Abstract
Objective
The cardiorespiratory fitness (CRF) of college students is showing a downward trend, this study aimed to explore the effects of three exercise programs on CRF and body composition indicators in college students.
Methods
A total of 50 non-smoking, healthy and physically inactive students were recruited from campus in Beijing, China, and randomly assigned to 4 groups: low-intensity continuous training with blood flow restriction (LICT-BFR, n = 13), moderate-intensity continuous training (MICT, n = 13), high-intensity interval training (HIIT, n = 12), and no exercise control (n = 12), the intervention continued for 8 weeks. Body composition and aerobic capacity were measured before and after the intervention.
Results
Exercise groups reached significant improvements in maximal oxygen uptake (VO2max, p < 0.01) and a decrease in body fat percentage (p < 0.05) comparing to the control group. The fat mass and visceral fat area reduced significantly (p < 0.05) with a muscle mass growth (p < 0.05) in the LICT-BFR and MICT groups comparing to the control group. Changes of fat and muscle mass were trivial in the HIIT group (p = 0.842, p = 0.247).
Conclusion
All three exercise programs can improve the CRF of college students, with LICT-BFR has the most profound effects, and MICT is more beneficial for body composition improvement than other programs. From an overall perspective, LICT-BFR should be the ideal choice, however, due to limited equipment, college students can choose MICT or HIIT according to their situations.
Keywords: LICT-BFR, HIIT, College students, CRF, Body composition
1. Introduction
As a core component of health-related physical fitness,1 cardiorespiratory fitness (CRF) has been recommended by the AHA statement2 for its ability to predict cardiovascular disease (CVD) and all-cause mortality independently. Over the past six decades, CRF has declined internationally,3,4 and there was a downward trend among college students in China.5, 6, 7 Responding to the COVID-19 outbreak, strategies such as lockdown and home quarantine were implemented to contain the pandemic, which led to insufficient physical activity and lower CRF as a consequence.8 According to a survey, physical activity (PA) has decreased,9 and sedentary behaviors have increased after the COVID-19.10 With many students returning to online classes, breaking the inactive circle and improving their PA level weekly is essential.
CRF reflects the individual PA habits, health status, genetics,2,11 and the ability to carry out a prolonged exercise involving large body muscles objectively,11 it can be tracked over time and compared across populations.2,4 According to the ACSM's Guidelines for Exercise Testing and Prescription,12 exercise to a certain threshold (i.e., intensity, duration, frequency) results in CRF improvements.13 Additionally, regular PA is crucial for maintaining a healthy weight and muscular fitness,14 which can be challenging for college students due to external factors such as academic stress15 and the university's Recreational Services.16 The importance of preventing weight gain in early adulthood to avoid premature deaths was highlighted,17 especially in fat mass control. Excess fat mass accumulation (particularly the abdominal fat) and low lean body mass can adversely affect health, increasing the mortality risk in later life.18,19
Based on the current situation, effective PA interventions are required. Moderate-intensity continuous training (MICT) and high-intensity interval training (HIIT) improve physical fitness across various populations, with the exercise effects widely compared.20,21 Blood flow restriction (BFR) exercise is known for the inflated cuff applied to the limb's proximal end during various training forms, resulting in musculoskeletal improvements.22 This technique is a viable replacement for traditional heavy-load training.23 Besides, several studies reported an increased maximal oxygen uptake (VO2max) after low-intensity continuous training with blood flow restriction (LICT-BFR) compared to other aerobic exercise forms.24,25 It appears to be the venous blood volume pooling and restricted arterial blood inflow simultaneously, resulting in a decreased stroke volume and increased HR while maintaining cardiac output.26 However, few researchers have compared the physical fitness responses of LICT-BFR to HIIT and MICT simultaneously.
Thus, this study aimed to compare the effects of LICT-BFR, HIIT, and MICT on CRF level and body composition in college students through an 8-wk intervention. Based on previous studies,23, 24, 25 we hypothesized that MICT will show less training effects on VO2max and body composition than HIIT and LICT-BFR.
2. Methods
2.1. Participants
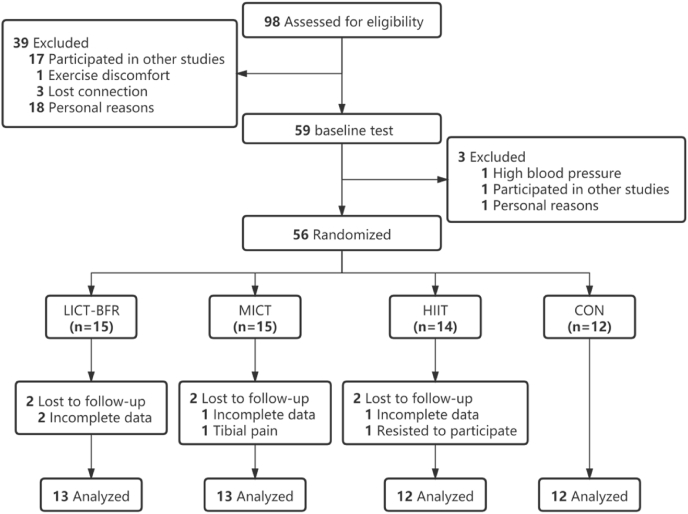
Fifty-six non-smoking college students (age 18–25 years) were recruited into this study. All participants were physically inactive for at least three months according to the International Physical Activity Questionnaire (IPAQ) results. The exclusionary criteria included: 1. Individuals with diagnosed cardiovascular, respiratory, or metabolic diseases; 2. Individuals with musculoskeletal disorders or other clinical issues that cannot complete the training sessions. All participants provided written informed consent and completed the Physical Activity Readiness Questionnaire before baseline tests. This study was approved by the Ethics Committee for Human Experiments at Beijing Sport University (No. 2020128H). Sample size was determined a priori (G∗Power, Version 3.1.9.2) using ANOVA with the effect size of 0.25. This study required approximately 52 for all outcome measures to achieve a statistical power>0.95 with an alpha level of p < 0.05. After further exclusion, we arrived at the final enrollment of 50 participants randomly assigned to four groups: LICT-BFR, MICT, HIIT, and CON groups (Fig. 1). Baseline characteristics are presented in Table 1. No significant baseline differences existed between groups for any variable.
