95% CI (2.7 to 11.9)) of the cases in the video group. No serious adverse event occurred. Communication and behaviour within the anaesthesia team were appropriate in all cases.
Conclusion
In patients without predicted difficult intubation, videolaryngoscopy did not decrease the requirement for assistance to perform intubation.
Trial registration number
Keywords: adult anaesthesia, adult intensive & critical care, adult surgery
Strengths and limitations of this study.
This study aimed to assess if the use of a videolaryngoscope modifies the practice of tracheal intubation in real-life conditions.
A major strength of this study performed on patients without a predicted difficult intubation was the choice of the main outcome: the need for help for the anaesthesiologist or the nurse anaesthetist in performing tracheal intubation.
Permanent presence of a two-person team may have induced a bias because it facilitates the practice of an alternative technique.
Another weakness comes from the choice of the McGrath MAC videolaryngoscope and, consequently, results cannot be generalised to other videolaryngoscopes which differ by the shape of the blade, and the existence or not of a channel.
Introduction
Airway management remains a major concern for anaesthesiologists while related morbimortality is determinant for anaesthesia.1–3 Securing the patient’s airway is a critical step in providing general anaesthesia and several recommendations have been published regarding the practice of intubation in anaesthesia.4 5 Direct laryngoscopy using the original Macintosh laryngoscope has been the rule for the past half century; however, a wide range of videolaryngoscopes has been developed in recent years to provide an indirect visualisation of the glottis via a camera. In patients with a suspected difficult airway, there is no doubt that videolaryngoscopy is associated with a significantly better view of the glottis, increases the first-attempt success and reduces mucosal trauma.6
In patients with no predicted difficult airway, no difference in failed intubation has been reported when comparing a videolaryngoscope and Macintosh laryngoscope.7 Nevertheless some authors consider that the use of videolaryngoscopes must be generalised for all patients, even for those in whom preoperative assessment has not found evidence of a particular risk of access to the airways.8–10
In their analysis of the literature, Lewis et al7 emphasise the importance of the choice of the evaluation criteria used to compare the techniques: glottic view, time required for intubation, successful intubation particularly at the first-attempt, risks of complications like hypoxia or other respiratory complications, laryngeal or airway traumas, and sore throat in the postanaesthesia care unit. Another question that needs to be asked when a new technology is proposed is: does this technology change the practice?
This randomised multicentre study done in our real-life conditions, presence of an anaesthesiologist and of a nurse anaesthetist during the induction-intubation period, compared two scenarios, both using the same videolaryngoscope, one using the video function and the other not, for orotracheal intubation of surgical patients without particular risk of access to the airways. The hypothesis was that the use of the videolaryngoscope modifies the practice of tracheal intubation, the main outcome being the need for help for the anaesthesiologist or the nurse anaesthetist in performing tracheal intubation.
Methods
Patient and public involvement
Patients and public are not involved in any of the phases of this study.
Study design and setting
The McGrath Mac Videolaryngoscope versus McGrath Mac No-Video Laryngoscope for Orotracheal Intubation in Operating Room (video–no-video study) trial was an institutionally sponsored, single-blinded, multicentre, two parallel-groups randomised clinical trial conducted at three Health Institutions in France (one academic, one non-profit and one profit).
Patient population
Inclusion criteria were patients aged 18 years minimum, requiring general anaesthesia and orotracheal intubation with a single lumen tube, without a predicted difficult intubation (Arne score <11).11 Non-inclusion criteria were currently pregnant or breastfeeding woman, out-patients who could not be contacted within 24 hours following surgery, patients requiring a rapid-sequence intubation, and patients for whom general anaesthesia using sufentanil, propofol, atracurium or rocuronium was not suitable.
Inclusion and exclusion criteria were assessed by an investigator who could be different from the one who was to perform the intubation. Once in the operating room, inclusion criteria were confirmed by the anaesthesiologist in charge and randomisation was managed online.
Randomisation, allocation concealment
Centralised randomisation using fixed-size blocks had been performed by an independent biostatistician not involved in the trial. The randomisation scheme was balanced 1:1 and stratified by centre. Each patient received a unique patient number and a randomisation number (patient code) when the investigator connected to an Interactive Web Response System managed by an independent Contract Research Organisation (Epiconcept Company, 75012, Paris, France) using a protected password just before the induction of anaesthesia. Thus, patients were randomised into two groups: a video group, in which intubation is performed using a McGrath Mac videolaryngoscope with its screen activated, and a no-video group, in which intubation is performed using a McGrath Mac videolaryngoscope with its screen hidden. The software used to allocate the patients to their group also was in-live fulfilled to collect data by the investigator in an electronic report form, ensuring concealment.
Study protocol
Patients received care during the induction and intubation periods from an anaesthesiologist and a nurse anaesthetist as is usual in the hospitals where the protocol took place. All anaesthesiologists and nurse anaesthetists had performed at least ten intubations with the McGrath Mac Videolaryngoscope. This experience seems sufficient since the learning curve is steep especially among this population12 especially since the professionals received specific training pertaining to the study procedures prior to the beginning of the trial including the fact that they must rely on the video screen in the video group and use the direct view in the no-video group.
