The blue circle is the universal symbol for diabetes mellitus [Fig. 1]. It was introduced in 2006 to give diabetes a common identity. The symbol aims to support all existing efforts to raise awareness about diabetes, inspire new activities, bring diabetes to the attention of the general public, brand diabetes, and provide a means to show support for the fight against diabetes. The blue circle icon was initially developed for the campaign that resulted in the passage of the United Nations (UN) Resolution 61/225, “World Diabetes Day” (WDD). The WDD was created in 1991 by the International Diabetes Federation (IDF) in response to growing concerns about the escalating health threat posed by diabetes. The WDD became an official United Nations day in 2007 with the passage of the UN resolution. It is marked every year on November 14 and celebrates the birthday of Sir Frederick Banting, who codiscovered insulin along with John MacLeod, Charles Best, and James Collip in 1922.[1]
Figure 1.
The blue circle- the global symbol for diabetes awareness and the logo of World Diabetes Day
Why a Circle?
The circle is a universal symbol with extensive meaning. It represents totality, wholeness, original perfection, the self, the infinite, the eternity, and timelessness. Most significantly for the campaign, the circle symbolized unity to support a UN resolution on diabetes and the need to remain united to make a difference.
Why Blue?
The IDF explains that the color is blue because it “reflects the sky that unites all nations and is the colour of the United Nations flag” and the shape is circle “because of the circle is a frequent occurrence in nature and because myriad cultures over time have used the circle to symbolize life, mother earth and health.”[2]
UN Resolution
The People's Republic of Bangladesh sponsored the campaign at the United Nations and fought a resolute diplomatic battle that see-sawed but, in the end, resulted in the 133 developing and transitional countries of the G77 accepting ownership of the resolution. The President Country of the G77, together with China, introduced the resolution into the UN General Assembly on December 20, 2006, and finally, the UN Resolution 61/225 was passed by consensus.[3] First United Nations World Diabetes Day was celebrated on November 14, 2007.
The UN resolution includes all forms of diabetes, type 1 and type 2. The resolution confirms that all member states recognize that diabetes is a “chronic, costly, and debilitating disease” and that it poses “challenges to achieving international development goals.” The General Assembly encouraged all member states to develop national programs for the prevention, care, and treatment of diabetes in line with the sustainable development and maturity of their health care systems.[4,5]
The story of blue circle and UN resolution is incomplete without mentioning the mother–daughter duo, Kari and Clare Rosenfeld [Fig. 2]. Clare was diagnosed with type 1 diabetes at the age of 7 years. In 2000, she served as the National Youth Ambassador for the American Diabetes Association. In 2001, over a kitchen table conversation, Clare, then 16-year-old, discussed about diabetes with her mother, Kari, to explore ways to help young people with the disease and imagined a possible UN involvement. In 2003, the Rosenfelds attended the IDF World Congress in Paris, where Clare spoke on the importance of involving youth in diabetes prevention. Later, Kari Rosenfeld met Professor Martin Silink, the federation's then president-elect, and asked him if his group, which already had its own diabetes day, had thought about lobbying for a UN resolution. It caught Professor Silink “off guard,” though, in 2005, he appointed Kari Rosenfeld as the project manager for the UN resolution. The IDF board approved the “United for Diabetes” campaign, and the People's Republic of Bangladesh offered to sponsor the resolution.[6] Although a resolution could only be a piece of paper and does not mandate a law, a UN resolution undoubtedly imposes the moral will of the people and their needs.
Figure 2.

Left: Clare and Kari Rosenfeld. Right: Alain Baute (circa 2005). Source: World Diabetes Day: Looking at the past, present and future. www.healthline.com
Kari Rosenfeld always imagined a simple and recognizable design. A five-person team worked on developing a symbol. There was an agreement on the blue color with soft edges and that it would not carry any letter or numbers for international purpose and also that it would be easy to reproduce. Finally, Mr. Alain Baute [Fig. 2], who then worked in the Information Technology department of IDF, came up with the actual blue circle concept. It was based on the idea of a bubble.