Fig. 1.
Flow diagram depicting the study design.
Table 1.
Baseline characteristics.
| Variables | Group |
|||
|---|---|---|---|---|
| LICT-BFR (M = 4, F = 9) | MICT (M = 3, F = 10) | HIIT (M = 4, F = 8) | CON (M = 2, F = 10) | |
| Age (y) | 19.85 ± 1.46 | 20.77 ± 1.96 | 21.33 ± 2.54 | 20.42 ± 1.93 |
| Height (cm) | 163.23 ± 9.15 | 166.86 ± 8.37 | 170.23 ± 11.48 | 167.57 ± 8.12 |
| Weight (kg) | 56.92 ± 10.40 | 64.03 ± 14.28 | 65.50 ± 16.78 | 59.96 ± 9.58 |
| BMI (kg/m2) | 21.19 ± 2.08 | 22.83 ± 3.76 | 22.31 ± 3.59 | 21.33 ± 2.93 |
Note: All data are presented in means ± SD. M, male; F, female.
2.2. Training protocol
All participants were required to refrain from any form of physical activity other than the study protocol. The intervention was 3 times a week lasting for 8 weeks in total. A standardized 5-min warm-up was preceded each session and 10-min resting phase after, all sessions were performed on the treadmill. Participants in the MICT group engaged in 45-min of training session at 64–70% HRmax for the first week, and 64–76%HRmax for the remaining 7 weeks. Participants in the HIIT group performed a 4 × 4 interval training session, containing 4-min of running at 85–90% HRmax followed by 3-min of active resting at 64–70%HRmax for the first week, and 4-min of running at 90–95%HRmax followed by 3-min of active resting at 64–76%HRmax for 7 weeks (Table 2).28
Table 2.
Description of training protocols for each group.
| Variables | Group |
||
|---|---|---|---|
| HIIT | MICT | LICT-BFR | |
| Warm-up | 5min | 5min | 5min |
| Work load | (4 + 3)∗4 = 28min | 45min | 15min |
| Resting phase | 10min | 10min | 10min |
| Exercise HR (b/min) | |||
| 1 wk | 85–90% HRmax; 64–70% HRmax | 64–70% HRmax | 57–63% HRmax |
| 2–8wk | 90–95% HRmax; 64–76% HRmax | 64–76% HRmax | 57–63% HRmax |
| Cuff pressure (mm Hg) | |||
| 1 wk | None | None | 200–220 |
| 2 wk | 220–240 | ||
| 3 wk | 240–260 | ||
| 4 wk | 260–280 | ||
| 5 wk | 280–300 | ||
| 6 wk | 300–320 | ||
| 7 wk | 320–340 | ||
| 8 wk | 340–360 | ||
Participants in the LICT-BFR group attached the elastic cuffs (B STRONG, USA, width 5–8 cm) at the proximal ends of the thighs with pressure set at 200 mm Hg initially, then increased by 20 mm Hg for each week, ending up with training pressure as 340–360 mm Hg for wk-8, and the pressure range was determined by echocardiography equipment (Vscan, USA). Participants in the LICT-BFR group performed a 15-min training session at 57–63%HRmax for 8 weeks.29 Participants in the CON group were asked to remain the same lifestyle receiving health education once a week as the intervention groups. Maximal heart rate was measured by polar belt during the exercise testing and the RPE was reported by each subject at the end of training sessions (Table 2).
2.3. Body composition
Height and body weight were measured by the research staff using equipment (GMCS-IV model, China), and the body mass index was calculated. The bioelectrical impedance analysis (Inbody720, South Korea) was used to measure body fat mass, muscle mass, waist-to-hip ratio, and visceral fat area. Anthropometric measurements were taken with participants wearing light clothing and no shoes. Participants were tested in a fast statement and recorded their urine, feces, and menstruation to control irrelevant variables.
2.4. Cardiopulmonary exercise testing
An exercise test to maximal voluntary exertion using the treadmill was performed according to the Bruce protocol recommended by ACSM's Guidelines for Exercise Testing and Prescription (10th edition).13 Gas exchange and ventilatory variables were analyzed using a computer-based system (COSMED, Italy). The equipment was set up in a standardized procedure with reference gas and volume calibrations. Every test began with a 5-min rest to reach steady-state conditions, and a trained research staff supervised the whole process to avoid any accident. All tests were continued until the following exhaustion criteria (at least three) were reached by the participants27: (1) VO2 maintained or dropped when workload increased; (2) Maximal heart rate > age-predicted HRmax (208–0.7∗age); (3) RER>1.1; (4) RPE>17. During the test, a polar heart rate belt was used to monitor the HR, and participants' Rating of Perceived Fatigue (RPE) was recorded on the Borg scale (6–20) within 5 s after each stage. This test was performed at baseline, 4-wk, and 8-wk of the intervention.
