ABSTRACT
Background: Recent evidence showed adverse mental health outcomes associated with the COVID-19 pandemic, including trauma-related symptoms. The Global Psychotrauma Screen (GPS) is a brief instrument designed to assess a broad range of trauma-related symptoms with no available validation in the Italian population.
Aims: This study aimed to examine the factor structure of the Italian version of the GPS in a general population sample exposed to the COVID-19 pandemic and to evaluate trauma-related symptoms in the context of COVID-19 related risk factors associated with lockdown measures.
Methods: We conducted a cross-sectional web-based observational study as part of a long-term monitoring programme of mental health outcomes in the general population. Eighteen thousand one hundred forty-seven participants completed a self-report online questionnaire to collect key demographic data and evaluate trauma-related symptoms using the GPS, PHQ-9, GAD-7, ISI, and PSS. Validation analyses included both exploratory and confirmatory factor analysis and correlation analyses. The relation with putative COVID-19 related risk factors was explored by multivariate regression analysis.
Results: Exploratory factor analyses supported a two-factor model. Confirmatory factor analysis showed that the best fitting model was a three-factor solution, with core Post-traumatic Stress Symptoms (PTSS) (re-experiencing, avoidance, hyperarousal), Negative Affect (symptoms of depressed mood, anxiety, irritability), and Dissociative symptoms. GPS Risk factors and specific COVID-19 related stressful events were associated with GPS total and the three factor scores.
Conclusions: Our data suggest that a wide range of trauma-spectrum symptoms were reported by a large Italian sample during the COVID-19 pandemic. The GPS symptoms clustered best in three factors: Negative Affect symptoms, Core PTSS, and Dissociative symptoms. In particular, high rates of core PTSS and negative affect symptoms were associated with the COVID-19 pandemic in Italy and should be routinely assessed in clinical practice.
KEYWORDS: Trauma-spectrum symptoms, post-traumatic stress symptoms, covid-19, post-traumatic stress disorder
HIGHLIGHTS
• This study examines the factor structure of the Global Psychotrauma Screen.
• Data were collected during the first COVID-19 lockdown in Italy.
• A three-factor model was the best solution.
• Core Post-Traumatic and Negative Affect symptoms were associated with the COVID-19 pandemic.
Antecedentes: Evidencias recientes revelaron resultados adversos para la salud mental asociados con la pandemia de COVID-19, incluyendo síntomas relacionados con el trauma. El Mapeo Global de Psicotrauma (GPS, en sus siglas en inglés) es un breve instrumento diseñado para evaluar una amplia gama de síntomas relacionados con el trauma, sin validación disponible en la población italiana.
Objetivos: El objetivo de este estudio fue examinar la estructura de factores de la versión italiana del GPS en una muestra de la población general expuesta a la pandemia de COVID-19 y evaluar los síntomas relacionados con el trauma en el contexto de los factores de riesgo relacionados con COVID-19 asociados con las medidas de confinamiento.
Métodos: Realizamos un estudio observacional transversal basado en la web como parte de un programa de vigilancia a largo plazo de los resultados de salud mental en la población general. Dieciocho mil ciento cuarenta y siete participantes completaron un cuestionario en línea de autorreporte para recopilar datos demográficos claves y evaluar los síntomas relacionados con el trauma utilizando el GPS, PHQ-9, GAD-7, ISI y PSS. Los análisis de validación incluyeron análisis factoriales y de correlación tanto exploratorios como confirmatorios. La relación con los posibles factores de riesgo relacionados con COVID-19 se exploró mediante un análisis de regresión multivariante.
Resultados: Los análisis factoriales exploratorios apoyaron un modelo de dos factores. El análisis factorial confirmatorio mostró que el modelo que mejor se ajustaba era una solución de tres factores, con los principales síntomas de estrés postraumático (PTSS, en sus siglas en inglés) (reexperimentación, evitación, hiperactivación), el efecto negativo (síntomas de depresión, ansiedad, irritabilidad) y los síntomas disociativos. Los factores de riesgo del GPS y los eventos estresantes específicos relacionados con COVID-19 se asociaron con el total del GPS y las tres puntuaciones de los factores.
Conclusiones: Nuestros datos sugieren que una amplia gama de síntomas de espectro traumático fueron reportados por una gran muestra italiana durante la pandemia de COVID-19. Los síntomas del GPS se agruparon mejor en tres factores: Síntomas de Afecto Negativo, PTSS Central y Síntomas Disociativos. En particular, las altas tasas de PTSS central y los síntomas de afecto negativo se asociaron con la pandemia de COVID-19 en Italia y deben ser evaluados rutinariamente en la práctica clínica.
PALABRAS CLAVE: síntomas del espectro traumático, síntomas de estrés postraumático, COVID-19, trastorno de estrés postraumático
Short abstract
背景: 最新证据显示, 不良心理健康结果与COVID-19疫情相关, 包括创伤相关症状。全面心理创伤筛查 (GPS) 是一个旨在评估广泛性创伤相关症状的简短工具, 但尚未在意大利人群中进行效度验证。
目的: 本研究旨在考查暴露于COVID-19疫情的一般人群样本中意大利语版GPS的因子结构, 并在与封锁措施相关的COVID-19相关风险因素背景下评估创伤相关症状。
方法: 我们进行了基于网络的横断面观察研究, 作为对一般人群心理健康结果长期监控计划的一部分。 18147名参与者完成了一份在线自我报告问卷, 以使用GPS, PHQ-9, GAD-7, ISI和PSS收集关键的人口统计学数据并评估创伤相关症状。效度分析包括探索性和确认性因子分析以及相关性分析。通过多元回归分析探讨了与假定COVID-19相关风险因素的关系。
结果: 探索性因子分析支持两因子模型。验证性因子分析表明, 最佳拟合模型是三因子模型:核心创伤后应激症状 (PTSS) (再体验, 回避, 高唤起), 负性情绪 (情绪低落, 焦虑, 易激惹症状) 和解离症状。 GPS风险因素和COVID-19相关特定压力事件与GPS总分及三个因子得分相关。
结论: 我们的数据表明, 在COVID-19疫情期间, 多种创伤谱系症状在一个大型意大利人样本中被报告。 GPS症状最好被划分为以下三个因子簇:负性情绪症状, 核心PTSS和解离症状。特别地, 在意大利核心PTSS高发生率和负性情绪症状与COVID-19疫情有关, 应在临床实践中定期测评。
关键词: 创伤谱系症状, 创伤后应激症状, COVID-19, 创伤后应激障碍
1. Introduction
The 2019 coronavirus (COVID-19) pandemic is a global health emergency with a severe impact on public health, including mental health (Brooks et al., 2020). At the time this paper was written, the pandemic was involving Europe, with Italy being the first country to be hit, leading to the implementation of unprecedented preventive measures aimed at containing the spread of infections. By the first ten days of March 2020, the Italian Government imposed lockdown measures on the national territory. People were asked to stay at home and socially isolate themselves to prevent contagion.