On arrival in the operating room, a dedicated peripheral intravenous cannula for the administration of intravenous anaesthetics was placed on the forearm, and routine monitoring was performed including bispectral index monitoring and quantitative measurement of neuromuscular block at the adductor pollicis. Patients were positioned in dorsal decubitus with the head on a 7 cm high pillow. Preoxygenation was achieved using a face mask, and oxygen at a flow of 15 L/min or greater for at least 3 min to achieve an end-tidal oxygen fraction of at least 90%.
General anaesthesia was then induced by injecting sufentanil, propofol and a neuromuscular blocking agent (atracurium or rocuronium) once the patient was unconsciousness. Intubation was performed by the anaesthesiologist or the nurse anaesthetist using the device allocated at random when bispectral index was under 60 and when there was no more muscle response to the train of four stimulation.
Intubation was performed using the video screen of the device in the McGrath Mac Videolaryngoscope group (video group) while the video screen was hidden with an opaque cover in the McGrath Mac No-Video Laryngoscope group (no-video group). Endotracheal tube size was 7 for women and 7.5 for men with blades size 3 or four according the practitioner’s preference.
Asking for help from the other member of the anaesthetic team was at the discretion of the individual performing intubation if he/she deemed it necessary to perform an easy and atraumatic intubation. Complementary techniques consisted in (1) backward, upward and rightward pressure (BURP) manoeuvre; (2) rail-roading the tube over a gum elastic bougie; (3) removing the opaque cover of the videolaryngoscope or change in the operator. If all these techniques failed, other manoeuvres could be used: (1) insertion of a stylet into the tube; (2) changing the blade and (3) removal of the pillow. Rescue techniques (insertion of an Intubating Laryngeal Mask Airway, transtracheal oxygenation, fiberoptic intubation, awakening) were considered if necessary according to the national recommendations.13 Number of intubation attempts, time to intubate or number of alternative techniques were not limited by the protocol.
After intubation, the cuff was inflated, the tube was connected to the ventilator, and intratracheal tube position was confirmed by analysing the capnography curve.
Anaesthesia was conducted according to good practices.
Patients were reviewed the following day. Sore throat and hoarseness were evaluated, and adverse events collected by investigators not knowing the group to which the patient has been assigned.
Data collection
All cases were video recorded by a person not involved in the study which followed a mandatory script. This person, placed at the feet of the patient, was unable to see whether the screen of the videolaryngoscope was activated. Videorecording began with preoxygenation and ended with the capnographic confirmation of successful tracheal intubation.
The framing of the videos was done in such a way that the patient’s anonymity was respected. Otherwise, the patient’s face was blurred before analysis.
Analysis of each video was performed by two anaesthesiologists blinded to the study group since the screen, transparent or opaque, of the videolaryngoscope was not apparent. The videos were reviewed by both anaesthesiologists in case of discordance.
All the variables used for the study were retrieved from the video apart from the glottis exposure which was recorded in real time by the person who performed the intubation using the Cormack and Lehane modified score and the Percentage of Glottis Opening Scale (POGO) score.14 15
Timeline of measurement of each variable is summarised in online supplemental table.
bmjopen-2021-049275supp001.pdf (93KB, pdf)
Primary and secondary outcomes
The primary outcome, the proportion of orotracheal intubations where assistance was necessary on request of the operator, was obtained from the video of the intubation sequence.
Secondary outcomes included during the intubation period (1) the intubation difficulty scale,16 (2) the Cormack and Lehane grade of glottis visibility,14 (3) the POGO score,15 (4) the proportion of patients intubated using alternative techniques: (BURP, rail-roading the tube over a gum elastic bougie, insertion of a stylet in the tube, laryngeal mask airway, fiberoptic endoscopy or rescue percutaneous or surgical transtracheal oxygenation …), anaesthesia discontinuation, (5) the time from introduction of the McGrath videolaryngoscope in the mouth to the confirmation of tracheal tube position based on partial pressure of end-tidal exhaled carbon dioxide (third capnogram), (6) the proportion of patients having had an oesophageal intubation, (7), the ease of intubation evaluated by the anaesthesiologist using a 11-level numeric scale from 0 (very easy) to 10 (very difficult), (8) the requirement of an abnormal traction force to intubate, (9) the heart rate and mean arterial pressure measured just before and after intubation and (10) complications such as oxygen desaturation (peripheral oxygen saturation <92%) or hypotension having required treatment. The cooperation between members of the anaesthesiology team during intubation was graded using a 4-point scale (0=no cooperation at all, 3=a great deal of cooperation).17
The postoperative secondary outcomes included the proportion of patient suffering from hoarseness18 or sore throat19 on postoperative day 1. Other adverse events will be also collected.