2.5. Statistical analysis
All analyses were conducted with Excel 2019 and SPSS version 24.0 (SPSS Inc). Continuous variables are presented as means with standard deviation (SD). Shapiro-Wilk tests were performed to determine the normality of data distribution, and baseline comparison for variables among four groups was evaluated by one-way analysis of variance (ANOVA). Between groups comparison overtime were conducted using a two-way analysis of repeated-measures ANOVA. If any significant differences occurred between groups and time interaction, the simple effect analysis was used to determine the effect. Statistical significance was considered as p < 0.05. The analysis of covariance (ANCOVA) was applied to evaluate the body composition differences between groups, with the baseline value of each outcome included as covariates.
3. Results
3.1. Cardiorespiratory fitness (VO2max)
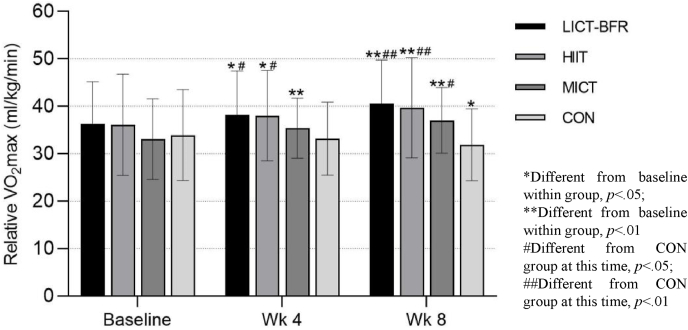
CRF is expressed relative to body weight, with VO2max expressed as mL/kg/min accounting for different body sizes. After 8 weeks, the VO2max significantly increased across all exercise groups and decreased in the CON group. For both LICT-BFR and HIIT groups, it increased from baseline to 4-wk (p < 0.05) and baseline to 8-wk (p < 0.01). As for the MICT group, the changes were significant from baseline to 4-wk (p < 0.01) and baseline to 8-wk (p < 0.01), respectively. Aerobic capacity in the CON group sightly decreased from baseline to 4-wk without reaching statistical significance and continued to drop, resulting in a significant difference from baseline and 8-wk, respectively. (Fig. 2).
Fig. 2.
Changes in relative VO2max.
Results regarding baseline and post-exercise comparison between groups are presented in Fig. 2. For both LICT-BFR and HIIT group, the VO2max was significantly higher than the CON group at 4-wk (p < 0.05) and 8-wk (p < 0.01), while changes between the MICT group and the CON group was not significant at 4-wk (p = 0.345) and increasingly reached a statistical significance at 8-wk (p < 0.05).
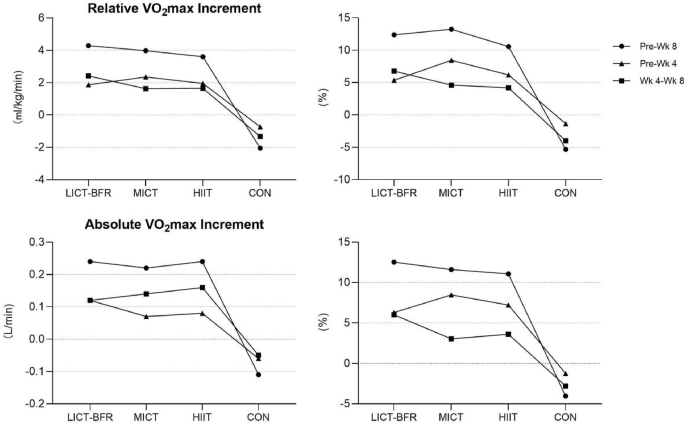
Differences existed between exercise groups when the VO2max improvements were presented numerically. After 8 weeks, the relative VO2max increased 4.29 ± 3.10 ml/kg/min (12.38 ± 9.42%)in the LICT-BFR group, 3.98 ± 2.70 ml/kg/min (13.24 ± 10.15%)in the MICT group, and 3.60 ± 2.41 ml/kg/min (10.58 ± 7.29%)in the HIIT group (Fig. 3).
Fig. 3.
Changes in relative and absolute VO2max.
As Fig. 3 presented, CRF changes in the groups were different from baseline to 4-wk and 4 to 8-wk. On the relative VO2max level, the increment was lower in the Pre-Wk 4 period than in the Wk 4-Wk 8 period in the LICT-BFR group, while the situation was opposite in the MICT and HIIT groups. On the absolute VO2max level, the increment of the LICT-BFR group was similar before and after 4-wk, while the increment was higher in the Pre-Wk 4 period than the Wk 4-Wk 8 period.