It has been previously shown that health emergencies such as epidemics can lead to detrimental and long-lasting psychosocial consequences. Epidemics are associated with a wide range of psychiatric comorbidities at the individual level, including anxiety, panic, depression, and trauma-related disorders (Tucci et al., 2017). Health emergencies’ psychosocial impact seems to be even higher during quarantine measures (Brooks et al., 2020). Quarantine was associated with high stress levels (DiGiovanni, Conley, Chiu, & Zaborski, 2004), depression (Hawryluck et al., 2004), irritability, and insomnia (Lee, Chan, Chau, Kwok, & Kleinman, 2005). Further, being quarantined was a predictor of acute stress (Bai et al., 2004) and trauma-related (Wu et al., 2009) disorders, particularly in specific at-risk populations such as health-care workers. Trauma-related symptoms may persist long after the actual emergency has ended, thus representing a long-lasting threat to mental health. In the context of the current COVID-19 pandemic, an online survey on 1210 Chinese subjects during the initial stage of the disease reported moderate to severe stress levels in 8,1% of the respondents (Wang et al., 2020). A month after the COVID-19 outbreak, the prevalence of PTSD symptoms was 7% in a sample of 285 participants from China’s hardest-hit areas (Liu et al., 2020). In a nationwide survey, including more than 50.000 Chinese respondents, almost 35% of the participants reported trauma-related distress symptoms (Qiu et al., 2020).
Demographic risk factors for mental health outcomes, such as female gender, have been well established (Olff et al., 2017). Also, in the context of the current pandemic, Liu et al. (2020) also reported significantly higher post-traumatic stress symptoms (PTSS) in women, particularly in the domains of re-experiencing, alterations in cognition and mood, and hyperarousal (Liu et al., 2020). Also, female and young adults showed significantly higher psychological distress (Qiu et al., 2020). Furthermore, anxiety and stress disorders’ incidence was high in front-line medical staff (Huang, Han, Luo, Ren, & Zhou, 2020). Among Chinese health-care workers, women, nurses, front-line workers, and those who worked in the hardest-hit areas were at higher risk of adverse mental health outcomes, including anxiety, insomnia, and distress (Lai et al., 2020), while social support positively affected stress, anxiety and self-efficacy levels in medical staff (Xiao, Zhang, Kong, Li, & Yang, 2020). In addition to the lack of social support, other well-known risk factors for post-traumatic stress reactions include socioeconomic status, a history of psychotrauma or psychiatric diagnoses, or specific event characteristics (Olff et al., 2019)
No study to date has investigated the range of trauma-related symptoms and associated risk factors of the COVID-19 pandemic in the Italian population. Implementing strict lockdown and social distancing measures is expected to impact on a wide range of mental health symptoms significantly.
Recently, the Global Collaboration on Traumatic Stress (www.global-psychotrauma.net) developed the Global Psychotrauma Screen (GPS) (Olff et al., 2020; Schnyder et al., 2017), a brief instrument designed to assess trauma-related symptoms as well as associated risk and protective factors. GPS consists of 17 items encompassing different symptoms domains (i.e. PTSD and complex PTSD, depression, anxiety, sleep problems, self-injurious behaviour, dissociation, other physical, emotional, or social problems, and substance abuse) and five risk or protective factors (i.e. other stressful events, childhood trauma, history of mental illness, social support and resilience. The first data suggest good internal reliability and concurrent validity with instruments measuring trauma-related domains (Olff et al., 2020). Therefore, the instrument has the potential to represent a brief screening measure of a range of psychotrauma-related symptoms in a variety of populations, not limited to core PTSD symptoms.
This study examines the factor structure of the Italian version of the GPS in a general population sample exposed to the COVID-19 pandemic. Further, we aimed at evaluating trauma-related symptoms and mental health risk factors, including specific COVID-19 related risk factors, associated with the implementation of lockdown measures and social distancing in Italy.
2. Methods
2.1. Study design
This cross-sectional web-based study is a part of a long-term monitoring programme of mental health outcomes in the general population (Rossi et al., 2020a). Approval for this study was obtained from the local IRB at the University of L’Aquila. Online consent was obtained from the participants. Participants were allowed to terminate the survey at any time they desired. The survey was anonymous, and confidentiality of information was assured.
Three weeks after the beginning of the lockdown, a survey was conducted among a self-selected sample. Every person living in Italy ≥ 18 years was eligible. Participants were invited using sponsored social network advertisements together with a snowball recruiting technique. A Facebook post containing a link to the questionnaire was spread using the University of L’Aquila Facebook page and advertised using Facebook Ads in order to be displayed on about 1 million user’s feed between March 27th and April 6th, 2020. Data were collected using an online questionnaire developed using the free software Google Forms®. According to epidemiological data confirmed by the World Health Organization, the investigated timeframe corresponds to Italy’s contagion peak (World Health Organization, 2020).
2.2. Study sample
A total of 18,147 individuals completed the questionnaire, of which 14,447 (79.6%) women, the median age was 38 (IQR = 23). Because of the web-based design, no response rate could be estimated as it was not possible to estimate how many persons were reached by social network advertisements.
2.3. Measures
2.3.1. Global psychotrauma screen
The Global Psychotrauma Screen (GPS) (Olff et al., 2020; Oe et al., in press) is a 22 self-report instrument with a dichotomous answer format that covers both stress-related symptoms and risk and protective factors. Symptoms investigated are (17 items): post-traumatic stress symptoms (PTSS), disturbances in self-organization (DSO), anxiety, depression, sleep problems, dissociation, self-harm, substance abuse, and other physical, emotional, or social problems. Risk and protective factors are (5 items): other stressful events, childhood trauma, history of mental illness, social support, and psychological resilience. The following scores were derived from the GPS: 1) ‘GPS symptoms’ (GPS-Sym): the sum of all 17 symptoms items 2) ‘GPS risk/protection index’ (GPS-RP): the sum of the five risk/protection items. In order to address COVID-related post-traumatic symptoms, items 1 and 2, regarding re-experiencing and avoidance, respectively, were slightly rephrased, referring to COVID-specific events or situations.
2.3.2. Patient Health Questionnaire
Depressive symptoms were assessed using the 9-item Patient Health Questionnaire (PHQ-9). PHQ-9 comprises nine depressive symptoms, rated on a 4-point Likert scale, range 0–27 (Spitzer, Kroken, & Williams, 1999). The total score has been taken into consideration as a continuous variable. PHQ-9 is a widely used instrument in epidemiological research as a depression screener. In our sample, internal consistency was α = 0.87.
2.3.3. Generalized anxiety disorder questionnaire
Anxiety symptoms were assessed using the 7-item Generalized anxiety disorder questionnaire (GAD-7), rated on a 4-point Likert scale, range 0–21 (Spitzer, Kroenke, Williams, & Löwe, 2006). The total score has been taken into consideration as a continuous variable. GAD-7 is a widely used instrument in epidemiological research as an anxiety screener. In our sample, internal consistency was α = 0.91.
2.3.4. Insomnia severity index
The Insomnia Severity Index (ISI) is a 7-item self-report questionnaire assessing the nature, severity, and impact of insomnia, on a 5-point Likert scale, range 0–28, with higher scores indicating higher severity of insomnia symptoms (Bastien, Vallières, & Morin, 2001; Castronovo et al., 2016). The total score has been taken into consideration as a continuous variable. ISI is a widely used instrument to evaluate sleep disorders. In our sample, internal consistency was α = 0.90.
