Abstract
Background
Continuous education of clinicians improves quality of care. One Minute Wonder (OMW) summarize best practice knowledge on one page that can be hung on a wall and can be read during waiting times of just one minute. OMW are a fast, efficient and easy-to-adapt educational method and can easily be shared. Since 2018, an interprofessional network has been set up for OMW in German-speaking countries, but the benefits have not been evaluated yet.
Aim
The primary objective of this evaluation study was to examine whether and to what extent the members of the OMW network used OMW for training in different settings. Secondary objectives were subjective educational gain, OMW as a training method, and OMW-related structures and processes.
Methods
An online survey within the OMW network with 301 members over a period of 3 weeks in 2020 was conducted. Descriptive statistics were used for data analysis.
Results
Response rate was 62.8% (n = 191). Most participants have used OMW for < 6 months (32.5%, n = 62), developed 1–10 OMW (42.4%, n = 81) by themselves and changed them infrequently (43.5%, n = 74). Topics were most often nursing interventions (79.6%, n = 152), diseases (71.2%, n = 136), drugs (64.4%, n = 123) and others. Participants reported that OMW extended professional knowledge, stimulated them to reflect on their work and are useful for sharing best practice knowledge. Authors of OMW were most often nurses (53.9%, n = 103), who were inspired by the OMW network or by questions of the team.
Conclusion
Participants use OMW in practice to share best practice knowledge.
Supplementary Information
The online version of this article (10.1007/s00063-021-00892-3) includes Table E1.
Keywords: Evaluation, Continuing education, Intensive care unit, Knowledge transfer, Nursing
Abstract
Hintergrund
Kontinuierliche Fortbildung von medizinischem Personal verbessert die Versorgungsqualität. One Minute Wonder (OMW) fassen praxisbasiertes Wissen auf einer Seite zusammen, hängen an der Wand und können während Wartezeiten in nur einer Minute gelesen werden. Sie sind eine schnelle, effiziente und leicht anzupassende Bildungsmethode und können leicht weitergegeben werden. Seit 2018 wurde für OMW im deutschsprachigen Raum ein interprofessionelles Netzwerk aufgebaut, dessen Nutzen jedoch noch nicht evaluiert wurde.
Ziel
Das primäre Ziel dieser Evaluationsstudie war zu untersuchen, ob und inwieweit die Mitglieder des OMW-Netzwerks OMW für die Fortbildung in unterschiedlichen Settings nutzen. Sekundäre Ziele waren: subjektiv bewerteter Bildungserfolg, OMW als Bildungsmethode sowie OMW-bezogene Strukturen und Prozesse.
Methode
Es wurde eine Onlinebefragung des OMW-Netzwerks mit 301 Teilnehmenden über einen Zeitraum von 3 Wochen im Jahr 2020 durchgeführt. Zur Datenanalyse kamen Methoden deskriptiver Statistiken zum Einsatz.
Ergebnisse
Die Rücklaufquote betrug 62,8 % (n = 191). Die meisten Teilnehmenden setzten OMW < 6 Monate ein (32,5 %, n = 62), haben 1–10 OMW (42,4 %, n = 81) selbst entwickelt und diese selten gewechselt (43,5 %, n = 74). Themen waren am häufigsten Pflegeinterventionen (79,6 %, n = 152), Krankheiten (71,2 %, n = 136), Medikamente (64,4 %, n = 123) und andere. Die Teilnehmenden berichteten, dass OMW ihr Fachwissen erweitert, sie zum Nachdenken über ihre Arbeit anregen und für den Austausch von best verfügbarem Wissen nützlich sind. Autoren von OMW waren am häufigsten Pflegende (53,9 %, n = 103), die sich vom OMW-Netzwerk oder von Fragen des Teams inspirieren ließen.
Diskussion
Die Teilnehmenden nutzen OMW zum Austausch von bestem praxisbasiertem Wissen.
Schlüsselwörter: Evaluation, Fortbildung, Intensivstation, Wissenstransfer, Pflege
Introduction
Continuing education is an important aspect for providing best care by healthcare professionals in intensive care units (ICU). One feasible educational method is the One Minute Wonder (OMW). OMW present healthcare-related information, are hung up in clinicians’ waiting areas, printed on a single page and can be read within a minute.
Since 2018, an interprofessional network has been set up for the development and distribution of OMW in German-speaking countries, but its benefits had not been evaluated yet.
The following study presents the results of the survey of the OMW network and the effects of OMW in different settings—especially the ICU.