Sample size calculation
The number of patients to be included took into consideration the frequency with which external laryngeal pressure is used. Adnet et al published in 2001 a survey of tracheal intubation difficulty among 1171 surgical patients and found that the Intubation Difficulty Scale was >0 in 522 cases (45%) and that external laryngeal pressure, requiring an assistant to help, was used in 271 of these cases (23% of all patients).20 Based on this data, the expected rate for the assistance of another person for intubation was 25% for patients in the No-Video group. Presuming that the video function would decrease this proportion to 12.5%, with type 1 error set at 5% and power set at 80%, 131 patients were needed in each group (ie, 262 patients total). We planned to recruit 300 patients to mitigate an attrition of the sample or the absence of values.
Statistical analyses
Statistical analysis was conducted using the principle of the intention-to-treat analysis. Results are presented as number (proportion) (95% CI) for categorical variables and compared by the χ2 test when the number of observations was greater than five, and by the Fischer’s exact test when one of the numbers was less than five. For continuous variables, results are presented as median (IQR) (CI 95 of the median) and compared by a Wilcoxon rank-sum test, after verification of the normality with a Shapiro-Wilk test. All tests were two sided. The types of all variables, categorical or continuous, are summarised in online supplemental table.
P values of less than 0.05 were considered significant. Bonferroni correction was used to correct p values of the comparison between groups of the Intubation Difficulty Scale and of its parameters.
The statistics were generated using SAS V.9.4 software.
Results
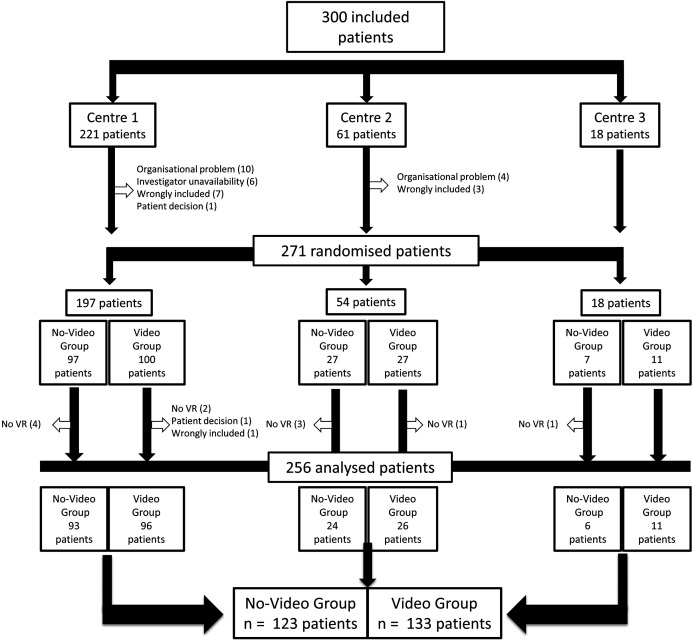
Patients were recruited between 29 November 2016 and the 1 April 2019. Of 300 included patients, 271 were randomised and 256 analysed with 123 patients in the no-video group and 133 in the video group (figure 1).
Figure 1.
Flow chart no-video group: intubation was performed using a McGrath MAC videolaryngoscope with its screen deactivated video group: intubation was performed using a McGrath MAC videolaryngoscope with its screen activated. no VR, no video recording.
Baseline features were well balanced between groups (table 1).
Table 1.
Patient characteristics
| Video group (n=133) | No-video group (n=123) | |
| Male patients | 61 (45.9) (37.2 to 54.7) | 58 (47.1) (38.3 to 56.4) |
| Age, years | 58 (23) (54 to 62) | 60 (26) (52 to 64) |
| Body mass index, kg/m-2 | 25.1 (6.3) (24.2 to 26.1) | 24.7 (5.8) (23.7 to 25.4) |
| Arné score11 | 2 (5) (2 to 3) | 2 (4) (2 to 2) |
| Previous knowledge of difficult intubation | 1 (0.8) (0.0 to 4.1) | 1 (0.8) (0.0 to 4.4) |
| Pathologies associated with difficult intubation | 1 (0.8) (0.0 to 4.1) | 0 |
| Clinical symptoms of airway pathology | 6 (4.5) (1.7 to 9.6) | 6 (4.9) (1.8 to 10.3) |
| Interincisor gap (<25 mm) and limited mandible luxation | 0 | 0 |
| Thyromental distance <65 mm | 4 (3.0) (0.8 to 7.5) | 2 (1.6) (0.2 to 5.7) |
| Maximum range of head and neck movement ≤80° | 4 (3.0) (0.8 to 7.5) | 1 (0.8) (0.0 to 4.4) |
| Mallampati score | ||
| 1 | 71 (53.4) (44.5 to 62.1) | 69 (56.1) (46.9 to 65.0) |
| 2 | 51 (38.3) (30.0 to 47.2) | 42 (34.1) (25.8 to 43.2) |
| 3 | 10 (7.5) (3.7 to 13.4) | 12 (9.7) (5.1 to 16.4) |
| 4 | 1 (0.8) (0.0 to 4.1) | 0 |
Categorical variables are presented as number (proportion) (Confidence Interval 95 of the percentage).