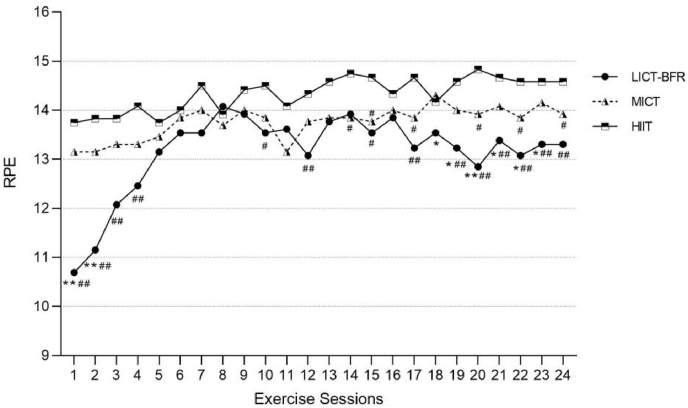
3.2. Rating of perceived exertion
The RPE of LICT-BFR group was lower than other groups through the whole period, and group differences existed at early and late sessions (Fig. 4).
Fig. 4.
RPE in exercise groups.
3.3. Body composition
Participants in the MICT group reduced fat mass significantly after 8 weeks, while the changes were trivial in the LICT-BFR (p = 0.217) and HIIT (p = 0.842) group. The CON group slightly increased at 8-wk (p = 0.075). For both LICT-BFR and MICT groups, the muscle mass increased significantly from baseline to 8-wk, but only slightly increased in the HIIT group (p = 0.247) and decreased in the CON group (p = 0.11), respectively. The body fat percentage decreased significantly across all exercise groups, but only the MICT group showed a decrease in the visceral fat area, as for the CON group, these two indicators were significantly increased after 8 weeks. No significant change existed in the waist-to-hip ratio across all groups (Table 3).
Table 3.
Changes in body composition.
| Group | Time | Fat mass (kg) | Muscle mass (kg) | Lean body mass (kg) | Skeletal muscle mass (kg) | Body fat percentage (%) | Waist-to-hip ratio | Visceral fat area (cm2) |
|---|---|---|---|---|---|---|---|---|
| LICT-BFR | Pre | 14.05 ± 4.21 | 40.34 ± 9.46 | 42.87 ± 9.93 | 23.51 ± 6.08 | 24.99 ± 6.82 | 0.82 ± 0.04 | 44.78 ± 19.34 |
| Wk 8 | 13.55 ± 3.99# | 41.19 ± 9.41∗# | 43.78 ± 9.89∗# | 24.09 ± 6.12∗# | 24.05 ± 7.23∗## | 0.82 ± 0.03 | 43.52 ± 14.61# | |
| MICT | Pre | 18.11 ± 7.11 | 43.15 ± 9.27 | 45.92 ± 9.82 | 25.30 ± 6.02 | 27.80 ± 7.06 | 0.85 ± 0.05 | 56.92 ± 23.71 |
| Wk 8 | 17.13 ± 5.88∗## | 43.96 ± 9.28∗# | 46.78 ± 9.82∗## | 25.88 ± 6.02∗## | 26.63 ± 6.42∗## | 0.84 ± 0.04 | 50.98 ± 21.08∗∗## | |
| HIIT | Pre | 15.92 ± 5.87 | 46.63 ± 12.83 | 49.58 ± 13.6 | 27.54 ± 8.33 | 24.32 ± 6.28 | 0.83 ± 0.05 | 51.59 ± 23.79 |
| Wk 8 | 15.83 ± 5.66 | 47.13 ± 12.04# | 50.08 ± 12.8# | 27.93 ± 7.87# | 24.06 ± 6.65∗# | 0.84 ± 0.05 | 52.63 ± 21.57 | |
| CON | Pre | 15.89 ± 6.60 | 41.38 ± 6.60 | 44.07 ± 6.96 | 24.17 ± 4.30 | 26.02 ± 8.22 | 0.82 ± 0.04 | 42.66 ± 20.98 |
| Wk 8 | 16.65 ± 6.84 | 40.70 ± 6.87 | 43.32 ± 7.20 | 23.66 ± 4.47 | 27.38 ± 8.91∗∗ | 0.83 ± 0.04 | 48.06 ± 19.77∗ |
Note: All data are presented in means ± SD. ∗ Different from baseline within group, p < 0.05; ∗∗ Different from baseline within group, p < 0.01; # Different from CON group at this time, p < 0.05; ## Different from CON group at this time, p < 0.01.
Considering the differences of baseline data between the four groups were not significant, the baseline data were used as covariates, and the pre-post differences of each index were used as dependent variables to conduct the analysis of covariance (ANCOVA). The similar regression slopes of each group of covariates served as a precondition for ANCOVA. Results showed that the LICT-BFR and MICT groups had a significant decreasing effect on fat mass and visceral fat area compared to the CON group without a between-group difference (p < 0.05). The exercise groups can improve muscle mass and reduce body fat percentage compared to the CON group (p < 0.05), with no significant difference among the three groups.
4. Discussion
This study showed that compared to the CON group, all three exercise programs achieved positive changes in CRF level, muscle mass, and body fat percentage after 8 weeks of intervention without any significant differences among groups. Furthermore, the fat mass and visceral fat area decreased in the LICT-BFR and MICT groups at 8-wk compared to the CON group.
The magnitude of the exercise-induced VO2max, muscle mass, and body fat changes were similar to Abe et al.29 They conducted an experiment using low-intensity cycle training with and without BFR, showing that LICT-BFR improved muscle hypertrophy and aerobic capacity. Besides, Alves et al.30 reported positive impact on body composition (i.e., muscle mass, body fat) in HIV/AIDS participants after 12-wk resistance training with BFR. The current study reached similar results with a shorter intervention (i. e., 8-wk) than 12-wk, although the participants’ diversity should be considered for this difference.