Background
Continuous education of clinicians is an important aspect of professionalism in healthcare, especially in ICUs [21, 27]. One goal is the transfer of knowledge into practice [9]. There are different ways of learning and further training for healthcare workers like e‑learning [18], conferences [25], seminars, workshops or degree courses [2]. Furthermore, short offers from seconds to minutes like SMS [5, 24], videos, or podcasts are also possible [7]. It is not always necessary to be a part of a training course because work-based learning (WBL) also takes place day by day, e.g., during a discussion of a few minutes with colleagues [1] or on the regular work like handovers of nurses or other healthcare professionals [4].
One Minute Wonder (OMW) is a training method for the continuous education of clinicians in different healthcare settings, with a focus on critical care [23]. Usually, OMW summarize best practice knowledge such as ventilator settings, blood sugar management, new rules of bandages/dressing changes etc., on one page. OMW include text, tables or figures. OMW are hung up in places with regularly recurring waiting times in daily nursing practice ([23]; Fig. 1). In nursing departments, recurring short waiting times occur in different frequency and duration at certain locations, e.g., at a microwave oven or a laboratory device. OMW are changed in regular intervals of, for example, two weeks. The content of an OMW should be designed to be taken in within about one minute [23]. In addition, the method can be used in many other areas of healthcare, such as the ambulance service [8, 23], gastroenterology [20] or neonatal intensive care units [12]. So-called “OMW managers” can be appointed for coordination and implementation of this educational method [16]. In first pilot projects in anesthesia, OMW were perceived as helpful by caregivers [13]. In combination with continuous educational methods, OMW were able to lead to an improvement in patient care [6]. In addition, two pilot evaluations [15, 19] and one evaluation study [17] with nurses from ICU proved that the staff appreciated OMW as a learning method.
Fig. 1.
One Minute Wonder (OMW) in an intensive care unit near a blood gas analyzer
Following the inspiring example of England [23], an OMW network in German-speaking countries (Austria, Germany, Luxembourg, and the German-speaking part of Switzerland) was founded in March 2018. Participation and registration in the OMW network was via email request and without any charges. The aims are free exchange, discussion and dissemination of OMW. Members of the network have access to many OMW of other settings in healthcare, which gives them the opportunity to receive additional external impulses and ideas for their own nursing activities. A newsletter with updates and new OMW are distributed within the network quarterly. Currently, about 300 people from different healthcare settings are taking part [16]. However, the benefits of this network have not been scientifically evaluated yet.
The primary objective of this evaluation study was to examine whether and to what extent the members of the OMW network used OMW for training in different settings. Secondary objectives were subjective educational gain, OMW as a training method, and OMW-related structures and processes.
Methods
Study design
The study is an evaluation study using a closed online survey. The survey was designed in accordance with recommendations for reporting electronical surveys ([26]; Table E1 in the online supplementary material).
Setting
OMW network members were from different settings including ICUs, intermediate care, hospitals’ wards, long-term outpatient and inpatient care facilities and others. They are from Germany (n = 289), Austria (n = 7) and Switzerland (n = 5).
Participants
All OMW network participants (n = 301) from German-speaking countries were invited to participate in this study. Inclusion criteria were (a) ≥ 18 years of age, (b) registered member of the OMW network. Exclusion criteria were less than 50% of the questions answered. The subjects were informed about the study and received a link to an online questionnaire, using SurveyMonkey (SurveyMonkey, San Mateo, CA, USA). The data collection was anonymous and performed in April 2020. Three reminders were sent by email.
Variables
The primary outcome was the use of the OMW, operationalized by the questions of how many participants were using OMW, for how many years OMW have been used and how many have been created during that time.
The secondary outcome parameters are operationalized by:
The subjective educational gain entered on a scale of 1–6 stars (6 = maximum educational gain).
the assessment of OMW as a training method entered on a scale of 1–6 stars (6 = maximum educational gain).
OMW-related structures and processes.
Instrument/data
Based on previous evaluations [15, 19], we developed a questionnaire for data collection. In addition to questions about the use of OMW, sociodemographic data (country, profession, work experience etc.) were added (Table 1). The development of the questionnaire was carried out within an expert panel of nurses and researchers. The current questionnaire was standardized pretested by 13 clinicians with experience of the implementation and development of OMW for comprehensibility, linguistic adjustments and the time to fill in the questionnaire, resulting in minimal modifications.
Table 1.
