Abstract
Introduction:
Depression is one of the most common comorbid psychiatric disorders among diabetic patients. Depression among diabetic people has led to poor treatment adherence, defective treatment outcomes, and consequently worsened quality of life. However, there is a limited study conducted to assess the magnitude and factors associated with depression among diabetic patients in Ethiopia including this study area.
Objective:
This study aimed to assess the prevalence and factors associated with depression among adult diabetic outpatients attending diabetic clinic in Eastern Ethiopia.
Methods:
An institution-based cross-sectional study was conducted among 407 adult diabetic outpatients on treatment in Ethiopia in 2020. Patient Health Questionnaire-9 was used to assess depression among randomly selected samples. Bivariate and multivariate logistic regression was fitted to identify factors associated with depression among diabetic outpatients. A p value less than 0.05 with a 95% confidence interval was considered statistically significant.
Results:
The overall prevalence of depression among diabetic outpatients was found to be 48.9% (95% confidence interval: 44.2%, 53.4%). Being female (adjusted odds ratio = 1.50, 95% confidence interval: 1.39, 2.73), Khat chewing (adjusted odds ratio = 1.88, 95% confidence interval: 1.22, 2.93), having poor and moderate social support (adjusted odds ratio = 1.79, 95% confidence interval: 1.07, 2.98 and adjusted odds ratio = 1.90, 95% confidence interval: 1.14, 3.17, respectively), taking both oral hypoglycemic agents and insulin medication (adjusted odds ratio = 1.33, 95% confidence interval: 1.13, 2.80) and duration of diabetes mellitus for more than 6 years (adjusted odds ratio = 5.40, 95% confidence interval: 3.42, 8.14) were significantly associated with depression.
Conclusion:
This study revealed a relatively high prevalence of depression in diabetic outpatients. A lesser level of social support, taking oral and insulin treatment regimes, longer duration of illness, using Khat, and being female were associated with depression among diabetic outpatients. Therefore, early screening and identification of such factors could help ameliorate some of the deleterious effects of depression in diabetic outpatients.
Keywords: Depression, diabetes mellitus, prevalence, Ethiopia
Introduction
Diabetes mellitus (DM) is a heterogeneous group of metabolic diseases that are characterized by chronic hyperglycemia (high blood sugar) and disturbances in carbohydrate, lipid, and protein metabolism resulting from defects in insulin secretion and/or insulin action. 1 It is a devastating illness that needs lifelong treatment and significantly increases the risk of serious, long-term complications. 2 In 2019, the prevalence of diabetes was projected to be 9.3% (463 million) and expected to rise to 10.2% (578 million) by 2030 worldwide.3,4 There is substantial evidence that diabetes is an epidemic in many low- and middle-income countries (LMICs), where it is a home for more than 75% of the diabetic population. 5 The global burden of disease study predicted that diabetes will take 10th place with 2.3% of the overall disease burden as a percentage of the overall disability-adjusted life years by 2030. 6
About 15%–20% of diabetic patients are expected to have moderate to severe depression and of this, 50%–75% of patients remain under diagnosed.7–10 In Ethiopia, according to World Health Organization (WHO) estimation, the number of diabetics cases will increase from 800,000 to 1.8 million by the year 2030 11 and a prevalence is as high as 8% in patients with other co-morbid illnesses. 12 A recent review reported a depression rate of 39.7% among diabetic patients in Ethiopia. 13
Thinking about depression among diabetic patients in a broader way, bearing in mind other factors associated with DM that have a role in increasing the possibility of developing depression is the cornerstone. In one study, gender, having diabetes complications, and being on insulin treatment have been associated significantly with higher occurrence of depression.14,15 Also, higher body mass index and poor glycemic control have been associated with an increased risk of major depression among diabetic patients. 16 In regard to age, there are studies that reported that age is linearly related to greater depression.17,18 On the other hand, a study reported that middle-aged diabetic patients have the highest risk of developing depression, 19 while others suggested that the younger the age, the higher the prevalence to develop depression.14,20 To add to the confusion, several studies stated that there is no relationship between age and depression among diabetic patients.21,22
Education has also been considered as a significant factor to affect the prevalence of depression among diabetic patients; some studies reported that low educational status has been associated with an increased depression rate.16,23 However, other studies failed to show a significant relationship between the educational level and depression among diabetic patients. 24 Other factors contributing to the development of depression among diabetic patients include marital status, work status, family income, medical co-morbidity, anxiety, quality of life, duration of illness, fear of complication, substance use, lack of physical activity, and poor social support.25–28
Depression has a profound adverse effect on the quality of life, treatment adherence and outcome, self-care, and health care costs in patients with diabetes. 29 It is evidenced that the co-morbidity of depression with a chronic illness incrementally deteriorates health outcomes as compared to having depression or chronic illness alone.30,31 Most people with diabetes were undiagnosed and left untreated for their comorbid depressive disorder. 32 An unprocessed ill-health state is specifically significant in Africa, where health care systems primarily focus on communicable diseases than non-communicable diseases like diabetes.33,34
Although developing countries carry a higher burden of diabetes and comorbid depression with diabetes, very little information is available about the magnitude of depression among diabetic patients and factors associated with it. Identifying factors of depression in patients with diabetes will help to develop strategies and interventions for treatment and mitigate the psychological distress of diabetic patients. To the level of investigators’ understanding, no studies have been done to find out the magnitude and predictors of depression among diabetic patients in the study area. Therefore, this study was aimed to determine the prevalence of depression and its associated factors among diabetic outpatients attending diabetic clinic at public hospitals in Ethiopia.
