Abstract
Background/Objective:
Previous clinical trials have documented that soy protein reduces low-density lipoprotein cholesterol and increases high-density lipoprotein (HDL) cholesterol compared with milk protein. However, the effect of soy protein on lipids compared with carbohydrate has not been not well studied. We examined the effect of soy and milk protein supplementation on lipids and lipoproteins compared with carbohydrate among adults without hypercholesterolemia.
Subjects/Methods:
We conducted a randomized, double-blind, 3-phase crossover trial among 352 US adults with serum total cholesterol level of <240 mg/dl from September 2003 to April 2008. Trial participants were assigned to 40 g/day supplementation of soy protein, milk protein or complex carbohydrate from wheat each for 8 weeks in random order with a 3-week washout period between interventions. Overnight fasting blood samples were collected at the termination of each intervention phase.
Results:
Compared with carbohydrate, soy protein supplementation was significantly associated with a net change (95% confidence interval (CI)) in total cholesterol and total/HDL cholesterol ratio of −3.97 mg/dl (−7.63 to −0.31, P=0.03) and −0.12 (−0.23 to −0.01, P=0.03), respectively. Compared with milk protein, soy protein supplementation was significantly associated with a net change (95% CI) in HDL and total/HDL cholesterol ratio of 1.54 mg/dl (0.63 to 2.44, P=0.0009) and −0.14 (−0.22 to −0.05, P=0.001), respectively. Compared with carbohydrate, milk protein supplementation was significantly associated with a net change (95% CI) in HDL of −1.13 mg/dl (−2.05 to −0.22, P=0.02).
Conclusions:
This randomized controlled trial indicates that soy protein, but not milk protein, supplementation improves the lipid profile among healthy individuals.
Keywords: soybean proteins, milk proteins, carbohydrates, cholesterol, lipids
Introduction
Cardiovascular disease (CVD) is a major public health problem, with an estimated one in three American adults having one or more types of CVD (Roger et al., 2011). Observational studies have indicated that dyslipidemia is a modifiable risk factor for CVD (Wilson et al., 1997; Stamler et al., 2000; Sharrett et al., 2001; Greenland et al., 2003). Clinical trials have documented that lowering blood lipids reduces risk of coronary heart disease and stroke (LaRosa et al., 1999; De Caterina et al., 2010). According to the most recent statistics, 44.4% of the US population have borderline-high or higher total cholesterol (⩾200 mg/dl, ⩾5.2 mmol/l) and 31.9% have borderline-high or higher low-density lipoprotein (LDL) cholesterol (⩾130 mg/dl, ⩾3.4 mmol/l) (Roger et al., 2011). The National Cholesterol Education Program emphasizes the importance of therapeutic lifestyle changes for primary prevention, including dietary modification, body weight reduction and increased physical activity (Grundy et al., 2004). Improvement of overall lipid profile is an important public health and clinical goal for reducing the burden of CVD and its associated economic impact on the US health care system.
Clinical studies of soy protein have reported findings that vary with respect to the magnitude of serum lipids reduction (Anderson et al., 1995; Reynolds et al., 2006; Sacks et al., 2006). In a meta-analysis of 38 clinical studies, Anderson et al., 1995 reported that soy protein intake (averaged 47 g/day) was associated with significant reduction in total cholesterol, LDL cholesterol and triglycerides of 23.2 mg/dl (0.6 mmol/l), 21.7 mg/dl (0.6 mmol/l) and 13.3 mg/dl (0.2 mmol/l), respectively, and a nonsignificant increase in high-density lipoprotein (HDL) cholesterol of 1.2 mg/dl (0.03 mmol/l). In a recent meta-analysis of 41 randomized controlled trials, Reynolds et al. (2006) reported a much smaller effect of isolated soy protein supplementation on lipids: a significant reduction in total cholesterol of 5.26 mg/dl (0.14 mmol/l), LDL cholesterol of 4.25 mg/dl (0.11 mmol/l) and triglycerides of 6.26 mg/dl (0.07 mmol/l), and a significant increase in HDL cholesterol of 0.77 mg/dl (0.02 mmol/l). In the American Heart Association Science Advisory that assessed 22 randomized trials of soy protein, the committee reported a modest average reduction in LDL cholesterol of about 3% and no significant effect on HDL cholesterol, triglycerides or lipoprotein(a) (Sacks et al., 2006). However, most of these studies used milk protein supplementation as control and were conducted in patients with hypercholesterolemia or postmenopausal women (Anderson et al., 1995; Reynolds et al., 2006; Sacks et al., 2006). In this study, we compare the effects of soy protein, milk protein and complex carbohydrate supplementations on serum lipids and lipoproteins in a randomized controlled crossover trial among men and women aged 22 years and older without hypercholesterolemia.
