ABSTRACT
Objective: In a pragmatic and randomized clinical trial, patients with lateral ankle sprains were assessed, under blinded conditions, for their responsiveness and improvements during Mulligan mobilization-with-movement (MWM) therapy. Methods: Overall, 51 participants with subacute lateral ankle sprains (Grade I–II) were recruited. Following an MWM screening procedure, responders were randomized to either an intervention group (MWM) or a sham group. The MWM group received inferior tibiofibular, talocrural, or cubometatarsal MWM. The treatment or sham was administered upon three sessions, each 4 days apart. Changes from baseline were measured and compared between the sessions for dorsiflexion range of motion, pain, stiffness perception, and the Y-balance test. Results: In total, 43 participants were considered responders to MWM. Using a two-way repeated-measure ANOVA, a statistical and clinically meaningful improvement in dorsiflexion range of motion was revealed in the MWM group (p = 0.004, 1rst = +1.762 cm; 3rd = +2.714 cm), whereas no improvement following the first session occurred in the sham group (p = 0.454, 1rsttrial = +1.091 cm; 3rdtrial = +1.409 cm). Pain and stiffness significantly improved, yet below the clinically meaningful level. The MWM group demonstrated a significant improvement after three sessions for the Y-balance test (p = 0.001, +8.857 cm). Conclusion: More than 80% of participants with subacute lateral ankle sprains responded well to the MWM approach. Three sessions of pragmatically determined MWM provided a significant and clinically meaningful benefit in dorsiflexion range of motion and Y-balance test performance compared to a sham treatment.
KEYWORDS: Ankle sprain, manual therapy, mobilization with movement, mulligan, pragmatic study, weight-bearing lunge test
Introduction
Lateral ankle sprains (LAS) are one of the most common musculoskeletal injuries of the lower limb [1]. Yet, the true incidence is underestimated, as many patients do not seek medical attention [2]. However, the majority of people with LAS suffer long-term consequences, as they reinjure or develop long-lasting functional instability [3].
The International Ankle Consortium reports that LAS can lead to chronic ankle instability, defined as a feeling of the ankle joint ‘giving away,’ or chronic swelling with functional impairment and altered proprioception [4]. In 2019, Delahunt et al. proposed the Rehabilitation Oriented AsseSsmenT protocol to guide clinicians through all the areas that need to be explored in patient with LAS [5]. These authors concluded that management should consist of an individualized, clinically reasoned approach. Based on the model proposed by Hertel et al. (2019), which describes the relationship between mechanical and functional impairment and recurrent ankle sprain, the international recommendations are focused on pain, swelling, dorsiflexion range of motion (ROM) deficit, joint arthrokinematics, static and dynamic postural stability, strength, physical and sport activities, as well as gait [5,6].
Dorsiflexion ROM deficit is found during all LAS stages, ranging from acute to chronic [7]. Reduced dorsiflexion ROM may affect daily life functional activities, including, among others, walking, running, stair use, and squatting [8]. In subacute and chronic LAS, there is radiographic evidence of an anterior displacement of the talus or fibula bones with respect to the tibia, as compared to the non-traumatized ankle [9,10]. Such impairment could lead to an altered talocrural or inferior tibiofibular joint arthrokinematics and decreased ROM, hereby increasing ankle stiffness [11]. In acute LAS, pain is likely to limit dorsiflexion ROM, in addition to weakness of the ankle dorsiflexion and plantar flexor muscles [12].
The Mulligan concept of mobilization with movement (MWM) is a manual therapy modality where the therapist applies a manual gliding force in conjunction with an active, patient-performed movement [13]. Mulligan proposed that MWM could be effective in rehabilitation following LAS. Following LAS, the protocol is designed to apply MWM to the fibula, talus, and cuboid bones, respectively, in order to identify potential responders to MWM treatment.
Several authors suggest that MWM therapy could exert potential benefits on pain, function, or strength, in the LAS setting. Hudson et al. [13] reported a case-series of five adolescents suffering from Grade II LAS, who promptly benefited from Mulligan therapy in terms of pain and functional improvement. In chronic LAS patients, Vicenzino et al. demonstrated the efficacy of posterior talar glide MWM, under non-weight bearing and weight bearing conditions, with an improvement in dorsiflexion ROM below 1 cm [7]. Collins et al. [14], Hidalgo et al. [15], and Marron-Gomez et al. [8] all demonstrated the efficacy of Mulligan therapy in terms of ankle dorsiflexion ROM improvement. However, the previously cited studies have mostly demonstrated results of small effect size, which are not all clinically relevant [16]. One possible explanation for this is that not everyone responds similarly to manual therapy, with possibly a subgroup of patients that respond better than the others. To our knowledge, no studies have so far described the exact proportion of responders to the Mulligan protocol conducted following LAS.