Discovery of Insulin
Clare Rosenfeld, at the age of 16, could link youth and diabetes (she had type 1 diabetes) because she was leading a reasonably healthy life herself, thanks to insulin. Insulin has been the center of diabetes care for over a century since its discovery in the 1920s. The credit of insulin discovery goes to four people in the University of Toronto [Fig. 3], although it mostly owes to the tenacity of a young surgeon Frederick Banting, deeply interested in the functions of the pancreas and diabetes. Earlier works of Bernhard Naunyn, Oskar Minkowski, Eugene Opie, and Edward Sharpey-Schafer had indicated that diabetes was caused by the lack of a protein hormone secreted by the islets of Langerhans in the pancreas.[7] Bernhard Naunyn (German pathologist; 1839–1925) established the link between excess carbohydrate intake and diabetes; Oskar Minkowski (German physician and physiologist; 1858–1931) created dog-induced diabetes and proved that removal of the pancreas produced severe and fatal diabetes in dogs; Eugene Opie (American physician and pathologist; 1873–1971) documented consistent morphological alterations in the pancreatic islets of Langerhans in patients with diabetes mellitus; and Edward Sharpey-Schafer (English physiologist and endocrinologist; 1850–1935) theorized that a single substance from the pancreas was responsible for diabetes mellitus. It was supposed that the substance, later named insulin, controls the metabolism of sugar and the lack of it results in the accumulation of sugar in the blood and the excretion of the excess of sugar in the urine. Attempts to supply the missing insulin by feeding patients with the fresh pancreas, or extracts of it, had failed, presumably because the proteolytic enzyme of the pancreas had destroyed the protein insulin in them. The problem, therefore, was how to extract insulin from the pancreas before it had been thus destroyed.
Figure 3.
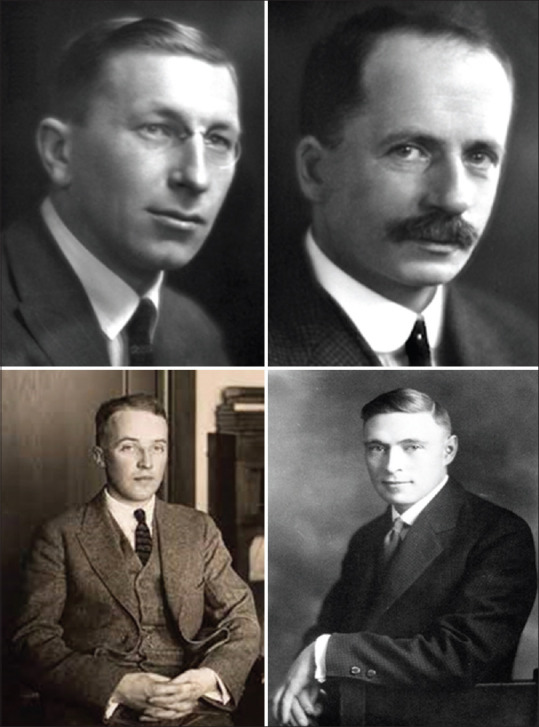
Fredrick G. Banting (1891–1941) [upper left], John J.R. MacLeod (1876–1935) [upper right], Charles H. Best (1899–1978) [lower left], and James B. Collip (1892–1965) [lower right]. Banting and MacLeod received the Nobel Prize in Physiology or Medicine in 1923 for the discovery of insulin and shared the prize money with Best and Collip, respectively. Source: Wikipedia.