Sociodemographic data
| Itema | Total (n = 191) |
|---|---|
| Country | n (%) |
| Germany | 183 (95.8) |
| Switzerland | 5 (2.6) |
| Austria | 3 (1.6) |
| Profession | n (%) |
| Registered nurses | 176 (93.6) |
| Physicians | 3 (1.6) |
| Others | 9 (4.8) |
| Work experience | n (%) |
| 0–2 years | 2 (1.1) |
| 3–4 years | 3 (1.6) |
| 5–10 years | 37 (19.6) |
| > 10 years | 147 (77.8) |
| Place of work | n (%) |
| Intensive care unit | 96 (50.8) |
| Management, research, education | 46 (24.3) |
| General ward | 15 (7.9) |
| Other | 32 (16.9) |
| Specialty | n (%) |
| Adult care | 157 (84) |
| Pediatric care | 14 (7.5) |
| Geriatric care | 2 (1.1) |
| Other | 14 (7.5) |
aData reported as n (%). Proportions may not add up to 100% due to rounding
Survey
The survey was a closed online questionnaire consisting of 25 questions on 4 pages, including 151 items, with a mean of 6 items per question. The survey included closed questions with single and multiple items. In 12 questions a comment option was possible. Participants had the choice to go back and forth while answering the questions but had no access to overall results. Participants did not have to fill in every question and had an option of “not applicable” or the like. In the pretest, the mean required time to fill out the questionnaire was 8 min 30 s.
The survey assessed the following: implementation of OMW, country, profession, years of ICU experience, place of work (bedside, management, education etc.), pediatric, adult, or geriatric care, educational possibilities, number of units with OMW and discipline, number of OMW locations within one unit, OMW location, frequency of change, OMW archives, ideas for creating OMW, authorship, time since implementation, number of OMW produced, peer-review, topics, personal benefit, benefit for unit, conflicts, support, personal educational gain, overall ranking of OMW from 1 to 6 stars with 6 representing highest score.
All authors approved the final version of the survey. The survey’s items and answers in the survey were in a different order than in this publication.
Statistical methods
The survey’s data were exported to SPSS 22.0 (IBM, Armonk, NY, USA), coded including missing data and calculated. Nominal and categorical data are reported as number and percent, ordinal data in its modus. Metrical data are reported as median and interquartile range (IQR), due to nonnormal distribution. Items were not weighted. Possible statistical relationship between the implementation of OMW and different countries, professions, years of work experience, place of work, specialty or institutions with more or less than 4 educational offers were calculated by Fisher’s exact test on the base of double-sided α = 0.05.
Ethical considerations
No personal data were requested. All participants were informed about the voluntary, anonymous approach and the time required to answer all questions. Participation was counted as consent. In advance, the local ethics committee of the Medical Faculty of the Christian Albrechts University in Kiel approved the survey (file number D 441/20). Afterwards the study has been registered in the German register of clinical trials (DRKS00021116) on 18 March 2020 (www.drks.de).
Results
In all, 301 members of the OMW network were invited for participation in to the study. Response rate was 62.8% (n = 191), completion rate 85.8% (n = 164). All returned questionnaires could be included.
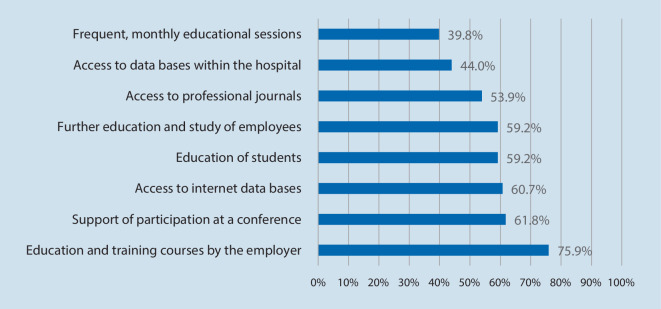
Most participants were from Germany (95.8%, n = 183), nurses (93.6%, n = 176), had more than 10 years’ work experience (77.8%, n = 147), worked on ICU (50.8%, n = 96) and cared for adult patients (84%, n = 157; Table 1). More than half of the participants reported having educational trainings offered by the employer, education of students or supported participation at conferences (Fig. 2).
Fig. 2.