The objectives of this study are twofold: 1) to determine the responsiveness of patients with subacute lateral ankle sprain in regard to Mulligan concept; 2) to determine the effectiveness of Mulligan MWM compared to a sham treatment.
Methods
Population
The participants were recruited by means of word-of-mouth, as well as through print and social media notifications among the student community from the faculty of the Université Catholique de Louvain (UCLouvain, Louvain-La-Neuve, Belgium). Overall, 62 participants were recruited during the enrollment phase, with 51 (30 women and 21 men, mean age = 22.6 ± 3.73) actually included in the pragmatic trial. To be included in the study, subjects were required to suffer from a Grade I–II subacute LAS (2–10 weeks post-injury) and exhibit a 20% deficit in ankle dorsiflexion ROM on the involved side, as measured using the weight-bearing lunge test (WBLT). The LAS grade was classified based on the ligamentous integrity, with Grades I and II demonstrating a positive anterior drawer test, and Grade III demonstrating both a positive anterior drawer test and positive talar tilt test [17]. Subjects were excluded if they suffered from acute (<2 weeks) or chronic (>10 weeks) LAS or if no impairment in dorsiflexion ROM was noted. In addition, subjects with any history of ankle fracture, ligament ruptures, or neurological disorders or those Grade III LAS were not allowed to participate (Figure 1).
Figure 1.
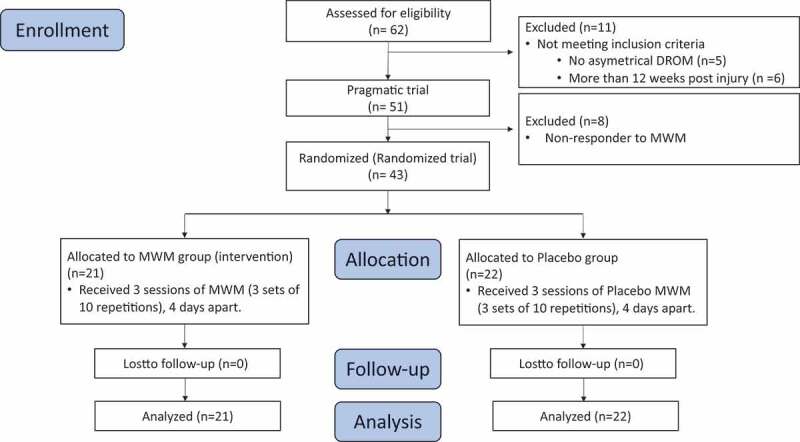
CONSORT Flow diagram Design of the current study divided in three sessions. MWM group represents the intervention group, whereas the sham group received sham therapy. DROM = dorsiflexion range of motion; MWM = mobilization with movement
Every participant was fully informed of the study’s purpose and provided written consent to participate. The subjects enrolled on a voluntary basis without any financial compensation, and they were free to leave the study at any time, without having to give any reason. The current study was approved by the local ethics’ committee, the ‘Comité d’éthique hospitalo-facultaire’ (Belgium) (B403201938921), and registered into ClinicalTrial.gov (NCT03948503).
Design
The study was designed as a pragmatic randomized controlled trial. For the pragmatic part, we identified responders to the Mulligan protocol following LAS. All responders were consequently randomized by an independent operator to one of two groups, MWM or Sham, using a randomized sequence developed via Excel 2010 (Microsoft, Redmond, WA, USA). The responder process is detailed in the procedure section. Allocation concealment was maintained at all times. The MWM group received the real MWM treatment, whereas the Sham group received a sham MWM. A postgraduate physiotherapist, who was blinded to group allocation, supervised all outcome measurements, while a non-blinded physiotherapist, i.e., a certified Mulligan practitioner with 5-years of clinical experience applied either the MWM or sham intervention. All participants were kept blinded for group allocation throughout the experiment.
