Abstract
Objectives:
The current study aimed to examine the relationship between patient characteristics (internal psychological, external psychological, internal physical, external physical, and educational) and self-monitoring of blood glucose among noninsulin-treated patients with type 2 diabetes in a local primary care setting.
Methods:
This was a cross-sectional study, in which data were collected by a structured questionnaire. Correlational and multivariate multiple regression analyses were performed. Three hundred seventy-four noninsulin-treated patients with type 2 diabetes were eligible and completed the questionnaire in August 2019. The response rate was 93.5%. The respondents’ self-reported self-monitoring of blood glucose adherence was the main outcome measure.
Results:
In predicting self-monitoring of blood glucose adherence, the current regression model accounted for 12.3% of the variance (Adjusted R2 = 0.123, p < 0.05), with internal psychological factors and educational factors being significant. External psychological factors, external physical factors, and internal physical factors were found to be statistically nonsignificant.
Conclusion:
The findings highlighted the facilitating role of internal psychological factors and educational factors in SMBG adherence in noninsulin-treated type 2 diabetic patients. Among these factors, the education aspect was relatively strongly associated with increased SMBG adherence. With adequate patient education on diabetes and SMBG, the increased literacy would possibly strengthen patients’ internal psychological factors and motivate them to uptake SMBG practice. Implications from the current findings suggested that further research on different SMBG parameters is warranted to fill the knowledge gap in structuring an individualized and targeted SMBG protocol for better diabetic care.
Keywords: Facilitators, SMBG, noninsulin-treated type 2 diabetes, primary care, Hong Kong
Introduction
Epidemiology of diabetes
As recognized by the World Health Organization (WHO), diabetes is one of the most common chronic diseases that has risen in global prevalence and is regarded as a major cause of blindness, kidney failure, heart attack, stroke, and lower limb amputation. 1 Approximately 463 million adults (20–79 years) were diagnosed with diabetes worldwide in 2019, and this number is estimated to reach 700 million by 2045. 2 Within this population, the proportion of people with type 2 diabetes is increasing in most countries. According to the International Diabetes Federation, 2 374 million people are at the risk of developing type 2 diabetes. 2 In Hong Kong, diabetes was reported to affect 10% of individuals, or in other words, a total of 700,000 people in 2012. 3 In 2019, the diabetes prevalence in Hong Kong reported an average of 12.2%. 4
Diabetes is a chronic disease that poses considerable health challenges. The need for better diabetes management is asserted. Given the essential role of primary care settings in diabetes management, one of the common tools for diabetes care in the local health system, the self-monitoring of blood glucose (SMBG), is examined in this study. By investigating the potential barriers and facilitators of SMBG adherence, it is with hope that the knowledge of SMBG practices would be enriched for better self-management and health outcomes.
Overview of common SMBG practices
In 1997, the American Diabetes Association (ADA) Clinical Practice Recommendations suggested the SMBG frequency to be once daily for type 2 diabetes treated pharmacologically, but it did not specify a frequency for diet-controlled type 2 diabetic patients. 5 A more updated release of the ADA in 2013 did maintain the advocation of appropriate and regular SMBG for effective diabetes management, and still did not specify any prescribed frequency for these patients. 6 Guidelines from the International Diabetes Federation (IDF) for noninsulin-treated patients with type 2 diabetes recommended regular and low-intensity use of SMBG in the early treatment of patients, but no individualized prescription was suggested. 7
In Hong Kong, based on the recent publication of the Hong Kong Reference Framework for Diabetes Care for Adults in Primary Care Settings, 8 SMBG is an effective self-management tool for diabetic patients to improve glycemic control. The publication also suggested that SMBG should be individualized to meet the particular needs and treatment goals of each patient. In practice, however, Hong Kong doctors in local general out-patient clinics (GOPCs) are required to follow standard guidelines when prescribing the SMBG (i.e. certain frequency and timing) to diabetic patients Apart from the different guidelines or lack thereof in the prescription of SMBG, the effectiveness of this well-advocated treatment paradigm, especially for noninsulin-treated type 2 diabetic patients, is also being disputed in some research reviews.