Subjects and methods
Study design
The Protein and Blood Pressure Study was a randomized, double-blinded and placebo-controlled trial designed primarily to test whether a soy protein or milk protein supplementation would reduce systolic blood pressure (BP) compared with a complex carbohydrate and secondarily to assess the impact of these supplements on serum lipids and lipoproteins (He et al., 2011). The Protein and Blood Pressure study utilized a 3-phase crossover study design. Following a 2-week run-in period, eligible participants were allocated to receive 40 g of soy protein per day, 40 g of milk protein per day and 40 g of complex carbohydrate placebo per day in a random order, each for 8 weeks. During the run-in period, study participants received 40 g of complex carbohydrate supplement. During each of the three 8-week phases, participants were seen at two study visits at the beginning and another two study visits at the termination of the phase. A 3-week washout period was implemented between each intervention period. Participant recruitment and the intervention occurred between September 2003 and April 2008.
Written informed consent was obtained from each participant before the initial screening visit and before randomization. The Institutional Review Boards at the Tulane University Health Sciences Center and the University of Mississippi Medical Center approved the study protocol.
Study participants
The study participants were men and women aged 22 years or older who had a mean systolic BP from 120 to 159 mm Hg and a diastolic BP from 80 to 95 mm Hg, based on six readings at two screening visits. Persons with a systolic BP ⩾160 mm Hg or a diastolic BP ⩾95 mm Hg or that were taking antihypertensive medications were excluded. In addition, persons with a self-reported history of clinical CVD, cancer, chronic kidney disease (or a serum creatinine ⩾1.7 mg/dl (⩾150.3 μmol/l) for men and ⩾1.5 mg/dl (⩾132.6 μmol/l) for women), hypercholesterolemia (or serum total cholesterol ⩾240 mg/dl (⩾6.2 mmol/l)), diabetes (or serum glucose ⩾126 mg/dl (⩾7.0 mmol/l)), body mass index ⩾40 kg/m2 or consumption of > 14 drinks of alcoholic beverages per week were excluded. Persons who consumed dietary protein ⩾1.63 g/kg/day (85th percentile of dietary protein intake in the US general population) based on two 24-hour dietary recalls were also excluded. Women who were pregnant or who intended to become pregnant during the study were excluded.
Study participants were recruited by mass mailing and work-site and community-based screenings in New Orleans, Louisiana and Jackson, Mississippi. We invited 1626 persons to the study clinics for screening visits and 391 persons met all eligibility criteria (Figure 1). Among those who met inclusion criteria, 352 successfully completed a 2-week run-in (intake of ⩾85% supplements) and were randomized to the intervention.
Figure 1.
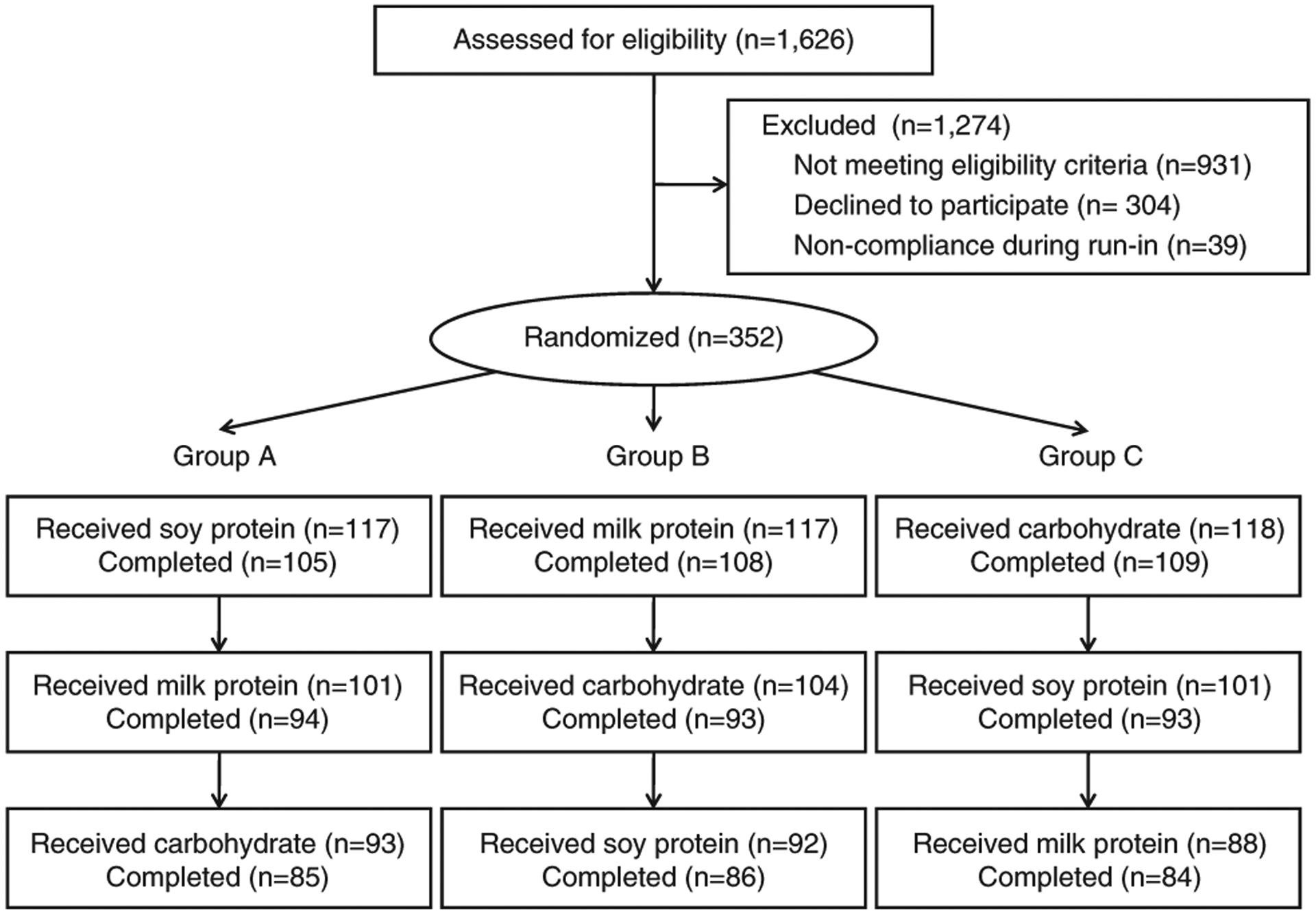
Flow diagram of participants in the Protein and Blood Pressure Study.