2.3.5. Perceived stress scale
The 10-item Perceived Stress Scale (PSS) was used to assess subjectively perceived stress on a 5-point Likert scale, range 0–50 (Mondo, Sechi, & Cabras, 2019). Internal consistency in our sample was α = 0.87.
2.3.6. COVID-19 related risk factors
In this study, we addressed the impact of the COVID-19 pandemic and related lockdown measures exploring COVID-19 related stressful events that had previously shown an association with mental health outcomes (Rossi et al., 2020b; Shi et al., 2020; Wang et al., 2020, p. 1) lockdown status, i.e. lockdown as imposed by the Government, being under quarantine because infected or exposed to an infected person, hospitalized;
2) any change in working activity due to the COVID-19 pandemic, i.e. working as usual, working from home, working activity discontinued, working more than usual;
3) having a loved one infected, hospitalized, or deceased due to COVID-19;
4) Any other stressful life event due to pandemic or lockdown, including financial, one’s own or a loved one’s health, work/study, relational, housing, or caregiving problems.
Finally, gender, age, job, education, and region of residence were collected as demographic variables.
2.4. Analytic plan
All analyses were performed using Stata 16® (StataCorp). The analytic plan was based on a split-sample exploratory/confirmatory factor analysis approach. According to a standard procedure in psychometric analyses (Kyriazos, 2018) the sample was randomly half-split into two halves that were checked for homogeneity on key variables (age, gender, region, exposure to key risk factors, PHQ, GAD GPS total scores) using t-test or χ2 as appropriate. The two halves consisted of 9073 and 9074 subjects and no difference was observed in the selected variables.
Firstly, an exploratory factor analysis (EFA) on the GPS symptoms was conducted using maximum-likelihood estimation, followed by oblique promax rotation, to allow correlations between factors. Standard factor analyses are based on a matrix of Pearson’s correlations and assume that the variables are continuous and follow a multivariate normal distribution. Because the GPS has 0/1 response items, a factor analysis based on tetrachoric correlations was performed.
Factor retention was firstly based on Eigenvalue > 1, followed by a likelihood-ratio test in order to compare a model with k factors resulting from Eigenvalues inspection vs. a model with k-1 factors. The internal consistency of the extracted factors was examined using Cronbach’s alpha, with the threshold of.7 used to indicate acceptable reliability. Furthermore, item-test and item-rest correlations were estimated as measures of reliability. Barlett’s sphericity test and Kaiser–Meyer–Olkin (KMO) measure were inspected to ascertain data suitability for factor analysis.
Secondly, to assess the GPS-Sym’s internal validity, a confirmatory factor analysis (CFA) was conducted on three models selected according to previous evidence, current EFA results, and theoretical principles of trauma-related psychopathology. The first model is a single-factor solution with all of the items loading on a single factor, as proposed in a recent EFA of the GPS (Frewen et al. submitted). The second model is a two-factor solution resulting from our EFA. Finally, we tested a third model that jointly took into account ICD-11 and DSM 5 models, in which 1. core PTSD symptoms (PTSS) (i.e. re-experiencing, hyperarousal and avoidance) are grouped onto a single factor, 2. DSO symptoms, anxiety and depression, as well as disorder unspecific psychopathological symptoms (including sleep problems, other physical and psychological problems), are loaded on a second factor, and 3. dissociative symptoms loaded on a third factor (Birkeland, Greene, & Spiller, 2020; Cloitre, Garvert, Brewin, Bryant, & Maercker, 2013; Hyland, Shevlin, Fyvie, & Karatzias, 2018).
Theoretically, according to a three-factor solution, one might expect core PTSS and DSO to load on different factors, as proposed in the ICD-11 organization of PTSD and Complex PTSD (cPTSD) (Cloitre et al., 2018). Simultaneously, if the ‘PTSD with dissociative symptoms’ specifier, as introduced in the DSM 5 (van Huijstee & Vermetten, 2017), would be a relevant distinction, this would result in the dissociative symptoms to load on a third separate factor.
CFA was fitted using a tetrachoric covariance matrix. Model parameter appraisal used weighted least square (WLS) estimation, as WLS is considered a better option compared to maximum likelihood estimation when dealing with binary variables. Residual covariances between the GPS items were specified in the CFA models after inspecting modification indices and only if covariances reflected a theoretically sound association and if of magnitude ≥0.2.
Goodness-of-fit (GOF) was evaluated using chi-square test, Comparative Fit Index (CFI), Standardized Root-Mean-Square Residual (SRMR), Root-Mean-Square Error of Approximation (RMSEA), and Tucker-Lewis Index (TLI).
After establishing the best fitting factor structure of the GPS-Sym, the appropriate factor scores were calculated as the sum score of each factor’s endorsed items. Factor scores were preferred over latent factors in order to provide a more reproducible scoring system.
Descriptive statistics of the resulting GPS factors, as well as the overall sum score in our sample, were conducted.
In order to assess convergent validity with depression and anxiety symptoms and insomnia, Pearson’s correlations between GPS-Sym resulting factor sub-scores with PHQ GAD and ISI were performed. Divergent validity was assessed by correlation with the PSS.
Finally, in order to assess the association of the GPS factors with different COVID-19 related stressors, the GPS factors were introduced as dependent variables in a panel of seemingly unrelated regression (SURE) models with the following independent variables:
Any change in job activity due to COVID-19 lockdown, including discontinued working activity
personal lockdown/quarantine/hospitalized status,
having a loved one infected, hospitalized, or deceased by COVID-19.
Any of the following stressful life events due to COVID-19: economic, work/study, housing, relational problems, own’s or a loved one health, problems associated with caregiving.
Furthermore, the following covariates were introduced: age, gender, education, region, relational status, occupation, and GPS-RP total score. These covariates were selected as being associated with mental health outcomes during the COVID-19 pandemic (Wang et al., 2020), the region of residence was included to account for the large regional differences in COVID-19 pandemic impact in Italy (Dipartimento Della Protezione Civile, 2020). Parallel to this analysis, a multiple regression was conducted to test the association on GPS-Sym with the aforementioned putative risk factors and covariates.
Seemingly Unrelated Regression Models (SURE) are multivariate regression techniques that jointly model a set of regression equations in which cross-equation error terms are not uncorrelated. Although there was no difference in using SURE models compared to fitting a sem model with CFA and risk factors altogether, given the categorical nature of most of our independent variables, results of SURE models would produce easier to interpret. SURE models were estimated using the – sureg- command in Stata (UCLA: Statistical Consulting Group.).
Missing data for CFA and SURE models were treated conducting a multiple imputation by chained equations (MICE) using the -ice- command suite for Stata, with M = 50 cycles of imputation. As MICE is a technique designed for obtaining point estimates and standard errors, only CFA coefficients and no fit indices were recalculated using MI data.
3. Results
3.1. Demographic and mental health characteristics of the sample
The demographic characteristics of the sample are reported in Table 1. A total of 18,147 participants completed the questionnaire, 14,448 (79.6%) women and 3699 (20.38%) men. Regional distribution was very similar to national demographical data, with 7991 (44%) participants from Northern Italy, 4695 (25.9%) from Central Italy, and 5175 (28.52%) from Southern Italy. Missing data affected 11% of observation and were treated by simple listwise deletion.
Table 1.