The controversy over SMBG as an effective tool for diabetes management
Although SMBG has long been regarded as a key component for glycemic control in diabetes management, 9 - 11 this common practice has been challenged by some equivocal findings reporting that SMBG only had minimal clinical efficacy for noninsulin-treated type 2 diabetic patients.12,13 To respond to such controversy and to address the implications for health policy and medical resource allocation, Dr Polonsky and his team investigated the SMBG practice more carefully and provided compelling conclusions.14,15 In their 12-month multicenter prospective study that was cluster-randomized, it was found that the appropriate use of structured SMBG could significantly improve glycemic control in noninsulin-treated diabetic patients. 15 The team concluded that SMBG could be effective and beneficial if it is used in a structured way, while implementing SMBG in an unstructured way could be of little value, as reported in counter-point narratives.12,13 The team also argued that SMBG should not be examined as a uniform and unvarying form of intervention, and reminded that its efficacy would depend on how well-structured it is when being practiced.
As such, Dr. Polonsky and his fellows recommended the importance of evaluating different crucial parameters to define and provide structure to the SMBG protocol for more proper practice. 14 Some of these parameters included the SMBG frequency and timing, clinicians’ SMBG-related knowledge and skills to work with patients in a collaborative manner, as well as factors that could possibly affect patients’ compliance to SMBG practice. The present study resonated with this suggestion and aimed to evaluate some possible psychological, physical, and educational parameters that might facilitate or hinder the adherence and efficacy of SMBG for noninsulin-treated type 2 diabetic patients. This study also echoed the emphasis of using an individualized SMBG protocol as recommended in the guidelines in the United States and Hong Kong.7,8
Possible facilitators and barriers of SMBG practice
Patients were generally found to have poor adherence to the self-management plan and glucose monitoring at home. 16 - 18 As reported in a local descriptive study conducted in the North District region in Hong Kong in 2006, 16 only 20% performed SMBG in the sample, with the remaining 80% describing barriers such as self-management knowledge, financial difficulties, and older age.
Referring to findings from other international studies, lower neighborhood socioeconomic status, older age, fewer HbA1c tests, and fewer physician visits were associated with lower rates of self-monitoring. 18 In another study of more than 44,000 patients with type 1 and type 2 diabetes patients, the nonadherent practice of SMBG in diabetic patients was predicted by a longer time frame after their diagnosis, less intensive therapy, younger age, being male, ethnic minority, lower educational levels, lower socioeconomic status, weaker English communication, smoking, excessive alcohol consumption, and higher out-of-pocket costs for glucometer strips. 10
A qualitative study conducted by Ong and her fellows in Malaysia 17 identified further barriers and facilitators of SMBG through semistructured interviews with patients. The reported barriers included patients’ cost concern of test strips and needles, frustration related to high blood glucose reading, a perception that SMBG was only for insulin titration, lack of knowledge and perceived self-efficacy, lack of motivation, stigma, fear of needles and pain, inconvenience, and unconducive workplaces. In parallel, some facilitators of SMBG also noted that patients’ experiences of hypoglycemic symptoms, family motivation, desire to see the effects of dietary changes, and desire to please the physician when approaching their appointment dates were factors affecting their adherence to SMBG.
Present knowledge gap
Learning from both local and international studies, and given the knowledge gap in the parameters constituting a structured and individualized SMBG protocol for noninsulin-treated type 2 diabetic patients, the present research attempted to explore a few of the possible parameters for insight on better diabetes management.