Materials and methods
Study design
An institution-based cross-sectional study was carried out.
Study setting
The study was conducted at public Hospitals in Harar, eastern Ethiopia from June 01 to July 01, 2020. Harar city is 526 km away from Addis Ababa, the capital of Ethiopia. The total population of Harar town is 183,415 (91,099 (49.7%) females and 92, 316 (50.3%) males). Of the total population, 54% were urban dwellers, and the rest were rural dwellers. 35 In Harar, there are two public hospitals, one police hospital, one private general hospital, one medical center, eight health centers, and 26 health posts. The two public hospitals have a total of 819 patients with diabetes on treatment, 421 in Hiwot Fana Specialized University Hospital, and 398 in Jugal Hospital.
Inclusion criteria
Patients with DM who are at the age of 18 years and above, and attending a diabetic follow-up clinic at public hospitals of eastern Ethiopia were included in the study.
Exclusion criteria
Severely ill patients who are unable to communicate and give required information were excluded from the study.
Study variables
The outcome variable was depression (presence/absence). The explanatory variables were socio-demographic factors like age, gender, relationship status, occupation, educational status, income, and residence; clinical variables such as co-morbidity, duration of DM, types of DM, types of medication for DM, level of blood glucose, and social and substance-related variables like poor social support, physical inactivity, tobacco, alcohol, Khat, and self-care practice.
Data collection instruments
A semi-structured, pre-tested questionnaire containing five components was administered by the interviewers to collect information. Socio-demographic variables were assessed using a structured questionnaire developed by reviewing similar related articles. 36 Information related to medication was obtained from the patient and confirmed by reviewing the medical chart. Self-care activities were assessed using the standard tool developed for diabetic self-care activity. It includes dietary practice, medication adherence, physical activity, and glucose monitoring, and foot care domains. To calculate the overall diabetic self-care practice value, the average of the mean values in each of the domains was used, 37 and it was highly reliable in the study with a Cronbach’s alpha of 0.82. The social support of the diabetic patient was assessed by the Oslo social support scale 3-item (OSSS-3). It is a standard tool developed to provide a brief measure of social functioning, and it is considered to be one of the best predictors of depression. 38 It was highly reliable in the study (Cronbach’s alpha = 0.88). Current and ever use of a substance as defined by reviewing the WHO Stepwise approach to assess non-communicable disease risk factors. 39 Patient Health Questionnaire-9 (PHQ-9) was used to assess depression. It has high sensitivity (88%) and specificity (88%) based on the structured psychiatric interview. 37 It was adopted and translated to the local language (Amharic and Afaan-Oromo) and back to English and was highly reliable in the study (Cronbach’s alpha = 0.86).
Sample size determination and sampling technique
The sample size for the study was estimated by a single population proportion formula with the assumption of 95% level of confidence, 5% margin of error, and 40.4% prevalence of depression from a study done in Bahirdar, Ethiopia. 36 By adding the 10% non-response rate, the final sample size became 407.
From the total of 819 diabetic patients who were on treatment at DM clinics, 407 patients were recruited for the study and proportionally allocated for both hospitals (209 and 198, for Hiwot Fana Specialized University Hospital and Jugal Hospital, respectively). A systematic random sampling technique was employed to select study participants by calculating the sampling interval (kth). Accordingly, every second patient was selected from each hospital and the first patient (out of the two) was selected by lottery method.
Data collection methods
Four trained nurses who are fluent in speaking local languages (Afaan-Oromo and Amharic languages) were selected to collect the data through face-to-face interviews and patient medical record review. One Health officer (BSc) and the principal investigator have supervised the daily activities. The training was given to data collectors and supervisors for 2 days on the data collection and ethical issues.
Operational definitions
Depression: A patient with a score of 5 and above in the PHQ-9 was considered to have depression. A total PHQ-9 score of 1–4 indicated “minimal depression,” 5–9 indicated “mild depression,” 10–14 indicated “moderate depression,” 15–19 indicated “moderately severe depression,” and 20–27 indicated “severe depression.” 37
Current use and ever of a substance: is using of at least one substance in the last 3 months and once in a lifetime, respectively. 39
Social support is classified into three categories based on OSSS-3; “poor social support” if a sum score was 3–8, “moderate social support” if a sum score was 9–11, and “strong social support” if a sum score was 12–14. 40
Good glycemic control: a fasting blood glucose level less than or equals 130 mg/dL.
Poor glycemic control: a fasting blood glucose level greater than 130 mg/dL. 41
Data quality control
Quality of data were assured by beginning with 2 days of guidance for the data collectors on interviewing patients and abstracting data from patient record charts. The local language (Afan-Oromo and Amharic) versions of the questionnaire were used for data collection and checked for their reliability. The collected data from the participants was reported to the supervisor every day to enable him or her to take immediate action in case of inconsistencies or problems that happened on the reported data. The pretest of data collection tools was carried out on 5% (20 diabetic patients) of sample size in the Jenela health center and modifications were incorporated into the tools.