Intervention
The study participants were randomly assigned to three sequences at a fixed 1:1:1 allocation ratio: those who were assigned to sequence A received 40 g of soy protein for 8 weeks, then 40 g of milk protein for 8 weeks and finally 40 g of complex carbohydrate for 8 weeks; those who were assigned to sequence B first received milk protein, then carbohydrate and finally soy protein; and those who were assigned to sequence C first received carbohydrate, then soy protein and finally milk protein. The randomization was stratified by clinic site, gender and hypertension status and used a block size of six. The randomization assignment was conducted centrally at the Data Coordinating Unit at Tulane University. The randomization assignment list was generated by a computer program, which could only be accessed by the data coordinator. All other research personnel, including clinical coordinators and laboratory technicians, and the study participants were unaware of treatment assignment.
The soy protein, milk protein and complex carbohydrate supplements were provided for the Protein and Blood Pressure study by Solae, LLC (St Louis, Missouri, MO, USA). The nutrient composition of the supplements is provided in Table 1. The complex carbohydrates were from wheat, which consisted of 90.6% maltodextrin, 4.7% sucrose and 4.7% fructose. The caloric content and amount of fat was similar in the soy protein, milk protein and complex carbohydrate supplements. The milk protein supplements contained a small amount of cholesterol, which was not present in the other supplements. The glycemic index varied among the supplements, with the lowest index in the soy protein supplement and the highest index in the carbohydrate supplement. The soy protein, milk protein and complex carbohydrate powders looked the same and were provided to study participants in identical packets. The study participants were instructed to take the supplements twice per day; once in the morning and once in the evening in water or juice. Based on the participants’ two 24-hour dietary recalls during screening visits, individualized recommendations were given in order for participants’ total energy intake to remain consistent over the supplementation periods; for example, protein and carbohydrate supplement was recommended to partially replace breakfast, snack or supper based on participants’ dietary habits. The study participants returned unconsumed packets at follow-up clinic visits. The study coordinator counted the number of returned packets, and we used this information to assess participants’ adherence to the assigned intervention.
Table 1.
Nutrient composition of soy protein, milk protein and complex carbohydrate supplements, per daya
| Soy protein | Milk protein | Carbohydrate | |
|---|---|---|---|
| Energy (kcal) | 200 | 200 | 200 |
| Protein (g) | 40 | 40 | 0.4 |
| Carbohydrate (g) | 8 | 10 | 50 |
| Fat (g) | 1.2 | 0.2 | 0 |
| Saturated fat (g) | 0 | 0 | 0 |
| Cholesterol (mg) | 0 | 10 | 0 |
| Isoflavones (mg) | 84 | 0 | 0 |
| Glycemic index | 47.7 | 67.2 | 98.9 |
Nutrient composition of soy protein, milk protein and complex carbohydrate supplements was provided by Solae, LLC, St Louis, MO, USA.
Measurements
Study participants were instructed to fast for 10 h before their clinic visits for blood sample collection. Blood samples were promptly centrifuged at 3000 g for 10 min at 4 °C. Serum and plasma were separated and aliquoted for different analyses at the clinical laboratory. The samples for lipoprotein analysis were kept at 4 °C in the laboratory. Serum total cholesterol and triglycerides were measured by enzymatic procedures (Hitachi 902 Chemistry Analyzer, Roche Diagnostics, Indianapolis, IN, USA). Serum HDL was quantified by a combined procedure of heparin-calcium precipitation of apo-B-containing lipoproteins and agar-agarose gel electrophoresis of lipoproteins (Srinivasan and Berenson, 1983). Serum LDL cholesterol was calculated using the Friedewald equation for individuals with serum triglyceride <400 mg/dl (4.5 mmol/l) (Friedewald et al., 1972).