Continuous variables are presented as median (Interquartile Range) (Confidence Interval 95 of the median).
Requirement for assistance was not decreased in the video group (36.1% (95% CI 27.9% to 44.9%) vs 45.5% (95% CI 36.5% to 54.7%) in the no-video group, p=0.74 after Bonferroni correction; OR: 0.7 (95% CI 0.4 to 1.1) and absolute risk: 0.10 (95% CI −0.03 to 0.22) (table 2). Requirement for assistance was similar between groups when considering each centre separately (p=0.99).
Table 2.
Intubation variables (final values)
| Video group (n=133) | No-video group (n=123) | P value | |
| Required assistance by the additional person, yes | 48 (36.1) (27.9 to 44.9) | 56 (45.5) (36.5 to −54.7) | 0.74* |
| Intubation Difficulty Scale (IDS), classes | 0.05* | ||
| IDS=0 | 77 (57.9) (49.0 to 66.4) | 50 (40.6) (31.9 to 49.9) | |
| 0<IDS ≤ 5 | 55 (41.3) (32.9 to 50.2) | 68 (55.3) (46.1 to 64.2) | |
| >5 | 1 (0.8) (0.0 to 4.1) | 5 (4.1) (1.3 to 9.2) | |
| Railroading the tube over a gum elastic bougie, yes | 16 (12.0) (7.0 to 18.8) | 13 (10.6) (5.7 to 17.4) | 0.71 |
| Percentage of glottic opening score | 100 (10) (100–100) | 80 (40) (80–90) | <0.001 |
| Oesophageal Intubation, yes | 4 (3.1) (0.8 to 7.5) | 2 (1.6) (0.2 to 5.7) | 0.68 |
| BURP, yes | 46 (34.6) (26.6 to 43.3) | 53 (43.1) (34.2 to 52.3) | 0.16 |
| Removing the cover, yes | 9 (7.3) (2.7 to 11.9) | ||
| Time between the introduction of the McGrath and the third capnogram, sec | 50 (31) (46 to 57) {113} | 49 (31) (42 to 53) {104} | 0.13 |
| Ease of intubation, 0 (very easy) to 10 (very difficult) | 0 (2) (0 to 0) | 2 (4) (1 to 2) | <0.001 |
Categorical variables are presented as number (proportion) (Confidence Interval 95 of the percentage).
Continuous variables are presented as median (Interquartile Range) (Confidence Interval 95 of the median).
In cases in which the data are incomplete, the number of available data points is indicated between curly brackets {}.
*P value with Bonferroni correction.
BURP, backward, upward and rightward pressure.
The Intubation Difficulty Scale was similar between groups (p=0.05; table 2); its parameters are presented in table 3.
Table 3.
Parameters of the Intubation Difficulty Scale, (final values)
| Video group (n=133) | No-video group (n=123) | P value* | |
| No of attempts, classes | 0.99 | ||
| 1 | 122 (91.7) (87.0 to 96.4) | 112 (91.1) (86.0 to 96.1) | |
| 2 | 10 (7.5) (3.0 to 12.0) | 6 (4.9) (1.1 to 8.7) | |
| 3 | 1 (0.8) (0.0 to 2.2) | 4 (3.2) (0.1 to 6.4) | |
| 4 | 0 (0.0) (0.0 to 0.0) | 1 (0.8) (0.0 to 2.4) | |
| Required assistance by the additional person, yes | 48 (36.1) (27.9 to 44.9) | 56 (45.5) (36.5 to 54.7) | 0.74 |
| No of alternatives techniques | |||
| None | 85 (63.9) (55.7 to 72.1) | 69 (56.1) (47.3 to 64.8) | |
| 1 | 34 (25.6) (18.1 to 33.0) | 42 (34.1) (25.8 to 42.6) | |
| 2 | 14 (10.5) (5.3 to 15.7) | 12 (9.8) (4.5 to 15.0) | |
| Cormack and Lehane grade | 0.001 | ||
| 1 | 111 (83.5) (76.0 to 89.3) | 63 (51.2) (42.0 to 60.3) | |
| 2a | 19 (14.3) (8.8 to 21.4) | 33 (26.8) (19.2 to 35.6) | |
| 2b | 1 (0.8) (0.0 to 4.1) | 18 (14.6) (8.9 to 22.1) | |
| 3 | 2 (1.5) (0.2 to 5.3) | 9 (7.3) (3.4 to 13.4) | |
| Abnormal traction force, yes | 13 (9.8) (5.3 to 16.1) | 27 (21.9) (15.0 to 30.3) | 0.04 |
| Vocal cord position, abduction, yes | 133 (100) (100 to 100) | 123 (100) (100 to 100) | NA |
In cases in which the data are incomplete, the number of available data points is indicated between curly brackets {}.
Results are presented as number (proportion) (Confidence Interval 95 of the percentage).
*P values were calculated using Bonferroni correction.