In 1920, Moses Barron (American physician, 1884–1974), in his classic paper “The Relation of the Islets of Langerhans to Diabetes,” published in the Surgery, Gynaecology and Obstetrics, reported that when the pancreatic duct was experimentally closed by the ligatures, the cells of the pancreas secreted trypsin degenerate, but the islets of Langerhans remained intact.[8] This suggested to Banting that the ligation of the pancreatic duct would destroy the cells that secrete trypsin, and in turn, avoid the destruction of insulin, so that, after sufficient time had been allowed for the degeneration of the trypsin-secreting cells, insulin might be extracted from the intact islets of Langerhans. He discussed this idea with several people, including Professor John MacLeod (University of Toronto), who gave him the facilities to work on his research laboratory. Charles Best, a 22-year old medical student, was appointed as Banting's assistant. The breakthrough happened in 1921 when insulin was first extracted, and in 1922 a diabetic teenager Leonard Thompson became the first person to receive an insulin injection as a treatment for type 1 diabetes.[9]
Frederick was knighted by King George V in 1934 for the outstanding discovery. He was offered a large sum of money for the patent of insulin. An Insulin Clinic was proposed with Banting as the person in charge and would make the medicine available to all those who could pay for it. Banting's simple statement was “insulin does not belong to me; it belongs to the world.” His generosity gave the world insulin that was accessible to everyone who needed it.[10]
Three other scientists were intimately connected with Banting's journey of insulin discovery. They were Professor John MacLeod, Charles Best, and James Collip. On November 7, 1920, Banting requested MacLeod, a Scottish biochemist and physiologist, chiefly interested in carbohydrate metabolism, who was then teaching at the University of Toronto.[11] MacLeod was traveling on a summer holiday when Banting requested him to use his laboratory to isolate pancreatic extracts from dogs. Following a brief hesitation, MacLeod agreed, and he supplied Banting with 10 dogs for the experiment and two medical students, Charles Best and Clark Noble, as laboratory assistants. Since Banting required only one assistant, Best and Noble flipped a coin to see who would assist Banting first; the coin favored Best, and when Banting decided to keep one assistant, Best worked for the entire summer. MacLeod was overseeing the work of Banting. By December 1921, the duo had difficulty refining the pancreatic extract and monitoring glucose levels. MacLeod assigned his biochemist James Collip to the team. Collip was working with MacLeod on a Rockefeller travel scholarship on the effect of pH on the sugar concentration in the blood. Collip's task was to prepare insulin in a more pure form than what Banting and Best had achieved till that date.
On January 11, 1922, while Collip was working on insulin purification, Best and Banting administered their pancreatic extracts prematurely to 14-year-old Leonard Thompson with type 1 diabetes. Following the injection, Thompson suffered a severe allergic reaction. However, Collip's “relatively purer” pancreatic extract helped Leonard recover after the second dose was injected 12 days later, on January 23, 1922. Leonard improved and lived 13 years longer before he died of pneumonia at the age of 27. (Another patient injected during the same time, Ted Ryder, died in 1993 after 73 years.[11]) With this brief and successful human “clinical trial,” the future of insulin was secured. Banting, Best, and Collip subsequently shared the patent for insulin, which they sold to the University of Toronto for 1 dollar in December 1922.
In 1923, the Nobel Prize Committee honored Banting and MacLeod with the Nobel Prize in Medicine for the discovery of insulin, ignoring Best and Collip. Banting chose to share half of the prize money with Best, and MacLeod shared half of the prize money with Collip.
John MacLeod delivered his Nobel lecture on May 26, 1925, and Fredrick Banting delivered his Nobel lecture on September 15, 1925, in Stockholm.[12,13] They both acknowledged all previous work of identifying the ductless gland like the pancreas and the function of the islet of Langerhans in secreting the hormone, which played an essential role in carbohydrate metabolism in animals. They also acknowledged the extraordinary work of Best and Collip. Banting recalled the influence of Moses Barron's work of experimental ligation of the pancreatic duct and continued, “Having read this article [in preparation of a physiology lecture on the function of the pancreas], the idea presented itself that by ligating the duct and allowing time for the degeneration of the acinus cells, a means might be provided for obtaining an extract of the islet cells free from the destroying influence of trypsin and other pancreatic enzymes.” The experiment started on May 14, 1921; different means of extraction of insulin from other animals continued, and its clinical efficacy was proven in the treatment of type 1 diabetes nearly a year later.
Insulin Treatment for Diabetes
The only effective treatment of type 1 diabetes before insulin was a no-carbohydrate and a strict low-calorie diet, often limited to as low as 500 calories per day. It was slow starvation and demanded the strong willpower of the patient. Leonard Thompson, a 14-year-old boy with type 1 diabetes and the first recipient of insulin, was struggling with life, weighing only 65 pounds (29.5 kg) suffering from the end stages of diabetes mellitus. His father, desperate to save the life of his son, agreed to the newly discovered but never tested molecule “insulin.”[14] Leonard received the first injection of a “less purified” insulin on January 11, 1922, that did not help him much, but he improved after the second series of a “better purified” insulin injected on January 23, 1922.
