Abstract
Quadriceps femoris strength asymmetry at the time of return to sports participation after anterior cruciate ligament (ACL) reconstruction contributes to worse function and asymmetric landing patterns, but the impact on longitudinal outcomes is not known. This study determined if young athletes after ACL reconstruction with quadriceps femoris strength asymmetry at return to sports clearance would demonstrate markers of knee cartilage degeneration 5 years later compared to those with symmetric quadriceps femoris strength at return to sports. Participants (n=27) were enrolled at time of medical clearance for sports participation (baseline testing) and followed for 5 years. At baseline, quadriceps femoris strength was measured bilaterally and a limb symmetry index was used to divide the cohort into 2 groups: return to sport clearance with high quadriceps femoris strength (RTS-HQ; limb symmetry index≥90%) and return to sport clearance with low quadriceps femoris strength (RTS-LQ; limb symmetry index<85%). At 5 years post-baseline, quantitative magnetic resonance imaging (MRI) (T2 relaxation times (ms): involved knee medial/lateral femoral condyle and tibial plateau) data were collected. Group differences were evaluated with independent samples t-tests. At 5-years post-return to sports, the RTS-LQ strength group (n=14) demonstrated elevated T2 relaxation times at the anterior region of the lateral femoral condyle compared to the RTS-HQ strength group (n=13).
Key Terms: ACL reconstruction, MRI, quadriceps femoris, osteoarthritis
INTRODUCTION
Anterior cruciate ligament (ACL) injuries are a common and physically debilitating occurrence among athletes participating in cutting and pivoting sports.1 ACL reconstruction is often performed to restore ligamentous stability, reduce abnormal loading across joint surfaces, and facilitate return to physical activity and sports participation.1 However, outcomes for young, active individuals after ACL reconstruction are suboptimal, with persistent altered movement patterns2–5, a high incidence of second injury6–11, and reduced levels of physical activity12–14 and sports participation15 compared to peers.
A substantial portion of young athletes after ACL reconstruction have quadriceps femoris strength asymmetry that persist following rehabilitation and are present at the time of medical clearance for sports participation.2,4,16–18 These asymmetries present as deficits in the strength of the involved limb compared to the uninvolved limb. Quadriceps strength asymmetries in young indivdiuals after ACL reconstruction are significant as they contribute to reduced knee-related function, worse functional performance, and altered movement patterns2–4,16,18. Involved limb quadriceps femoris strength deficits of >15% (compared to the uninvolved side) present at the time of medical clearance for sports participation are associated with altered lower limb loading strategies during double-leg and single-leg landing activities, specifically reduced involved limb vertical ground reaction force, loading rate, and internal knee extension moments.2,4,18 Lower limb asymmetries in vertical ground reaction force and knee extension moments observed during landing at six months post-ACL reconstruction are associated with markers of tibiofemoral cartilage degeneration three years later.19 While quadriceps femoris strength asymmetries are associated with altered lower limb loading strategies, and altered lower limb loading is associated with markers of cartilage degeneration after ACL reconstruction; less is known about the impact of quadriceps femoris strength asymmetries that persist following post-operative rehabilitation directly on long-term knee cartilage integrity. Evaluation of quadriceps femoris strength is recommended to inform the decision for return to sports participation after ACL reconstruction; however, the recommended target criterion-value varies widely. Understanding the long-term impact of quadriceps strength deficits present at the time of return to sports is imperative in an effort to progress towards evidence-based criterion values to better inform return to sport decision-making.
ACL injury and quadriceps femoris weakness are associated with increased prevalence of knee osteoarthritis (OA). The odds of developing knee OA following ACL injury are approximately 4 times higher compared to the non-injured knee.20 Radiographic joint space narrowing has been directly linked with quadriceps femoris strength deficits after ACL reconstruction.21 While radiographic imaging and radiographic scoring systems (i.e. Kellgren-Lawrence scale22) have been traditionally used to quantify knee OA, these measures underestimate the severity of articular damage and fail to detect early, non-structural OA onset.23 This underestimation of disease onset and progression presents challenges in early detection of articular cartilage damage in young athletes after ACL reconstruction. The development of quantitative magnetic resonance imaging (MRI) techniques allow for earlier detection of articular cartilage degeneration through the evaluation of initial physiologic changes in the cartilage matrix. Elevated T1ρ and T2 relaxation times, indicative of compositional changes in the cartilage and early joint degeneration, have been identified within 5-years of return to activity/sports participation in young individuals after ACL reconstruction.24–28 Further, lower knee-related function reported at 2-years after return to sports participation was associated with elevated T1ρ and T2 relaxation times at 5-years after return to sports participation,29 indicating that there may be early markers of subsequent cartilage integrity in young, active individuals after ACL reconstruction. While quadriceps femoris weakness after ACL reconstruction is linked with subsequent long-term structural joint changes and morphological knee OA, further study is needed to understand if quadriceps femoris weakness is associated with quantitative measures of early cartilage matrix degeneration.
The purpose of this study was to investigate the impact of quadriceps femoris strength symmetry at the time of return to sports participation after ACL reconstruction on knee cartilage integrity 5 years later. The primary hypothesis tested was that young athletes following ACL reconstruction with quadriceps femoris strength asymmetry at return to sport would demonstrate elevated T2 relaxation times, indicative of compositional changes in the cartilage and early joint degeneration, in the medial femoral condyle at 5-years post-return to sports compared to those with more symmetrical strength at return to sports.
METHODS
Participants
A sub-cohort of individuals in the ACL REconstruction Long-term outcomes in Adolescents and Young adults (ACL-RELAY) Study were analyzed as part of this secondary analysis. The ACL-RELAY Study, a collaboration between Ohio State University and Cincinnati Children’s Hospital Medical Center, is an ongoing, prospective cohort study (Level of Evidence: 2) examining outcomes after ACL reconstruction, collecting injury, clinical, and biomechanical data beginning at the time of medical clearance for full sports participation. Participants in the ACL-RELAY Study are recruited from local orthopaedic practices and physical therapy clinics from the tri-state community surrounding Cincinnati, Ohio (USA) and enrolled at the time of medical return to sports clearance (baseline study visit) after primary, unilateral ACL reconstruction. To be enrolled, participants are 13–25 years old, required to have completed a formal rehabilitation program, have been cleared for return for participation in cutting, pivoting, jumping, or lateral motion sports by their respective orthopaedic surgeon and treating rehabilitation specialist, and whose goal is to return to cutting, pivoting, jumping, or lateral motion sport participation, either at a competitive or recreational level, at a regular basis of at least 50 hours/year. The ACL-RELAY Study controls neither the rehabilitation program nor the decision for clearance to participate in sports. Individuals with bone-patellar tendon-bone autograft, hamstring tendon autograft, or allograft are included; as well as, those with and without meniscus repair or partial meniscectomy at the time of ACL reconstruction. Individuals are excluded from participation if they have a history of: 1) low back pain or a lower extremity injury or surgery (besides the primary ACL injury) requiring the medical management by a physician within the past year or 2) a concomitant knee ligament injury (beyond grade 1 medial collateral ligament injury) in the involved limb.