Statistical analysis
Data were checked for its completeness on the day it was collected. The data were entered using Epi-Data 3.1 and analyzed using SPSS 20. Findings were described using percentages and frequencies. Bivariate and multivariate logistic regression was carried out to identify factors associated with depression among diabetic patients. The presence and absence of depression (PHQ-9 ⩾ 5 vs PHQ-9 < 5) was used in the logistic regression analysis. The strength of the association was described by odds ratio and 95% confidence interval (CI), and a p value less than 0.05 was considered statistically significant.
Ethical consideration
Ethical clearance was obtained from the Institutional Health Research Ethics Review Committee (IHRERC) of the College of Health and Medical Sciences, Haramaya University with the approval number of IHRERC/120/2020. A formal letter of support was obtained from Haramaya University, College of Health and Medical Sciences, and submitted to Hiwot Fana Specialized University Hospital and Jugal Hospital. Before the questionnaire was administered to any eligible participant, informed voluntary written and signed consent was obtained from heads of the hospitals, and each study participant. Confidentiality was maintained at all levels of the study. Diabetic patients who were found to have severe depression were referred to psychiatry clinics for further investigations.
Results
Socio-demographic and economic descriptions of the respondents
From 407 patients selected for the study, 401 consented to the study yielding a response rate of 98%. The mean age of the participants was 48.6 years with a standard deviation of 13.2 (Table 1).
Table 1.
Socio-demographic and economic characteristics of diabetic patients attending at public hospitals in Harar, East Ethiopia, 2020.
| Variables | Frequency (n = 401) | Percentage (%) | |
|---|---|---|---|
| Sex | Male | 197 | 49.10 |
| Female | 204 | 50.90 | |
| Age | 18–29 | 43 | 10.70 |
| 30–49 | 168 | 41.90 | |
| 50 + | 190 | 47.40 | |
| Residency | Urban | 293 | 73.10 |
| Rural | 108 | 26.90 | |
| Marital status | Single | 79 | 19.70 |
| Married | 242 | 60.30 | |
| Divorced | 66 | 16.50 | |
| Widowed | 14 | 3.50 | |
| Educational status | No formal education | 209 | 52.10 |
| Primarily school (1–8) | 104 | 25.90 | |
| Secondary school (9–12) | 55 | 13.70 | |
| Collage/university | 33 | 8.20 | |
| Occupational status | Farmer | 77 | 19.20 |
| Governmental employer | 163 | 40.60 | |
| Privet worker | 129 | 32.20 | |
| Others | 32 | 8.00 | |
| Living circumstance | With family | 316 | 78.9 |
| Alone | 85 | 21.1 | |
| Average monthly income of the household (in USD) | Less than 25 | 103 | 25.70 |
| 25–65 | 151 | 37.70 | |
| 66–95 | 69 | 17.20 | |
| Greater than 95 | 78 | 19.50 | |
Clinical characteristics of the participants
Around 57.1% of the study participants attained the target glycemic control of <130 mg/dL (Table 2).
Table 2.
Clinical characteristics of diabetic patients attending public hospitals in Harar, East Ethiopia, 2020.
| Variables | Frequency (n = 401) | Percentage (%) | |
|---|---|---|---|
| Types of diabetes mellitus | Type I | 100 | 24.90 |
| Type II | 301 | 75.10 | |
| Glycemic control | Good | 229 | 57.10 |
| Poor | 172 | 42.90 | |
| Diabetics treatment regimen | Oral hypoglycaemic | 280 | 69.80 |
| Insulin | 89 | 22.20 | |
| Both | 32 | 8.00 | |
| Duration of DM (in years) | <6 years | 253 | 63.10 |
| 6+ years | 148 | 36.90 | |
| Complication of DM | Yes | 52 | 12.70 |
| No | 349 | 87.30 | |
| Types of complication of DM | Ophthalmologic | 28 | 53.80 |
| Hypoglycaemic | 21 | 40.40 | |
| Renal | 3 | 5.80 | |
| Co-morbidity | Yes | 74 | 18.40 |
| No | 327 | 81.60 | |
| Types of Co-morbidity with DM | Hypertension | 45 | 60.80 |
| Renal disease | 29 | 39.20 | |
| Previous diagnosis of depression | Yes | 13 | 3.2 |
| No | 388 | 96.8 | |
| Family history of depression | Yes | 49 | 12.00 |
| No | 352 | 88.00 | |
| Relationship of a family member with depression | Mother | 27 | 55.10 |
| Father | 14 | 28.50 | |
| Others | 8 | 16.40 | |
DM: diabetes mellitus.
Self-care practice of the participants
About two-third (62.8%) of the patients had a good self-care practice. The well-attained domain-specific self-care practice was medication adherence (Figure 1).
Figure 1.