Sample characteristics
| No./Median (%/IQR) | |
|---|---|
| Age | 38 (23) |
| Gender | |
| Women | 14,448 (79.61) |
| Men | 3699 (20.38) |
| Education | |
| ≤Undergraduate | 8682 (47.84) |
| ≥Graduate | 7795 (42.95) |
| Lower education | 1670 (9.20) |
| Occupation | |
| Housemaker | 1155 (6.36) |
| Unemployed | 2127 (11.72) |
| Employed | 10,984 (60.53) |
| Retired | 293 (1.61) |
| Student | 3588 (19.77) |
| Region | |
| North | 7991 (44.03) |
| Centre | 4695 (25.87) |
| South | 5175 (28.52) |
| Missing | 286 (1.58) |
| Lockdown/quarantine | |
| Lockdown | 17,486 (96.36) |
| Quarantine | 148 (0.8) |
| Missing | 513 (2.83) |
| Working activity change | |
| As usual | 2349 (12.94) |
| aSmart-working | 6804 (37.49) |
| Discontinued | 7601 (41.89) |
| More than usual | 672 (3.7) |
| Missing | 721 (3.97) |
| Loved one’s status | |
| Not infected, deceased or Hospitalized | 16,576 (91.34%) |
| Infected | 801 (4.41) |
| Deceased | 254 (1.4) |
| Hospitalized | 428 (2.36) |
| Missing | 88 (0.48) |
| GPS-Risk/Protective Items | |
| Other stressful life events | 9325 (51.39) |
| Poor Social Support | 6949 (38.29) |
| Early adverse life events | 8637 (47.59) |
| History of mental illness | 5114 (28.18) |
| Poor Resilience | 3761 (20.73) |
asmart working refers to working online from home.
Figure 1 shows the endorsement of individual GPS symptoms. In the total sample, mean (standard deviation, SD) were for GPS-Sym: 7.2 (3.83), GPS-RP: 1.86 (1.23); GPS-total: 9.1 (4.5); PHQ-9: 10.58 (6.31); GAD-7: 9.0 (5.9); PSS 24.54 (8.32) and ISI 10.23 (7.2)(see Supplementary Table S1 for further details). As a reference, the reader may consider that for PHQ-9 Scores of 5, 10, 15 and 20 represent cutpoints for mild, moderate, moderately severe and severe depression, respectively. For GAD-7 scores of 5, 10 and 15 represent cutpoints for mild, moderate and severe anxiety, respectively. For ISI, a score of 22 represents the cutpoint for severe insomnia.
Figure 1.
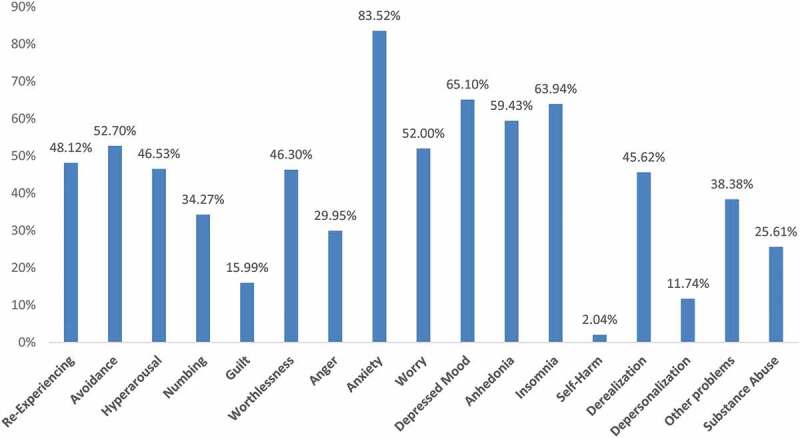
Percentage of endorsement of GPS-Sym items
3.2. EFA
Due to missing data, EFA was performed on a total of 8819 subjects. The Kaiser–Meyer–Olkin (KMO) measure confirmed the sampling adequacy for the analysis (KMO = 0.90) and Bartlett’s test of sphericity [=25,130.32, p < .001] suggested that correlations between items were suitably large, confirming the appropriateness of the analysis. Tetrachoric factor analysis with Promax rotation suggested a two-factor solution (Tables 2–3) with three core PTSD symptoms, two anxiety symptoms (feeling anxious and worrying,), guilt ideation, depressed mood and sleep problems loading on factor 1, and all the remaining items (numbing, worthlessness, irritability, anhedonia, self-harm, dissociation, other physical problems and substance misuse) loading on the second factor. In this solution, item 5 (guilt) had similarly low loadings on both factors (0.32 and 0.26).
Table 2.
Exploratory factor analysis
| Factor | Eigenvalue | Difference | Proportion | Cumulative |
|---|---|---|---|---|
| Factor1 | 5.401 | 3.582 | 0.443 | 0.443 |
| Factor2 | 1.818 | 1.166 | 0.149 | 0.592 |
| Factor3 | 0.652 | −0.201 | 0.054 | 0.646 |
| Factor4 | 0.853 | −0.083 | 0.070 | 0.716 |
| Factor5 | 0.936 | 0.280 | 0.077 | 0.792 |
| Factor6 | 0.656 | −0.042 | 0.054 | 0.846 |
| Factor7 | 0.698 | 0.030 | 0.057 | 0.903 |
| Factor8 | 0.668 | 0.367 | 0.055 | 0.958 |
| Factor9 | 0.302 | 0.095 | 0.025 | 0.983 |
| Factor10 | 0.207 | . | 0.017 | 1.000 |
Table 3.
Factor loadings, promax rotated
| Variable | Factor 1 | Factor 2 | Uniqueness | |
|---|---|---|---|---|
| GPS02 | Avoidance | 0.8233 | 0.4604 | |
| GPS01 | Re-experiencing | 0.8038 | 0.4487 | |
| GPS08 | Anxiety | 0.7333 | 0.2411 | |
| GPS03 | Hyperarousal | 0.6805 | 0.6319 | |
| GPS09 | Worry | 0.6058 | 0.3579 | |
| GPS10 | Depressed mood | 0.5095 | 0.2957 | |
| GPS12 | Insomnia | 0.484 | 0.6271 | |
| GPS05 | Guilt | 0.3281 | 0.7296 | |
| GPS13 | Self-harm | 0.8866 | 0.3456 | |
| GPS04 | Numbing | 0.6019 | 0.7183 | |
| GPS11 | Anhedonia | 0.5425 | 0.5347 | |
| GPS06 | Worthlessness | 0.5212 | 0.5822 | |
| GPS15 | Depersonalization | 0.4825 | 0.7098 | |
| GPS16 | Other problems | 0.4666 | 0.6073 | |
| GPS18 | Substance Abuse | 0.4523 | 0.7098 | |
| GPS07 | Anger | 0.4415 | 0.5636 | |
| GPS14 | Derealization | 0.3379 | 0.7644 | |
| Cronbach’s Alpha | 0.76 | 0.66 | ||
| Avg. Interitem Corr | 0.06 | 0.03 | ||
This solution explained 45.13% of the total variance.
3.3. CFA
Fit indices from CFA are reported in Table 4; the models’ coefficients with MI results are reported in table S2. No residual covariance met the pre-specified criteria for inclusion, so none was added to the models. Solution 1 had suboptimal fit indices, Solution 2 had intermediate fit indices, while Solution 3 had the best fit indices. Depending on the index considered, Solution 3 showed good (RMSEA<0.05, SRMR<0.08) to mediocre (CFI and TLI<0.9) fit. χ2 difference test confirmed solution three as the best fitting model, which was selected for subsequent analyses. CFA results did not vary using MI.