On the treatment of Leonard, the authors stated, “the extracts given on January 11th were not as concentrated as those used at a later date, and, other than a slightly lowered sugar excretion and a 25% fall in the blood sugar level, no clinical benefit was evidenced…. Daily injections of the extract were made from January 23rd to February 4th. This resulted in immediate improvement.” These results were published in the February 1922 issue of the Journal of Laboratory and Clinical Medicine.[15] In a later publication in the Canadian Medical Association Journal, they shared a detailed description of the treatment of Leonard and a brief description of another six patients.[16] The discovery of insulin and its application to human beings made front-page news around the world. The year 2021 marks the 100th anniversary of insulin's discovery. Two years after its discovery, insulin was commercially made available in 1923 by Eli Lilly and Company (Indianapolis, USA, marketed as “Isletin”).[17] (Charles Best had first used the word “isletin” on August 4, 1921, in his laboratory notes.)
History of Diabetes
The first known reference to diabetes is by the Egyptian physician Hesy-ra (1550 BCE), who described “excessive urination” as the most important symptom.[18] The term diabetes was coined by Apollonius (250 BCE) from the Greek word meaning “siphon” – to pass through – after noting the frequent urination seen in these patients. The Greek physician Aretaeus (81–138 CE) produced the first clear written description of diabetes.[18] He described diabetes as “a melting down of the flesh and limbs into urine.” The English physician Thomas Willis (1721–1775) renamed the disease “diabetes mellitus”; the term mellitus translates to “like honey” in Greek.[18]
Twenty years before Oskar Minkowski and Joseph von Mering documented (in 1889) the connection between pancreatic secretions and diabetes, Paul Langerhans (German pathologist, physiologist and biologist, 1847–1888) had discovered two systems of cells in the pancreas: The acini, which he knew produced the pancreatic digestive secretions, and another system whose function was unknown to him. Langerhans was a 22-year-old medical student working on his doctorate thesis at the Berlin Pathological Institute, when in February 1869, he presented a thesis on “Contributions to the microscopic anatomy of the pancreas.” These cells looked to Langerhans like tiny clusters of cells, or islands, floating among the acini – the “islets of Langerhans.”[19] In 1901, Eugene Opie made the association between the degeneration of these cells and the onset of diabetes.[19] In 1916, Edward Albert Sharpey-Schafer described the role of insulin in the pathogenesis of diabetes. He coined the word insulin derived from the Latin word insula, meaning island, referring to the insulin-producing pancreatic cells, the islets of Langerhans.[19]
The discovery of insulin was a quintessential Eureka moment of 20th-century medical science. It all began with a borrowed laboratory, a few experimental dogs, a desperate patient, and an inspired surgeon with an excellent idea and a laser-like focus.[14] The concluding statement of Banting's Nobel lecture in 1925 that “insulin is not a cure for diabetes; it is a treatment”[13] holds nearly a century after it was said.
Diabetes and its complications are major health problems in the world. In 2019, the IDF estimated that half of the 463 million adults living with diabetes were unaware of the condition. Globally, 11.3% of deaths are due to diabetes. The IDF estimated that approximately 4.2 million adults would die due to diabetes and its complications in 2019; it equals one death every 8 seconds.[20] There is an equally significant social and economic impact. The IDF estimates that the annual global health expenditure on diabetes at USD 760 billion in 2019 would increase to USD 825 by 2030 and to USD 845 billion by 2045, an increase by 8.5% and 11.2%, respectively, over 2019 expenditure.[20] This does not include indirect and intangible costs.
The story of insulin teaches us two important lessons: One, it is a shining example of bench-to-bedside medical discovery. In preparation for his physiology lecture on the function of the pancreas, on October 31, 1920, at 2 a.m., Banting jotted, “Ligate pancreatic ducts of dog. Keep dogs alive till acini degenerate, leaving Islets. Try to isolate the internal secretion of these to relieve glycosurea [glycosuria].” And 15 months later, on January 23, 1922, a patient with type 1 diabetes was successfully treated. Two, it is an excellent example of academia–industry interaction. On January 25, 1922 (2 days after the first successful human treatment), the discovers, Banting, Best, MacLeod, and Collip, signed an agreement of cooperation with the University of Toronto's wholly-owned, noncommercial, public health entity, the Connaught Antitoxin Laboratories (established in 1914 by Dr. John G. FitzGerald; now Connaught campus of Sanofi Pasteur) [Fig. 4]. In 1923, Eli Lilly made commercial production of insulin and distributed it free for one year.[21]
Figure 4.