Objectives
The purpose of the current study was to examine the relationship between patient characteristics and SMBG among noninsulin-treated patients with type 2 diabetes in a local GOPC setting. It aimed to investigate the possible predictors for patients’ SMBG adherence to fill the knowledge gap in the structuring of SMBG practice for potentially more effective and valuable outcomes. The five categories of predictors investigated included the internal psychological, external psychological, internal physical, external physical, and educational according to Simmons’ theoretical framework. 19
Method
Sample
The convenient sampling method was adopted in this study. Four hundred noninsulin-treated patients with type 2 diabetes who met the inclusion criteria and attended the primary care setting in the designated diabetes room of the Violet Peel GOPC in the Hong Kong East Cluster of the hospital authority in August 2019 were invited by the principal researcher to complete a structured questionnaire. This designated room had a daily attendance of around 70 patients. Among the 400 invited patients in this study, 374 were eligible and completed the questionnaire. The response rate to this survey was 93.5%.
Procedure
The current research was a cross-sectional study conducted from June to September in 2019, in which data was collected by a structured questionnaire in a single center. Approval of this study was obtained from the Hong Kong East Cluster Research Ethics Committee (Ethics Approval Number: HKECREC-2019-052). Participants qualified for this study if they were aged 18 or above, diagnosed with type 2 diabetes but noninsulin-treated, and able to understand Chinese. Noninsulin-treated diabetic patients with known psychiatric illnesses were excluded from the study.
Written informed consent was obtained from all subjects before the study. All the eligible respondents were given a consent form to sign when they agreed to participate in this study as invited by the principal researcher. A nurse then distributed a self-reported questionnaire to the respondents to fill in. They were required to complete it in 10 minutes. The respondents were then asked to return it to the researcher directly in the consultation room. For respondents who were illiterate or unable to fill in the questionnaire by themselves, a nurse would assist on the side by reading the questions out loud and recording their responses on the questionnaire. During the process, the confidentiality of information was guaranteed so the participants could ensure their information would not be disclosed.
Measures
Demographics
Demographic information including the sex, age, employment status (full-time employment, part-time employment, retired, unemployed), and living conditions (lived alone, lived with others) of participants was collected by the questionnaire.
Independent variables
The potential predictors of SMBG were categorized into five factors adapted from Simmons et al.’s 19 framework and used as the independent variables for investigation in this study. The five variables were (1) internal psychological factors (health beliefs, perception of the normality of blood glucose levels, perceived self-efficacy, motivation, priorities/time, and perceived usefulness of SMBG), (2) external psychological factors (stigma due to having diabetes, family motivation, and support), (3) internal physical factors (onset age of diabetes, duration of diabetes, other health conditions and complications, experience of hypoglycemia, pain, and other side effects associated with SMBG), (4) external physical factors (personal finance, affordability of test strips and needles, physical access to services and information, living with family), and (5) educational factors (educational level, diabetes knowledge, knowledge of SMBG).
Following this theoretical framework, a total of 20 items divided into five subscales were constructed by the principal researcher. Each item was self-rated by participants on a 5-point Likert-type scale. A higher rating indicated a higher intensity or stronger inclination for that item, except for items 2 and 7, which were reversely scored. A higher composite score for each sub-scale indicated a stronger effect for that factor. The face validity and content validity of the questionnaire were evaluated by the researcher and a registered clinical psychologist working in the government sector. The items were also translated and back-translated by the researcher and psychologist.
Dependent variable/outcome measure
The outcome measure was a measure of the respondent’s self-reported SMBG adherence. It was the composite score of the following two items: (1) perceived adherence to SMBG practice on a 5-point Likert-type scale (ranging from “1,” representing “Never Complied” to “5,” representing “Always Complied”) and (2) their self-reported frequency of SMBG in a 3-month interval (ranging from “1,” representing “Seldom” to “5,” representing “Very Frequent”). A higher composite score indicated stronger self-reported adherence.
Reliability and validity of the questionnaire
As abovementioned, the questionnaire for this study consisted of a total of 22 items, including 20 items grouped under the five independent variables, and 2 items for the dependent variable. All 22 items were used in the subsequent quantitative analyses. According to the internal consistency analysis for the 20-item measure of independent variables, the overall reliability indicated by a Cronbach’s alpha value was 0.58. While the number of items and Cronbach’s alpha value for each independent variable is shown in Table 1, with a range from 0.55 to 0.61. Given a Cronbach’s alpha values between 0.50 and 0.70, this measure indicated a modest but acceptable reliability because of the exploratory nature of the study.20,21 For the dependent variable, the internal consistency analysis of the two items indicated a Cronbach’s alpha value of 0.92, which showed good reliability of the measure.20,22
Table 1.