A consecutive sub-cohort of participants in the ACL-RELAY Study were recruited between 2014–2017 to undergo morphologic and quantitative knee MRI scans at 5-years post-RTS to evaluate knee cartilage health.29 Potential participation in the 5-year testing session was offered sequentially based on the date of the baseline (time of medical clearance to return to sports participation) testing session. At the time of eligibility for 5-year testing, potential participants were contacted and screened. Exclusion from the current analysis included sustaining a second ACL injury, or other lower extremity injury requiring medical management, in either limb following baseline testing or a contraindication to MRI. Between the baseline testing session and 5 years later, 57 individuals were excluded (21 sustained a second ACL injury after baseline testing, 3 sustained another injury, 30 were lost to follow-up or were unable to participate (due to moving from the area), 2 declined participation, and 1 had contraindication to MRI). Participants were included in the current analysis if they completed ACL-RELAY Study baseline testing (at time of return to sports) and knee MRI scans 5 years later.
The study protocol was approved by the Institutional Review Board of Cincinnati Children’s Hospital Medical Center, and all participants and guardians, when required, provided written, informed consent/assent.
Baseline Testing Session: Group Classification
Baseline study testing occurred within 4 weeks of medical clearance for full sports participation and included the collection of measures as previously reported.2,4,16 For this analysis, only data from the quadriceps femoris strength assessment were used. Quadriceps femoris strength was assessed using an electromechanical dynamometer (Biodex Medical Systems, Inc., Shirley, NY) during a maximal volitional isometric contraction (60o of knee flexion).2,4,16 Participants were securely positioned with the trunk supported, the hips flexed to approximately 90°, the knee joint aligned with the dynamometer axis, and the dynamometer resistance pad at the anterior aspect of the distal shank. Real-time visual feedback and verbal encouragement was provided to encourage maximum effort trials. Three maximum-effort trials were recorded for each knee (5 seconds in duration, separated by 15 seconds of rest). The average of the peak torque of the test trials from each limb was used to calculate limb symmetry index (ratio of the performance of the involved and uninvolved limbs x 100%), with a limb symmetry index<100% indicating involved limb strength deficits. At the time of analysis, the quadriceps femoris limb symmetry index was used to classify participants into strength groups: return to sport participation with high quadriceps (RTS-HQ, LSI≥90%) strength and return to sports with low quadriceps (RTS-LQ, LSI<85%) strength, based on previous work.2,16–18,30 There were no participants with quadriceps femoris limb symmetry index values between 85% and 89%.
5-Year Testing Session
The same participants returned for a 5-year post-return to sports (± 6 months) testing session. In addition to demographic data, activity level was assessed with the Marx Activity Rating Scale that uses 4 questions to evaluate the frequency and intensity of an individual’s “most active state in the past year.”31 It is scored on a 0–16 point scale, with 16 indicating the most active in cutting and pivoting-related activities. Quadriceps femoris strength data were collected with the same methods as the baseline testing session and MRI data were also collected.
Morphologic and Quantitative Knee MRI
MRI imaging was performed on the involved knee using a 3-T scanner (GE Healthcare) with an eight-channel receive-only coil using methods previously reported.29 Morphological sequences were performed to calculate a Whole-Organ Magnetic Resonance Imaging Score (WORMS)32 for the knee. To calculate a WORMS, a turbo spin-echo intermediate-weighted and fat-suppressed sequence (echo time 40 ms; repetition time 3000 ms; echo train length 12; field of view 14 cm; matrix size 312 × 234 cm; slice thickness 3 mm), proton density turbo spin-echo sequence (echo time 20 ms; repetition time 3000 ms; echo train length 9; field of view 14 cm; matrix size 400 × 390 cm; slice thickness 3 mm), and a 3D isotropic proton density turbo spin-echo sequence (echo time set a minimum; repetition time 1000 ms; echo train length 65; field of view 14 cm; matrix size 280 × 320 cm; slice thickness 0.5 mm) were performed in the sagittal plane. Post-processing of the 3D isotropic sequence allowed for generation of axial and coronal plane images.
Quantitative measures of cartilage composition were evaluated with T2 map sequences performed with a 3D fast spin-echo sequence (slice thickness of 3mm, repetition time of 1315–1431 ms, flip angle of 90°, matrix size of 320 × 200–256 cm, and variable echo times of 6.5/13.4/27.0/40.7 ms). Five participants had only 2D T2 map sequences (slice thickness of 4 mm, repetition time of 800 ms, matrix size 256 × 192 cm, and eight echo times of 6.9/13.9/20.9/27.9/34.9/41.9/55.8 ms).
Involved knee morphological changes were evaluated with the WORMS, a multi-feature measure of degenerative joint changes within the cartilage and subchondral bone of the medial and lateral femoral condyles , medial and lateral tibial plateaus, patella, and trochlea. In addition to cartilage integrity, additional features evaluated by the WORMS include: meniscal integrity, collateral and cruciate ligament integrity, synovitis, effusion, loose bodies, cysts, and bursitis. WORMS has a maximum score of 332, with a higher score indicating more degenerative features. All WORMS evaluations were performed by a senior musculoskeletal radiologist (AMZ) and a cumulative score was calculated for each participant.
T2 mapping images were constructed in four compartments: medial femoral condyle, lateral femoral condyle, medial tibial plateau, and lateral tibial plateau. For regional analysis, the cartilage in the medial/lateral femur and medial/lateral tibia were subdivided based on the spatial relationship to the meniscal horns (FIGURE 129).24,26 The anterior regions were identified above and below the anterior horn of the meniscus for the medial/lateral condyles and medial/lateral plateaus, respectively. The posterior regions were identified above and below the posterior horn of the meniscus for the medial/lateral condyles and medial/lateral plateaus, respectively. The middle regions were between the anterior and posterior horns of the meniscus for the medial/lateral condyles and medial/lateral plateaus, respectively. Custom-written software24,29 (MATLAB; Mathworks, Natlick, MA) calculated mean T2 relaxation times (ms) in each region of interest for the full-thickness cartilage, as well as two equally spaced layers (superficial layer and deep layer), with higher values indicating early cartilage degeneration and cartilage disorganization).25,33 Each region of interest was measured by the same author (MPI), confirmed by a senior musculoskeletal radiologist (AMZ), and performed with high between-day reliability (ICC 3,1 > 0.96 for all T2 mapping procedures for all full-thickness, superficial, and deep ROI) and blinded to quadriceps femoris strength group classification.