Educational trainings. Based on n = 191 respondents. Multiple answers. Data reported as %
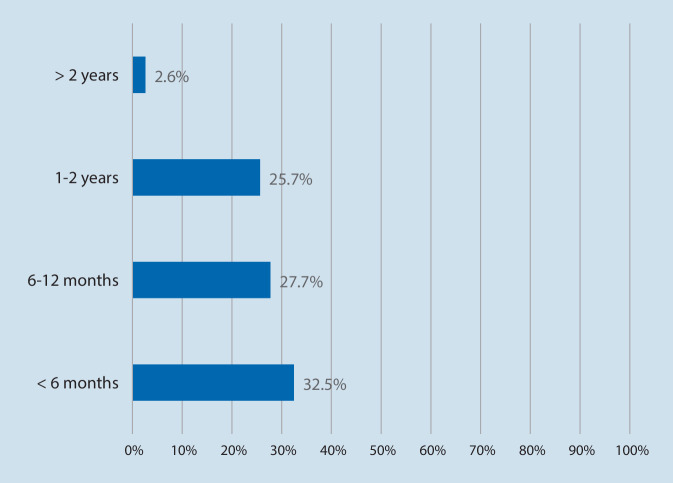
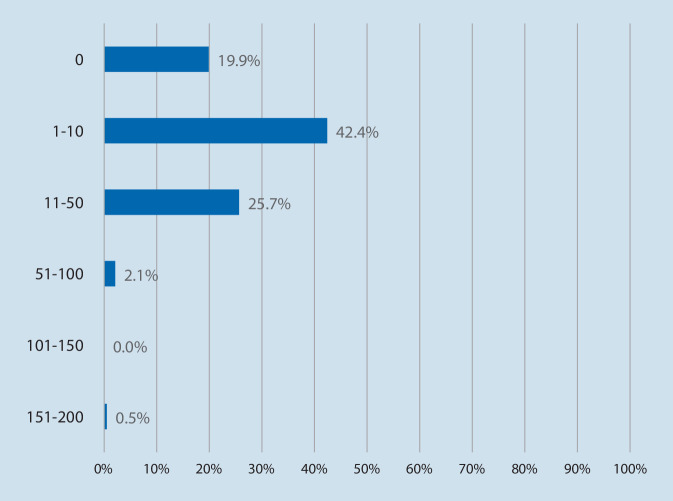
The majority of respondents were using OMW in their hospitals (74.2%, n = 141), others were planning implementation (25.8%, n = 49), and no one was unaffected by OMW. Related to the time OMW are used in practice, most participants reported to have been using OMW for less than 6 months (32.5%, n = 62) and developed 1–10 OMW (42.4%, n = 81; Figs. 3 and 4).
Fig. 3.
One Minute Wonder are used since. Based on n = 191 respondents. Multiple answers. Data reported as %. Proportions may not add up to 100% due to rounding
Fig. 4.
Extent of self-produced One Minute Wonder. Based on n = 191 respondents. Multiple answers. Data reported as n %. Proportions may not add up to 100% due to rounding
Participants ranked the median educational gain for themselves with 5 (IQR 5–6) and for their teams with 6 (IQR 5–6) of maximum 6 stars.
Participants reported benefits due to OMW. OMW extended their professional knowledge, helped to reflect their work und extended professional competence (Table 2). Some participants used OMW for writing homework or a professional thesis. Most respondents reported to have no conflicts with using OMW (56.5%, n = 103), while one in five participants reported that OMW led to conflicts with colleagues (19.4%, n = 37). These conflicts were judged as positive by the majority (19.9%, n = 38).
Table 2.
Ranking of the benefits and conflicts
| Itema … | Total (n = 191) |
|---|---|
| One Minute Wonder (OMW)b … | Median (IQR) |
| Extend my professional knowledge | 1 (1–1) |
| Stimulate to reflect my work | 1 (1–1.75) |
| Extend my professional competence | 1 (1–2) |
| Lead to implementation of OMW | 1 (1–2) |
| Improve quality of care in my unit/ward | 1 (1–2) |
| Is useful for sharing evidence-based knowledge with my colleagues | 1 (1–2) |
| Have improved my motivation | 2 (1–2) |
| Improve cooperation in my team | 2 (1–3) |
| Supported quality improvement projects on my unit/ward | 2 (1–3) |
| Lead to communication with other healthcare institutions | 2 (1–4) |
| Lead to ask for help and advice how to develop OMW | 3 (2–4) |
| Supported quality improvement projects in my hospital | 3 (2-4) |
| Has improved my work in a negative manner | 5 (5–5) |
| None of the above | 5 (2–5) |
| Helped to write ac … | n (%) |
| Thesis | 23 (12) |
| Homework | 21 (10.9) |
| Bachelor’s thesis | 9 (4.7) |
| Dissertation thesis | 9 (4.7) |
| Master’s thesis | 4 (2) |
| OMW led to conflicts … | n (%) |
| No, we have had no conflicts so far | 103 (56.5) |
| Between my colleagues and myself | 37 (19.4) |
| Between my knowledge and to content of OMW | 21 (11) |
| Between different professions | 13 (6.8) |
| Between nursing management and myself | 11 (5.8) |
| And I rank these conflicts as very positive | 38 (19.9) |
| And I rank these conflicts as very negative | 4 (2.1) |
aMultiple answers. Data reported as n (%), or median (IQR). Proportions may not add up to 100% due to rounding
bOptions to answer were yes, rather yes, do not know, rather no, no, and coded as 1 (= yes), 2, 3, 4, and 5 (= no)
cYes and rather yes from b were summarized
Questions about the structure of OMW showed that a broad range of topics, mostly nursing interventions (79.6%, n = 152), were covered by OMW. OMW were placed mostly on one unit/ward in the hospital (32.1%, n = 54), which was most often an ICU (68.1%, n = 130). OMW were hung up in median in 2 (IQR 1–2.7) places, most often next to the blood gas analyzer (62.3%, n = 119) and were stored in folders for later relocating (40.6%, n = 69; Table 3). A few participants reported using OMW as screensavers on monitors with frequent changes.