Reliability of the five independent variables and dependent variable.
| Variable | No. of items | Cronbach’s alpha (α) |
|---|---|---|
| Internal psychological | 6 | 0.58 |
| External psychological | 2 | 0.61 |
| Internal physical | 5 | 0.57 |
| External physical | 4 | 0.61 |
| Educational | 3 | 0.55 |
| SMBG adherence | 2 | 0.92 |
SMBG: self-monitoring of blood glucose.
According to Kelloway, 22 it is suggested that the sample size should be no smaller than 200, and the sample size to model parameter ratio should be at least 5:1. Our sample size consisted of 374 subjects who met both criteria. 22 The questionnaire was validated with 100 respondents, which was approximately 27% of the sample size. The questionnaire is shown in Supplemental Appendix A.
Statistical analysis
The percentage of the categorical parameters for the sample characteristics were calculated, while the descriptive statistics of the mean and standard deviations of the independent variables and dependent variable were also performed. Correlational and multivariate multiple regression analyses were conducted to investigate the association between the independent variables and dependent variable, with a p < 0.05 being considered to be statistically significant.
For this regression analysis, the normality of data was assumed according to the central limit theorem and Kolmogorov–Smirnov test. The central limit theorem states a sample size over 100 could assume normal distribution. While the Kolmogorov–Smirnov test conducted on our sample reported a value of p > 0.05, which accepted the null hypothesis and indicated data were normally distributed. In addition, a collinearity test was also conducted, in which the data met the assumption of collinearity and that multicollinearity was not a concern in this study.
Results
Of the 374 respondents, 49.2% (184/374) were male and 50.8% (190/374) were female. Their age ranged from 39 to 93 years old, with a mean of 66.73 years old and a standard deviation of 9.602. Among these respondents, 29.9% (112/374) were employed full-time, 8.6% (32/374) were employed part-time, 41.7% (156/374) were retired, and 19.8% were unemployed (74/374); 14.2% (53/374) reported to be living alone, while 85.8% (321/374) reported to be living with others. The sample characteristics are shown in Table 2.
Table 2.
Characteristics of the sample.
| Characteristics | Number of participants (%) |
|---|---|
| N = 374 | |
| Mean age (SD) | 66.73 (9.602) |
| Sex | |
| Male (n = 184) | 49.2 |
| Female (n = 190) | 50.8 |
| Employment status | |
| Employed full-time (n = 112) | 29.9 |
| Employed part-time (n = 32) | 8.6 |
| Retired (n = 156) | 41.7 |
| Unemployed (n = 74) | 19.8 |
| Living condition | |
| Lived alone (n = 53) | 14.2 |
| Lived with others (n = 321) | 85.8 |
SD: standard deviation.
Descriptive statistics (mean and standard deviation) of the sample scores for the five independent variables measured as SMBG predictive factors (internal psychological, external psychological, internal physical, external physical, and educational), and the dependent variable of SMBG adherence rated on a 5-point Likert-type scale are shown in Table 3. A higher sample score for each predictive factor indicated a stronger self-reported effect of the factor, while a higher sample score on the outcome measure indicated a higher self-reported SMBG adherence.
Table 3.
Descriptive statistics of the sample scores on the measures of SMBG predictive factors and SMBG adherence.
| Variable | Min. score | Max. score | Mean of score | SD of score |
|---|---|---|---|---|
| Internal psychological | 1 | 5 | 3.74 | 0.49 |
| External psychological | 1 | 5 | 3.72 | 0.67 |
| Internal physical | 1 | 5 | 2.91 | 0.57 |
| External physical | 1 | 5 | 2.87 | 0.56 |
| Educational | 1 | 5 | 3.44 | 0.61 |
| SMBG adherence | 1 | 5 | 2.53 | 1.14 |
SMBG: self-monitoring of blood glucose.