The intervention was applied over three sessions with an assessment made at the beginning and end of each, resulting in six evaluation times: T1 and T2 represented the recordings made at the beginning and end of the first session, T3 and T4 measurements made at the beginning and end of the second session, and T5 and T6 measurements made at the beginning and end of the third session (Table 2). Each session took place in a laboratory at the Faculty of motor Science of UCLouvain (Belgium). Clinical and functional outcomes were assessed through every session, with MWM and Sham group results compared (Figure 1).
Table 2.
Description of raw data for both groups at each measurement point (T)
| MWM group |
Sham Group |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T4 | T5 | T6 | T1 | T2 | T3 | T4 | T5 | T6 | ||
| WBLT | I | 8.7 | 10.4 | 9.2 | 10.9 | 10.4 | 11.4 | 9.4 | 10.5 | 10.2 | 11.0 | 10.4 | 10.9 |
| (cm) | (2.71) | (2.40) | (2.62) | (2.59) | (2.60) | (2.48) | (2.80) | (2.58) | (3.14) | (2.49) | (2.54) | (2.81) | |
| NI | 12.7 | 12.8 | 12.9 | 13.5 | 12.2 | 13.2 | 12.5 | 12.8 | 12.9 | 12.9 | 12.6 | 12.7 | |
| (1.83) | (1.72) | (2.27) | (2.24) | (3.58) | (2.54) | (2.92) | (2.53) | (2.76) | (2.35) | (2.42) | (2.47) | ||
| Pain | 2.5 | 3.1 | 2.4 | 2.5 | 2.2 | 2.1 | 2.0 | 2.5 | 1.9 | 1.9 | 1.9 | 1.7 | |
| (/10) | (2.80) | (1.88) | (1.57) | (2.05) | (1.83) | (1.81) | (1.78) | (1.50) | (1.61) | (1.73) | (1.86) | (1.53) | |
| Stiffness | 4.0 | 3.3 | 3.7 | 3.5 | 2.8 | 2.4 | 3.4 | 2.8 | 2.6 | 2.3 | 2.5 | 2.1 | |
| (/10) | (2.08) | (2.24) | (2.04) | (2.17) | (1.84) | (1.54) | (2.20) | (1.50) | (1.84) | (1.63) | (1.99) | (1.67) | |
| YBT | 76.3 | 81.2 | 81.1 | 84.2 | 84.3 | 85.1 | 77.5 | 80.5 | 81.3 | 83.2 | 81.7 | 83.2 | |
| (cm) | (11.27) | (12.27) | (8.30) | (8.38) | (10.96) | (10.95) | (8.35) | (8.67) | (9.54) | (9.33) | (8.34) | (8.36) | |
Data were presented as means (SD). I = injured, NI = non-injured, T1: data at baseline T2: data at completion of first treatment session. T3: data at beginning of the second treatment session 2. T4: data at completion of second treatment session. T5: data at beginning of third treatment session. T6: data at completion of third treatment session. WBLT: weight-bearing lunge test; I = injured ankle; NI = non-injured ankle; Pain and Stiffness on a visual analogue scale; YBT: Y-balanced test. Cohen’s d measured the effect size between T1 and T6 for each group.
Outcomes
Socio-demographic and anthropometric data were collected at enrollment, with weight, height, gender, age, and any previous relevant medical information retrieved (Table 1). The same physiotherapist who was blinded to group allocation measured all outcomes. No interaction was permitted between the treating therapist and the assessor across the three treatment sessions.
Table 1.