Glottis visualisation was significantly better in the video group with a lower Cormack and Lehane score (p<0.001), and higher percentage of glottic opening score (p<0.001). There was no difference between groups considering other outcomes, in particular for duration of intubation, number of attempts, use of complementary techniques (BURP and railroading), except for ease of intubation, better in the Video group (p=0.001), and for requirement of an abnormal traction force, lower in the video group (p=0.007). The opaque cover was withdrawn in 7.3% of the cases in the no-video group (tables 2 and 3).
Bispectral index increased after intubation only in the Video group (p=0.04). Heart rate and mean arterial pressure increased in both groups after intubation with a smaller increase in mean arterial pressure in the video group (p=0.04) (table 4).
Table 4.
Bispectral index, heart rate and arterial pressure measurements (change from baseline and from preintubation period)
| Group | Before induction | Before intubation | After intubation | Difference between before and after intubation | Before intubation vs after intubation |
Video vs No-video group |
|
| P value | |||||||
| BIS | Video group | 94 (8) (93 to 97) {74} |
40 (19) (37 to 45) {88} |
44 (18) (40 to 47) {102} |
2 (15) (0 to 5) {85} |
0.11 | 0.20 |
| No-video group | 96 (6) (94 to 97) {75} |
46 (21) (42 to 48) {84} |
50 (17) (46 to 53) {89} |
5 (17) (2 to 9) {79} |
0.04 | ||
| HR, beats/min | Video group | 74 (20) (71 to 78) {129} |
67 (16) (63 to 70) {130} |
79 (27) (75 to 82) {131} |
9 (17) (7 to 14) {129} |
<0.001 | 0.103 |
| No-video group | 72 (22) (68 to 76) {115} |
65 (16) (61 to 69) {121} |
83 (23) (78 to 86) {121} |
13 (19) (10 to 19) {120} |
<0.001 | ||
| MAP, mm Hg | Video group | 98 (20) (93 to 100) {128} |
74 (24) (72 to 81) {125} |
82 (28) (78 to 87) {125} |
4 (25) (0 to 7) {121} |
0.007 | 0.04 |
| No-video group | 99 (22) (97 to 104) {114} |
77 (22) (74 to 84) {118} |
87 (41) (82 to 93) {113} |
12 (39) (5 to 20) {110} |
<0.001 | ||
Results are presented as median (IQR) (95% CI of the median). Number of available data points is indicated between curly brackets {}.
BIS, Bispectral Index; HR, heart rate (beats per minute); MAP, mean blood pressure (mmHg).
Communication and behaviour within the anaesthesia team was appropriate in all cases (values of 3). Oxygen desaturation, hypotension or hypertension requiring treatment during the intubation period and postoperative complications (hoarseness or sore throat) were observed similarly in both groups (table 5).
Table 5.
Intraoperative and postoperative complications
| Video group (n=133) | No-video group (n=123) | P value | |
| Intraoperative complications | |||
| Oxygen desaturation (peripheral oxygen saturation <92%) | 2 (1.5) (0.2 to 5.3) | 0 | 0.50 |
| Hypotension having required treatment | 4 (3.0) (0.1 to 5.9) | 3 (2.4) (0.0 to 5.2) | 0.99 |
| Hypertension having required treatment | 0 (0.0) (0.0 to 0.0) | 1 (0.0) (0.0 to 2.4) | 0.48 |
| Dental injury | 0 | 0 | |
| Postoperative complications | |||
| Hoarseness | {n=34} | {n=37} | 0.99 |
| Grade 1 | 23 (68) (49.5 to 82.6) | 25 (68) (50.2 to 82.0) | |
| Grade 2 | 11 (32) (17.4 to 50.5) | 12 (32) (18.0 to 49.8) | |
| Grade 3 | 0 | 0 | |
| Sore throat | {n=42} | {n=33} | 0.41 |
| Grade 1 | 33 (78.6) (63.2 to 89.7) | 23 (69.7) (51.3 to 84.4) | |
| Grade 2 | 8 (19.0) (8.6 to 34.1) | 10 (30.3) (15.6 to 48.7) | |
| Grade 3 | 1 (2.4) (0.1 to 12.6) | 0 |
Results are presented as number (proportion) (Confidence Interval 95 of the percentage).
When the data were incomplete, the number of available data points is indicated between curly brackets {}.
No serious adverse event occurred.
Discussion
In this video-no video trial performed in surgical patients without particular risk of difficulty in airway management, videolaryngoscopy did not decrease the requirement for assistance to perform intubation.
This result corroborates studies which consider that the use of a videolaryngoscope is of little interest in the management of such patients. Advantages of videolaryngoscopy seem to be secondary, especially better glottic visualisation7 which does not translate directly into a higher success rate on the first attempt.7 21
There is no universal rule regarding anaesthetic staffing neither for qualifications, anaesthesiologists or registered nurse anaesthetists nor for the required number during the whole procedure or during the induction-intubation sequence. In our study, patients received care during the induction and intubation periods from an anaesthesiologist and a nurse anaesthetist as is usual in the hospitals where the protocol takes place. This probably explains the high percentage of recourse to a second person since he or she is available without delay. Such incidence is not reported per se in studies contrary to the use of alternative techniques. Except for cases where tracheal intubation is easy, help is needed to perform a BURP manoeuvre or give a gum elastic bougie or a stylet for example.