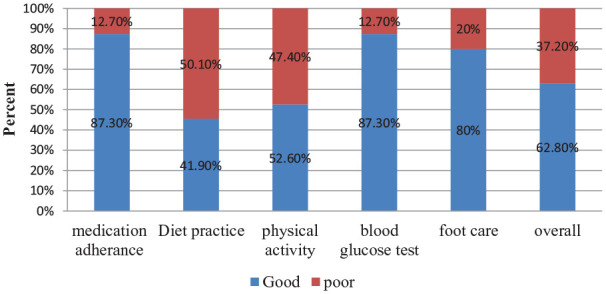
Domain-specific and the overall diabetic self-care activities of diabetic patients attending at public hospitals in Harar, East Ethiopia, 2020.
Psychosocial and substance use behavior of participants
Based on the assessment made on the social support using the OSSS-3, about one-fourth of the patients had a poor level of social support. Concerning the substance use behavior, the median age of starting smoking was 21 years with the inter-quartile range of 33 years (Table 3).
Table 3.
Psychosocial and substance use behavior of diabetic patients attending at public hospitals in Harar, East Ethiopia, 2020.
| Variables | Frequency (n = 401) | Percentage (%) | |
|---|---|---|---|
| Social support | Poor | 96 | 23.90 |
| Moderate | 98 | 24.40 | |
| Strong | 207 | 51.60 | |
| Payment modality to get DM service | Fee waiver | 51 | 12.70 |
| 338 | 84.30 | ||
| Health Insurance | 12 | 3.00 | |
| Ever smokers | Yes | 116 | 28.90 |
| No | 285 | 71.10 | |
| Current smoker | Yes | 63 | 15.70 |
| No | 338 | 84.30 | |
| Ever drink alcohol | Yes | 87 | 21.70 |
| No | 314 | 78.30 | |
| Current alcohol users | Yes | 71 | 17.80 |
| No | 330 | 82.20 | |
| Ever use Khat | Yes | 231 | 57.60 |
| No | 170 | 42.40 | |
| Current Khat users | Yes | 210 | 52.40 |
| No | 191 | 47.60 | |
| Current users of Shisha | Yes | 68 | 17.00 |
| No | 333 | 83.00 | |
| Ever use illicit drugs (cocaine, amphetamine, marijuana) | Yes | 46 | 11.50 |
| No | 355 | 88.50 | |
DM: diabetes mellitus.
Prevalence and levels of depression among diabetic patients
The overall prevalence of depression was 48.9% (95% CI: 44.2, 53.4); of whom, 80 (40.8%) had mild depression, 41 (20.92%) had moderate depression, 55 (28.1%) had moderately severe depression, and 20 (10.2%) had severe depression.
Factors associated with depression among diabetic patients
Binary logistic regression was fitted to identify factors associated with depression. Accordingly, after adjusting for confounding factors having p value < 0.05 on bivariate analysis, the final multivariate analysis of depression revealed that; being female (AOR = 1.50, 95% CI: 1.39, 2.73), Khat chewing (AOR = 1.88, 95% CI: 1.22, 2.93), having poor and moderate social support (AOR = 1.79, 95% CI: 1.07, 2.98 and AOR = 1.90, 95% CI: 1.14, 3.17 respectively), taking both insulin and hypoglycemic agent (AOR = 1.33, 95% CI: 1.13, 2.80), and having the illness for more than 6 years (AOR = 5.40, 95% CI: 3.42, 8.14) remained statistically significant with depression (Table 4).
Table 4.
Factors associated with depression among diabetic outpatients attending at public hospitals in Harar, East Ethiopia, 2020.
| Variables | Depression | OR (95% CI) | |||
|---|---|---|---|---|---|
| Yes | No | COR (95% CI) | AOR (95% CI) | ||
| Sex | Female | 108 | 96 | 1.39 (1.94, 2.06) | 1.50 (1.39, 2.73)* |
| Male | 88 | 109 | 1 | 1 | |
| DM complication | Yes | 31 | 20 | 1.74 (1.95, 3.17) | 1.78 (0.83, 3.83) |
| No | 165 | 185 | 1 | 1 | |
| Treatment regime | Oral | 140 | 140 | 1 | 1 |
| Insulin | 46 | 43 | 1.07 (0.66, 0.87) | 1.08 (0.64, 1.83) | |
| Both | 10 | 22 | 0.46 (0.21, 0.99) | 1.33 (1.13, 2.80)* | |
| Duration of the illness | <6 years | 137 | 136 | 1 | 1 |
| 6+ years | 59 | 89 | 1.78 (1.18, 2.67) | 5.40 (3.42, 8.14)* | |
| Presence of co-morbidity | Yes | 46 | 27 | 2.02 (1.20, 3.41) | 1.52 (0.4, 3.14) |
| No | 150 | 178 | 1 | 1 | |
| Currently using Khat | Yes | 122 | 88 | 2.19 (1.47, 3.27) | 1.88 (1.22, 2.93)* |
| No | 74 | 117 | 1 | 1 | |
| Social support | Poor | 55 | 41 | 1.85 (1.13, 3.02) | 1.79 (1.07, 2.98)* |
| Moderate | 54 | 44 | 1.69 (1.04, 2.75) | 1.90 (1.14, 3.17)* | |
| Strong | 87 | 120 | 1 | 1 | |
OR: odds ratio; CI: confidence interval; COR: crude odds ratio; AOR: adjusted odds ratio; DM: diabetes mellitus.