Baseline characteristics of patients for MWM and Sham groups
| Characteristics | Subgroup | MWM | Sham |
|---|---|---|---|
| Gender | Female | 13 | 14 |
| Male | 8 | 8 | |
| Ankle injured | Right | 12 | 14 |
| Left | 9 | 8 | |
| Time since ankle sprain (months) | 2 (1.69) | 1,8 (1.61) | |
| Age (year) | Female | 24.5 (6.37) | 21.7 (2.43) |
| Male | 22.6 (1.85) | 22.3 (1.77) | |
| Primary outcome | |||
| WBLT (cm) | Injured | 8.6 (2.72) | 9.2 (2.78) |
| Non-injured | 12.6 (1.91) | 12.5 (2.89) | |
| Secondary outcomes | |||
| Pain (/10) | 2.4 (1.49) | 1.9 (1.66) | |
| Stiffness (/10) | 4 (2.21) | 3.4 (2.14) | |
| YBT (cm) | Injured | 76.1 (11.28) | 77.5 (8.28) |
| No-injured | 80.6 (9.75) | 80.2 (8.37) | |
| BESS (/30) | 11.7 (6.15) | 11.1 (5.2) | |
| FAAM 1 (%) | 84.5 (12.42) | 87.6 (9.46) | |
| FAAM 2 (%) | 62.1 (25.28) | 72.2 (18.69) | |
| Data were presented as means (SD). MWM = mobilization with movement. WBLT = weight-bearing lunge test; pain and stiffness on a visual analogue scale (/10); YBT = Y-balance test; BESS = Balance Error Scoring System; FAAM 1: foot and ankle ability measure, Everyday life activities; FAAM 2: foot and ankle ability measure, sports activities. Two-way repeated measure ANOVA post-hoc analysis revealed no significant differences between the MWM and Sham groups at baseline. | |||
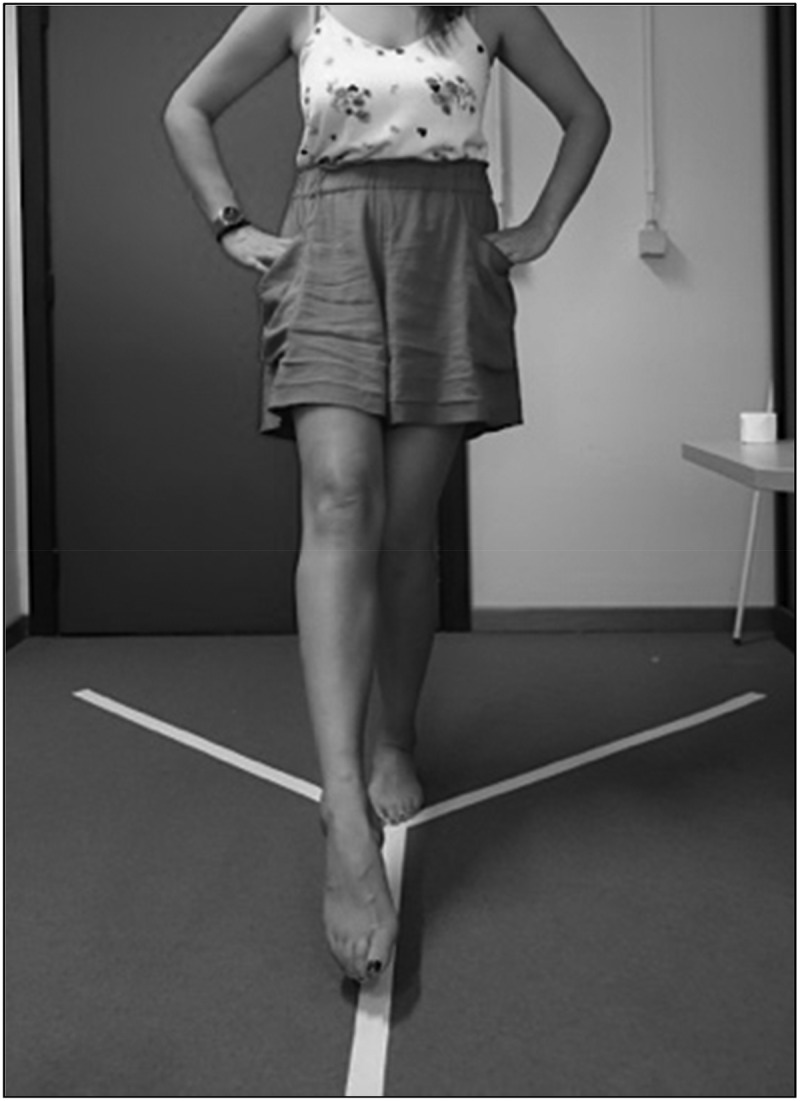
Primary Outcome
The primary outcome was an ankle DROM determined using the weight-bearing lunge test (WBLT), as illustrated in Figure 2 [18,19]. The WBLT represents the distance between the distal end of the first toe and the wall, with the heel on the ground. This test has proven excellent intra- and inter-rater reliability (intraclass correlation [ICC] between 0.8 and 0.99), with a minimal detectable change of 1.9 cm [20]. Both the injured and non-injured ankles were measured using WBLT at the beginning and end of each session.
Figure 2.