However, there are other studies inconsistent with ours. Kim31 reported low-intensity cycling with BFR (30% heart rate reserve [HRR] with BFR at 160–180 mm Hg) did not have better responses in CRF, muscle strength, and body fat compared with vigorous-intensity (60–70%HRR) and no exercise control group. Considering the participants in their study were physically active male students with no restriction on daily activity, the relative low exercise intensity may be the reason for this inconsistency. In addition, Araujo et al.32 reported similar findings with Kim. They performed intervention as water aerobics with BFR, and the underwater pressure can affect blood flow dynamics.33 Hence, the exercise condition is considered a determinant factor for this difference. Thus, the current studies showed that LICT-BFR is beneficial for CRF level, with some controversial results on body composition improvement. Furthermore, it is difficult to quantify the LICT-BFR intensity due to the unclear factors of pressure belts, and more research is required to explore this field.
In this study, VO2max increased similarly in the HIIT and the MICT groups with no significant difference. For body composition, muscle mass increased, and body fat percentage decreased in both groups. The MICT group also had positive changes in fat mass and visceral fat area.
Helgerud et al.28 reported HIIT groups (15s of running at 90–95% HRmax followed by 15s of active resting at 70% HRmax; 4 min of running at 90–95% HRmax followed by 3 min of active resting at 80% HRmax) have significantly increased VO2max compared with MICT (70%HRmax, 45min) and lactate threshold running (85%HRmax, 24.25 min) after an 8-wk intervention. The varied physical active background of participants may cause for different outcomes. Consistent with our findings, Overend et al.34 and Berger et al.35 showed that MICT and HIIT were similarly effective in enhancing aerobic capacity in previously untrained young participants, along with other similar studies.36, 37, 38, 39 In addition, HIIT has also been supported by other reviews40,41 to be an efficient method for improving CRF levels.
In this study, the MICT was the most efficient for improving body composition indicators. Andreato L. V. et al.42 reported equivalent fat loss levels of HIIT and MICT under similar energy expenditure, and results from another meta-analysis conducted by Maillard F. et al.43 showed HIIT is a time-efficient strategy to decrease fat-mass deposits, including abdominal and visceral fat mass. However, our findings are inconsistent with previous studies. Potential reasons for this difference may be the participant characteristics variations. According to these reviews, most participants were untrained adults with overweight/obesity, and for Maillard F. et al.43 the results did not show any effect of HIIT on abdominal/visceral fat tissue when the statistical analysis was performed in normal-weight participants. The inconsistent populations and caloric control in various studies make it hard to compare the exercise effects on body composition.
The energy expenditure for the HIIT and MICT groups was equivalent during sessions. However, the daily energy consumption and intake of our participants were not strictly controlled. Further studies are needed to confirm the difference between groups in fat loss. Achten et al.44 reported the fat oxidation decrease markedly and barely contributes to energy expenditure with exercise intensity above 85%VO2max, meaning that the fat loss effect in the HIIT group is not necessarily produced during training sessions. Further studies are required to explore the specific mechanism.
From an overall perspective, VO2max significantly improved for all the exercise groups, but differences existed numerically. On the relative VO2max level, the increment in the LICT-BFR group was the highest, followed by the MICT group and the HIIT group. On the absolute VO2max level, the increment was similar in the LICT-BFR and HIIT groups, higher than the MICT group. This situation is because the changes in body composition varied between the exercise groups, as reflected in reduced body fat reduction and gained muscle mass (Table 3).
The CRF trends over 8 weeks differed among the exercise groups. Potential reasons may be that the long duration of MICT and the high intensity of HIIT were hard for the participants in both groups to follow the program, affecting the experimental effects. Moreover, RPE is strongly related to exercise intensity. Training intensities corresponding to an RPE range of 11–13 should be recommended for sedentary, less fit, and untrained individuals.45 As Fig. 4 presented, RPE in the HIIT and MICT groups exceeded this range, which might cause poor compliance of the participants considering their physically inactive background. For the LICT-BFR group, a lower value for RPE was presented in most sessions. Compared to other groups, the short duration (i. e., 15-min) and lower intensity (i. e. 57-63%HRmax) might be the dominant factor for this outcome.
These results suggest that LICT-BFR can achieve similar CRF improvements with lower RPE and shorter duration than other protocols. The previous study showed that vigorous exertion increases the incidence of acute coronary events in physically inactive individuals.46 However, a 12-year follow-up study by Albert et al.47 suggested that regular vigorous exercise diminishes the risk of sudden death during vigorous exertion. HIIT appears to promote superior improvements in aerobic fitness and similar improvements in some cardiometabolic risk factors compared to MICT.48 The safety of HIIT should be considered for various populations. Therefore, the primary health screening (i.e., PAR-Q+ questionnaire) was mandatory before exercise, and the exercise choice should be based on individual situations.
In this study, several limitations should be mentioned. Due to limited equipment and methodological consideration, it was difficult to quantify the total oxygen uptake and the energy expenditure of LICT-BFR as the other exercise groups. For the blood flow restriction method, quantification cannot be achieved by a single bout of exercise considering the individual variability. The amount of restricted blood flow differs between participants when the same pressure is applied due to different sizes of the thighs,49 shifting the exercise volume from its initial calculation. Unrestricted diet of our participants can potentially affect the body composition changes caused by intervention. The seasonal changes made it impossible to quantify the authentic effect of each training protocol on body composition. Finally, the blood flow restriction equipment may not be accessible for all. College students can choose MICT or HIIT according to their situations.