At the baseline and termination visits during each intervention/control phase, three BP readings were measured using the Hawksley random-zero sphygmomanometer by trained and certified observers who were masked to group assignment. Body weight, height and waist circumference were measured by trained staff using a standard protocol and body mass index was calculated as kg/m2. Two 24-hour dietary recalls were conducted at the screening visits and at the termination visits during each intervention/control phase. Computer software was used to conduct 24-hour dietary recalls and calculate nutrient intakes (Minnesota Nutrition Data System for Research, University of Minnesota, 2002). An overnight timed urine sample was collected at the baseline and termination visits to measure urinary excretion of sodium, potassium, urea nitrogen and creatinine. Side effects and compliance were assessed using a questionnaire, packet counts and self-reported supplement calendar report.
Statistical analysis
The primary outcome of interest was the difference in serum lipid levels (total cholesterol, LDL, HDL, triglycerides and total cholesterol to HDL ratio) among the three intervention phases. A mixed effects model was used to compare the effects of soy protein, milk protein and complex carbohydrate on serum lipid levels, in which participants and period were assumed to be random effects and treatment and sequence were assumed to be estimable fixed effects. PROC MIXED of SAS version 9.2 (SAS Institute Inc., Cary, NC, USA) was used to obtain point estimates and standard errors of the treatment and sequence effects and to test for differences between treatments. We examined the effect of period by testing its interaction with treatment and the interaction was not statistically significant. First-order carryover and sequence were also not statistically significant for any of the outcome measures. We used an autoregressive correlation structure to account for repeated measures in the crossover study design. The intention-to-treat principle was used for all primary analyses.
Results
Of these 352 study participants, 322 (91.5%) completed the first phase, 280 (79.5%) completed the second phase and 255 (72.4%) completed the third phase (Figure 1). Follow-up rates were similar according to intervention (80.7% in soy protein supplementation phase, 81.3% in milk protein supplementation phase and 81.5% in carbohydrate supplementation phase). Based on returned packet counts and supplement calendar report, the study participants who completed the supplementation intervention consumed over 85% of their supplements during the corresponding intervention phase.
Baseline characteristics of the study population are presented according to randomization sequence in Table 2. Baseline characteristics were generally evenly distributed across randomization sequence. For the overall study population, the mean (s.d.) lipids level at baseline were 194.2 (31.4) mg/dl (5.0 (0.8) mmol/l) for total cholesterol, 117.4 (28.9) mg/dl (3.0 (0.7) mmol/l) for LDL, 52.3 (14.5) mg/dl (1.4 (0.4) mmol/l) for HDL and 120.6 (64.4) mg/dl (1.4 (0.7) mmol/l) for triglycerides.
Table 2.
Baseline characteristicsa of 352 trial participants
| Randomization groups | |||
|---|---|---|---|
| A (n = 117) | B (n = 117) | C (n = 118) | |
| Age (years) | 48.4 (11.5) | 46.7 (10.7) | 48.1 (8.7) |
| Male (%) | 59.0 | 58.1 | 57.6 |
| African-American (%) | 33.3 | 32.5 | 37.3 |
| Some college education (%) | 92.3 | 89.7 | 86.4 |
| Current smoking (%) | 5.1 | 11.1 | 5.1 |
| Alcohol drinking (%) | 39.3 | 48.7 | 48.3 |
| Physical activity ⩾3 times/week (%) | 56.9 | 55.7 | 58.8 |
| Body mass index (kg/m2) | 29.0 (4.5) | 29.5 (4.5) | 29.3 (4.6) |
| Systolic blood pressure (mmHg) | 127.2 (9.3) | 126.7 (11.0) | 126.1 (9.7) |
| Total cholesterol (mg/dl) | 197.7 (27.7) | 200.0 (26.4) | 194.6 (27.7) |
| High-density lipoprotein (HDL) (mg/dl) | 51.1 (12.4) | 52.6 (15.6) | 53.8 (15.2) |
| Low-density lipoprotein (mg/dl) | 122.5 (27.1) | 123.1 (26.0) | 115.7 (26.3) |
| Triglycerides (mg/dl) | 118.3 (61.2) | 124.5 (67.7) | 119.2 (64.8) |
| Total/HDL cholesterol ratio | 4.0 (1.0) | 4.1 (1.3) | 3.9 (1.2) |
Mean (s.d.) or percentage.