Table 4.
Confirmatory factor analysis fit indices
| Fit statistic | 1-factor model | two-factor model | three-factor model |
|---|---|---|---|
| χ2 | χ2(119) = 2537.5 | χ2(118) = 2343.91 | χ2(116) = 1725.5 |
| RMSEA [90%CI] | 0.048 [0.046, 0.049] | 0.046 [0.044, 0.048] | 0.040 [0.038, 0.041] |
| CFI | 0.769 | 0.788 | 0.847 |
| TLI | 0.736 | 0.755 | 0.820 |
| SRMR | 0.082 | 0.075 | 0.070 |
| CD | 0.857 | 0.893 | 0.944 |
χ2difference test, model 1 vs model 2: χ2(1) = 193.6, p < 0.001.
χ2difference test, model 1 vs model 3: χ2(3) = 812, p < 0.001.
χ2difference test, model 2 vs model 3: χ2(2) = 618.4 p < 0.001.
Correlations between PHQ, GAD, ISI and PSS and GPS-Sym and the factors obtained from the EFA are shown in Table 5.
Table 5.
Pairwise correlations
| three-factor model |
||||
|---|---|---|---|---|
| PTSS | Negative Affect | Dissociation | GPS-Sym | |
| PHQ-9 | 0.39 | 0.77 | 0.39 | 0.76 |
| GAD-7 | 0.50 | 0.76 | 0.38 | 0.78 |
| ISI | 0.37 | 0.58 | 0.27 | 0.59 |
| PSS | 0.46 | 0.74 | 0.33 | 0.74 |
PTSS: Post-Traumatic symptoms; Global Psychotrauma Scale – total symptom score; PHQ-9: Patient Health Questionnaire; GAD-7: Generalized Anxiety Disorder Questionnaire; ISI: Insomnia Severity Index; PSS: Perceived Stress Scale.
All correlation coefficients were statistically significant (p < 0.001). Results from pairwise correlations showed a strong correlation of both Depression-S1 and Depression-S2 with the PHQ (r = 0.75 in both cases) and GAD total score (r = 0.71 and r = 0.75), PTSS-S1 showed a slightly higher correlation with GAD compared with PTSS-S2 (r = 0.66 vs. r = 0.56). Dissociation showed moderate to small correlation with PHQ, GAD, ISI and PSS (r < 0.4).
3.4. Trauma spectrum in the population and its relationship with general and COVID-19 related risk factors
The raw and averaged scores of the three resulting GPS factors were calculated and reported in Table 6. Scores were averaged in order to be more easily comparable between each other.
Table 6.
Raw and averaged scores of the GPS factors
| Raw scores |
Averaged Scores |
|||||
|---|---|---|---|---|---|---|
| Variable | Mean | SD | Range | Mean | SD | Range |
| Negative Affect | 5.15 | 2.83 | 0–12 | 0.43 | 0.23 | 0–1 |
| PTSS | 1.47 | 1.13 | 0–3 | 0.49 | 0.37 | 0–1 |
| Dissociation | 0.57 | 0.66 | 0–2 | 0.28 | 0.33 | 0–1 |
| GPS-sym | 7.19 | 3.83 | 0–17 | 0.42 | 0.22 | 0–1 |
| GPS-Tot | 9.06 | 4.5 | 0–22 | 0.41 | 0.20 | 0–1 |
The relationship between GPS factors Negative Affect, PTSS, and Dissociation and several risk factors was assessed by seemingly unrelated linear regression (sureg) analysis (see Table 7). Parallel to the sureg model, a multiple regression model was fitted with the same independent variables on GPS-Sym. Due to missingness, the final SURE model was estimated on data from 17,231 respondents. In order to have more easily interpretable results, dependent variables scores were standardized. Younger age and female gender were associated with Negative Affect, PTSS, and Dissociation. Compared to being in lockdown, being under quarantine because infected or exposed to someone infected was associated with both Negative Affect and PTSS. Participants from Southern Italy had higher PTSS symptoms than participants from Northern or Central Italy. Being a housemaker was associated with Negative Affect and PTSS while being a student was associate with lower PTSS. Having experienced any stressful life event due to COVID-19 was associated with Negative Affect, PTSS, and Dissociation. ‘Working more than usual’ was associated with PTSS and dissociation. Having a loved one deceased by COVID-19 was associated with Negative Affect and PTSS. Having a loved one hospitalized was associated with PTSS. GPS-RP was associated with Negative Affect, PTSS, and Dissociation. Multiply imputed data showed no relevant differences due to missing data (Table S2).
Table 7.
Demographic and risk/protective factors as predictors of GPS scores (N = 17,231)
| Variable |
PTSSa b [95% CI] |
Negative affecta b [95% CI] |
Dissociationa b [95% CI] |
GPS-Symb b [95% CI] |
|---|---|---|---|---|
| Any Stressful Event Due To COVID-19 | 0.13*** [0.10,0.16] | 0.22*** [0.19,0.24] | 0.12*** [0.09,0.15] | 0.85*** [0.74,0.95] |
| Working Activity change due to COVID-19 | ||||
| As Usual | ref | |||
| Smart Working c | 0.06* [0.01,0.11] | 0.08*** [0.03,0.12] | 0.05 [−0.01,0.10] | 0.28*** [0.12,0.44] |
| Discontinued | 0.08*** [0.03,0.13] | 0.10*** [0.06,0.14] | −0.01 [−0.05,0.04] | 0.33*** [0.17,0.48] |
| More Than Usual | 0.21*** [0.12,0.30] | 0.11* [0.02,0.19] | 0.09 [−0.01,0.18] | 0.55*** [0.23,0.86] |
| Loved One Involved w/COVID-19 | ||||
| Not infected/deceased/hospitalize | ref | |||
| Infected | 0.08* [0.01,0.15] | 0.03 [−0.03,0.10] | 0.05 [−0.03,0.12] | 0.24 [−0.01,0.48] |
| Deceased | 0.25*** [0.13,0.38] | 0.16** [0.05,0.27] | 0.08 [−0.05,0.21] | 0.82*** [0.40,1.24] |
| Hospitalized | 0.16** [0.06,0.26] | 0.02 [−0.07,0.10] | −0.01 [−0.10,0.09] | 0.22 [−0.11,0.55] |
| Lockdown Status | ||||
| Lockdown | ref | |||
| Quarantine | 0.20* [0.04,0.37] | 0.26*** [0.11,0.41] | −0.06 [−0.23,0.11] | 0.91** [0.35,1.48] |
| Hospitalized | −0.31 [−1.24,0.63] | 0.17 [−0.67,1.00] | 0.39 [−0.56,1.34] | 0.48 [−2.42,3.38] |
| Age (Reversed) | 0.04*** [0.02,0.06] | 0.22*** [0.20,0.23] | 0.05*** [0.03,0.07] | 0.69*** [0.63,0.76] |
| Female | 0.39*** [0.36,0.43] | 0.26*** [0.23,0.29] | 0.20*** [0.17,0.24] | 1.33*** [1.20,1.45] |
| Region | ||||
| North | ref | |||
| Centre | −0.02 [−0.06,0.01] | −0.03 [−0.06,0.01] | −0.03 [−0.07,0.00] | −0.11 [−0.24,0.01] |
| South | 0.17*** [0.14,0.21] | 0.07*** [0.04,0.10] | 0.05** [0.02,0.09] | 0.42*** [0.30,0.54] |
| Education | ||||
| ≥Graduate | ref | |||
| Undergraduate | 0.05** [0.02,0.08] | 0.05** [0.02,0.07] | 0.11*** [0.08,0.15] | 0.27*** [0.16,0.38] |
| Lower Education | 0.06* [0.00,0.11] | 0.07** [0.02,0.12] | 0.17*** [0.11,0.23] | 0.43*** [0.24,0.62] |
| In A Relationship | 0.11*** [0.08,0.14] | 0 [−0.03,0.03] | −0.04* [−0.08,-0.01] | 0.11 [−0.00,0.22] |
| Occupation | ||||
| Employed | ref | |||
| Housemaker | 0.15*** [0.08,0.21] | 0.10*** [0.04,0.16] | −0.03 [−0.10,0.04] | 0.46*** [0.24,0.69] |
| Unemployed | 0 [−0.05,0.05] | 0.07** [0.03,0.12] | 0.02 [−0.03,0.07] | 0.24** [0.07,0.41] |
| Retired | −0.09 [−0.23,0.05] | 0.06 [−0.07,0.18] | −0.08 [−0.21,0.06] | 0.01 [−0.41,0.44] |
| Student | −0.15*** [−0.20,-0.10] | 0.04* [0.00,0.09] | −0.05 [−0.10,0.00] | −0.07 [−0.24,0.09] |
| GPS-RP | 0.14*** [0.13,0.15] | 0.30*** [0.29,0.31] | 0.15*** [0.13,0.16] | 1.10*** [1.06,1.14] |
aseemingly unrelated regression, the three dependent variables are jointly modelled; b multiple linear regression model. PTSS: Post-Traumatic Stress Symptoms; GPS-Sym: Global Psychotrauma Scale – total symptom score. * p < 0.05; **p < 0.01; ***p < 0.001. c: smart working refers to working online from home.