4.1. Practical applications
For the physically inactive population trying to improve their health status through aerobic exercise, HIIT was not recommended at the beginning due to high mechanical stress and possible cardiac problems. LICT-BFR is considered a safer alternative for its ability to improve CRF and body composition using relatively low intensity (57–63%HRmax). In addition, LICT-BFR elicited similar physiological responses and lower RPE compared with HIIT and MICT, making it a time-efficient method for participants to follow easily. This training method is also beneficial for active young adults31 and athletes.50 Considering the low-intensity characteristics, LICT-BFR can be performed to help individuals recover from their detraining period and get back to previous exercise routines without high injury risk.
5. Conclusion
In conclusion, all three exercise programs improved CRF in college students, with LICT-BFR considered the most time-efficient method. The LICT-BFR and HIIT groups showed greater absolute VO2max improvements than the MICT group, consistent with the previous hypothesis. In terms of relative VO2max, the LICT-BFR group has the most notable improvement, followed by the MICT and HIIT groups. This outcome can be explained by the changes in lean body mass and fat mass, showing weight loss for the MICT group and weight gain for other groups.
Funding/support statement
The authors thank all the participants volunteering in this study. This study was financed in part by the National Key R&D Program of China (2018YFC2000600).
Authorship
Category 1.
Conception and design of study: Chao Lan, acquisition of data: Chao Lan, Yujie Liu; analysis and/or interpretation of data: Chao Lan.
Category 2.
Drafting the manuscript: Chao Lan, Yujie Liu; revising the manuscript critically for important intellectual content: Chao Lan, Yujie Liu.
Category 3.
Approval of the version of the manuscript to be published (the names of all authors must be listed):Yan Wang∗, Chao Lan, Yujie Liu.
Declaration of competing interest
The authors declare no conflict of interest relevant to this article.
Acknowledgments
All persons who have made substantial contributions to the work reported in the manuscript (e.g., technical help, writing and editing assistance, general support), but who do not meet the criteria for authorship, are named in the Acknowledgments and have given us their written permission to be named. If we have not included an Acknowledgments in our manuscript, then that indicates that we have not received substantial contributions.
Contributor Information
Chao Lan, Email: 2019210434@bsu.edu.cn.
Yujie Liu, Email: 2020210447@bsu.edu.cn.
Yan Wang, Email: wyweiwei@126.com.
References
- 1.Xie M., Li H., Wang Z., et al. Cardiorespiratory fitness: a core component of health-related physical fitness—introduction to the aerobic center longitudinal study. J Beijing Sport Univ. 2011;34:1–7. 02. [In Chinese, English abstract] [Google Scholar]
- 2.Ross R., Blair S.N., Arena R., et al. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American heart association. Circulation. 2016;134(24):e653–e699. doi: 10.1161/CIR.0000000000000461. [DOI] [PubMed] [Google Scholar]
- 3.Raghuveer G., Hartz J., Lubans D.R., et al. Cardiorespiratory fitness in youth: an important marker of health: a scientific statement from the American heart association. Circulation. 2020;142(7) doi: 10.1161/CIR.0000000000000866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tomkinson G.R., Lang J.J., Tremblay M.S. Temporal trends in the cardiorespiratory fitness of children and adolescents representing 19 high-income and upper middle-income countries between 1981 and 2014. Br J Sports Med. 2019;53(8):478–486. doi: 10.1136/bjsports-2017-097982. [DOI] [PubMed] [Google Scholar]
- 5.Lamoureux N.R., Fitzgerald J.S., Norton K.I., et al. Temporal trends in the cardiorespiratory fitness of 2,525,827 adults between 1967 and 2016: a systematic review. Sports Med. 2019;49(1):41–55. doi: 10.1007/s40279-018-1017-y. [DOI] [PubMed] [Google Scholar]
- 6.Wei X., Meng X., Deng X., et al. Research of the current situation and promotion of college students' physique health[J] Sport Sci Tech. 2019;40:79–81. 06. [In Chinese, English abstract] [Google Scholar]
- 7.Gan X., Wen X., Lu Y., et al. Economic growth and cardiorespiratory fitness of children and adolescents in urban areas: a panel data analysis of 27 provinces in China, 1985–2014. Int J Environ Res Publ Health. 2019;16(19):3772. doi: 10.3390/ijerph16193772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Qin F., Song Y., Nassis G.P., et al. Physical activity, screen time, and emotional well-being during the 2019 novel coronavirus outbreak in China. Int J Environ Res Publ Health. 2020;17(14):5170. doi: 10.3390/ijerph17145170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ammar A., Brach M., Trabelsi K., et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 international online survey. Nutrients. 2020;12:1583. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huckins J.F., daSilva A.W., Wang W., et al. Mental health and behavior of college students during the early phases of the COVID-19 pandemic: longitudinal smartphone and ecological momentary assessment study. J Med Internet Res. 2020;22(6) doi: 10.2196/20185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bouchard C., An P., Rice T., et al. Familial aggregation of VO(2max) response to exercise training: results from the HERITAGE Family Study. J Appl Physiol. 1999;87(3):1003–1008. doi: 10.1152/jappl.1999.87.3.1003. [DOI] [PubMed] [Google Scholar]