The Weight-Bearing Lunge Test (WBLT) against a wall
Secondary Outcomes
A visual analogue scale was used to assess pain and ‘stiffness perception’ during WBLT conducted on the injured ankle [21]. The Y-balance test (YBT) was employed to assess dynamic stability. A tape with a Y-shape was placed on the ground, with a 135-degree angle between arms (Figure 3). This test has been proven reliable for the three directions, with an ICC of 0.8–0.85 and minimal detectable change of 8.7–11.5 cm [22]. To assess static stability, the Balance Error Score System (BESS) was applied; this is a relevant screening test for athletes with static postural deficits [23]. The Frontal Step down (FSD) test displays excellent intra- and inter-rater reliability (ICC: 0.96–0.99), translating into three categories of performance, i.e., poor, medium, or good [24]. Using the FSD test, Lebleu et al. [25] demonstrated the impact of restricted ankle dorsiflexion-induced compensations and perturbations on the lower limb kinematic chain. The self-reported Foot and Ankle Ability Measure (FAAM) was instrumental in assessing the impact of LAS on everyday life activities (FAAM1) and sports activities (FAAM2). This form was completed at the beginning and end of each experiment [26]. The FAAM was conducted in French for every participant [27]. While WBLT, pain, stiffness, and YBT were measured at the six assessment times, the BESS, FSD, and FAAM were only accomplished at T1 and T6.
Figure 3.
Y-balanced test
Procedure
Pragmatic trial
Before randomization, responders to the Mulligan protocol for LAS were identified. (Hing et al. 2019) A passive postero-superior glide was applied to the anterior part of the lateral malleolus during passive supination, i.e., plantar flexion, inversion, and adduction of the foot (Figure 5).This preliminary test has been designed to assess the sensitivity and integrity of the anterior talofibular ligaments. If the participant described no pain during this maneuver, the screening algorithm commenced with the inferior tibiofibular MWM (ITF-MWM) (Figure 4A). A passive posterior, lateral, and superior glide was applied by the physiotherapist while the participant undertook weight-bearing active dorsiflexion, with three to five repetitions. This technique was applied with minimal body weight through the treated ankle that was maintained, while the participant performed this active dorsiflexion. Immediately after the ITF-MWM application, the dorsiflexion ROM, pain, and YBT were reassessed. In order to be considered as MWM responders, the participants were required to demonstrate an increase in dorsiflexion ROM above the minimal detectable change of 1.9 cm, an improvement in pain of at least 2 cm on the VAS during dorsiflexion, or an increase in YBT for the involved leg of at least 8.9 cm.
Figure 5.
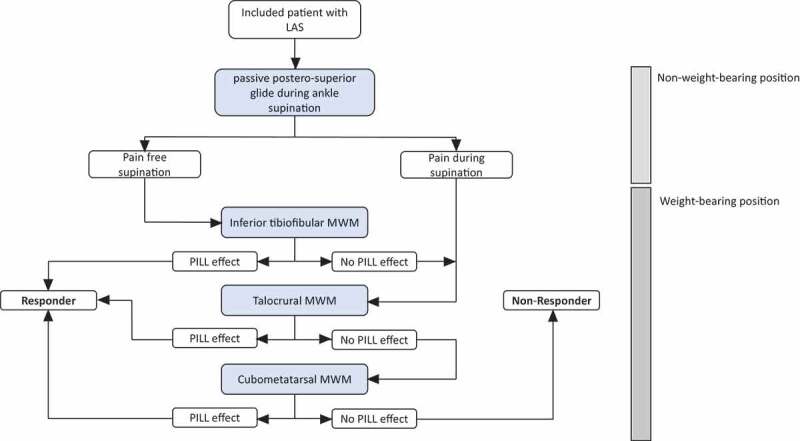
Pragmatic trial MWM = Mobilization with movement; PILL effect corresponds to the responsiveness of the participant after application of a define MWM therapy. The PILL effect is positive when the patient described a significant decrease in pain, increase in dorsiflexion range of motion or a functional assessment significantly improved. Responder were randomized while non-responders were excluded from further analysis
Figure 4.