Note: *Significant association at p value < 0.05.
Discussion
This study revealed 48.9% of diabetic outpatients have developed some level of depression. This result was similar with studies conducted in other parts of the country (Ambo general Hospital 47%, 42 Addis Ababa black lion hospital 47%, 43 and Felege Hiwot referral hospital 40%), 36 Saudi Arabia (49.6%), 44 and Pakistan (43.5%). 45
On the contrary, the result of this study was relatively higher than a studies done in Malaysia (12.3%), 46 Bangladesh (28.3%), 47 Guinea (34.4%), 17 Uganda (34.8%), 48 and Ethiopia (17%). 49 This discrepancy might be due to the variation in socio-economic characteristics, study period, relatively poor health care delivery systems, and using different data collection instruments with varying specificity and sensitivity scale to detect the outcome variable.
But, the finding of this study was lower than other similar studies in Iran (61%), 50 Cameroon (60%), 51 and Tanzania (87%). 45 The likely explanation for this discrepancy might be the variation in sampling size, design (prospective study in Iran), outcome assessment tools (CESD in Cameron), and description of the participants.
Female diabetic outpatients were 1.5 times more likely to develop depression than male diabetic outpatients. This result was consistent with a similar study conducted in Ambo general hospital, Ethiopia. 42 This might be due to cultural discrimination, sexual harassment at the workplace, the sentimental nature of female’s responses to traumatic events, hormonal differences, and managing personal relationships while simultaneously attempting to manage their disease.52–54
In this study, the duration of the illness was also significantly associated with depression. Having diabetes persisting for a long duration increased 5.4 times the odds of having depression. In the same manner, the long duration of the illness has been recognized as an important predictor for depression in studies done in Ambo 42 and Gondar, Ethiopia. 41 The previous study has proven that an increased risk of having complications and health care expenditures with increased duration of DM may prone diabetic patients to develop psychological illnesses. 55
Another important predictor of depression among diabetic patients was the treatment regime; individuals who took both insulin and oral hypoglycemic agent were more likely to develop depression than individuals who took only insulin or oral hypoglycemic agent. This result is in line with the study conducted in Bahirdar, Ethiopia. 36 Depression creates barriers to the management of diabetes, and the presence of behavioral disturbance might be associated with difficulties adhering to the complex self-management of diabetes, both injection and orally, as a result, it creates fear to take two medications at a time.56,57
Depression was also significantly associated with social support. This finding is similar to studies done in Saudi Arabia 58 and Addis Ababa, Ethiopia. 59 Even though the exact mechanism by which social support affects patient adherence is not yet completely understood, social support from family provides patients with practical help and can buffer the stresses of living with illness. This is because poor social support negatively affects self-care and treatment adherence.60,61
In this study, using a Khat was significantly associated with depression. Patients who were chewing a Khat were about 1.9 times more likely to have depression than their counterparts. This result is in agreement with the finding from studies conducted in Muhimbili National Hospital, Tanzania 62 and Jimma, Southwest Ethiopia. 63 This finding could result from the fact that the amphetamine-like psychoactive chemicals found in the khat stimulate the release of monoamine neurotransmitters like dopamine in the limbic area, resulting in reward sensations consequently to depression. 64 Also, it might be due to the fact that patients with depression using a Khat as self-medication which helps in reducing their depressive symptoms. 42
Such a high occurrence of depression has a variety of implications. In the first place, this entity has a profound impact on the quality of life of the patients with chronic diseases, independent of the possibility of being treated. When depression is recognized in a timely manner, it is possible to decrease the intensity of symptoms as well as to prevent new episodes. Diabetes is associated with higher rates of lost work time, disability, and premature mortality. Diabetes and its complications bring about substantial economic loss to people with diabetes and their families and to health systems and national economies through direct medical costs and loss of work and wages.
Limitation of the study
This study has some important limitations that should be kept in mind when interpreting the results. Due to a lack of sophisticated screening tests, diabetes complications addressed in this study were only confirmed by the patient’s subjective response and their chart review. The cross-sectional nature of the study design does not confirm a definitive cause-and-effect relationship. Some variables like duration of illness rely on the patient’s history that might have recalled bias.
Conclusion
This study revealed a relatively high prevalence of depression in diabetic outpatients. A lesser level of social support, taking oral and insulin treatment regimes, longer duration of illness, using Khat, and being female were significantly associated with depression among diabetic outpatients. Based on the findings, diabetic clinics should develop guidelines to detect and manage depression among diabetic patients. Clinicians need to give emphasis to diabetic patients with long duration of the illness and low level of social support. Heath educators should provide continuous health information and education toward raising awareness about substances and early signs and symptoms of depression to be delivered for patients to promoting early detection.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121211066244 for Prevalence and associated factors of depression among diabetic outpatients attending diabetic clinic at public hospitals in Eastern Ethiopia: A cross-sectional study by Mohamed Ebrahim, Dawit Tamiru, Behailu Hawulte and Tadesse Misgana in SAGE Open Medicine
Acknowledgments
The authors thank Haramaya University for ethical approval. The authors would like to extend their gratitude to the Hiwot Fana Specialized University Hospital and Jugal hospital Diabetic Clinic, and the staff working there for facilitating the research work to happen. The authors would also like to thank data collectors and study participants.