- 12.Thompson W., Gordon N., Pescatello L. tenth ed. 2010. ACSM Guidelines for Exercise Testing and Prescription; pp. 9–15. Indiana: Indianapolis. [Google Scholar]
- 13.Garber C.E., Blissmer B., Deschenes M.R., et al. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 14.Moholdt T., Wisløff U., Lydersen S., et al. Current physical activity guidelines for health are insufficient to mitigate long-term weight gain: more data in the fitness versus fatness debate (The HUNT study, Norway) Br J Sports Med. 2014;48(20):1489–1496. doi: 10.1136/bjsports-2014-093416. [DOI] [PubMed] [Google Scholar]
- 15.Chen Y., Liu X., Yan N., et al. Higher academic stress was associated with increased risk of overweight and obesity among college students in China. Int J Environ Res Publ Health. 2020;17(15):5559. doi: 10.3390/ijerph17155559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deng Y., Hwang Y., Campbell S., et al. Institutional factors associated with college students' healthy physical activity and body composition: a first semester follow-up. J Am Coll Health. 2021:1–9. doi: 10.1080/07448481.2021.1922416. [DOI] [PubMed] [Google Scholar]
- 17.Chen C., Ye Y., Zhang Y., et al. Weight change across adulthood in relation to all cause and cause specific mortality: prospective cohort study. BMJ. 2019:l5584. doi: 10.1136/bmj.l5584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tchernof A., Després J.P. Pathophysiology of human visceral obesity: an update. Physiol Rev. 2013;93(1):359–404. doi: 10.1152/physrev.00033.2011. [DOI] [PubMed] [Google Scholar]
- 19.Lee D.H., Keum N., Hu F.B., et al. Predicted lean body mass, fat mass, and all cause and cause specific mortality in men: prospective US cohort study. BMJ. 2018:k2575. doi: 10.1136/bmj.k2575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Milanović Z., Sporiš G., Weston M. Effectiveness of high-intensity interval training (hit) and continuous endurance training for VO2max improvements: a systematic review and meta-analysis of controlled trials. Sports Med. 2015;45(10):1469–1481. doi: 10.1007/s40279-015-0365-0. [DOI] [PubMed] [Google Scholar]
- 21.Andreato L.V. High-intensity interval training: methodological considerations for interpreting results and conducting research. Trends Endocrinol Metabol. 2020;31(11):812–817. doi: 10.1016/j.tem.2020.08.003. [DOI] [PubMed] [Google Scholar]
- 22.da Cunha Nascimento D., Schoenfeld B.J., Prestes J. Potential implications of blood flow restriction exercise on vascular health: a brief review. Sports Med. 2020;50(1):73–81. doi: 10.1007/s40279-019-01196-5. [DOI] [PubMed] [Google Scholar]
- 23.Loenneke J.P., Wilson J.M., Marín P.J., et al. Low intensity blood flow restriction training: a meta-analysis. Eur J Appl Physiol. 2012;112(5):1849–1859. doi: 10.1007/s00421-011-2167-x. [DOI] [PubMed] [Google Scholar]
- 24.Amani-Shalamzari S., Rajabi S., Rajabi H., et al. Effects of blood flow restriction and exercise intensity on aerobic, anaerobic, and muscle strength adaptations in physically active collegiate women. Front Physiol. 2019;10:810. doi: 10.3389/fphys.2019.00810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karabulut M., Esparza B., Dowllah I.M., et al. The impact of low-intensity blood flow restriction endurance training on aerobic capacity, hemodynamics, and arterial stiffness. J Sports Med Phys Fit. 2021;61(7):877–884. doi: 10.23736/S0022-4707.20.11526-3. [DOI] [PubMed] [Google Scholar]
- 26.Takano H., Morita T., Iida H., et al. Hemodynamic and hormonal responses to a short-term low-intensity resistance exercise with the reduction of muscle blood flow. Eur J Appl Physiol. 2005;95(1):65–73. doi: 10.1007/s00421-005-1389-1. [DOI] [PubMed] [Google Scholar]
- 27.Howley E.T., Bassett D.R., Jr., Welch H.G. Criteria for maximal oxygen uptake: review and commentary. Med Sci Sports Exerc. 1995;27(9):1292–1301. [PubMed] [Google Scholar]
- 28.Helgerud J., Høydal K., Wang E., et al. Aerobic high-intensity intervals improve VO2max more than moderate training. Med Sci Sports Exerc. 2007;39(4):665–671. doi: 10.1249/mss.0b013e3180304570. [DOI] [PubMed] [Google Scholar]
- 29.Abe T., Fujita S., Nakajima T., et al. Effects of low-intensity cycle training with restricted leg blood flow on thigh muscle volume and VO2MAX in young men. J Sports Sci Med. 2010;9(3):452–458. [PMC free article] [PubMed] [Google Scholar]
- 30.Alves T.C., Santos A.P., Abdalla P.P., et al. Resistance training with blood flow restriction: impact on the muscle strength and body composition in people living with HIV/AIDS. Eur J Sport Sci. 2021;21(3):450–459. doi: 10.1080/17461391.2020.1757765. [DOI] [PubMed] [Google Scholar]