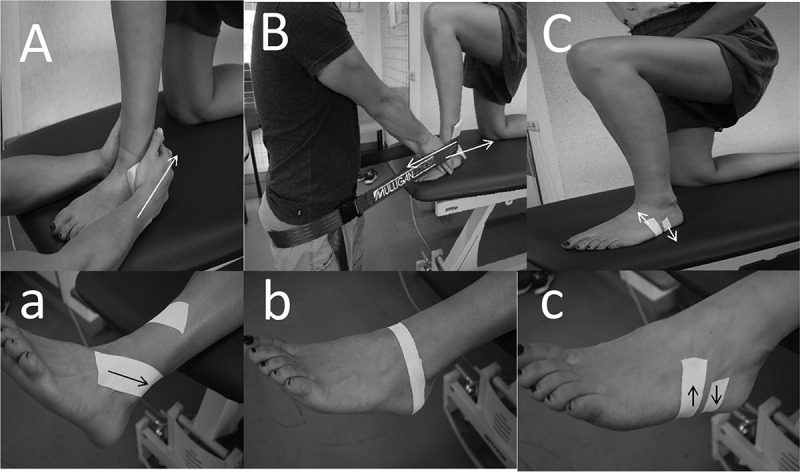
MWM intervention Position of the physiotherapist’s hands and participant position for the different mobilization with movement (MWM) techniques. A = inferior tibiofibular MWM, B = talocrural MWM, C = cubometatarsal MWM. White arrows indicate the direction of the therapist’s manual force. For C, the tape and consequent arrow direction can be reversed depending on the patient’s response. The three figures below represent the taping applied at the end of each session: a = inferior tibiofibular taping, b = talocrural taping, c = cubometatarsal taping. Black arrows indicate the direction of applied tension
If the participant did not respond to the ITF-MWM or felt any pain during the intervention, a talocrural MWM (TC-MWM) was then performed (Figure 4B). The TC-MWM consists of a passive posterior glide of the talus relative to the tibia, during the same active weight-bearing dorsiflexion movement. A mobilization belt that was looped around the physiotherapist and the posterior part of the patient's leg was used to assist the anterior glide force of the tibia relative to the talus. Identical to the ITF-MWM, the TC-MWM (Figure 4) was first applied with minimal subject body weight on the treated leg and maintained during the weight-bearing active dorsiflexion, with three to five repetitions.
Thereafter, according to the MWM protocol for LAS, if the participant did not meet the responder criteria, a third and final MWM was applied. Due to the difficulty of a therapist to apply manual MWM in a weight-bearing position, the cubometatarsal MWM (CM-MWM) was applied using a 20 mm wide non-stretch sports tape (Strappal®, BSN Medical, Luxembourg) under tension in a counter-force direction (Figure 4C). This was aimed to create a mobilization effect at the cubometatarsal joint. Two layers of tape were applied in a non-weight bearing position. If the first application of tape was not effective, then the tape direction was reversed.
Randomized Trial
After identifying responders and excluding non-responders (Figure 5), both groups received either the real treatment (MWM group) or the sham treatment (Sham group). The real treatment consisted of three sets of 10 repetitions of the tailored MWM, i.e., ITF-MWM, TC-MWM, or CM-MWM, with a 1-minute rest separating the sets.
The sham treatment consisted of the same MWM identified as helpful in the MWM responder protocol, except that the physiotherapist applied only light pressure on the skin during the active dorsiflexion. For the CM-MWM, no tension was applied on the tape.
According to the Mulligan concept, following each MWM session, a non-stretched sports tape was to be applied to replicate the MWM and, thus, maintain treatment effects. The tape technique was matched to the corresponding MWM identified as helpful in the MWM responder protocol, and it was thus applied to each treated ankle. For the ITF-MWM, a 2.5 cm layer of tape started 2 cm in front of the anterior edge and 1 cm proximal to the tip of the lateral malleolus. Two layers of tape were applied in a spiral direction from the distal to the proximal ending at the anterior aspect of the tibia. Tape was applied in a non-weight bearing position, and the therapist applied a MWM to the fibula while tape was applied (Figure 4a).
The TC-MWM tape, 2.5 cm wide, was applied in two layers in non-weight bearing, with the treated ankle in a plantar grade position. Tape started on the superior surface of the talus neck and it was directed posteriorly, passing below the tip of each malleolus, and crossing the posterior and distal face of the calcaneus (Figure 4b). Finally, for the CM-MWM, the same tape was applied during the responder trial and treatment was applied (Figure 4c).