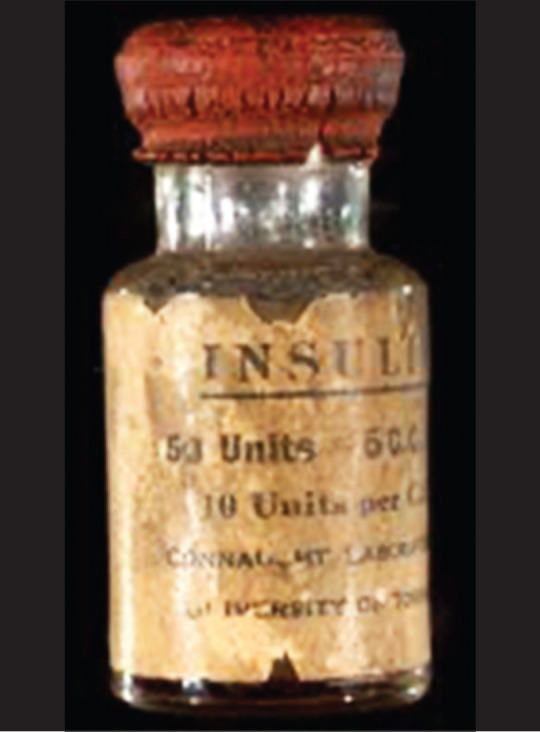
Original insulin produced by Connaught Antitoxin Laboratories, Toronto, Canada, 1922. Source: Sanofi Pasteur, Canada.
Insulin remains a treatment, not a cure for diabetes. We have not yet discovered a proven “cure” for diabetes. A century after the discovery of insulin, new therapies are explored in the search for cure and/or prevention of diabetes. Two emerging therapies are possible replacement of functional insulin-producing pancreatic cells with pancreas or islet-cell transplants with embryonic/adult stem cells[22] and a revisit to understand the role of the gut microbiome[23] with probable supplementation with probiotics.[24] Meanwhile, we need a greater commitment in every sphere, political and scientific, united under the blue circle, to reduce the prevalence of diabetes and its complications in the world. To do nothing is no longer an option.
About the authors

Dr. Taraprasad Das is currently Vice Chairman and faculty of Srimati Kanuri Shanthamma Centre for Vitreoretinal diseases, L V Prasad Eye Institute, Hyderabad; fellow of National Academy of Medical Science; Vice President, Asia Pacific Academy of Ophthalmology; and Fellow of Academy of Asia- Pacific Professors in Ophthalmology. His research includes diabetic retinopathy, infectious endophthalmitis, and public health ophthalmology. He has published over 300 research papers in medical journals, written over 50 book chapters.

Dr. Padmaja Kumari Rani is a vitreoretinal surgeon and an expert in the management of diabetic retinopathy with 18 years of professional experience. She has over 120 peer reviewed publications. She is the author of Sankara Nethralaya's Atlas of Retina Diseases. Dr. Rani is the Global Health Associate Editor for BMJ Case Reports. Dr Rani is currently a faculty of Srimati Kanuri Shanthamma Centre for Vitreoretinal diseases, L V Prasad Eye Institute, Hyderabad (India) and Associate Director of Teleophthalmology.

Dr. Sobha Sivaprasad is a Consultant Ophthalmologist in Moorfields Eye Hospital and Professor in Retinal Clinical Research in University College London. Her main research interests are clinical trials, imaging and risk prediction. She has been the Editor-in-Chief of Eye from January 2018. She leads the Retina Clinical Study Group within the UKCRN Ophthalmology subspeciality and is the Chair of the Scientific Committee RCOphth. She has published over 300 peer-reviewed research papers.

Dr. Rajiv Raman is a Senior Consultant at Department of Vitreoretinal services, Sankara Nethralaya, Chennai, India. He is also a Visiting Professor at Vision and Eye Research Unit, Anglia Ruskin University (ARU), Cambridge, UK. His research focus are Diabetic retinopathy, Age-related Macular Degeneration, Retinal imaging & Artificial Intelligence. He is a reviewer of 33 international peer-reviewed journals and section editor of Journal “Eye”. He has published 348 peer reviewed articles in medical journals.