Figure 1. Representative 3D fast spin-echo image showing subcompartment definition for the lateral femoral condyle and tibia plateau.
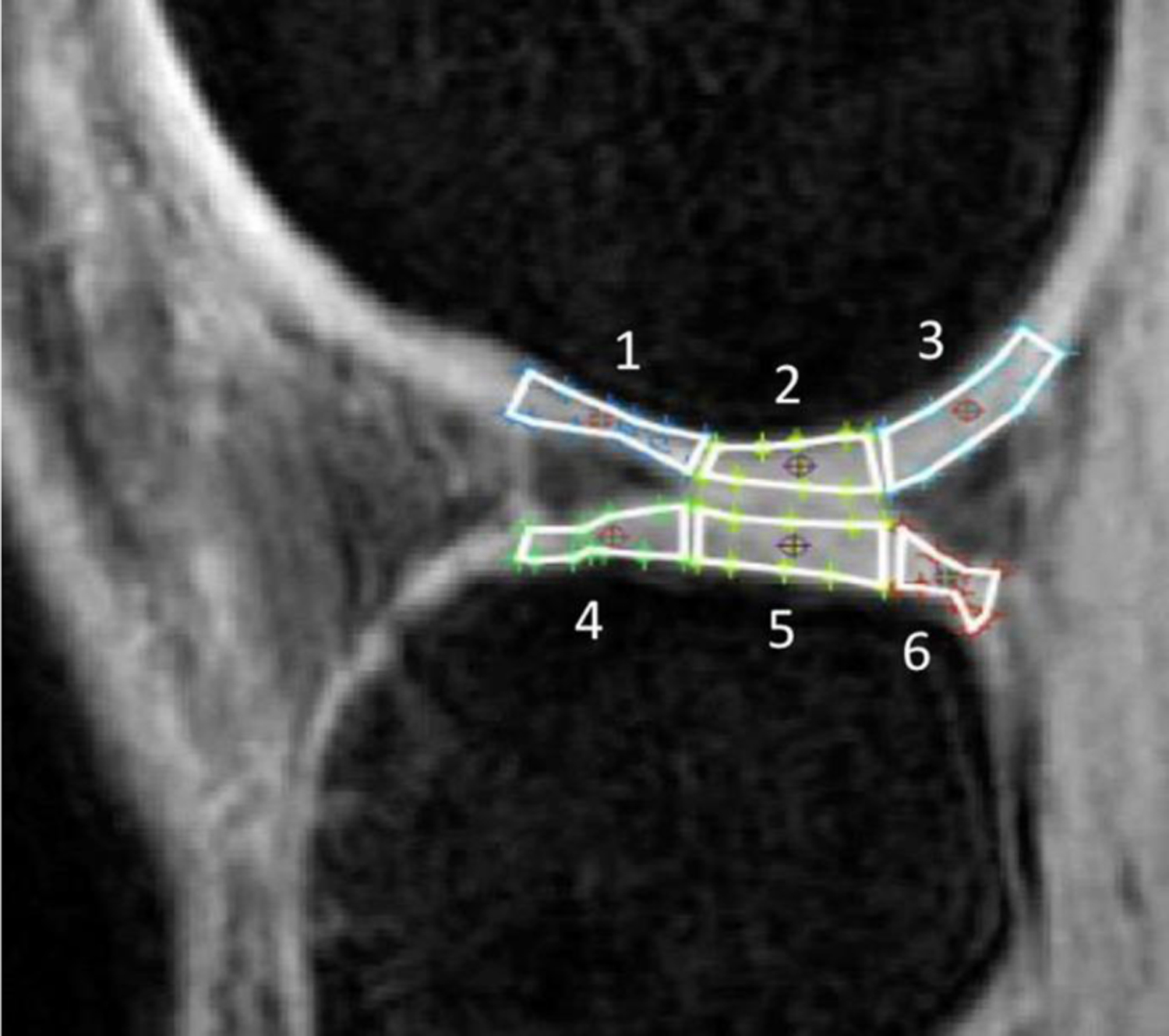
The anterior regions (1, 4) are regions above and below the anterior horn of the meniscus, respectively; the posterior regions (3, 6) are regions above and below the posterior horn of the meniscus, respectively; the middle regions (2, 5) are between the anterior and posterior horns of the meniscus, respectively. 1, anterior femoral condyle; 2, middle femoral condyle; 3, posterior femoral condyle; 4, anterior tibial plateau; 5, middle tibial plateau; 6, posterior tibial plateau. Image with permission.29
Statistical Analysis
Statistical analyses were performed using SPSS (v21.0; IBM SPSS Statistics). Descriptive analyses of demographic data consisted of calculating frequencies and percentages for categorical data and means and standard deviations for continuous data. Categorical and continuous demographic variables were compared between the quadriceps femoris strength groups with Pearson Chi-Square tests and independent samples t-test, respectively (p<0.05). MRI variables of interest (5-year WORMS score and T2 relaxation times in the anterior, middle, and posterior regions of the medial/lateral femoral condyle and medial/latera tibial plateau, respectively were compared between the RTS-HQ strength and RTS-LQ strength groups with independent samples t-tests. Holm-corrected p values were used to interpret MRI findings to account for multiple comparisons.34
RESULTS
Participant and Group Demographics
A total of 27 young athletes met inclusion for this analysis, with 13 (48%) being classified in the RTS-HQ group and 14 (52%) being classified in the RTS-LQ group (TABLE 1). At the time of return to sports, the cohort was an average age of 16.8 years and 82% female. The RTS-HQ and RTS-LQ groups did not differ in terms of age, sex distribution, graft type distribution, presence of concomitant meniscus injury, or time from ACL reconstruction to return to sports clearance (TABLE 1) (p>0.05). As expected based on a-priori group classification, the RTS-HQ group had higher quadriceps femoris strength limb symmetry index at return to sports compared to the RTS-LQ group (TABLE 1) (p<0.001). At 5-years later, the RTS-HQ and RTS-LQ groups did not differ in terms of age, time from return to sports to 5-year testing, or 5-year quadriceps femoris strength limb symmetry index (TABLE 1) (p>0.05).