Table 3.
Structure of One Minute Wonder (OMW)
| Itema | Total (n = 191) |
|---|---|
| OMW covers following subjects | n (%) |
| Nursing interventions | 152 (79.6) |
| Diseases | 136 (71.2) |
| Drugs | 123 (64.4) |
| Medical interventions | 98 (51.3) |
| Monitoring, equipment | 96 (50.3) |
| Scales and scores | 89 (46.6) |
| Devices | 81 (42.4) |
| “Good to know” issues | 77 (40.3) |
| Ethical issues | 39 (20.4) |
| Team cooperation | 35 (18.3) |
| Summaries of studies | 33 (17.3) |
| Work–life balance of staff | 32 (16.8) |
| Alternative nursing and interventions (music, pets etc.) | 22 (11.5) |
| Family centered care | 13 (6.8) |
| OMW are distributed on following number of units in the hospital | n (%) |
| 1 | 54 (32.1) |
| 2 | 39 (23.2) |
| 3 | 24 (14.3) |
| 4 | 10 (6) |
| 5 | 6 (3.6) |
| > 5 | 35 (20.8) |
| OMW are distributed on following specialties | n (%) |
| Intensive care units | 130 (68.1) |
| Intermediate care units | 59 (30.9) |
| General ward | 48 (25.1) |
| Anesthesia | 24 (12.6) |
| Emergency department | 13 (6.8) |
| Research and education | 12 (6.3) |
| Management | 11 (5.8) |
| Living area | 5 (2.6) |
| Other | 14 (7.3) |
| Places of OMW | n (%) |
| Blood gas analyzer | 119 (62.3) |
| Centre of unit | 63 (33) |
| Staff pantry | 61 (31.9) |
| Kitchen | 33 (17.3) |
| Storage | 32 (16.8) |
| Staff’s washroom | 22 (11.5) |
| Drinks trailer | 4 (2.1) |
| Other | 35 (18.3) |
| Archives of previous OMW | n (%) |
| OMW are stored in a folder | 69 (40.6) |
| OMW are stored electronically | 38 (22.4) |
| OMW can be read | 23 (13.5) |
| OMW are stored in different medias | 8 (4.7) |
| OMW are not stored | 31 (18.2) |
OMW One Minute Wonder
aMultiple answers. Data reported as n (%). Proportions may not add up to 100% due to rounding
Participants reported OMW-related processes. OMW were most often infrequently changed (43.5%, n = 74). Attendees reported receiving their inspiration for developing OMW most often from the OMW network (63.9%, n = 122). Creators of OMW were most often nurses of the unit/ward (53.9%, n = 103). OMW were reviewed for quality before publishing by the leading nurses (42.9%, n = 82). Developing OMW was most often honored by the acknowledgement of overtime (28.8%, n = 55). Some participants also reported that development was done in their regular working time (Table 4).
Table 4.
Processes related to One Minute Wonder (OMW)
| Itema | Total (n = 191) |
|---|---|
| Frequency of renewing OMW | n (%) |
| Infrequently | 74 (43.5) |
| Once per 1 week | 9 (5.3) |
| Once per 2 weeks | 52 (30.6) |
| Once per 4 weeks | 20 (10.5) |
| Other | 15 (7.8) |
| Inspiration for development of OMW is generated by | n (%) |
| OMW network | 122 (63.9) |
| Questions by team, meetings | 99 (51.8) |
| Journals | 75 (39.3) |
| Conferences | 55 (28.8) |
| Further education, study | 50 (26.2) |
| Team leaders | 28 (14.7) |
| Social media | 16 (8.4) |
| Other | 25 (13.1) |
| Creators of OMW | n (%) |
| Nurses of the unit/ward | 103 (53.9) |
| OMW delegate | 51 (26.7) |
| Staff of quality management | 18 (9.4) |
| Internal education/internal training | 14 (7.3) |
| Students | 13 (6.8) |
| Other professions | 13 (6.8) |
| Trainees | 9 (4.7) |
| Other | 48 (25.1) |
| OMW are reviewed before publishing by | n (%) |
| Leading nurse | 82 (42.9) |
| Specific experts | 63 (33) |
| Themselves (respondent of survey) | 63 (33) |
| Leading physician | 37 (19.4) |
| OMW project group | 36 (18.8) |
| OMW are not reviewed | 12 (6.3) |
| Other | 12 (6.3) |
| The creation and development of OMW is honored by | n (%) |
| Acknowledgement of overtime | 55 (28.8) |
| Support in literature search | 18 (9.4) |
| Exemption from work | 14 (7.3) |
| Financial bonus | 2 (1) |
| A certification | 1 (0.5) |
| Other | 23 (12) |
aMultiple answers. Data reported as n (%). Proportions may not add up to 100% due to rounding. In some items, data were missing, all < 5%
There were no significant differences for the implementation of OMW and different countries (p = 0.255), professions (p = 0.421), years of work experience (p = 0.831), place of work (p = 0.224), specialty (0.222), or institutions with more or less than 4 educational offers (p = 0.620).