4. Discussion
This study had the objective to assess the factor structure of the Italian version of the Global Psychotrauma Screen (GPS), which evaluates a wide range of traumatic spectrum symptoms in a large web-based study carried out during the COVID-19 pandemic. Secondly, we explored the association between traumatic spectrum symptoms and COVID-19 related risk factors. This study is an addition to the field of stress and trauma-related disorders, as it allows to detail how a wide range of traumatic symptoms may be associated with exposure to pandemic and lockdown measures in the general population.
The GPS is a brief screening tool but, at the same time, taps a wide range of potential post-traumatic symptoms. Indeed, a broad spectrum of symptoms was endorsed, with only a small minority endorsing the Self-harm item, an item that may be expected more after severe and or long-lasting interpersonal violence. The GPS-Total score was within the same range as found in a more extensive study on child maltreatment (Olff et al., 2020).
Our EFA suggested a two-factor solution with core PTSS, anxious and some depressive symptoms (depressed mood and guilt), and sleep problems on one factor; numbing, dissociation, anger, self-harm, substance abuse and other depressive symptoms (worthlessness and anhedonia) on the other. This solution is not convincing as the four depressive symptoms load on both factors. One possible partial explanation for this could be that Factor 1 includes symptoms that are more frequently associated with single traumatic events and a diagnosis of PTSD, while symptoms loading on Factor 2 are more frequently associated with complex enduring traumatic experiences and cPTSD.
Notwithstanding the EFA results, the CFA shows that a three-factor structure of post-traumatic symptoms has a superior fit, with acceptable to good fit indices. In this model, the first factor encompasses core post-traumatic symptoms (‘PTSS’), such as re-experiencing, avoidance and hyperarousal; the second factor includes depressive and anxious symptoms as well as anger, irritability and sleep disturbances, and was termed ‘Negative Affect’; the third factor includes ‘Dissociative symptoms’, i.e. depersonalization and derealization.
The factor structure emerging from this study needs to be discussed in the light of recent taxonomic advances in stress-related disorders proposed in the International Classification of Diseases – 11th edition (ICD-11) and the diagnostic and Statistical Manual of Mental Disorders 5th edition (DSM 5).
The factor ‘PTSS’ includes the classic PTSD core symptoms, i.e. hyperarousal, re-experiencing and avoidance, similar to those in the ICD-11 PTSD diagnosis. The second factor, i.e. ‘Negative Affect’, includes depressed mood, irritability, anxiety, self-harm, sense of worthlessness, guilt, and substance abuse. This factor partially overlaps with DSM 5 criterion D ‘Negative alterations in mood and cognition’ as well as with the ‘disturbances in self-organization’ (DSO) criteria that characterize complex-PTSD in ICD-11 (Cloitre et al., 2013; Karatzias et al., 2017; Shevlin et al., 2018). Finally, in the GPS, dissociative symptoms constitute a separate factor, coherently with the DSM-5 dissociative specification of PTSD (‘PTSD with dissociative symptoms’) (Hansen, Ross, & Armour, 2017b; Longo, Cecora, Rossi, Niolu, & Siracusano, 2019; Rossi et al., 2019) and with the Dissociative Subtype model of PTSD (Hansen et al., 2017b; Ross, Baník, Dědová, Mikulášková, & Armour, 2018).
The inclusion of cognitive and affective symptoms in the PTSD criteria by DSM 5 has produced a large number of different hypothesized latent factor structures of PTSD, with the result of increased confusion in stress-related disorders taxonomy (Hansen, Hyland, Armour, Shevlin, & Elklit, 2015). At the same time, ICD-11 diagnostic criteria are associated with increased diagnostic accuracy, reducing comorbidities with other traumatic responses (Cloitre et al., 2013; Hansen et al., 2015, 2017a). Furthermore, ICD-11 criteria are associated with a much more limited number of proposed latent structures in the literature (Hansen et al., 2015). Our data support that core PTSD symptoms are separated from affective and cognitive symptoms. This psychometric structure resembles the ICD-11 nosography of trauma-related disorders, with PTSD and cPTSD being two separate disorders, rather than the DSM-5 organization, with the only possible diagnosis being PTSD, which includes affective symptoms, without contemplating cPTSD. A single-factor solution would have been more coherent with the DSM-5 nosography; however, our data do not support this latent structure of the GPS.
Our data add to the theory that affective symptoms are separated from core PTSS and could contribute to a more severe PTSD clinical picture or a distinct disorder like cPTSD. Another relevant aspect of negative affective symptoms is its high centrality in DSM-5 based networks of PTSS, which is thought to underlie some mechanisms underpinning high comorbidities with other mental disorders (Birkeland et al., 2020).
Although the best-fitting model was a three-factor solution, its fit-indices were less-than-optimal: this could be due to several issues, including the strict criteria we set up for specifying residual covariances after inspecting modification indices, that led us not to overfit the model, but it could also depend on the imbalance in item numbers across factors, with the dissociation factor having only two items. Finally, poor fit indices may reflect the sampling strategy, as we recruited a non-clinical population.