TABLE 1.
Demographics between quadriceps strength groups
| Variable | Cohort | RTS-HQ | RTS-LQ | P-value | |
|---|---|---|---|---|---|
| n | 27 | 13 (48%) | 14 (52%) | - | |
| Biologic sexa, n (% female) | 22 (82%) | 9 (69%) | 13 (93%) | 0.11 | |
| Graft Typea, n (%) | AL: 2 (7%) HS: 18 (67%) PT: 7 (26%) |
AL: 1 (8%) HS: 11 (85%) PT: 1 (8%) |
AL: 1 (7%) HS: 7 (50%) PT: 6 (43%) |
0.11 | |
| Meniscus Injurya, n (%) | 13 (48%) | 7 (54%) | 6 (43%) | 0.57 | |
| At RTS b | Age (years) | 16.8 ± 2.3 | 16.7±3.0 | 16.9±1.6 | 0.79 |
| Months from surgery to RTS | 7.7 ± 2.3 | 8.4±2.9 | 7.1 ± 1.4 | 0.15 | |
| QF LSI (%) | 87.9 ± 17.7 | 102.1 ± 12.2 | 74.6 ± 10.1 | <0.001 | |
| At 5-year b | Age (years) | 22.0 ± 2.5 | 21.8±2.8 | 22.2±2.2 | 0.77 |
| Months from RTS to 5-year | 59.1 ± 6.6 | 59.6 ± 7.1 | 58.7 ± 6.3 | 0.73 | |
| QF LSI (%) | 97.7 ± 11.2 | 96.3 ± 7.2 | 99.0 ± 14.1 | 0.59 | |
|
Marx Activity Rating Scale
(0–16, most active) |
10.5 ± 4.3 | 10.1 ± 3.5 | 10.9 ± 4.9 | 0.65 |
AL, allograft; HS, hamstring autograft; PT= patellar tendon-bone-tendon autograft; RTS, at the time of return to sport; QF LSI, quadriceps femoris limb symmetry index (0–100%, <100% indicates deficit on the involved limb)
Compared with Pearson Chi-Square test
Data reported as mean ± standard deviation
MRI
At 5-years post-return to sports, the WORMS did not differ between the RTS-HQ strength and RTS-LQ strength groups (8.1 ± 5.9 vs. 13.6 ± 15.6; p=0.24; respectively). For full-thickness cartilage T2 mapping at 5-years , the involved limb of the RTS-LQ strength group had higher relaxation times, indicative of early joint degeneration, compared to the RTS-HQ strength group at the anterior lateral femoral condyle (TABLE 2) (p=0.054, strong trend with Holm’s correction). For superficial and deep layer cartilage T2 mapping at 5-year post-return to sports, the RTS-LQ strength group had higher relaxation times than the RTS-HQ strength group at the superficial (p=0.007) and deep (p=0.008) layers of the anterior lateral femoral condyle (TABLE 3). There was also a strong statistical trend toward the RTS-HQ strength group having higher T2 relaxation times at the superficial cartilage layer at the posterior medial femoral condyle (TABLE 4) (p=0.055).
TABLE 2.
Involved limb comparisons of full-thickness T2 relaxation timesa between groups
| RTS-HQ (n=14) |
RTS-LQ (n=13) |
p-value | Effect size (Cohen’s D) | 95% CI, [lower, upper bound] |
||
|---|---|---|---|---|---|---|
| LFC | Anterior | 33.3 ± 4.4 | 37.5 ± 5.9 | 0.054† | 0.80 | [−0.07, 8.52] |
| Middle | 34.9 ± 5.4 | 35.3 ± 5.4 | 0.85 | 0.07 | [−3.80, 4.60] | |
| Posterior | 37.8 ± 4.1 | 35.9 ± 4.0 | 0.25 | −0.45 | [−5.08, 1.38] | |
|
| ||||||
| LTP | Anterior | 32.3 ± 6.3 | 29.7 ± 4.8 | 0.24 | −0.48 | [−7.13, 1.86] |
| Middle | 28.9 ± 2.7 | 26.9 ± 3.2 | 0.11 | −0.66 | [−4.39, 0.45] | |
| Posterior | 36.5 ± 4.6 | 36.7 ± 5.9 | 0.94 | 0.03 | [−4.07, 4.37] | |
|
| ||||||
| MFC | Anterior | 35.4 ± 6.4 | 34.9 ± 6.8 | 0.85 | −0.07 | [−5.76, 4.77] |
| Middle | 34.5 ± 9.9 | 33.3 ± 6.0 | 0.72 | −0.15 | [−7.87, 5.51] | |
| Posterior | 36.4 ± 4.0 | 33.4 ± 3.7 | 0.06 | −0.77 | [−6.51, 0.13] | |
|
| ||||||
| MTP | Anterior | 41.0 ± 12.0 | 35.8 ± 8.5 | 0.21 | −0.49 | [−13.31, 3.06] |
| Middle | 36.8 ± 6.0 | 34.4 ± 5.9 | 0.33 | −0.39 | [−7.25, 2.57] | |
| Posterior | 33.7 ± 4.5 | 36.2 ± 7.0 | 0.30 | 0.42 | [−2.29, 7.24] | |
LFC, lateral femoral condyle; LTP, lateral tibial plateau; MFC, medial femoral condyle; MTP, medial tibial plateau
All values are in milliseconds (mean ± standard deviation)
Indicates trend with Holm-corrected p value
TABLE 3.