Discussion
The electronical survey within the German-speaking OMW network including nearly 200 respondents showed that three quarter of clinicians were using OMW in practice, while one quarter is planning implementation. Regarding the time OMW have been used in practice, most participants reported having used OMW for less than 6 months and developed fewer than 10 OMW. OMW were hung up next to the blood gas analyzer or used as screen savers on monitors. OMW topics were most often nursing interventions, diseases, drugs, and others. Authors of OMW were most often nurses who were inspired by the OMW network or by questions of the team. Participants reported that OMW extended their professional knowledge, stimulated them to reflect on their work, and were highly ranked for sharing best practice knowledge.
The results show that three quarters of the participated clinicians used OMW most frequently in hospital settings. Considering that the original idea of the OMW also originates from the hospital setting and has been significantly communicated in this environment in the German-speaking region [8, 19], this result is not surprising. The usage mainly takes place in ICU. This is probably due to the fact that the network was founded by ICU staff and was therefore also presented to this group, for example at conferences and by publications [12, 15]. The educational offers in the hospitals indicate the extent of support of their employees (Fig. 2). At the same time, the results show that other healthcare facilities, such as emergency services, also use OMW to impart knowledge (6.8%, n = 13) and these facilities also communicate this through publications [8]. The work of Herrmann et al. [12] shows that the method has also established itself in other specialist areas, for example in a neonatal ICU. Anecdotally, we notice an increasing interest for OMW in other settings such as nursing facilities, ambulant care, or hospice care. Nevertheless, the reasons for nonparticipation in the OMW network can be manifold such as use of other educational methods, no knowledge about the network, no interest, language barriers, time und staff constraints, and others.
The number of members of the OMW network shows that the method is frequently used in German-speaking countries and represents an effective method of knowledge transfer. Given that the network has only existed since March 2018, the high number of respondents intending to implement this method is consistent. The fact that the OMW has been used by many for less than 6 months is also attributable to the age of the network that continues to grow. Since this study in April 2020, more than 80 new members were registered in the OMW network as of March 2021. A further interpretation of the high number of interested parties is that this method is highly accepted in practice. At the time of the survey, the majority of respondents had created 1–10 OMW. This depicts the high willingness of nursing staff to actively participate in this educational method. A further indication of the high acceptance of this low-threshold method is also shown by the fact that this approach is also be used in times of crisis [14] and is supported in this context by the German Interdisciplinary Association for Intensive Care and Rescue Medicine and further professional associations in nursing and medicine [11]. The website of the network (https://omw.hdz-nrw.de) currently offers learning posters on the topic of COVID-19 free of charge.
Overall, the personal educational gain through the OMW is rated by the respondents with a median of 5 out of 6 stars. This shows that this method certainly has a self-reported effect for the participants and is frequently used in practice. On the whole, the OMW is given a median of 6 out of 6 stars for the benefit to the team. It is interesting to note that the OMW is also used for critical reflection of one’s own work and leads to constructive discussions within the team, which in itself has its own learning effect [1]. Since the critical reflection of external evidence in relation to the individual patient arrangement and thus to one’s own work is a cornerstone of evidence-based care [3] and WBL [1, 22]. Billett pointed out that there are different activities during the regular work “… that are potentially pedagogically rich” [4]. OMW seems to be that for the participants in this study. Thus, the OMW is not only an educational tool, but also an instrument for quality-oriented practice development.
Regarding educational offers, effectiveness always depends on the scope, the didactic preparation, the target groups orientation and the general conditions in the context of the setting [23]. As OMW always present a condensed presentation of complex topics, the daily working conditions have to be considered when creating OMW [10]. A positive attitude towards education and individual training measures also supports the absorption and implementation of new knowledge [10]. Krüger et al. [17] have shown their study that 73.55% of those questioned confirmed the contents of OMW as helpful in their daily work. Lehnen et al. [19] could point out that 80% of the respondents remember the contents of OMW. Due to the small sample size of the first two cross-sectional surveys of Krüger [15] (n = 43) and Lehnen et al. [19] (n = 55) and the evaluation study of Krüger et al. [17] (n = 189), the external validity is limited.