Correlational and multivariate multiple regression analyses were performed to investigate the association between the predictive factors and SMBG adherence in noninsulin-treated type 2 diabetic participants, while sex, age, employment status, and living conditions of participants were analyzed as covariates in the regression model.
The correlations between the five predictive variables and outcome variables of SMBG adherence are shown in Table 4. Three out of the five predictive factors (internal psychological, external physical, and educational) were found to have a statistically significant positive correlation with the outcome of SMBG adherence. Nevertheless, the external physical factor was positively correlated with external psychological and educational factors.
Table 4.
Correlation between the five SMBG predictive factors and SMBG adherence.
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. Internal psychological | 1.00 | |||||
| 2. External psychological | 0.297* | 1.00 | ||||
| 3. Internal physical | −0.176* | −0.082 | 1.00 | |||
| 4. External physical | 0.118 | 0.135* | 0.024 | 1.00 | ||
| 5. Educational | 0.283* | 0.102 | −0.111 | 0.175* | 1.00 | |
| 6. SMBG Adherence | 0.244* | 0.110 | −0.009 | 0.179* | 0.294* | 1.00 |
SMBG: self-monitoring of blood glucose.
Note. *p < 0.01.
With regard to the regression model predicting SMBG adherence, the overall regression model was statistically significant and accounted for 14.4% of the variance (R2 = 0.144, p < 0.05). Age, sex, employment status, and living condition were entered into the regression model as covariates in the first step as model 1, and the five predictor variables (internal psychological, external psychological, internal physical, external physical, and education) were entered into the regression model in the second step as model 2. The results indicated that adding in the five predictive variables had significantly improved the regression model on predicting SMBG adherence (△R2 = 0.113, F(5, 363) = 9.624, p < 0.001) despite age, sex, employment status, and living condition. The model summary is shown in Table 5.
Table 5.
Model summary.
| Model | R | R2 | Adjusted R2 | Std. error of the estimate | Change statistics | ||
|---|---|---|---|---|---|---|---|
| △R2 | F change | Sig. F change | |||||
| 1 | 0.176 a | 0.031 | 0.020 | 1.132 | 0.031 | 2.934 | 0.021 |
| 2 | 0.380 b | 0.144 | 0.123 | 1.071 | 0.113 | 9.624 | 0.000 |
Predictors: (constant), age, sex, employment status, living condition.
Predictors: (constant), age, sex, internal psychological, external psychological, internal physical, external physical, educational.
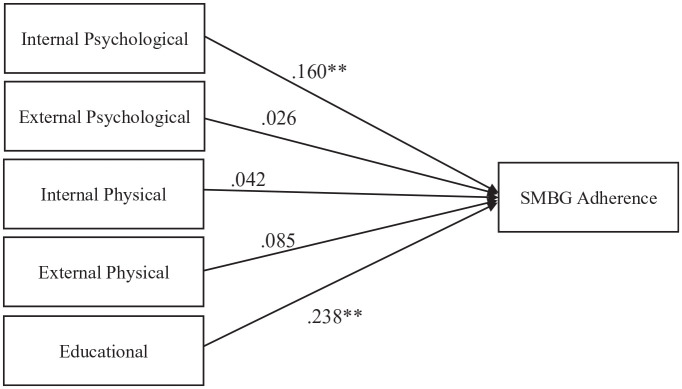
An examination of the weights assigned to the five predictor variables in the regression analysis revealed that only two of the predictor variables made unique, statistically significant contributions to the predictive accuracy (see Table 5). Specifically, the independent variables of internal psychological (β = 0.160, p < 0.01), and educational (β = 0.238, p < 0.01) factors were revealed to have a significant positive weighing on the dependent variable, indicating that the presence of higher internal psychological factor and educational factor were associated with higher SMBG adherence. The results are shown in Table 6, and the regression model is presented in Figure 1.