Dietary nutrient intake information is presented according to intervention phase in Table 3. By design, protein and carbohydrate intake varied across interventions with a mean increased protein intake of 30.5 g/day during the soy intervention and 32.8 g/day during the milk protein intervention compared with the carbohydrate intervention, and an increased daily intake of about 30.7 g of carbohydrate during the carbohydrate intervention compared with soy protein and milk protein interventions. The percentage of total energy from protein, carbohydrate and fat, respectively, was 20.8, 45.3 and 33.9% during the soy protein intervention, 21.2, 45.3 and 33.5% during the milk protein intervention and 16.1, 51.9 and 32.9% during the carbohydrate intervention. Daily intake of overall, saturated, polyunsaturated and monounsaturated fat as well as cholesterol and glycemic index was not significant different across intervention phases. Urinary excretion of urea nitrogen but not creatinine was significantly increased in the soy protein and milk protein supplementation phases compared with carbohydrate supplementation phase.
Table 3.
Mean (s.d.) for daily dietary nutrient intake and urinary overnight excretion of urea nitrogen and creatinine according to intervention phase
| Soy protein | Milk protein | Carbohydrate | P-values | |
|---|---|---|---|---|
| Dietary intake | ||||
| Energy (kcal) | 2095.4 (666.1) | 2091.3 (628.4) | 2057.8 (621.0) | 0.80 |
| Protein (g) | 108.4 (31.3) | 110.7 (33.8) | 77.9 (30.8) | <0.0001 |
| Carbohydrate (g) | 236.4 (85.4) | 236.5 (84.4) | 267.1 (88.5) | 0.0002 |
| Fat (g) | 78.7 (35.1) | 77.6 (31.5) | 75.3 (29.9) | 0.56 |
| Saturated fat (g) | 25.3 (12.7) | 25.7 (11.8) | 24.5 (11.5) | 0.56 |
| Polyunsaturated fat (g) | 15.3 (7.6) | 15.5 (6.6) | 15.2 (7.1) | 0.92 |
| Monounsaturated fat (g) | 30.6 (14.7) | 29.6 (13.2) | 29.2 (12.1) | 0.57 |
| Cholesterol (mg) | 289.1 (173.6) | 301.2 (183.0) | 282.0 (182.3) | 0.55 |
| Glycemic index | 60.8 (5.7) | 60.6 (5.3) | 61.5 (5.6) | 0.25 |
| Urinary excretion | ||||
| Urea nitrogen (mg/8h) | 443.6 (276.5) | 467.5 (258.6) | 356.8 (194.4) | < 0.0001 |
| Creatinine (mg/8h) | 40.1 (30.1) | 41.0 (29.5) | 40.9 (28.4) | 0.95 |
The mean levels of serum lipids according to intervention phase and the net change in lipid levels for all three comparisons are presented in Table 4. Compared with carbohydrate supplementation, soy protein supplementation significantly reduced total cholesterol by 3.97 mg/dl (95% confidence interval (CI), −7.63 to −0.31; P=0.03) (−0.10 mmol/l (95% CI, −0.20 to −0.01)) and total/HDL cholesterol ratio by 0.12 (95% CI, −0.23 to −0.01; P=0.03), and borderline significantly reduced LDL by 3.03 mg/dl (95% CI, −6.29 to 0.22; P=0.07) (−0.08 mmol/l (95% CI, −0.16 to 0.01)) and triglycerides by 8.63 mg/dl (95% CI, −18.46 to 1.19; P=0.08) ((−0.10 mmol/l (95% CI, −0.21 to 0.01)). Compared with milk protein supplementation, soy protein supplementation significantly increased HDL by 1.54 mg/dl (95% CI, 0.63 to 2.44; P=0.0009) (0.04 mmol/l (95% CI, 0.02 to 0.06)) and reduced total/HDL cholesterol ratio by 0.14 (95% CI, −0.22 to −0.05; P=0.001), and borderline significantly reduced LDL by 2.45 mg/dl (95% CI, −4.95 to 0.04; P=0.05) (−0.06 mmol/l (95% CI, −0.13 to 0.001)). Compared with carbohydrate supplementation, milk protein supplementation significantly reduced HDL by 1.13 mg/dl (95% CI, −2.05 to −0.22, P=0.02) (−0.03 mmol/l (95% CI, −0.05 to −0.01)), and borderline significantly reduced total cholesterol by 2.56 mg/dl (95% CI, −5.40 to 0.28; P=0.08) (−0.07 mmol/l (95% CI, −0.14 to 0.01)).
Table 4.