Following factor analyses, we assessed how trauma-related symptoms were associated with several risk factors and covariates, including demographic variables, COVID-19 specific factors, and risk-protection GPS factors.
Concerning demographic variables, women were more likely to endorse the GPS total as well as the three symptom-clusters, particularly the PTSS factor, while young age was particularly associated with Negative Affect. This is in line with previous PTSD research (De Vries & Olff, 2009; Dückers & Olff, 2017; Olff, 2017) and with other studies from China that highlight a higher vulnerability for stress-related symptoms in women (Liu et al., 2020a; Qiu et al., 2020; Wang et al., 2020). Other demographic variables associated with higher GPS scores were lower education level and being unemployed or a housemaker, as found in China (Wang et al., 2020). GPS risk and protective factors (including poor social support and a history of trauma and psychiatric disorders or low sense of resilience) were associated with higher symptom profiles.
COVID-19 related stressful events were also associated with the GPS total symptoms and the three factors. Being under quarantine because of being infected or exposed to contagion and losing a loved one due to COVID-19 were associated with higher levels of PTSS and Negative Affect. COVID-19 related stressful events were correlated with the three symptoms clusters. These findings confirm a relevant impact of COVID-19 related events on mental health, even after adjusting for pre-existing risk factors included in the GPS-RP such as early traumatic experiences, previous mental illness, or poor social support. These results warrant close monitoring of the evolution of stress-related symptoms in the general population over time and support the need to enforce community-based mental health interventions.
This study has several limitations. Firstly, it is not a representative population sample. Social-network sampling strategy has its pros and cons. In the context of the COVID-19 pandemic, it was essential to collect a large sample in a very short time as a part of a long-term monitoring programme of mental health outcomes in the general population. However, this web-based survey may have introduced several potential biases, including self-selection bias as suggested by the large disproportion in the gender ratio and the unusually high rate of self-reported lifetime prevalence of a history of mental illness or psychiatric/psychological treatment at around 28% compared to previous evidence (de Girolamo et al., 2006). This may indicate that a vulnerable group in the population is more inclined to participate in a survey on the pandemic’s mental health effects, leading to an overestimation of the prevalence of traumatic-spectrum symptoms. Furthermore, only a limited number of instruments could be included in the survey. Ideally, a larger battery would have been included to assess the concurrent and divergent validity of the GPS. In particular, previous studies already defined convergent validity with other instruments such as PTSD Checklist (PCL-5) or Clinician-Administered PTSD Scale (CAPS-5) (Olff et al., 2020), which could not be replicated in the present study. Also, self-report instruments inherently introduce measuring biases, especially in the absence of normative data. Another major limitation is the absence of clinical interviews or other normative cut-offs that would have allowed estimating a prevalence of PTSD or clinically relevant PTSS. The study’s strength is its large sample size and the timely data collection around the peak of the COVID-19 outbreak providing a unique set of data on the impact of the pandemic in its early phases in Italy.
5. Conclusions
This is the first study to address in detail the traumatic spectrum related to COVID-19 in Italy and provide a first validation of the Italian GPS, showing the psychometric properties of a novel screening tool for trauma-related symptoms. The GPS captured the wide range of symptoms with a three-factor model best explaining the symptoms: 1. Negative Affect; 2. Core post-traumatic stress symptoms (PTSS); 3. Dissociative symptoms. Our findings suggest that the COVID-19 pandemic and related lockdown measures in Italy seriously affect the general population’s mental health, with a wide range of trauma spectrum symptoms being endorsed.
Supplementary Material
Acknowledgments
This study was supported by Territori Aperti, a project funded by the Fondo Territori Lavoro e Conoscenza of the Confederazione Generale Italiana del Lavoro, the Confederazione Italiana Sindacati Lavoratori, and the Unione Italiana del Lavoro.
Disclosure statement
The authors have no conflict of interest to disclose.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author, GDL. The data are not publicly available due to privacy restrictions, as they contain information that could compromise the privacy of research participants.
Supplementary material
Supplemental data for this article can be accessed here.
References
- Bai, Y. M., Lin, C. C., Lin, C. Y., Chen, J. Y., Chue, C. M., & Chou, P. (2004). Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatric Services, 55(9), 1055–12. [DOI] [PubMed] [Google Scholar]
- Bastien, C. H., Vallières, A., & Morin, C. M. (2001). Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Medicine, 2(4), 297–307. [DOI] [PubMed] [Google Scholar]
- Birkeland, M. S., Greene, T., & Spiller, T. R. (2020). The network approach to post-traumatic stress disorder: A systematic review. European Journal of Psychotraumatology, 11, 1700614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet, 395, 912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castronovo, V., Galbiati, A., Marelli, S., Brombin, C., Cugnata, F., Giarolli, L., … Ferini-Strambi, L. (2016). Validation study of the Italian version of the Insomnia Severity Index (ISI). Neurological Sciences : Official Journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology, 37, 1517–1524. [DOI] [PubMed] [Google Scholar]
- Civile, D. P. (2020). COVID-19 Italia - Monitoraggio della situazione. Retrieved from https://arcg.is/C1unv
- Cloitre, M., Garvert, D. W., Brewin, C. R., Bryant, R. A., & Maercker, A. (2013). Evidence for proposed ICD-11 PTSD and complex PTSD: A latent profile analysis. European Journal of Psychotraumatology, 4(4), 20706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., … Hyland, P. (2018). The International Trauma Questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta psychiatrica Scandinavica, 138, 536–546. [DOI] [PubMed] [Google Scholar]
- de Girolamo, G., Polidori, G., Morosini, P., Scarpino, V., Reda, V., Serra, G., … Warner, R. (2006). Prevalence of common mental disorders in Italy. Social Psychiatry and Psychiatric Epidemiology, 41, 853–861. [DOI] [PubMed] [Google Scholar]
- De Vries, G. J., & Olff, M. (2009). The lifetime prevalence of traumatic events and post-traumatic stress disorder in the Netherlands. Journal of Traumatic Stress, 22(4), 259–267. [DOI] [PubMed] [Google Scholar]
- DiGiovanni, C., Conley, J., Chiu, D., & Zaborski, J. (2004). Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecurity and Bioterrorism, 2, 265–272. [DOI] [PubMed] [Google Scholar]
- Dückers, M. L. A., & Olff, M. (2017). Does the vulnerability paradox in PTSD apply to women and men? An exploratory study. Journal of Traumatic Stress, 30(2), 200–204. [DOI] [PubMed] [Google Scholar]
- Hansen, M., Hyland, P., Armour, C., Shevlin, M., & Elklit, A. (2015). Less is more? Assessing the validity of the ICD-11 model of PTSD across multiple trauma samples. European Journal of Psychotraumatology, 6(6), 28766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen, M., Hyland, P., Karstoft, K.-I., Vaegter, H. B., Bramsen, R. H., Nielsen, A. B. S., … Andersen, T. E. (2017a). Does size really matter? A multisite study assessing the latent structure of the proposed ICD-11 and DSM-5 diagnostic criteria for PTSD. European Journal of Psychotraumatology, 8, 1398002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen, M., Ross, J., & Armour, C. (2017b). Evidence of the dissociative PTSD subtype: A systematic literature review of latent class and profile analytic studies of PTSD. Journal of Affective Disorders, 213, 59–69. [DOI] [PubMed] [Google Scholar]