Footnotes
Author contributions: M.E. and B.H. conceived and designed the study. M.E., D.T., B.H, and T.M. adopted data collection instrument and acquisition of data. M.E., D.T., B.H, and T.M. carried out the data management. M.E. and B.H. analyzed the data and interpreted findings. M.E., D.T., B.H, and T.M. drafted the manuscript and performed the critical revision and approval of the final manuscript.
Data availability: The data used to support the findings of this study are available from the corresponding author upon request.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval: Ethical approval for this study was obtained from the Institutional Health Research Ethics Review Committee (IHRERC) of the College of Health and Medical Sciences, Haramaya University (IHRERC/120/2020).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from all subjects before the study.
ORCID iDs: Dawit Tamiru  https://orcid.org/0000-0002-0201-8138
https://orcid.org/0000-0002-0201-8138
Behailu Hawulte  https://orcid.org/0000-0001-6023-7542
https://orcid.org/0000-0001-6023-7542
Tadesse Misgana  https://orcid.org/0000-0002-5022-1915
https://orcid.org/0000-0002-5022-1915
Supplemental material: Supplemental material for this article is available online.
References
- 1. Beusenberg M, Orley JH. World Health Organization. A user’s guide to the self reporting questionnaire. Geneva: World Health Organization, 1994. [Google Scholar]
- 2. World Health Organization. Definition, diagnosis and classification of diabetes mellitus and its complication. Geneva: World Health Organization, 1999. [Google Scholar]
- 3. World Health Organization. Guidelines on second- and third-line medicines and type of insulin for the control of blood glucose levels in non-pregnant adults with diabetes mellitus. Geneva: World Health Organization, 2018. [PubMed] [Google Scholar]
- 4. Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract 2019; 157: 107843. [DOI] [PubMed] [Google Scholar]
- 5. NCD Risk Factor Collaboration (NCD-RisC). Effects of diabetes definition on global surveillance of diabetes prevalence and diagnosis: a pooled analysis of 96 population-based studies with 331,288 participants. Lancet Diabetes Endocrinol 2015; 3(8): 624–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nitin J, Bhaskaran U, Raghavendra Babu MA, et al. The global burden of disease. Indian J Endicronol Metab 2013; 17(4): 681–688. [Google Scholar]
- 7. Bajwa SJ, Bajwa S, Saroha R. Psychosocial concerns among patients with diabetes attending the preanesthetic and pain clinic. J Soc Health Diabetes 2015; 3(2): 72. [Google Scholar]
- 8. Lunghi C, Zongo A, Moisan J, et al. The impact of incident depression on medication adherence in patients with type 2 diabetes. Diabetes Metab 2017; 43(6): 521–528. [DOI] [PubMed] [Google Scholar]
- 9. Khamseh ME, Baradaran HR, Rajabali H. Depression and diabetes in Iranian patients: a comparative study. Int J Psychiatry Med 2017; 37: 81–86. [DOI] [PubMed] [Google Scholar]
- 10. Mikaliukstiene A, Zagminas K, Juozulynas A, et al. Prevalence and determinants of anxiety and depression symptoms in patients with type 2 diabetes in Lithuania. Med Sci Monit 2014; 20: 182–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wild S, Bchir M, Roglic G, et al. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004; 27: 1047–1053. [DOI] [PubMed] [Google Scholar]
- 12. Gebre MW. Diabetes mellitus and associated diseases from Ethiopian perspective: systematic review. Ethiop J Health Dev 2013; 3: 249–253. [Google Scholar]
- 13. Teshome HM, Ayalew GD, Shiferaw FW, et al. The prevalence of depression among diabetic patients in Ethiopia: a systematic review and meta-analysis, 2018. Depress Res Treat 2018; 2018: 6135460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Katon W, von Korff M, Ciechanowski P, et al. Behavioral and clinical factors associated with depression among individuals with diabetes. Diabetes Care 2004; 27(4): 914–920. [DOI] [PubMed] [Google Scholar]
- 15. Katon WJ, Simon G, Russo J, et al. Quality of depression care in a population-based sample of patients with diabetes and major depression. Med Care 2004; 42(12): 1222–1229. [DOI] [PubMed] [Google Scholar]
- 16. Engum A, Mykletun A, Midthjell K, et al. Depression and diabetes: a large population-based study of sociodemographic, lifestyle, and clinical factors associated with depression in type 1 and type 2 diabetes. Diabetes Care 2005; 28(8): 1904–1909. [DOI] [PubMed] [Google Scholar]
- 17. Camara A, Baldé NM, Enoru S, et al. Prevalence of anxiety and depression among diabetic African patients in Guinea: association with HbA1c levels. Diabetes Metab 2015; 41(1): 62–68. [DOI] [PubMed] [Google Scholar]
- 18. Lloyd C, Dyer P, Barnett AH. Prevalence of symptoms of depression and anxiety in a diabetes clinic population. Diabet Med 2000; 17(3): 198–202. [DOI] [PubMed] [Google Scholar]
- 19. Peyrot M, Rubin RR. Levels and risks of depression and anxiety symptomatology among diabetic adults. Diabetes Care 1997; 20(4): 585–590. [DOI] [PubMed] [Google Scholar]