Mean serum lipids and lipoproteins at the termination of each intervention phase and net changes by comparison phases
| Mean (95% confidence interval) at the termination of each intervention phase | Net change (95% confidence interval) and P-value by comparison phases | |||||
|---|---|---|---|---|---|---|
| Soy protein | Milk protein | Carbohydrate | Soy protein vs carbohydrate | Milk protein vs carbohydrate | Soy protein vs milk protein | |
| Total cholesterol (mg/dl) | 192.25 (188.68, 195.81) | 193.66 (190.12, 197.19) | 196.22 (192.66, 199.78) | −3.97 (−7.63, −0.31) | −2.56 (−5.40, 0.28) | −1.41 (−4.24, 1.42) |
| 0.03 | 0.08 | 0.33 | ||||
| HDL (mg/dl) | 52.90 (51.27, 54.52) | 51.36 (49.74, 52.98) | 52.49 (50.86, 54.12) | 0.40 (−0.82, 1.63) | −1.13 (−2.05, −0.22) | 1.54 (0.63, 2.44) |
| 0.52 | 0.02 | 0.0009 | ||||
| LDL (mg/dl) | 115.52 (112.20, 118.84) | 117.97 (114.68, 121.26) | 118.55 (115.22, 121.88) | −3.03 (−6.29, 0.22) | −0.58 (−3.10, 1.94) | −2.45 (−4.95, 0.04) |
| 0.07 | 0.65 | 0.05 | ||||
| Triglycerides (mg/dl) | 118.68 (110.06, 127.30) | 122.55 (114.01, 131.09) | 127.31 (118.68, 135.94) | −8.63 (−18.46, 1.19) | −4.76 (−12.62, 3.09) | −3.87 (−11.69, 3.95) |
| 0.08 | 0.23 | 0.33 | ||||
| Total/HDL cholesterol ratio | 3.87 (3.74, 4.01) | 4.01 (3.88, 4.14) | 4.00 (3.87, 4.13) | −0.12 (−0.23, −0.01) | 0.01 (−0.07, 0.10) | −0.14 (−0.22, −0.05) |
| 0.03 | 0.76 | 0.001 | ||||
Abbreviations: HDL, high-density lipoprotein; LDL, low-density lipoprotein.
Discussion
This randomized controlled trial indicates that, compared with carbohydrate intake, soy protein supplementation reduces total cholesterol and total/HDL cholesterol ratio among individuals without hypercholesterolemia. In addition, compared with milk protein, soy protein supplementation increased HDL and reduced total/HDL cholesterol ratio. On the other hand, milk protein might reduce HDL cholesterol compared with carbohydrate. These study findings contribute significantly to our understanding of the relationship between dietary protein intake and lipid levels and have important public health and clinical implications.
Our study is the first randomized controlled trial to compare the effects of soy protein, milk protein and complex carbohydrate on serum lipids. There is increasing evidence that consumption of soy protein in place of animal protein lowers blood cholesterol levels and may provide other cardiovascular benefits (Erdman, 2000). Our study provides additional evidence that consumption of soy protein in place of carbohydrate might improve the lipid profile. Animal experiments and clinical studies indicate that hormone replacement therapy has favorable effects on serum lipids and lipoprotein concentrations, antioxidant protection, endothelial function and vascular reactivity (Barrett-Conner and Stuenkel, 1999; Joswig et al., 1999). Soy protein is a rich source of the polyphenolic isoflavones genistein and daidzein. Isoflavones are structurally similar to estradiol and have a high binding affinity for the primary estrogen receptors in the vascular wall, estrogen receptor-α and -β (Kuiper et al., 1998; Hodges et al., 2000; Aavik et al., 2001). Several clinical trials have indicated that isoflavones in soy protein may have an important role in lowering serum lipids (Baum et al., 1998; Crouse et al., 1999; Merz-Demlow et al., 2000; Gardner et al., 2001; Clerici et al., 2007). In addition, epidemiologic studies have documented that the Asian populations who consume soy foods as a dietary staple have a lower incidence of CVD than those who consume a typical Western diet (Beaglehole, 1990; Zhang et al., 2003; Sacks et al., 2006).
In a meta-analysis of clinical studies, Anderson et al. (1995) reported soybean protein intake reduced ~10% of total cholesterol, LDL cholesterol and triglycerides, without significantly affecting HDL cholesterol. However, many clinical studies included in the meta-analysis were not randomized controlled trials. In a more recent meta-analysis of randomized controlled clinical trials, Reynolds et al. (2006) reported that the lipid-lowering effect of soy protein was smaller than previously reported. Our study showed that the effects of soy protein on lipids are moderate. The more conservative magnitude of effect of soy protein on lipid levels in our studies and more recent randomized trials is likely due to the minimization of confounding effect compared with non-randomized clinical studies. Recent randomized controlled trials have well-balanced macro-nutrient profiles between comparison groups thereby estimating the more modest intrinsic effect of soy on lipid levels. In contrast, earlier trials may additionally depict the ability of soy protein to displace saturated fats and cholesterol from animal sources of protein in the overall dietary portfolio and the combined effect of multiple lipid-lowering plant foods and components, which may explain the larger observed effect on lipids (Carroll, 1991; Jenkins et al., 2010). In addition, the previous studies were mostly conducted in patients with elevated serum cholesterol or postmenopausal women (Anderson et al., 1995; Reynolds et al., 2006). Our study is conducted in healthy adults 22 years of age and older without hypercholesterolemia. Finally, when lipid levels from either of the interventions that were being compared were missing, we set the difference equal to zero. As such, our estimates may underestimate the magnitude of effect of soy protein on the lipid profile.