Interestingly, Jones et al studied the impact of the use the C-MAC videolaryngoscope (Karl Storz Endoscopy, Slough, Berkshire, UK) on nurse anaesthetist working practices and training which has not previously been reported.22 Most respondents claimed that the videolaryngoscope improved team work with the anaesthesiologist and allow anticipation of the required alternative technique by observing the view at laryngoscopy on a screen. Laryngoscopy is thus moving from an individual process to a shared procedure. Therefore, it is better to use a screen separate from the videolaryngoscope. The participation of the nurse facilitated by the glottic visualisation is particularly valuable when he or she performs a BURP to quickly find the most efficient gesture avoiding also a worsening of the glottic visualisation.23
Alternative techniques were used at a similar incidence in both groups, mainly the BURP in around 40% of the patients and the use of a gum elastic bougie (railroading technique) in around 10% of the patients. Such incidence of use of BURP is not surprising in that incidences of 23%20 and 36%24 have been reported previously. High incidence of their use is probably explained by the fear of dental breakage, with an incidence up to 0.2% of all general anaesthesia procedures, is responsible for 40% of the complaints against anaesthesiologists in France.25
The BURP manoeuvre improves laryngoscopic visualisation more easily than simple back pressure on the larynx26 and limits the forces exerted during laryngoscopy.27 28 However, the best condition is represented when the assistant can view the laryngeal view in real time on a remote screen during intubation to adapt the BURP to have the best glottic view.29 The McGrath MAC videolaryngoscope has not this possibility contrary to other videolaryngoscopes which have the possibility to have a remote screen and thus be accessible to all participants (Airtraq, Glidescope and King Vision, eg). This is important because poor BURP practice is counterproductive and aggravates glottic vision.30 The second alternative technique used is tube rail-roading over a gum elastic bougie.31 This technique of choice when BURP does not align the oral, pharyngeal and laryngeal axes is more complex since it requires good coordination between the members of the team.
It should also be noted that the anaesthesiologist chose to remove the screen cover to benefit from the video function of the videolaryngoscope in 7% of the cases.
Finally, complications noticed during the induction-intubation sequence and after it up to the next day were similar in both groups. Contrary to others who used a Glide Scope, we did not find that the use of a videolaryngoscope decreased the incidence and severity of sore throat and hoarseness after tracheal intubation.32
The strengths of the study come from the usual practice of the centres which were used, including especially the staffing ratio with one anaesthesiologist and one nurse anaesthetist (1 to 1) in each case. But this permanent presence of a two-person team may have induced a bias because it facilitates the practice of an alternative technique. Another strength is the use of the same laryngoscope in both groups, the only difference being the use or not of the video screen). The last strength is that this study is the first single blinded study since most of the criteria of judgement, in particular the main criterion, are obtained from a videorecording of the intubation sequence without the possibility for the evaluator to know if the video function of the McGrath MAC videolaryngoscope was used.
One weakness comes from the choice of the McGrath MAC videolaryngoscope. We chose this device since it requires limited training because of its similarity to the Macintosh laryngoscope with especially a similar blade, a small size and a low cost. Consequently, our results could be valid for other videolaryngoscopes having a blade-shape like the Macintosh laryngoscope (C-MAC or APA, eg), but not acutely angled videolaryngoscopes (McGrath and GlideScope, eg) or with an integrated channel videolaryngoscope (KingVision, AWS-S200 and Airtraq). Another point explaining why generalisation is not possible is that our procedure includes the simultaneous presence of an anaesthesiologist, and a nurse anaesthetist as is the rule in the healthcare institutions that participated in the study, but this practice is far from being the rule. In these institutions, anaesthesiologists and nurse anaesthetists have an identical practice when intubation concerns patients with no particular risk of access to the airways. Other weakness are the risk of 7% misclassification when using the Arné score to predict difficult intubation11 and the large number of patients who were not seen the day after the operation, which makes the postoperative data very questionable. Another major point is that we used the need for assistance from a member of the anaesthetic team as the primary outcome. This choice is not usual, but it seemed to us more interesting than the time to successful tracheal intubation or the number of attempts, outcomes that have little interest in a population without risk of difficult intubation. On the other hand, we felt it was important to evaluate the possible benefit of a new technology on the ergonomics of the work of anaesthesiologists. However, one of the limitations of our primary outcome is its personal nature and we could have been more specific in the need for assistance and possibly create a score combining for example force exerted and POGO. We sought to have this primary outcome assessed blind to the randomisation arm. As noted, the person recording the video sequence was positioned at the foot of the patient, making it impossible to see if there was an opaque cover on the videolaryngoscope screen. It is possible, however, that the persons who was watching the video could see, or thought they could see, if the video function was being used. Finally, eight patients were missing in the video-group since the calculation of the number to be included resulted in a minimum number of 131 patients in each group. However, it is highly unlikely that this would change the results significantly.