- Hawryluck, L., Gold, W. L., Robinson, S., Pogorski, S., Galea, S., & Styra, R. (2004). SARS control and psychological effects of quarantine, Toronto, Canada. Emerging Infectious Diseases, 10, 1206–1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, J. Z., Han, M. F., Luo, T. D., Ren, A. K., & Zhou, X. P. (2020). [Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19]. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi, 38, E001. [DOI] [PubMed] [Google Scholar]
- Hyland, P., Shevlin, M., Fyvie, C., & Karatzias, T. (2018). Posttraumatic stress disorder and complex posttraumatic stress disorder in DSM-5 and ICD-11: Clinical and behavioral correlates. Journal of Traumatic Stress, 31, 174–180. [DOI] [PubMed] [Google Scholar]
- Karatzias, T., Cloitre, M., Maercker, A., Kazlauskas, E., Shevlin, M., Hyland, P., … Brewin, C. R. (2017). PTSD and complex PTSD: ICD-11 updates on concept and measurement in the UK, USA, Germany and Lithuania. Eur. J. Psychotraumatol, 8(sup7), 1418103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyriazos, T. A. (2018). Applied psychometrics: The 3-faced construct validation method, a routine for evaluating a factor structure. Psychology, 09, 2044–2072. [Google Scholar]
- Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., … Hu, S. (2020). Factors associated with mental health outcomes among health care workers exposed to Coronavirus Disease 2019. JAMA Network Open, 3, e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, S., Chan, L. Y. Y., Chau, A. M. Y., Kwok, K. P. S., & Kleinman, A. (2005). The experience of SARS-related stigma at Amoy Gardens. Social Science and Medicine, 61, 2038–2046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, N., Zhang, F., Wei, C., Jia, Y., Shang, Z., Sun, L., … Liu, W (2020). Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Research, 287, 112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longo, L., Cecora, V., Rossi, R., Niolu, C., & Siracusano, A. (2019). Dissociative symptoms in complex post-traumatic stress disorder and in post-traumatic stress disorder. Journal of Psychopathology, 25, 212–219. [Google Scholar]
- Mondo, M., Sechi, C., & Cabras, C. (2019). Psychometric evaluation of three versions of the Italian Perceived Stress Scale. Current Psychology. doi: 10.1007/s12144-019-0132-8 [DOI] [Google Scholar]
- Oe, M., Kobayashi, Y., Ishida, T., Chiba, H., Matsuoka, M., Kakuma, T., … Olff, M. (in press). Screening for psychotrauma related symptoms: Japanese translation and pilot testing of the Global Psychotrauma Screen. European Journal of Psychotraumatology, 11(1). doi: 10.1080/20008198.2020.1810893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olff, M. (2017). Sex and gender differences in post-traumatic stress disorder: An update. European Journal of Psychotraumatology, 8(sup4), 1351204. [Google Scholar]
- Olff, M., Amstadter, A., Armour, C., Birkeland, M. S., Bui, E., Cloitre, M., … Thoresen, S. (2019). A decennial review of psychotraumatology: What did we learn and where are we going? European Journal of Psychotraumatology, 10, 1672948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olff, M., Bakker, A., Frewen, P., Aakvaag, H., Ajdukovic, D., Brewer, D., … Schnyder, U. (2020). Screening for consequences of trauma – An update on the global collaboration on traumatic stress. European Journal of Psychotraumatology, 11, 1752504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu, J., Shen, B., Zhao, M., Wang, Z., Xie, B., & Xu, Y. (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry, 33, 19–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross, J., Baník, G., Dědová, M., Mikulášková, G., & Armour, C. (2018). Assessing the structure and meaningfulness of the dissociative subtype of PTSD. Social Psychiatry and Psychiatric Epidemiology, 53, 87–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi, R., Longo, L., Fiore, D., Carcione, A., Niolu, C., Siracusano, A., & Di Lorenzo, G. (2019). Dissociation in stress-related disorders and self-harm : A review of the literature and a systematic review of mediation models. Journal of Psychopathology, 25, 162–171. [Google Scholar]
- Rossi, R., Socci, V., Pacitti, F., Di Lorenzo, G., Di Marco, A., Siracusano, A., & Rossi, A. (2020a). Mental health outcomes among frontline and second-line health care workers during the Coronavirus Disease 2019 (COVID-19) pandemic in Italy. JAMA Network Open, 3, e2010185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi, R., Socci, V., Talevi, D., Mensi, S., Niolu, C., Pacitti, F., … Di Lorenzo, G. (2020b). COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Frontiers in Psychiatry, 11. doi: 10.3389/fpsyt.2020.00790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnyder, U., Schäfer, I., Aakvaag, H. F., Ajdukovic, D., Bakker, A., Bisson, J. I., … Olff, M. (2017). The global collaboration on traumatic stress. European Journal of Psychotraumatology, 8, 1403257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shevlin, M., Hyland, P., Roberts, N. P., Bisson, J. I., Brewin, C. R., & Cloitre, M. (2018). A psychometric assessment of disturbances in self-organization symptom indicators for ICD-11 complex PTSD using the International Trauma Questionnaire. Eur. J. Psychotraumatol, 9(1), 1419749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi, L., Lu, Z. A., Que, J. Y., Huang, X. L., Liu, L., Ran, M. S., … Lu, L. (2020). Prevalence of and risk factors associated with mental health symptoms among the general population in China during the Coronavirus Disease 2019 pandemic. JAMA Network Open, 3, e2014053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder. Archives of Internal Medicine, 166, 1092. [DOI] [PubMed] [Google Scholar]
- Spitzer, R. L., Kroken, K., & Williams, J. B. (1999). Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA, 282, 1737. [DOI] [PubMed] [Google Scholar]
- Tucci, V., Moukaddam, N., Meadows, J., Shah, S., Galwankar, S. C., & Bobby Kapur, G. (2017). The forgotten plague: Psychiatric manifestations of ebola, zika, and emerging infectious diseases. Journal of Global Infectious Diseases, 9, 151–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UCLA: Statistical Consulting Group . What is seemingly unrelated regression and how can I perfom it on STATA? Retrieved from https://stats.idre.ucla.edu/stata/faq/what-is-seemingly-unrelated-regression-and-how-can-i-perform-it-in-stata/
- van Huijstee, J., & Vermetten, E. (2017). The dissociative subtype of post-traumatic stress disorder: Research update on clinical and neurobiological features. In Vermetten E., Baker D., Risbrough V. (Eds.), Current topics in behavioral neurosciences (pp. 229–248). Cham: Springer. doi: 10.1007/7854_2017_33 [DOI] [PubMed] [Google Scholar]
- Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., & Ho, R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17, 1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2020). World Health Organization - COVID-19. Retrieved from https://who.sprinklr.com/
- Wu, P., Fang, Y., Guan, Z., Fan, B., Kong, J., Yao, Z., … Hoven, C. W. (2009). The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Canadian Journal of Psychiatry, 54, 302–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao, H., Zhang, Y., Kong, D., Li, S., & Yang, N. (2020). The effects of social support on sleep quality of medical staff treating patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Medical Science Monitor : International Medical Journal of Experimental and Clinical Research, 26, e923549. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author, GDL. The data are not publicly available due to privacy restrictions, as they contain information that could compromise the privacy of research participants.