- 20. Mosaku K, Kolawole B, Mume C, et al. Depression, anxiety and quality of life among diabetic patients: a comparative study. J Natl Med Assoc 2008; 100(1): 73–78. [DOI] [PubMed] [Google Scholar]
- 21. Black SA. Increased health burden associated with comorbid depression in older diabetic Mexican Americans. Results from the hispanic established population for the epidemiologic study of the elderly survey. Diabetes Care 1999; 22(1): 56–64. [DOI] [PubMed] [Google Scholar]
- 22. Miyaoka Y, Miyaoka H, Motomiya T, et al. Impact of sociodemographic and diabetes-related characteristics on depressive state among non-insulin-dependent diabetic patients. Psychiatry Clin Neurosci 1997; 51(4): 203–206. [DOI] [PubMed] [Google Scholar]
- 23. Al-Amer RM, Sobeh MM, Zayed AA, et al. Depression among adults with diabetes in Jordan: risk factors and relationship to blood sugar control. J Diabetes Complicat 2011; 25(4): 247–252. [DOI] [PubMed] [Google Scholar]
- 24. Sevincok L, Guney E, Uslu A, et al. Depression in a sample of Turkish type 2 diabetes patients. Eur Psychiatry 2001; 16(4): 229–231. [DOI] [PubMed] [Google Scholar]
- 25. Arambewela MH, Somasundaram NP, Jayasekara H, et al. Prevalence of depression and associated factors among patients with type 2 diabetes attending the diabetic clinic at a Tertiary Care Hospital in Sri Lanka: a descriptive study. Psychiatry J 2019; 2019: 7468363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ell K, Katon W, Cabassa LJ, et al. Depression and diabetes among low-income Hispanics: design elements of a socioculturally adapted collaborative care model randomized controlled trial. Int J Psychiatry Med 2009; 39: 113–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Knychala MA, Jorge ML, Muniz CK, et al. High-risk alcohol use and anxiety and depression symptoms in adolescents and adults with type 1 diabetes mellitus: a cross-sectional study. Diabetol Metab Syndr 2015; 7: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sunny AK, Khanal VK, Sah RB, et al. Depression among people living with type 2 diabetes in an urbanizing community of Nepal. PLoS One 2019; 14(6): e0218119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Farooqi A, Snoek F, Khunti K. Management of chronic cardiometabolic conditions and mental health during COVID-19. Prim Care Diabetes 2021; 15(1): 21–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ismail K, Moulton CD, Winkley K, et al. The association of depressive symptoms and diabetes distress with glycaemic control and diabetes complications over 2 years in newly diagnosed type 2 diabetes: a prospective cohort study. Diabetologia 2017; 60(10): 2092–2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lunghi C, Zongo A, Tardif I, et al. Depression but not non-persistence to antidiabetic drugs is associated with mortality in type 2 diabetes: a nested case-control study. Diabetes Res Clin Pract 2021; 171: 108566. [DOI] [PubMed] [Google Scholar]
- 32. Baumeister H, Hutter N, Bengel J. Psychological and pharmacological interventions for depression in patients with diabetes mellitus: an abridged Cochrane review. Diabet Med 2014; 31: 773–786. [DOI] [PubMed] [Google Scholar]
- 33. Mukeshimana M, Mchunu G. Management of co-morbidity of depression and chronic non-communicable diseases in Rwanda. Ethiop J Health Sci 2017; 27(1): 17–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. World Health Organization. Integrating the response to mental disorders and other chronic diseases in health care systems. Geneva: World Health Organization, 2014. [Google Scholar]
- 35. Office of the Population Census Commission. Population and housing census of Ethiopia. Addis Ababa: Office of the Population Census Commission, 2007. [Google Scholar]
- 36. Teshager A, Giorgis B. Prevalence of depression and associated factors among adult diabetic patients attending Outpatient Department, at Felege Hiwot Referral Hospital, Bahir Dar, Northwest Ethiopia. Med Sci Monit 2016; 6: 264–276. [Google Scholar]
- 37. Katon WJ, Rutter C, Simon G, et al. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care 2015; 28: 2668–2672. [DOI] [PubMed] [Google Scholar]
- 38. Dalgard OS, Dowrick C, Lehtinen V, et al. Negative life events, social support and gender difference in depression. Soc Psychiatry Psychiatr Epidemiol. 2006; 41(6): 444–451. [DOI] [PubMed] [Google Scholar]
- 39. Guthold R, Louazani SA, Riley LM, et al. Physical activity in 22 African countries: results from the World Health Organization STEPwise approach to chronic disease risk factor surveillance. Am J Prev Med 2011; 41(1): 52–60. [DOI] [PubMed] [Google Scholar]
- 40. Necho M, Mekonnen S, Haile K, et al. Suicidal plan, attempt, and associated factors among patients with diabetes in Felegehiwot Referral Hospital, Bahirdar, Ethiopia: cross-sectional study. BMC Psychiatry 2019; 19: 258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Birhanu AM, Alemu FM, Ashenafie TD, et al. Depression in diabetic patients attending University of Gondar Hospital Diabetic Clinic, Northwest Ethiopia. Diabetes Metab Syndr Obes 2016; 9: 155–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Tiki T. Prevalence and associated factors of depression among type 2 diabetes mellitus patients on follow up at Ambo General Hospital, Oromia Regional state, Ethiopia. J Depress Anxiety 2017; 6(1): 1–5. [Google Scholar]