This randomized controlled trial used a 3-phase crossover design. We were able to provide precise measures of effect by enrolling a large number of participants and by reducing between subject variance with the crossover study design. This design also minimized the influence of variations in lifestyle and diet among individual participants. Because this was not a feeding study, we were not able to control participants’ dietary intake. Nonetheless, diet characteristics, aside from the protein and carbohydrate levels, remained constant across intervention periods as evidenced by the average nutrient intake from dietary recalls. In addition, the supplement calendar reports, returned packet counts and urinary excretion of urea nitrogen are objective evidence that participants adhered to the intervention. A prolonged washout period (3 weeks) reduced the carryover effects of intervention. Furthermore, statistical assessment revealed no evidence of carryover in this study. The limitations of this study include the relatively short duration of the intervention and the lack of testing for a dose–response relationship between dietary protein intake and lipid levels. Future studies should test the dose–response relationship between soy protein intake and lipid levels.
Our study suggests that soy protein supplement reduces total cholesterol and total/HDL cholesterol ratio compared with carbohydrate, and increases HDL and reduces total/HDL cholesterol ratio compared with milk protein. The effect of milk protein did not confer a significant favorable effect on any lipid measures compared with carbohydrate. Further randomized controlled trials are warranted to examine the effect of various amounts of soy proteins on lipid levels to recommend a particular optimal level to increase soy protein intake as part of a nutrition intervention strategy for the prevention and treatment of hypercholesterolemia and subsequent CVD.
Acknowledgements
This work was supported by a research grant (R01 HL68057) from the National Heart, Lung and Blood Institute of National Institutes of Health, Bethesda, MD, USA. The study supplements were provided for the study by Solae, LLC (St Louis, MO, USA).
Footnotes
Conflict of interest
The authors declare no conflict of interest.
References
- Aavik E, du Toit D, Myburgh E, Frosen J, Hayry P (2001). Estrogen receptor beta dominates in baboon carotid after endothelial denudation injury. Mol Cell Endocrinol 182, 91–98. [DOI] [PubMed] [Google Scholar]
- Anderson JW, Johnstone BM, Cook-Newell ME (1995). Meta-analysis of the effects of soy protein intake on serum lipids. N Engl J Med 333, 276–282. [DOI] [PubMed] [Google Scholar]
- Barrett-Conner E, Stuenkel C (1999). Hormones and heart disease in women: heart and estrogen/progestin replacement study in perspective. J Clin Endocrinol Metab 84, 1848–1853. [DOI] [PubMed] [Google Scholar]
- Baum JA, Teng H, Erdman JW Jr, Weigel RM, Klein BP, Persky VW et al. (1998). Long-term intake of soy protein improves blood lipid profiles and increases mononuclear cell low-density-lipoprotein receptor messenger RNA in hypercholesterolemic, postmenopausal women. Am J Clin Nutr 68, 545–551. [DOI] [PubMed] [Google Scholar]
- Beaglehole R (1990). International trends in coronary heart disease mortality, morbidity, and risk factors. Epidemiol Rev 12, 1–15. [DOI] [PubMed] [Google Scholar]
- Carroll KK. (1991). Review of clinical studies on cholesterol-lowering response to soy protein. J Am Diet Assoc 91, 820–827. [PubMed] [Google Scholar]
- Clerici C, Setchell KDR, Battezzati PM, Pirro M, Giuliano V, Asciutti S et al. (2007). Pasta naturally enriched with isoflavone aglycons from soy germ reduces serum lipids and improves markers of cardiovascular risk. J Nutr 137, 2270–2278. [DOI] [PubMed] [Google Scholar]
- Crouse JR 3rd, Morgan T, Terry JG, Ellis J, Vitolins M, Burke GL (1999). A randomized trial comparing the effect of casein with that of soy protein containing varying amounts of isoflavones on plasma concentrations of lipids and lipoproteins. Arch Intern Med 159, 2070–2076. [DOI] [PubMed] [Google Scholar]
- De Caterina R, Scarano M, Marfisi R, Lucisano G, Palma F, Tatasciore A et al. (2010). Cholesterol-lowering interventions and stroke: insights from a meta-analysis of randomized controlled trials. J Am Coll Cardiol 55, 198–211. [DOI] [PubMed] [Google Scholar]
- Erdman JW Jr. (2000). AHA Science Advisory: soy protein and cardiovascular disease: A statement for healthcare professionals from the Nutrition Committee of the AHA. Circulation 102, 2555–2559. [DOI] [PubMed] [Google Scholar]
- Friedewald WT, Levy RI, Fredrickson DS (1972). Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of preparative ultracentrifuge. Clin Chem 18, 499–502. [PubMed] [Google Scholar]