Strengths and limitations
A strength of this survey is the high response rate of participants. Another strength is the widespread OMW network, covering a broad range implementation in different types of ICUs. Our study has some limitations. Since our results are limited to answers of participants from the OMW network, respondents possibly represent a recruitment and/or performance bias. However, the survey was anonymous and participants had no benefit for providing best answers. Second, we could not prevent participants from multiple entries, but due to the noneconomical or nonpolitical nature of this survey, this is unlikely to have happened. The report of this survey is limited to German-speaking population and culture; in countries with English as the first language, or different medical education, the perception of such an educational method may be different. Another limit is the self-constructed questionnaire without any data about its validity, reliability or objectivity. However, the questionnaire has been developed within an expert panel and was standardized pretested by 13 clinicians as an important step for practical use.
Conclusions for practice
The majority of the survey’s respondents implemented OMW in their units and shared developed OMW within the network. The sharing process is free and all participants can have a benefit. Furthermore, this method is feasible, simple and helped clinicians to extend their professional knowledge.
OMW can cover a broad range of topics, should be changed frequently and stored in a folder for relocating later.
OMW support professional reflection, continuous education of the multiprofessional team as well as the implementation of new procedures and thus put knowledge into practice.
Different settings in critical care should use OMW in practice.
Supplementary Information
Table E1: Criteria for reporting electronical surveys
Acknowledgments
Funding
The study was financed by the institutions of the first and senior author.
Abbreviations
- OMW
One Minute Wonder
- WBL
Work-based learning
Author Contribution
The authors LK and PN contributed to the conceptualization, development of the design, its conduction, analysis, evaluation, and final writing and review. LK did the project administration. TM, MR, FT, and FW contributed to the development, design, writing and approved the final manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Declarations
Conflict of interest
L. Krüger, T. Mannebach, M. Rahner, F. Timpe, F. Wefer and P. Nydahl declare that they have no competing interests.
For this article all investigations on humans described were carried out with the approval of the responsible ethics committee, in accordance with national law and the declaration of Helsinki in 1975 (in the current, revised version). Consent for publication: The authors affirm that the participant provided informed consent for publication of the image in Fig. 1.
Footnotes
Availability of data and materials
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
Clinical trial registration number
This study is registered in the German register of clinical trials (DRKS00021116).

Scan QR code & read article online
References
- 1.Attenborough J, Abbott S, Brook J, et al. Everywhere and nowhere: work-based learning in healthcare education. Nurse Educ Pract. 2019;36:132–138. doi: 10.1016/j.nepr.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 2.Ayed A, Thulth AS, Sayej S. Impact of night shift and training development factors on performance of professional nurses in north west bank governmental hospitals. J Nurs Educ Pract. 2015;6:50–60. [Google Scholar]
- 3.Behrens J, Langer G. Das professionstypische Arbeitsbündnis: Zauberinnen, Dienerinnen, Pflegeprofessionelle-Qualitätssicherung. In: Behrens J, Langer G, editors. Evidence based nursing and caring. 2016. pp. 31–46. [Google Scholar]
- 4.Billett S. Learning in the circumstances of practice. Int J Lifelong Educ. 2014;33:674–693. doi: 10.1080/02601370.2014.908425. [DOI] [Google Scholar]
- 5.Bowling JE. Impact of repetitive text messages on retention of knowledge. J Contin Educ Nurs. 2019;50:399–403. doi: 10.3928/00220124-20190814-05. [DOI] [PubMed] [Google Scholar]
- 6.Bray L. Improving cranial ultrasound scanning strategy in neonates. BMJ Qual Improv Rep. 2016;5(1):u210346.w4219. doi: 10.1136/bmjquality.u210346.w4219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Gagne JC, Park HK, Hall K, et al. Microlearning in health professions education: scoping review. JMIR Med Educ. 2019;5:e13997. doi: 10.2196/13997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eppler F, Monninger M, Schempf B, et al. One minute wonder – Fachwissen to go [one minute wonder—expertise to go] Notfall Rettungsmed. 2019;22:642–644. doi: 10.1007/s10049-019-00639-w. [DOI] [Google Scholar]