Table 6.
Results of the regression model predicting SMBG adherence.
| Unstandardized coefficients | Standardized coefficients | Collinearity statistics | |||
|---|---|---|---|---|---|
| B | SE | β (Beta) | Tolerance | VIF | |
| Intercept | −1.629 | 0.837 | |||
| Internal psychological | 0.376** | 0.125 | 0.160** | 0.824 | 1.213 |
| External psychological | 0.044 | 0.090 | 0.026 | 0.864 | 1.158 |
| Internal physical | 0.084 | 0.104 | 0.042 | 0.877 | 1.140 |
| External physical | 0.173 | 0.109 | 0.085 | 0.826 | 1.211 |
| Education | 0.452** | 0.103 | 0.238** | 0.803 | 1.246 |
SMBG: self-monitoring of blood glucose.
Note. **p < 0.01 Dependent variable = SMBG adherence.
Figure 1.
The regression model predicting SMBG adherence.
SMBG: self-monitoring of blood glucose.
Discussion
The present study attempts to provide theoretical and practical implications for structuring SMBG practices in noninsulin-treated type 2 diabetic patients. Some of the current findings supported those in previous studies, while some were found to be unique to the local Hong Kong sample. In predicting SMBG adherence, the current research model accounted for 12.3% of the variance, with internal psychological factors and educational factors being significant. Although these two factors indicated statistically significant contributions to predict the SMBG adherence, the value was low that should be interpreted with caution. It implied that the examined factors in the current study might just represent few of the possible parameters for predicting SMBG adherence. Meanwhile, external psychological factors, external physical factors, and internal physical factors were found to be statistically non-significant in predicting SMBG adherence.
Internal psychological and educational factors
Implying from the results, internal psychological factors and educational factors were identified as possible facilitators to SMBG adherence among noninsulin-treated patients with type 2 diabetes in this local sample. These findings were consistent with those in previous studies.10,17,19 Specifically, diabetic patients with stronger internal psychological factors that were more health conscious, perceived higher self-efficacy, motivation, and usefulness of SMBG, were reported to adhere more to SMBG practices. Similarly, those with higher educational levels and knowledge of both diabetes and SMBG were found to have higher self-reported adherence.
External psychological, external physical, and internal physical factors
Unexpectedly, the external psychological factors, external physical factors, and internal physical factors were not found to be related to SMBG adherence in this study. These results deviated from previous findings in non-Hong Kong samples. 17 - 19 According to clinical observations and the primary care landscape in Hong Kong, it is speculated that the external psychological factors such as the stigma of having diabetes and having family motivation and support are not deemed to be key concerns for diabetic patients in the local culture. Similarly, external physical factors such as personal finance and affordability of test strips, physical access to services, and living with family might not be significant barriers for SMBG uptake for this sample. This may be related to the sampling location of Wanchai, which is one of the wealthiest districts in Hong Kong. Also, considering the accessibility of local clinics and that almost 86% of our respondents were living with others, it is likely that external physical factors might not be key barriers for this sample.
The lack of association between internal physical factors and SMBG adherence, however, calls for attention. In particular, internal physical factors, including the onset age and duration of diabetes, awareness of other health conditions and complications, experience of hypoglycemia, pain. and other side effects associated with SMBG, were surprisingly not determining factors for SMBG adherence. Some possibilities could be the patients’ limited understanding of the nature of diabetes and that the illness was asymptomatic in most cases. Indeed, not having sufficient knowledge and education on diabetes or being illiterate about their internal physical condition may be a possibility for poorer SMBG adherence.
Limitations
The results of this study need to be considered in light of its limitations. In particular, the adoption of self-reported measures could be a caveat that might lead to recall and response bias. As such, some objective measures including the provision of a glucometer and retrieval of medical records could be considered in future studies. For example, leveraging technology such as the use of smartphone-based SMBG could be an option. 23 Also, given the modest reliability of the current measure of the predictive factors, the question items could be revised and modified with consideration for further exploratory factor analyses and for streamlining the scales. In addition, as the present study was a cross-sectional study and adopted convenient sampling, it is suggested that random sampling and a longitudinal method could be used to enhance the empirical design of the study. The limitation of having a limited sample size from a single center could be improved by testing the research protocol in other primary care clinics and relevant medical units on a larger scale to enhance the generalizability of research findings in the future. In addition, a power analysis could be conducted for a better sample size estimation for future studies.