- 43. Habtewold TD, Radie YT, Sharew NT. Prevalence of depression among type 2 diabetic outpatients in Black Lion General Specialized Hospital, Addis Ababa, Ethiopia. Depress Res Treat 2015; 2015: 184902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. El Mahalli AA. Prevalence and predictors of depression among type 2 diabetes mellitus outpatients in Eastern Province, Saudi Arabia. Int J Health Sci (Qassim) 2015; 9(2): 119–126. [PMC free article] [PubMed] [Google Scholar]
- 45. Khan ZD, Lutale J, Moledina SM. Prevalence of depression and associated factors among diabetic patients in an outpatient diabetes clinic. Psychiatry J 2019; 2019: 2083196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Mohamed R, Kadir AA, Yaacob L, et al. A study on depression among patient with type 2 diabetes mellitus in North-Eastcoast Malaysia. Int J Collab Res Intern Med Public Health 2012; 4(8): 1590–1600. [Google Scholar]
- 47. Zahid N, Asghar S, Claussen B, et al. Depression and diabetes in a rural community in Pakistan. Diabetes Res Clin Pract 2011; 79(1): 124–127. [DOI] [PubMed] [Google Scholar]
- 48. Buchowski MS, Aslam M, Dossett C, et al. The association between depression, quality of life, and the health care expenditure of patients with diabetes mellitus in Uganda. J Affect Disord 2015; 174: 7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Mossie TB, Berhe GH, Kahsay GH, et al. Prevalence of depression and associated factors among diabetic patients at Mekelle City, North Ethiopia. Indian J Psychol Med 2017; 39(1): 52–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Azami M, Moslemirad M, Mansouri A, et al. The prevalence of depression in patients with diabetes in Iran. J Babol Univ Med Sci 2017; 19: 16–27. [Google Scholar]
- 51. Hall KK, Tambekou J, Penn L, et al. Association between depression, glycaemic control and the prevalence of diabetic retinopathy in a diabetic population in Cameroon. S Afr J Psychiatr 2017; 23: 983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Noble RE. Depression in women. Metabolism 2005; 54: 49–52. [DOI] [PubMed] [Google Scholar]
- 53. Brommelhoff JA, Conway K, Merikangas K, et al. Higher rates of depression in women: role of gender bias within the family. J Womens Health (Larchmt) 2004; 13(1): 69–76. [DOI] [PubMed] [Google Scholar]
- 54. Paykel ES. Depression in women. Br J Psychiatry 1991; 158: 22–29. [PubMed] [Google Scholar]
- 55. Getinet alemu W, Malefiya YD, Boru Bifftu B. Mental distress among patients admitted in Gondar University Hospital: a cross sectional institution based study. Health Sci J 2017; 10: 480. [Google Scholar]
- 56. Coventry PA, Hays R, Dickens C, et al. Talking about depression: a qualitative study of barriers to managing depression in people with long term conditions in primary care. BMC Fam Pract 2011; 12: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Lunghi C, Moisan J, Grégoire J-P, et al. The association between depression and medication nonpersistence in new users of antidiabetic drugs. Value Health 2017; 20(6): 728–735. [DOI] [PubMed] [Google Scholar]
- 58. Madkhali J, Hakami A, Dallak A, et al. Prevalence and associated factors of depression among patients with diabetes at Jazan Province, Saudi Arabia: a cross-sectional study. Psychiatry J 2019; 2019: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Habtewold TD, Alemu SM, Haile YG. Sociodemographic, clinical, and psychosocial factors associated with depression among type 2 diabetic outpatients in Black Lion General Specialized Hospital, Addis Ababa, Ethiopia: a cross-sectional study. BMC Psychiatry 2016; 16(1): 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Miller TA, Dimatteo MR. Importance of family/social support and impact on adherence to diabetic therapy. Diabetes Metab Syndr Obes 2013; 6: 421–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Song Y, Song HJ, Han HR, et al. Unmet needs for social support and effects on diabetes self-care activities in Korean Americans with type 2 diabetes. Diabetes Educ 2012; 38(1): 77–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Khan ZD. Prevalence of depression and associated factors among diabetic patients in an outpatient diabetes clinic. Psyciatry J 2019; 2019: 650–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Mossie A, Kindu D, Negash A. Prevalence and severity of depression and its association with substance use in Jimma Town, Southwest Ethiopia. Depress Res Treat 2016; 2016: 3460462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Bahari R. The psychological impact of diabetic limb problems. Int Med J Malays 2015; 14(2): 3–7. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121211066244 for Prevalence and associated factors of depression among diabetic outpatients attending diabetic clinic at public hospitals in Eastern Ethiopia: A cross-sectional study by Mohamed Ebrahim, Dawit Tamiru, Behailu Hawulte and Tadesse Misgana in SAGE Open Medicine