Involved limb comparisons of superficial and deep layer T2 relaxation times between groups
| RTS-HQ (n=14) |
RTS-LQ (n=13) |
p-value | Effect size (Cohen’s D) | 95% CI, [lower, upper bound] |
||
|---|---|---|---|---|---|---|
| Superficial Anterior | 34.3 ± 4.9 | 40.0 ± 5.2 | 0.007* | 1.1 | 1.68, 9.71 | |
| Deep Anterior | 29.6 ± 5.4 | 35.9 ± 5.8 | 0.008* | 1.1 | 1.78, 10.89 | |
| LFC | Superficial Middle | 38.5 ± 5.8 | 37.8 ± 5.9 | 0.77 | −0.12 | −5.31, 3.96 |
| Deep Middle | 30.8 ± 5.6 | 30.7 ± 5.4 | 0.97 | −0.02 | −4.46, 4.28 | |
| Superficial Posterior | 41.1 ± 4.9 | 38.6 ± 4.9 | 0.20 | −0.51 | −6.41, 1.38 | |
| Deep Posterior | 35.1 ± 4.4 | 33.0 ± 4.2 | 0.21 | −0.50 | −5.53, 1.27 | |
|
| ||||||
| Superficial Anterior | 37.1 ± 6.4 | 33.5 ± 3.6 | 0.08 | −0.71 | −7.74, 0.53 | |
| Deep Anterior | 28.7 ± 6.0 | 25.3 ± 6.7 | 0.19 | −0.53 | −8.67, 1.79 | |
| LTP | Superficial Middle | 31.7 ± 2.5 | 32.1 ± 2.6 | 0.68 | 0.16 | −1.65, 2.48 |
| Deep Middle | 25.0 ± 2.7 | 24.0 ± 4.7 | 0.53 | −0.25 | −4.15, 2.18 | |
| Superficial Posterior | 38.4 ± 6.1 | 38.6 ± 6.8 | 0.91 | 0.04 | −4.86, 5.42 | |
| Deep Posterior | 34.5 ± 4.9 | 34.6 ± 6.6 | 0.97 | 0.02 | −4.52, 4.71 | |
|
| ||||||
| Superficial Anterior | 37.4 ± 9.0 | 38.9 ± 12.5 | 0.73 | 0.14 | −7.18, 10.18 | |
| Deep Anterior | 32.0 ± 6.2 | 32.9 ± 6.1 | 0.71 | 0.15 | −4.16, 6.02 | |
| MFC | Superficial Middle | 39.4 ± 11.5 | 39.0 ± 7.6 | 0.91 | −0.05 | −8.70, 7.78 |
| Deep Middle | 27.8 ± 5.6 | 27.8 ± 4.4 | 0.99 | 0.00 | −4.24, 4.26 | |
| Superficial Posterior | 39.0 ± 5.5 | 35.1 ± 4.5 | 0.055† | −0.79 | −8.01, 0.10 | |
| Deep Posterior | 32.4 ± 5.6 | 28.6 ± 5.0 | 0.09 | −0.69 | −8.02, 0.61 | |
|
| ||||||
| Superficial Anterior | 47.1 ± 18.1 | 38.3 ± 11.1 | 0.14 | −0.59 | −20.58, 3.07 | |
| Deep Anterior | 33.9 ± 7.0 | 35.3 ± 10.4 | 0.67 | 0.17 | −5.60, 8.53 | |
| MTP | Superficial Middle | 48.6 ± 16.2 | 41.5 ± 7.7 | 0.17 | −0.56 | −17.41, 3.31 |
| Deep Middle | 31.7 ± 5.5 | 31.6 ± 7.1 | 0.97 | −0.02 | −5.42, 5.19 | |
| Superficial Posterior | 34.8 ± 4.2 | 37.1 ± 7.4 | 0.35 | 0.38 | −2.62, 7.18 | |
| Deep Posterior | 32.0 ± 5.3 | 35.2 ± 6.9 | 0.19 | 0.52 | −1.76, 8.20 | |
LFC, lateral femoral condyle; LTP, lateral tibial plateau; MFC, medial femoral condyle; MTP, medial tibial plateau
All values are in milliseconds (mean ± standard deviation)
Indicates Holm-corrected p value <0.05;
Indicates trend
DISCUSSION
The purpose of this study was to investigate the impact of quadriceps femoris strength symmetry at the time of medical clearance for sports participation after ACL reconstruction on knee cartilage integrity 5 years later. We hypothesized that young athletes following ACL reconstruction who were cleared for sports participation with quadriceps femoris strength asymmetry would demonstrate elevated T2 relaxation times in the medial femoral condyle 5-years later compared to those with symmetrical quadriceps femoris strength at return to sports. Elevated T2 relaxation times, indicative of early cartilage matrix degeneration, were observed in the reconstructed knees of young athletes 5 years after clearance for high-level sports participation. The most important finding of the present study was that young individuals who are cleared for sports participation with quadriceps femoris strength deficits in the involved limb demonstrated elevated T2 relaxation times in the involved knee 5 years later compared to individuals who are cleared for sports participation with greater quadriceps femoris strength symmetry. These differences were identified primarily in the lateral compartment of the knee.
For a substantial portion of young individuals after ACL reconstruction, quadriceps femoris strength deficits persist even after completion of post-operative rehabilitation.16–18 Young athletes who are cleared for sports participation with quadriceps femoris strength asymmetry report lower knee-related function, and demonstrate worse functional performance and altered joint loading strategies early after rehabilitation discharge following ACLR.2,4,16,18,35 Quadriceps femoris strength may be an important modifiable component of rehabilitation to identify young individuals after ACL reconstruction at risk for deleterious changes in cartilage matrix composition within 5 years of return to sports participation. Increases in cartilage T2 relaxation times, as observed in this study in the RTS-LQ strength group, are markers of increased water content and disorganization of the collagen matrix.36–38 These composition changes precede radiographic joint changes and are indicative of early-stage OA.39,40 The findings from this study highlight the importance of achieving nearly symmetric (limb symmetry index ≥ 90%) quadriceps femoris strength in young individuals prior to clearance for sports participation to potentially protect against subsequent adverse changes in articular cartilage composition.
In the current analysis, nearly 50% of the young cohort was cleared to return to high-level sports participation with quadriceps femoris strength symmetry below the recommended return to sports criterion cutoff (quadriceps femoris limb symmetry index ≥ 90%16–18). This is in line with previous work in young athletes indicating that between 20% and 40% achieve the recommended level of quadriceps femoris strength symmetry at the time of clearance for sports participation.16–18 This analysis shows that the asymmetries in quadriceps femoris strength at return to sport, which were used to classify participants, had resolved by the 5-year testing session as both quadriceps femoris strength groups demonstrated an average quadriceps strength limb symmetry index > 95% (TABLE 1). The focus on quadriceps femoris strength symmetry in this analysis did not allow for the evaluation of strength changes that may have occurred in both the reconstructed and/or uninvolved limbs over time. Further study of changes over time in individual limb quadriceps strength values is warranted to further inform interpretation of this finding.