Conclusion
In general, the findings highlighted the potential facilitating role of internal psychological factors and educational factors in SMBG adherence in noninsulin-treated type 2 diabetic patients under a theoretical framework. Responding to the controversy of the effectiveness of SMBG practices in this type of diabetic patients and recognizing the benefits of using a structured SMBG protocol, it is suggested that several parameters may be considered in the practice of SMBG. Among them, the educational aspect was revealed to be relatively strongly associated with increased SMBG adherence. As such, adequate patient education on diabetes and SMBG as well as increased literacy would likely strengthen patients’ internal psychological factors, including the perception of higher self-efficacy and usefulness of SMBG. Together, these may increase patients’ awareness of their internal physical condition and encourage their motivation to better uptake SMBG.
To translate these insights into meaningful clinical practices, it is suggested that patient education and self-care could be emphasized, and that community-based educational programs with simple and accessible methods for delivery could be considered to empower and motivate target patient groups to uptake SMBG practices. These implications also reaffirm the much-needed steer from the “disease-oriented” approach to “patient-oriented” approach in the overall health management of diabetes patients in the local population.
Acknowledging that this was a relatively small-scale local study, cautions should be made to avoid overgeneralizations of the findings. Nevertheless, the current study serves as an initiative to call for more concerted efforts to fill the knowledge gap in diabetes care in the community.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121211066150 for Predictors of self-monitoring of blood glucose among noninsulin-treated patients with type 2 diabetes in a primary care setting in Hong Kong: A cross-sectional study by Wing-hang Mak and Rebecca Wing-man Lau in SAGE Open Medicine
Acknowledgments
The authors would like to acknowledge the supervisors and colleagues in the relevant work departments, and the Research Ethics Committee of the Hong Kong East Cluster of Hospital Authority that made this research possible. The authors would also like to thank Dr Ivan CHOW and Dr Vince HO for their help in editing the manuscript.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from the Hong Kong East Cluster Research Ethics Committee of the Hospital Authority in Hong Kong (Ethics Approval Number: HKECREC-2019-052).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from all subjects before the study.
ORCID iD: Rebecca Wing-man Lau  https://orcid.org/0000-0001-5866-5521
https://orcid.org/0000-0001-5866-5521
Supplemental material: Supplemental material for this article is available online.
References
- 1. World Health Organization (WHO). Diabetes: key facts, 2019, https://www.who.int/news-room/fact-sheets/detail/diabetes (assessed 30 June 2020). [Google Scholar]
- 2. International Diabetes Federation (IDF). Diabetes facts and figures, 2019, https://www.idf.Org/aboutdiabetes/what-is-diabetes/facts-figures.html (assessed 30 June 2020).
- 3. Wong MC, Sin CK, Lee JP. The reference framework for diabetes care in primary care settings. Hong Kong Med J 2012; 18(3): 238–246. [PubMed] [Google Scholar]
- 4. International Diabetes Federation (IDF). IDF Diabetes Atlas, 2019, https://idf.org/our-network/regions-members/western-pacific/members/103-hongkong.html (assessed 30 June 2020).
- 5. Akhter J. The American diabetes association’s clinical practice recommendations and the developing world. Diabetes Care 1997; 20(6): 1044–1045. [DOI] [PubMed] [Google Scholar]
- 6. American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes Care 2013; 36(Suppl. 1): S11–S66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gagliardino JJ, Bergenstal R, Colagiuri S, et al. IDF guideline on self-monitoring of blood glucose in non-insulin treated type 2 diabetes. Bruselas: International Diabetes Federation, 2009. [Google Scholar]
- 8. Food Health Bureau. Hong Kong reference framework for diabetes care for adults in primary care settings, https://www.fhb.gov.hk/pho/english/resource/files/professionals_DM_Module5.pdf (assessed 22 June 2020).