Conclusion
The Difficult Airway Society guidelines for unanticipated difficult intubation recommend that all anaesthesiologists are trained to use a videolaryngoscope and that they have immediate access to one5 and several authors have called for videolaryngoscopes to be used for all intubations.9 One would have expected that the use of a videolaryngoscope, that is, the introduction of a new technology, would have changed the practice of intubation. In patients at low risk of intubation difficulty, the expected benefit should have been greater autonomy for the person performing the procedure. Our results do not confirm this hypothesis.
Supplementary Material
Acknowledgments
Assistance with the study: We would like to thank Polly GOBIN and by American Journal Experts for their linguistic help.
Footnotes
Contributors: OB, XP, J-MD, MF and MLG contributed substantially to conception and design of the study. OB, ZC, JO, L-AT, XP, SM and MLG contributed substantially to acquisition of data. All authors participated to the analysis and interpretation of data. TK performed the statistical analysis. MF wrote the first draft. MF took responsibility as the guarantor for the integrity of the work as a whole, from inception to published article. All authors revised it critically for important intellectual content. All authors approved the final version.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. Dataset are available from the Dryad repository (DOI: 10.5061/dryad.280gb5mp6).
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was approved by Comité de Protection des Personnes Ile de France VIII, Boulogne Billancourt, France, no 160108, 19 February 2016, Chairman Bertrand MUSSETTA.
References
- 1.Caplan RA, Posner KL, Ward RJ, et al. Adverse respiratory events in anesthesia: a closed claims analysis. Anesthesiology 1990;72:828–33. 10.1097/00000542-199005000-00010 [DOI] [PubMed] [Google Scholar]
- 2.Lienhart A, Auroy Y, Péquignot F, et al. Survey of anesthesia-related mortality in France. Anesthesiology 2006;105:1087–97. 10.1097/00000542-200612000-00008 [DOI] [PubMed] [Google Scholar]
- 3.Cook TM, Scott S, Mihai R. Litigation related to airway and respiratory complications of anaesthesia: an analysis of claims against the NHS in England 1995-2007. Anaesthesia 2010;65:556–63. 10.1111/j.1365-2044.2010.06331.x [DOI] [PubMed] [Google Scholar]
- 4.Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task force on management of the difficult airway. Anesthesiology 2013;118:251–70. 10.1097/ALN.0b013e31827773b2 [DOI] [PubMed] [Google Scholar]
- 5.Frerk C, Mitchell VS, McNarry AF, et al. Difficult airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth 2015;115:827–48. 10.1093/bja/aev371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pieters BMA, Maas EHA, Knape JTA, et al. Videolaryngoscopy vs. direct laryngoscopy use by experienced anaesthetists in patients with known difficult airways: a systematic review and meta-analysis. Anaesthesia 2017;72:1532–41. 10.1111/anae.14057 [DOI] [PubMed] [Google Scholar]
- 7.Lewis SR, Butler AR, Parker J, et al. Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation: a Cochrane systematic review. Br J Anaesth 2017;119:369–83. 10.1093/bja/aex228 [DOI] [PubMed] [Google Scholar]
- 8.Xue FS, Liu GP, Sun C. Videolaryngoscope as a standard intubation device. Br J Anaesth 2015;115:137–8. 10.1093/bja/aev175 [DOI] [PubMed] [Google Scholar]
- 9.Zaouter C, Calderon J, Hemmerling TM. Videolaryngoscopy as a new standard of care. Br J Anaesth 2015;114:181–3. 10.1093/bja/aeu266 [DOI] [PubMed] [Google Scholar]
- 10.Cook TM, Boniface NJ, Seller C, et al. Universal videolaryngoscopy: a structured approach to conversion to videolaryngoscopy for all Intubations in an anaesthetic and intensive care department. Br J Anaesth 2018;120:173–80. 10.1016/j.bja.2017.11.014 [DOI] [PubMed] [Google Scholar]
- 11.Arné J, Descoins P, Fusciardi J, et al. Preoperative assessment for difficult intubation in general and ENT surgery: predictive value of a clinical multivariate risk index. Br J Anaesth 1998;80:140–6. 10.1093/bja/80.2.140 [DOI] [PubMed] [Google Scholar]
- 12.Savoldelli GL, Schiffer E, Abegg C, et al. Learning curves of the Glidescope, the McGrath and the Airtraq laryngoscopes: a manikin study. Eur J Anaesthesiol 2009;26:554–8. 10.1097/EJA.0b013e3283269ff4 [DOI] [PubMed] [Google Scholar]