References
- 1. [Last accessed 2021 Apr 16]. www.worlddiabetesday.org.
- 2.World Diabetes Day: Looking at the past, present and future. [Last accessed 2021 Apr 17]. www.healthline.com.
- 3.Silink M. UN resolution 61/225: A gift to the diabetes world. Pract Diab Int. 2007;24:387–88. [Google Scholar]
- 4. [Last accessed 2021 Apr 16]. www.un.org.
- 5.A United Nations resolution on diabetes. The results of a joint effort. US Endocrinology. 2007 doi:10.17925/USE.2007.1.12. [Google Scholar]
- 6.Local duo helps diabetes get its day. The Free Library 2006. [Last accessed 2021 Apr 17]. www.thefreelibrary.com/Local+duo+helps+diabetes+get+its+da.-a0156457585.
- 7.Zinman B, Skyler JS, Riddle MC, Ferrannini E. Diabetes research and care through the ages. Diabetes Care. 2017;40:1302–13. doi: 10.2337/dci17-0042. [DOI] [PubMed] [Google Scholar]
- 8.Reimann HA. Moses barron and banting. JAMA. 1967;199:48. [Google Scholar]
- 9.Frederick G. Banting – Biographical. [Last accessed 2021 Apr 17]. www.nobelprize.org.
- 10.The man gifted insulin to mankind instead of selling it. [Last accessed 2021 Apr 17]. www.thelogicalindain.com.
- 11.Cardoso L, Rodrigues D, Gomes L, Carrilho F. Banting and best: The extraordinary discovery of insulin. Rev Port Endocrinol Diabetes Metab. 2017;12:106–15. [Google Scholar]
- 12.MacLeod J. The physiology of insulin and its source in animal body. Nobel lecture. May 26, 1925. [Last accessed 2021 Mar 18]. www.nobelprize.org.
- 13.Granting F. Diabetes and insulin: Nobel lecture, September 15, 1925. [Last accessed 2021 Mar 18]. www.insulin.library.utoronto.ca.
- 14.Markel H. How a boy became the first to beat diabetes. 2013. [Last accessed 2021 Apr 18]. www.deepblue.lib.umich.edu.
- 15.Banting FG, Best CH. The internal secretion of the pancreas. J Clin Med. 1922;7:251–71. [PubMed] [Google Scholar]
- 16.Banting FG, Best CH, Collip JB, Campbell WR, Fletcher AA. Pancreatic extracts in the treatment of diabetes mellitus. Can Med Assoc J. 1922;12:141–6. [PMC free article] [PubMed] [Google Scholar]
- 17. [Last accessed 2021 Apr 22]. www.lilly.com>discovery>100-years-of-insulin.
- 18.Harold JG. Harold on history: An historical perspective on diabetes and cardiovascular disease. [Last accessed 2021 Apr 18]. www.acc.org›latest-in-cardiology›articles›2017/08/16.
- 19. [Last accessed 2021 Apr 18]. www.sciencehistory.org.
- 20.International Diabetes Federation Atlas 2019. [Last accessed 2021 Apr 18]. www.diabetesatlas.org.
- 21.Lewis GF, Brubaker PL. The discovery of insulin revisited: Lessons for the modern era. J Clin Invest. 2021;131:e142239. doi: 10.1172/JCI142239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Husain MA, Theise ND. Stem-cell therapy for diabetes mellitus. Lancet. 2004;364:203–5. doi: 10.1016/S0140-6736(04)16635-X. [DOI] [PubMed] [Google Scholar]
- 23.Das T, Jayasudha R, Chakravarthy S, Prashanthi GS, Bhargava A, Tyagi M, et al. Alterations in the gut bacterial microbiome in people with type 2 diabetes mellitus and diabetic retinopathy. Sci Rep. 2021;11:2738. doi: 10.1038/s41598-021-82538-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kocsis T, Molnar B, Nemeth D, Hegyi P, Szakacs Z, Balint A, et al. Probiotics have beneficial metabolic effects in patients with type 2 diabetes mellitus: A meta-analysis of randomized clinical trials. Sci Rep. 2020;10:11787. doi: 10.1038/s41598-020-68440-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