- Gardner CD, Newell KA, Cherin R, Haskell WL (2001). The effect of soy protein with or without isoflavones relative to milk protein on plasma lipids in hypercholesterolemic postmenopausal women. Am J Clin Nutr 73, 728–735. [DOI] [PubMed] [Google Scholar]
- Greenland P, Knoll MD, Stamler J, Neaton JD, Dyer AR, Garside DB et al. (2003). Major risk factors as antecedents of fatal and nonfatal coronary heart disease events. JAMA 290, 891–897. [DOI] [PubMed] [Google Scholar]
- Grundy SM, Cleeman JI, Merz CN, Brewer HB Jr, Clark LT, Hunninghake DB et al. National Heart, Lung, and Blood Institute; American College of Cardiology Foundation; American Heart Association (2004). Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation 110, 227–239. [DOI] [PubMed] [Google Scholar]
- He J, Wofford MR, Reynolds K, Chen J, Chen C-S, Myers L et al. (2011). Effect of dietary protein supplementation on blood pressure: a randomized, controlled trial. Circulation 124, 589–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodges YK, Tung L, Yan XD, Graham JD, Horwitz LD (2000). Estrogen receptors alpha and beta: prevalence of estrogen receptor beta mRNA in human vascular smooth muscle and transcriptional effects. Circulation 101, 1792–1798. [DOI] [PubMed] [Google Scholar]
- Jenkins DJA, Mirrahimi A, Srichaikul K, Berryman CE, Wang L, Carleton A et al. (2010). Soy protein reduces serum cholesterol by both intrinsic and food displacement mechanisms. J Nutr 140, 2302S–2311S. [DOI] [PubMed] [Google Scholar]
- Joswig M, Hach-Wunderle V, Ziegler R, Nawroth PP (1999). Postmenopausal hormone replacement therapy and the vascular wall: mechanisms of 17 ˇ-estradiol’s effects on vascular biology. Exp Clin Endocrinol Diabetes 107, 477–487. [DOI] [PubMed] [Google Scholar]
- Kuiper GG, Lemmen JG, Carlsson B, Corton JC, Safe SH, van der Saag PT et al. (1998). Interaction of estrogenic chemicals and phytoestrogens with estrogen receptor beta. Endocrinology 139, 4252–4263. [DOI] [PubMed] [Google Scholar]
- LaRosa JC, He J, Vupputuri S (1999). Effect of statins on risk of coronary disease: a meta-analysis of randomized controlled trials. JAMA 282, 2340–2346. [DOI] [PubMed] [Google Scholar]
- Merz-Demlow BE, Duncan AM, Wangen KE, Xu X, Carr TP, Phipps WR et al. (2000). Soy isoflavones improve plasma lipids in normocholesterolemic, premenopausal women. Am J Clin Nutr 71, 1462–1469. [DOI] [PubMed] [Google Scholar]
- Reynolds K, Chin A, Lees KA, Nguyen A, Bujnowski D, He J (2006). A meta-analysis of the effect of soy protein supplementation on serum lipids. Am J Cardiol 98, 633–640. [DOI] [PubMed] [Google Scholar]
- Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee (2011). Heart disease and stroke statistics-2011 update: a report from the American Heart Association. Circulation 123, e18–e209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacks FM, Lichtenstein A, Van Horn L, Harris W, Kris-Etherton P, Winston M. American Heart Association Nutrition Committee (2006). Soy protein, isoflavones, and cardiovascular health: an American Heart Association Science Advisory for professionals from the Nutrition Committee. Circulation 113, 1034–1044. [DOI] [PubMed] [Google Scholar]
- Sharrett AR, Ballantyne CM, Coady SA, Heiss G, Sorlie PD, Catellier D et al. Atherosclerosis Risk in Communities Study Group (2001). Coronary heart disease prediction from lipoprotein cholesterol levels, triglycerides, lipoprotein(a), apolipoproteins A-I and B, and HDL density subfractions: The Atherosclerosis Risk in Communities (ARIC) Study. Circulation 104, 1108–1113. [DOI] [PubMed] [Google Scholar]
- Srinivasan SR, Berenson GS (1983). Serum lipoproteins in children and methods for study. In: Lewis LA (ed). CRC Handbook of Electrophoresis. Vol. 3, Lipoprotein Methodology and Human Studies CRC Press: Boca Raton, FL, USA, pp 185–203. [Google Scholar]
- Stamler J, Daviglus ML, Garside DB, Dyer AR, Greenland P, Neaton JD (2000). Relationship of baseline serum cholesterol levels in 3 large cohorts of younger men to long-term coronary, cardiovascular, and all-cause mortality and to longevity. JAMA 284, 311–318. [DOI] [PubMed] [Google Scholar]
- Wilson PW, Hoeg JM, D’Agostino RB, Silbershatz H, Belanger AM, Poehlmann H et al. (1997). Cumulative effects of high cholesterol levels, high blood pressure, and cigarette smoking on carotid stenosis. N Engl J Med 337, 516–522. [DOI] [PubMed] [Google Scholar]
- Zhang X, Shu XO, Gao YT, Yang G, Li Q, Li H et al. (2003). Soy food consumption is associated with lower risk of coronary heart disease in Chinese women. J Nutr 133, 2874–2878. [DOI] [PubMed] [Google Scholar]