Despite resolution of between-limb quadriceps femoris strength asymmetries over the 5-year study period, young athletes who are cleared for sports participation with quadriceps femoris strength asymmetries demonstrated quantitative MRI markers of cartilage matrix degeneration 5 years later. In line with our findings, previous studies report associations between quadriceps femoris weakness and joint degeneration following ACL reconstruction. Arhos and colleagues41 demonstrated an association between more symmetrical quadriceps femoris strength and lower odds of clinical knee OA within 5 years of ACL injury or reconstruction. Between 2 and 4 years post-ACL reconstruction, poorer quadriceps femoris strength was associated with more severe patellofemoral cartilage damage during a second-look arthroscopy.42 In the tibiofemoral joint, quadriceps femoris weakness at 6 months after ACL reconstruction was linked to elevated T1ρ relaxation times in the medial femoral condyle at the same time-point.43 Quadriceps femoris weakness is associated with altered lower limb and knee loading strategies relatively early after ACL reconstruction during gait44,45 and more demanding landing activities,2–4,16,18 particularly during the weight acceptance and limb loading portion of the tasks where eccentric muscle action is required. Longitudinal analysis indicates that quadriceps strength asymmetries, present at the time of return to sport clearance, are linked to asymmetric vertical ground reaction force and loading rate landing patterns 2 years later.46 Quadriceps femoris weakness may interfere with normal lower limb and knee loading strategies in a manner that shifts joint loads to areas of cartilage that are unable to effectively accommodate the increase or decrease in load.47–49
To our knowledge, the current analysis represents one of the first to report the longitudinal association between quadriceps femoris strength symmetry at the time of medical clearance for sports participation and subsequent cartilage matrix degeneration using quantitative MRI measures 5 years later. Previous studies after ACL reconstruction reported quantitative cartilage matrix changes in both the medial27,29,43 and lateral27,50 compartments of the tibiofemoral joint. Previous work in the current cohort found that 2-year post-return to sport knee-related function measures were associated with elevated T1ρ and T2 relaxation times between limbs, mostly in the medial compartment.29 The current study focused on T2 relaxation times with values compared between quadriceps femoris strength groups, rather than comparisons between limbs which may contribute to the finding of adverse compositional changes primarily in the lateral compartment in this analysis. This finding is in line with prospective, longitudinal work in individuals with ACL injury and reconstruction reporting most severe initial chondral injuries in the lateral compartment, with progressive elevation of T2 values in the lateral femoral compartment for up to 11 years post-ACL injury.50 The area of elevated T2 relaxation times observed in the RTS-LQ strength group, the anterior portion of the lateral femoral condyle, is the location of the pivot shift and bone bruises associated with ACL injury.51,52 While it was beyond the scope of the current analysis to evaluate the potential impact of concomitant bone bruise location or ACL injury mechanism on these findings, future research in this area is warranted.
Limitations
The findings of the current analysis indicate that achieving nearly symmetric (limb symmetry index ≥ 90%) quadriceps femoris strength prior to release to high-level activity may lessen the risk of future quantitative makers of early cartilage degeneration. However, there are several limitations to consider in the interpretation of these findings. First, this preliminary look into the longitudinal association of quadriceps femoris strength, at the meaningful time-point of return to sports clearance, and subsequent cartilage matrix degeneration 5 years later includes a small sample size with an average age of approximately 17 years old, both of which limit the generalizability of the results. A young, active cohort was specifically included in this study due to the prevalence of ACL injury within this demographic. Second, there are several potential confounding factors that were not considered in the current analysis. Levels of physical activity or sports participation over the time course of the study were not considered, and differences in the volume of high-impact activity between time points could have influenced MRI findings. However, the Marx Activity Rating Scale was no different between the groups at the 5-year testing session. The potential impact of concomitant injuries, such as meniscus injury or bone bruises at the time of ACL injury, on MRI findings were not considered in the current analysis. However, the proportion of concomitant meniscus injuries was similar between the groups. Graft type was also not considered as a confounding factor in this analysis. Future analyses with larger sample sizes would be informative and would allow for the consideration of potential confounding factors, such as concomitant injuries, that are known risk factors for knee cartilage degeneration.25,26 Third, there are several considerations with the study design and analysis, including no analysis of change over time, no comparison to an uninjured group, mixed imaging protocols and slice selection, and the potential for magic angle effects, that may impact the interpretation of findings. It is possible that the analysis of changes in individual limb quadriceps femoris strength over time and the potential impact on subsequent joint loading strategies would allow for additional insight. The inclusion of an injured control group may offer additional insights into interpretation of the findings between groups with regard to what might be considered typical cartilage composition for young individuals. The mixed imaging protocols were split between the groups (3 in the RTS-HQ strength group, 2 in the RTS-LQ strength group), but may have impacted our findings. The curved articular surface of the femoral condyle is susceptible to artifact from the magic angle effect, resulting in a longer T2 relaxation time. The femoral condyle regions of interest in this study are less susceptible to the magic angle effect,53 but this should be considered in interpreting these findings.
Conclusions
Markers of knee cartilage degeneration were observed in young athletes 5 years post-return to sports after ACL reconstruction. Specifically, young athletes who are cleared for sports participation with quadriceps femoris strength asymmetry demonstrated elevated knee cartilage T2 relaxation times, indicative of cartilage matrix degeneration, 5 years later compared to those with more symmetric quadriceps femoris strength. While this early analysis indicates that achieving quadriceps femoris strength symmetry ≥ 90% prior to the release to sports may mitigate future degenerative changes in the knee cartilage matrix, future research is warranted. Additional study with larger sample sizes and with consideration of potentially confounding factors will offer additional insight into the potential impact of early quadriceps femoris strength deficits on subsequent cartilage integrity.
Clinical Significance:
Just over 50% of this cohort was cleared for sports participation with involved limb quadriceps femoris strength deficits that may contribute to early markers of knee cartilage degeneration within the subsequent 5 years.
ACKNOWLEDGEMENTS
Funding Source(s): This work was funded by support from the National Institutes of Health grant R21-AR064923 and F32-AR055844, the National Football League Charities Medical Research Grants, and the APTA Sports Section Legacy Grant.
Footnotes
Institutional Review Board: This study was approved by the Cincinnati Children’s Hospital Intuitional Review Board (approval #: 2008–0514)
Public Trials Registry: N/A
Financial Disclosures: There are no disclosures.