- 9. American Diabetes Association. Epidemiology of diabetes interventions and complications (EDIC). Design, implementation, and preliminary results of a long-term follow-up of the diabetes control and complications trial cohort. Diabetes Care 1999; 22(1): 99–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Karter AJ, Ackerson LM, Darbinian JA, et al. Self-monitoring of blood glucose levels and glycemic control: the Northern California kaiser permanente diabetes registry. Am J Med 2001; 111(1): 1–9. [DOI] [PubMed] [Google Scholar]
- 11. Breland JY, McAndrew LM, Burns E, et al. Using the common sense model of self-regulation to review the effects of self-monitoring of blood glucose on glycemic control for non–insulin-treated adults with type 2 diabetes. Diabetes Educ 2013; 39(4): 541–559. [DOI] [PubMed] [Google Scholar]
- 12. Malanda UL, Welschen LM, Riphagen II, et al. Self-monitoring of blood glucose in patients with type 2 diabetes mellitus who are not using insulin. Cochrane Database Syst Rev 2012; 1: CD005060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Farmer AJ, Perera R, Ward A, et al. Meta-analysis of individual patient data in randomised trials of self monitoring of blood glucose in people with non-insulin treated type 2 diabetes. BMJ 2012; 344: e486. [DOI] [PubMed] [Google Scholar]
- 14. Polonsky WH, Fisher L. Self-monitoring of blood glucose in noninsulin-using type 2 diabetic patients: right answer, but wrong question: self-monitoring of blood glucose can be clinically valuable for noninsulin users. Diabetes Care 2013; 36(1): 179–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Polonsky WH, Fisher L, Schikman CH, et al. Structured self-monitoring of blood glucose significantly reduces A1C levels in poorly controlled, non-insulin treated type 2 diabetes: results from the structured testing program study. Diabetes Care 2011; 34(2): 262–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lau WH, Chiu SL, Wong WY, et al. Study on the demographics and social background of Type 2 diabetes in general out-patient settings of north district region and their relation to the attitude towards self-monitoring of blood glucose. Kowloon, Hong Kong: Hospital Authority Convention, 2006. [Google Scholar]
- 17. Ong WM, Chua SS, Ng CJ. Barriers and facilitators to self-monitoring of blood glucose in people with type 2 diabetes using insulin: a qualitative study. Patient Prefer Adherence 2014; 8: 237–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Adams AS, Mah C, Soumerai SB, et al. Barriers to self-monitoring of blood glucose among adults with diabetes in an HMO: a cross sectional study. BMC Health Serv Res 2003; 3(1): 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Simmons D, Weblemoe T, Voyle J, et al. Personal barriers to diabetes care: lessons from a multi-ethnic community in New Zealand. Diabet Med 1998; 15(11): 958–964. [DOI] [PubMed] [Google Scholar]
- 20. Streiner DL, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use. Aust N Z J Public Health 2016; 40(3): 294–295. [DOI] [PubMed] [Google Scholar]
- 21. Bowling A. Research methods in health: investigating health and health services. London: McGraw-Hill Education, 2014. [Google Scholar]
- 22. Kelloway EK. Using Mplus for structural equation modeling: a researcher's guide. New York: SAGE, 2014. [Google Scholar]
- 23. Kshanti IA, Mokoagow MI, Rosandi R, et al. Use of smartphone-based self-monitoring blood glucose application in type 2 diabetes mellitus patients in Indonesia: a pre and post-test study. Bali Medical J 2021; 10(1): 219–224. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121211066150 for Predictors of self-monitoring of blood glucose among noninsulin-treated patients with type 2 diabetes in a primary care setting in Hong Kong: A cross-sectional study by Wing-hang Mak and Rebecca Wing-man Lau in SAGE Open Medicine