- 9.Fessele K, Fandler M, Popp S. Innovative Fortbildungskonzepte im Schichtdienst [Innovative training concepts for shift work] Intesiv Notfallbehand. 2018;43:83–88. doi: 10.5414/IBX00524. [DOI] [Google Scholar]
- 10.Haslinger-Baumann E, Lang G, Muller G. Influence and correlation of attitude, availability and institutional support to research implementation in nursing practice—results from an exploratory, cross-sectional quantitative study. Pflege. 2015;28:145–155. doi: 10.1024/1012-5302/a000422. [DOI] [PubMed] [Google Scholar]
- 11.Hermes C, Ochmann T. Nursing division on the current intensive care situation in Germany : working group of the nursing division of the German society of medical intensive care and emergency medicine (DGIIN) Med Klin Intensivmed Notfmed. 2020;115:495–497. doi: 10.1007/s00063-020-00705-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herrmann A, Kusma L, Kwiatek A. Warten lohnt sich – Kurzfortbildungen auf der NICU [Worth the wait—short training courses at the NICU] intensiv. 2020;28:131–136. doi: 10.1055/a-1120-7808. [DOI] [Google Scholar]
- 13.Jonker G, Agricola G, Bosman E, et al. Digital interactive learning during idle time at work. Med Educ. 2016;50:1163–1164. doi: 10.1111/medu.13175. [DOI] [PubMed] [Google Scholar]
- 14.Kaltwasser A, Dubb R, Krüger L, et al. One minute wonder as part of the Covid-19 pandemic. 2. 2020. pp. 66–88. [Google Scholar]
- 15.Krüger L. Warten mit Sinn [waiting with meaning] intensiv. 2017;25:246–248. doi: 10.1055/s-0043-113025. [DOI] [Google Scholar]
- 16.Krüger L, Mannebach T. Wartezeiten zur Fortbildung nutzen [Using waiting times for further training] PflegenIntensiv. 2018;15:38–40. [Google Scholar]
- 17.Krüger L, Mannebach T, Wefer F, et al. One minute wonder—inservice training during working hours. HBScience. 2021;12:22–29. doi: 10.1007/s16024-021-00349-9. [DOI] [Google Scholar]
- 18.Lahti M, Kontio R, Pitkanen A, et al. Knowledge transfer from an e-learning course to clinical practice. Nurse Educ Today. 2014;34:842–847. doi: 10.1016/j.nedt.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 19.Lehnen T, Nydahl P, Krüger L. Evaluation der Einminutenfortbildung. Schnelle und effektive Wissensvermittlung [Evaluation of the one minute further education. Fast and effective transfer of knowledge] PflegenIntensiv. 2019;16:48–50. [Google Scholar]
- 20.Meick I. Qualitätsmanagement – Wissensmanagement in der Endoskopie [Quality management—knowledge management in endoscopy] Endo-Praxis. 2018;34:141–145. doi: 10.1055/a-0589-6757. [DOI] [Google Scholar]
- 21.Mueller M, Seidl N. Advanced and continuing education is an important indicator of professional satisfaction in nursing. Pflege. 2000;13:381–388. doi: 10.1024/1012-5302.13.6.381. [DOI] [PubMed] [Google Scholar]
- 22.Nevalainen M, Lunkka N, Suhonen M. Work-based learning in health care organisations experienced by nursing staff: a systematic review of qualitative studies. Nurse Educ Pract. 2018;29:21–29. doi: 10.1016/j.nepr.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 23.Rowlinson J. The one minute wonder network. Clin Teach. 2014;11:332–335. doi: 10.1111/tct.12160. [DOI] [PubMed] [Google Scholar]
- 24.Saffari M, Sanaeinasab H, Masoumbeigi H, et al. An education-based text messaging program to improve nurses’ knowledge, attitude, and practice related to nosocomial infections in intensive care settings. J Contin Educ Nurs. 2019;50:211–217. doi: 10.3928/00220124-20190416-07. [DOI] [PubMed] [Google Scholar]
- 25.Toonstra AL, Nelliot A, Aronson Friedman L, et al. An evaluation of learning clinical decision-making for early rehabilitation in the ICU via interactive education with audience response system. Disabil Rehabil. 2017;39:1143–1145. doi: 10.1080/09638288.2016.1186751. [DOI] [PubMed] [Google Scholar]
- 26.Turk T, Elhady MT, Rashed S, et al. Quality of reporting web-based and non-web-based survey studies: what authors, reviewers and consumers should consider. PLoS ONE. 2018;13:e0194239. doi: 10.1371/journal.pone.0194239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zoelch C, Berner V-D, Thomas J. Gedächtnis und Wissenserwerb [Memory and knowledge acquisition] In: Urhahne D, Dresel M, Fischer F, editors. Psychologie für den Lehrberuf [Psychology for teaching] Berlin, Heidelberg: Springer; 2019. pp. 23–52. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table E1: Criteria for reporting electronical surveys