REFERENCES
- 1.Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols CE. Treatment of anterior cruciate ligament injuries, part I. Am J Sports Med. 2005;33(10):1579–1602. [DOI] [PubMed] [Google Scholar]
- 2.Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE. Strength asymmetry and landing mechanics at return to sport after anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2015;47(7):1426–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ithurburn MP, Altenburger AR, Thomas S, Hewett TE, Paterno MV, Schmitt LC Young athletes after ACL reconstruction with quadriceps strength asymmetry at the time of return-to-sport demonstrate decreased knee function 1 year later. Knee Surgery, Sport Traumatol Arthrosc. 2018;26(2):426–433. [DOI] [PubMed] [Google Scholar]
- 4.Ithurburn MP, Paterno MV, Ford KR, Hewett TE, Schmitt LC. Young Athletes With Quadriceps Femoris Strength Asymmetry at Return to Sport After Anterior Cruciate Ligament Reconstruction Demonstrate Asymmetric Single-Leg Drop-Landing Mechanics. Am J Sports Med. 2015;43(11):2727–2737. [DOI] [PubMed] [Google Scholar]
- 5.Ithurburn MP, Paterno MV, Ford KR, Hewett TE, Schmitt LC. Young Athletes after Anterior Cruciate Ligament Reconstruction with Single-Leg Landing Asymmetries at the Time of Return to Sport Demonstrate Decreased Knee Function 2 Years Later. Am J Sports Med. 2017;45(11):2604–2613. [DOI] [PubMed] [Google Scholar]
- 6.Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of Secondary Injury in Younger Athletes after Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2016;44(7):1861–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paterno MV, Huang B, Thomas S, Hewett TE, Schmitt LC. Clinical Factors That Predict a Second ACL Injury After ACL Reconstruction and Return to Sport: Preliminary Development of a Clinical Decision Algorithm. Orthop J Sport Med. 2017;5(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kamath GV, Murphy T, Creighton RA, Viradia N, Taft TN, Spang JT. Anterior cruciate ligament injury, return to play, and reinjury in the elite collegiate athlete: Analysis of an NCAA Division i cohort. Am J Sports Med. 2014;42(7):1638–1643. [DOI] [PubMed] [Google Scholar]
- 10.Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: Not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946–951. [DOI] [PubMed] [Google Scholar]
- 11.Dekker TJ, Godin JA, Dale KM, Garrett WE, Taylor DC, Riboh JC. Return to sport after pediatric anterior cruciate ligament reconstruction and its effect on subsequent anterior cruciate ligament injury. J Bone Jt Surg - Am Vol. 2017;99(11):897–904. [DOI] [PubMed] [Google Scholar]
- 12.Bell DR, Pfeiffer KA, Cadmus-Bertram LA, et al. Objectively measured physical activity in patients after anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(8):1893–1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dunn WR, Spindler KP. Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR): A multicenter orthopaedic outcomes network (MOON) ACLR cohort study. Am J Sports Med. 2010;38(10):2040–2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spindler KP, Parker RD, Andrish JT, et al. Prognosis and predictors of ACL reconstructions using the MOON cohort: A model for comparative effectiveness studies. J Orthop Res. 2013;31(1):2–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Webster KE, Feller JA. Expectations for Return to Preinjury Sport Before and After Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2019;47(3):578–583. [DOI] [PubMed] [Google Scholar]
- 16.Schmitt LC, Paterno MV, Hewett TE. The Impact of Quadriceps Femoris Strength Asymmetry on Functional Performance at Return to Sport Following Anterior Cruciate Ligament Reconstruction. J Orthop Sport Phys Ther. 2012;42(9):750–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Toole AR, Ithurburn MP, Rauh MJ, Hewett TE, Paterno MV., Schmitt LC. Young Athletes After Anterior Cruciate Ligament Reconstruction Cleared for Sports Participation: How Many Actually Meet Recommended Return-to-Sport Criteria Cutoffs? J Orthop Sport Phys Ther. 2017;47(11):1–27. [DOI] [PubMed] [Google Scholar]
- 18.Palmieri-Smith RM, Lepley LK. Quadriceps Strength Asymmetry After Anterior Cruciate Ligament Reconstruction Alters Knee Joint Biomechanics and Functional Performance at Time of Return to Activity. Am J Sports Med. 2015;43(7):1662–1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shimizu T, Samaan MA, Tanaka MS, et al. Abnormal Biomechanics at 6 Months Are Associated With Cartilage Degeneration at 3 Years After Anterior Cruciate Ligament Reconstruction. Arthrosc - J Arthrosc Relat Surg. 2019;35(2):511–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Poulsen E, Goncalves GH, Bricca A, Roos EM, Thorlund JB, Juhl CB. Knee osteoarthritis risk is increased 4–6 fold after knee injury-a systematic review and meta-analysis. Br J Sports Med. 2019;53(23):1454–1463. [DOI] [PubMed] [Google Scholar]
- 21.Tourville TW, Jarrell KM, Naud S, Slauterbeck JR, Johnson RJ, Beynnon BD. Relationship between isokinetic strength and tibiofemoral joint space width changes after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(2):302–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schiphof D, Boers M, Bierma-Zeinstra SMA. Differences in descriptions of Kellgren and Lawrence grades of knee osteoarthritis. Ann Rheum Dis. 2008;67(7):1034–1036. [DOI] [PubMed] [Google Scholar]
- 23.Abdelaziz H, Balde OM, Citak M, Gehrke T, Magan A, Haasper C. Kellgren–Lawrence scoring system underestimates cartilage damage when indicating TKA: preoperative radiograph versus intraoperative photograph. Arch Orthop Trauma Surg. 2019;139(9):1287–1292. [DOI] [PubMed] [Google Scholar]
- 24.Li X, Kuo D, Theologis A, et al. Cartilage in Anterior Cruciate Ligament–Reconstructed Knees: MR Imaging T1 ρ and T2—Initial Experience with 1-year Follow-up. Radiology. 2011;258(2):505–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Su F, Hilton JF, Nardo L, et al. Cartilage morphology and T1ρ and T2 quantification in ACL-reconstructed knees: A 2-year follow-up. Osteoarthr Cartil. 2013;21(8):1058–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Theologis AA, Haughom B, Liang F, et al. Comparison of T1rho relaxation times between ACL-reconstructed knees and contralateral uninjured knees. Knee Surgery, Sport Traumatol Arthrosc. 2014;22(2):298–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li H, Tao H, Hua Y, Chen J, Li Y, Chen S. Quantitative magnetic resonance imaging assessment of cartilage status: A comparison between young men with and without anterior cruciate ligament reconstruction. Arthrosc - J Arthrosc Relat Surg. 2013;29(12):2012–2019. [DOI] [PubMed] [Google Scholar]