- 13.Langeron O, Bourgain JL, Laccoureye O. [Difficult airway algorithms and management]. Ann Fr Anesth Reanim 2008;27:41–5. [DOI] [PubMed] [Google Scholar]
- 14.Cormack RS. Cormack-Lehane classification revisited. Br J Anaesth 2010;105:867–8. 10.1093/bja/aeq324 [DOI] [PubMed] [Google Scholar]
- 15.Levitan RM, Ochroch EA, Kush S, et al. Assessment of airway visualization: validation of the percentage of glottic opening (POGO) scale. Acad Emerg Med 1998;5:919–23. 10.1111/j.1553-2712.1998.tb02823.x [DOI] [PubMed] [Google Scholar]
- 16.Adnet F, Borron SW, Racine SX, et al. The intubation difficulty scale (IDS): proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology 1997;87:1290–7. 10.1097/00000542-199712000-00005 [DOI] [PubMed] [Google Scholar]
- 17.Kraus MW, Huang C, Keltner D. Tactile communication, cooperation, and performance: an ethological study of the NBA. Emotion 2010;10:745–9. 10.1037/a0019382 [DOI] [PubMed] [Google Scholar]
- 18.Stout DM, Bishop MJ, Dwersteg JF, et al. Correlation of endotracheal tube size with sore throat and hoarseness following general anesthesia. Anesthesiology 1987;67:419–21. 10.1097/00000542-198709000-00025 [DOI] [PubMed] [Google Scholar]
- 19.Capan LM, Bruce DL, Patel KP, et al. Succinylcholine-Induced postoperative sore throat. Anesthesiology 1983;59:202–6. [PubMed] [Google Scholar]
- 20.Adnet F, Racine SX, Borron SW, et al. A survey of tracheal intubation difficulty in the operating room: a prospective observational study. Acta Anaesthesiol Scand 2001;45:327–32. 10.1034/j.1399-6576.2001.045003327.x [DOI] [PubMed] [Google Scholar]
- 21.Hoshijima H, Mihara T, Maruyama K, et al. McGrath videolaryngoscope versus MacIntosh laryngoscope for tracheal intubation: a systematic review and meta-analysis with trial sequential analysis. J Clin Anesth 2018;46:25–32. 10.1016/j.jclinane.2017.12.030 [DOI] [PubMed] [Google Scholar]
- 22.Jones L, Mulcahy K, Fox J, et al. C-MAC © videolaryngoscopy: The anaesthetic assistant’s view. J Perioper Pract 2018;28:83–9. 10.1177/1750458918762314 [DOI] [PubMed] [Google Scholar]
- 23.Cook TM. The cricoid debate - balancing risks and benefits. Anaesthesia 2016;71:721–2. 10.1111/anae.13492 [DOI] [PubMed] [Google Scholar]
- 24.Akhtar M, Ali Z, Hassan N, et al. A randomized study comparing the sniffing position with simple head extension for glottis visualization and difficulty in intubation during direct laryngoscopy. Anesth Essays Res 2017;11:762–6. 10.4103/0259-1162.204206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nouette-Gaulain K, Lenfant F, Jacquet-Francillon D, et al. [French clinical guidelines for prevention of perianaesthetic dental injuries: long text]. Ann Fr Anesth Reanim 2012;31:213–23. 10.1016/j.annfar.2012.01.004 [DOI] [PubMed] [Google Scholar]
- 26.Takahata O, Kubota M, Mamiya K, et al. The efficacy of the "BURP" maneuver during a difficult laryngoscopy. Anesth Analg 1997;84:419–21. 10.1213/00000539-199702000-00033 [DOI] [PubMed] [Google Scholar]
- 27.Bishop MJ, Harrington RM, Tencer AF. Force applied during tracheal intubation. Anesth Analg 1992;74:411–4. 10.1213/00000539-199203000-00016 [DOI] [PubMed] [Google Scholar]
- 28.Bucx MJ, van der Vegt MH, Snijders CJ, et al. Transverse forces exerted on the maxillary incisors during laryngoscopy. Can J Anaesth 1996;43:665–71. 10.1007/BF03017948 [DOI] [PubMed] [Google Scholar]
- 29.Loughnan TE, Gunasekera E, Tan TP. Improving the C-MAC video laryngoscopic view when applying Cricoid pressure by allowing access of assistant to the video screen. Anaesth Intensive Care 2012;40:128–30. 10.1177/0310057X1204000114 [DOI] [PubMed] [Google Scholar]
- 30.Snider DD, Clarke D, Finucane BT. The "BURP" maneuver worsens the glottic view when applied in combination with cricoid pressure. Can J Anaesth 2005;52:100–4. 10.1007/BF03018589 [DOI] [PubMed] [Google Scholar]
- 31.Macintosh RR. An aid to oral intubation. BMJ 1949;1:28. [Google Scholar]
- 32.Najafi A, Imani F, Makarem J, et al. Postoperative sore throat after laryngoscopy with MacIntosh or glide scope video laryngoscope blade in normal airway patients. Anesth Pain Med 2014;4:e15136. 10.5812/aapm.15136 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-049275supp001.pdf (93KB, pdf)
Data Availability Statement
Data are available in a public, open access repository. Dataset are available from the Dryad repository (DOI: 10.5061/dryad.280gb5mp6).