- 31.Kim D., Singh H., Loenneke J.P., et al. Comparative effects of vigorous-intensity and low-intensity blood flow restricted cycle training and detraining on muscle mass, strength, and aerobic capacity. J Strength Condit Res. 2016;30(5):1453–1461. doi: 10.1519/JSC.0000000000001218. [DOI] [PubMed] [Google Scholar]
- 32.Araújo J.P., Neto G.R., Silva J., et al. Does water aerobics with blood flow restriction change the body composition. J Exerc Physiol Online. 2015;18(6):25–31. [Google Scholar]
- 33.Wilcock I.M., Cronin J.B., Hing W.A. Physiological response to water immersion: a method for Sport recovery? Sports Med. 2006;36(9):747–765. doi: 10.2165/00007256-200636090-00003. [DOI] [PubMed] [Google Scholar]
- 34.Overend T.J., Paterson D.H., Cunningham D.A. The effect of interval and continuous training on the aerobic parameters. Can J Sport Sci. 1992;17(2):129–134. [PubMed] [Google Scholar]
- 35.Berger N.J., Tolfrey K., Williams A.G., et al. Influence of continuous and interval training on oxygen uptake on-kinetics. Med Sci Sports Exerc. 2006;38(3):504–512. doi: 10.1249/01.mss.0000191418.37709.81. [DOI] [PubMed] [Google Scholar]
- 36.Poole D.C., Gaesser G.A. Response of ventilatory and lactate thresholds to continuous and interval training. J Appl Physiol. 1985;58(4):1115–1121. doi: 10.1152/jappl.1985.58.4.1115. [DOI] [PubMed] [Google Scholar]
- 37.Esfandiari S., Sasson Z., Goodman J.M. Short-term high-intensity interval and continuous moderate-intensity training improve maximal aerobic power and diastolic filling during exercise. Eur J Appl Physiol. 2014;114(2):331–343. doi: 10.1007/s00421-013-2773-x. [DOI] [PubMed] [Google Scholar]
- 38.McKay B.R., Paterson D.H., Kowalchuk J.M. Effect of short-term high-intensity interval training vs. continuous training on O2 uptake kinetics, muscle deoxygenation, and exercise performance. J Appl Physiol. 2009;107(1):128–138. doi: 10.1152/japplphysiol.90828.2008. [DOI] [PubMed] [Google Scholar]
- 39.Gist N.H., Fedewa M.V., Dishman R.K., et al. Sprint interval training effects on aerobic capacity: a systematic review and meta-analysis. Sports Med. 2014;44(2):269–279. doi: 10.1007/s40279-013-0115-0. [DOI] [PubMed] [Google Scholar]
- 40.Costigan S.A., Eather N., Plotnikoff R.C., et al. High-intensity interval training for improving health-related fitness in adolescents: a systematic review and meta-analysis. Br J Sports Med. 2015;49(19):1253–1261. doi: 10.1136/bjsports-2014-094490. [DOI] [PubMed] [Google Scholar]
- 41.Cao M., Quan M., Zhuang J. Effect of high-intensity interval training versus moderate-intensity continuous training on cardiorespiratory fitness in children and adolescents: a meta-analysis. Int J Environ Res Publ Health. 2019;16(9):1533. doi: 10.3390/ijerph16091533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Andreato L.V., Esteves J.V., Coimbra D.R., et al. The influence of high-intensity interval training on anthropometric variables of adults with overweight or obesity: a systematic review and network meta-analysis. Obes Rev. 2019;20(1):142–155. doi: 10.1111/obr.12766. [DOI] [PubMed] [Google Scholar]
- 43.Maillard F., Pereira B., Boisseau N. Effect of high-intensity interval training on total, abdominal and visceral fat mass: a meta-analysis. Sports Med. 2018;48(2):269–288. doi: 10.1007/s40279-017-0807-y. [DOI] [PubMed] [Google Scholar]
- 44.Achten J., Gleeson M., Jeukendrup A.E. Determination of the exercise intensity that elicits maximal fat oxidation. Med Sci Sports Exerc. 2002;34(1):92–97. doi: 10.1097/00005768-200201000-00015. [DOI] [PubMed] [Google Scholar]
- 45.Scherr J., Wolfarth B., Christle J.W., et al. Associations between Borg's rating of perceived exertion and physiological measures of exercise intensity. Eur J Appl Physiol. 2013;113:147–155. doi: 10.1007/s00421-012-2421-x. [DOI] [PubMed] [Google Scholar]
- 46.Corrado D., Migliore F., Basso C., et al. Exercise and the risk of sudden cardiac death. Herz. 2006;31:553–558. doi: 10.1007/s00059-006-2885-8. [DOI] [PubMed] [Google Scholar]
- 47.Albert C.M., Mittleman M.A., Chae C.U., et al. Triggering of sudden death from cardiac causes by vigorous exertion. N Engl J Med. 2000;343(19):1355–1361. doi: 10.1056/NEJM200011093431902. [DOI] [PubMed] [Google Scholar]
- 48.Kessler H.S., Sisson S.B., Short K.R. The potential for high-intensity interval training to reduce cardiometabolic disease risk. Sports Med. 2012;42:489–509. doi: 10.2165/11630910-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 49.Loenneke J.P., Allen K.M., Mouser J.G., et al. Blood flow restriction in the upper and lower limbs is predicted by limb circumference and systolic blood pressure. Eur J Appl Physiol. 2015;115:397–405. doi: 10.1007/s00421-014-3030-7. [DOI] [PubMed] [Google Scholar]
- 50.Wortman R.J., Brown S.M., Savage-Elliott I., et al. Blood flow restriction training for athletes: a systematic review. Am J Sports Med. 2021;49(7):1938–1944. doi: 10.1177/0363546520964454. [DOI] [PubMed] [Google Scholar]