- 28.Haughom B, Schairer W, Souza RB, Carpenter D, Ma CB, Li X. Abnormal tibiofemoral kinematics following ACL reconstruction are associated with early cartilage matrix degeneration measured by MRI T1rho. Knee. 2012;19(4):482–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ithurburn MP, Zbojniewicz AM, Thomas S, et al. Lower patient-reported function at 2 years is associated with elevated knee cartilage T1rho and T2 relaxation times at 5 years in young athletes after ACL reconstruction. Knee Surgery, Sport Traumatol Arthrosc. 2019;27(8):2643–2652. [DOI] [PubMed] [Google Scholar]
- 30.Sapega AA. Muscle performance evaluation in orthopaedic practice. J Bone Jt Surg - Ser A. 1990;72 A(10):1562–1574. [PubMed] [Google Scholar]
- 31.Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29(2):213–218. [DOI] [PubMed] [Google Scholar]
- 32.Peterfy CG, Guermazi A, Zaim S, et al. Whole-organ magnetic resonance imaging score (WORMS) of the knee in osteoarthritis. Osteoarthr Cartil. 2004;12(3):177–190. [DOI] [PubMed] [Google Scholar]
- 33.Carballido-Gamio J, Link TM, Majumdar S. New techniques for cartilage magnetic resonance imaging relaxation time analysis: Texture analysis of flattened cartilage and localized intra- and inter-subject comparisons. Magn Reson Med. 2008;59(6):1472–1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Holm S A simple sequentially rejective multiple test procedure. Scand Stat Theory Appl. 1979;6:65–70. [Google Scholar]
- 35.Bodkin S, Goetschius J, Hertel J, Hart J. Relationships of Muscle Function and Subjective Knee Function in Patients After ACL Reconstruction. Orthop J Sport Med. 2017;5(7):232596711771904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mosher TJ, Dardzinski BJ. Cartilage MRI T2 relaxation time mapping: Overview and applications. Semin Musculoskelet Radiol. 2004;8(4):355–368. [DOI] [PubMed] [Google Scholar]
- 37.David-Vaudey E, Ghosh S, Ries M, Majumdar S. T2 relaxation time measurements in osteoarthritis. Magn Reson Imaging. 2004;22(5):673–682. [DOI] [PubMed] [Google Scholar]
- 38.Dardzinski BJ, Mosher TJ, Li S, Van Slyke MA, Smith MB. Spatial variation of T2 in human articular cartilage. Radiology. 1997;205(2):541–545. [DOI] [PubMed] [Google Scholar]
- 39.Joseph GB, Baum T, Alizai H, et al. Baseline mean and heterogeneity of MR cartilage T 2 are associated with morphologic degeneration of cartilage, meniscus, and bone marrow over 3years - data from the Osteoarthritis Initiative. Osteoarthr Cartil. 2012;20(7):727–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liebl H, Joseph G, Nevitt MC, et al. Early T2 changes predict onset of radiographic knee osteoarthritis: Data from the osteoarthritis initiative. Ann Rheum Dis. 2015;74(7):1353–1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Arhos EK, Thoma LM, Grindem H, Logerstedt D, Risberg MA, Snyder‐Mackler L. Association of Quadriceps Strength Symmetry and Surgical Status with Clinical Osteoarthritis 5 Years after Anterior Cruciate Ligament Rupture. Arthritis Care Res (Hoboken). October 2020:acr.24479. [DOI] [PMC free article] [PubMed]
- 42.Wang HJ, Ao YF, Jiang D, et al. Relationship between Quadriceps Strength and Patellofemoral Joint Chondral Lesions after Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2015;43(9):2286–2292. [DOI] [PubMed] [Google Scholar]
- 43.Pietrosimone B, Pfeiffer SJ, Harkey MS, et al. Quadriceps weakness associates with greater T1ρ relaxation time in the medial femoral articular cartilage 6 months following anterior cruciate ligament reconstruction. Knee Surgery, Sport Traumatol Arthrosc. 2019;27(8):2632–2642. [DOI] [PubMed] [Google Scholar]
- 44.Troy Blackburn J, Pietrosimone B, Harkey MS, Luc BA, Pamukoff DN. Quadriceps Function and Gait Kinetics after Anterior Cruciate Ligament Reconstruction. Med Sci Sports Exerc. 2016;48(9):1664–1670. [DOI] [PubMed] [Google Scholar]
- 45.Lewek M, Rudolph K, Axe M, Snyder-Mackler L. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech. 2002;17(1):56–63. [DOI] [PubMed] [Google Scholar]
- 46.Ithurburn M, McNally M, Hewett T, Paterno MSL. Quadriceps Strength Symmetry at the Time of Return-to-Sport and Landing Mechanics 2 Years Later in Young Athletes after ACL Reconstruction. J Orthop Sport Phys Ther. 2017;41(1):A40. [Google Scholar]
- 47.Palmieri-Smith RM, Thomas AC. A neuromuscular mechanism of posttraumatic osteoarthritis associated with ACL injury. Exerc Sport Sci Rev. 2009;37(3):147–153. [DOI] [PubMed] [Google Scholar]
- 48.Chaudhari AMW, Briant PL, Bevill SL, Koo S, Andriacchi TP. Knee kinematics, cartilage morphology, and osteoarthritis after ACL injury. Med Sci Sports Exerc. 2008;40(2):215–222. [DOI] [PubMed] [Google Scholar]
- 49.Wellsandt E, Gardinier ES, Manal K, Axe MJ, Buchanan TS, Snyder-Mackler L. Decreased Knee Joint Loading Associated with Early Knee Osteoarthritis after Anterior Cruciate Ligament Injury. Am J Sports Med. 2016;44(1):143–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Potter HG, Jain SK, Ma Y, Black BR, Fung S, Lyman S. Cartilage injury after acute, isolated anterior cruciate ligament tear: Immediate and longitudinal effect with clinical/MRI follow-up. Am J Sports Med. 2012;40(2):276–285. [DOI] [PubMed] [Google Scholar]
- 51.Patel SA, Hageman J, Quatman CE, Wordeman SC, Hewett TE. Prevalence and location of bone bruises associated with anterior cruciate ligament injury and implications for mechanism of injury: A systematic review. Sport Med. 2014;44(2):281–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shi H, Ding L, Jiang Y, et al. Bone Bruise Distribution Patterns After Acute Anterior Cruciate Ligament Ruptures: Implications for the Injury Mechanism. Orthop J Sport Med. 2020;8(4):232596712091116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mosher TJ, Smith H, Dardzinski BJ, Schmithorst VJ, Smith MB. MR Imaging and T2 Mapping of Femoral Cartilage. Am J Roentgenol. 2001;177(3):665–669. [DOI] [PubMed] [Google Scholar]