Data Analysis
The change scores for each outcome measure from the beginning to end of each treatment session were measured for all variables, in an effort to assess within session changes. The cumulative change score (from the end of each session as compared to the first session’s baseline) was also measured for each variable in order to assess any improvement between treatment sessions. The following statistical analysis was performed using Sigmaplot 14.0 (Systat Software Inc., USA). A two-way (group x session x interaction) repeated measured ANOVA was performed on within session change scores, as well as cumulative change scores. Holm–Sidak post-hoc analysis was performed. A two-way (group x session x interaction) ANOVA was performed for BESS, FSD, and FAAM (1 and 2) values. A Holm–Sidak post-hoc analysis was conducted to assess pairwise family comparison. Concerning the FSD, a Kruskal–Wallis one-way analysis of variance on ranks was carried out with a Dunn’s method if any differences were to be significant. The critical value of significance was set at p = 0.05 for all tests. Cohen’s d effect size was measured for cumulative change scores between treatment 1 and treatment 3, and between groups within treatment sessions, as well.
Results
Overall, 62 participants were initially recruited for enrollment, although five of them did not exhibit asymmetrical dorsiflexion restriction, while six others were injured for more than 12 weeks (Figure 1). Consequently, 51 participants were assessed using the MWM responder-screening protocol, with eight (15.69%) considered as non-responders, and thus excluded from further analysis. Of the 43 responders (84.31%) to the screening protocol, 25 (58%) responded to the ITF-MWM technique and taping, 14 (33%) TC-MWM technique and taping, and four (9%) to the CM-MWM taping technique.
The baseline characteristics of both groups, MWM and Sham, are summarized in Table 1. Raw data for each group concerning the three sessions have been provided in Table 2.
Primary Outcome: WBLT
Two-way repeated measure (group x session) ANOVA post-hoc analysis (Holm–Sidak) demonstrated a greater improvement in the MWM group than the Sham group (between groups) for Session 1 (p = 0.32, Cohen (d) = 0.75 [0.001 to 1.53], mean difference = 0.671 cm) and Session 2 (p = 0.011, Cohen (d) = 0.82 [0.13 to 1.61], mean difference = 0.799 cm). No differences were found between the MWM and Sham groups concerning session change scores.
For the cumulative change scores, only Session 3 demonstrated greater improvement (p = 0.001, Cohen (d) = 0.86 [0.25 to 1.59], mean difference = 1.305 cm) in the MWM group (+2.714 cm) versus the Sham group (+1.409 cm). In addition, the MWM group demonstrated a significant improvement when comparing Session 3 to Session 1 (p = 0.004, Cohen (d) = 0.85 [0.25 to 1.55], mean difference = 0.952), whereas the Sham group displayed no improvement between Session 1 and Session 3 (p = 0.454, Cohen (d) = 0.61 [−0.09 to 1.55]). (Table 3)
Table 3.
Improvement within and between sessions in the MWM and Sham groups
| |
Improvement within each session (Within session change) |
|
Cumulative improvement from baseline (Between session change) |
|||||
|---|---|---|---|---|---|---|---|---|
| Treatment session 1 | Treatment session 2 | Treatment session 3 | Treatment session 1 | Treatment session 2 | Treatment session 3 | Within group P value (Holm-Sidak); Effect size [95 CI](group x session)for cumulative change scores (Session 1 vs Session 3) | ||
| MWM | ||||||||
| WBLT Injured (cm) |
1.762 | 1.571 | 1 | 1.762 | 2.143 | 2.714 | 0.004; 0.85 [0.25 to 1.55] | |
| WBLT Non-injured (cm) |
0.143 | 0.476 | 0.952 | 0.143 | 0.714 | 0.524 | 0.301; 0.34 [−0.39 to 0.98] | |
| Pain (/10) |
0.0667 | 0.0952 | 0.09 | 0.667 | 0.047 | −0.381 | <0.001; 0.74 [0.06 to 1.41] | |
| Stiffness perception (/10) | −0.714 | −0.238 | −0.333 | −0.714 | −0.524 | −1.619 | 0.003; 0.66 [0.23 to 1.07] | |
| YBT (cm) |
4.905 | 2.81 | 0.8 | 4.905 | 7.238 | 8.857 | 0.001; 0.62 [0.17 to 0.99] | |
| Sham | ||||||||
| WBLT Injured (cm) |
1.091 | 0.773 | 0.5 | 1.091 | 1.455 | 1.409 | 0.454; 0.61 [−0.09 to 1.55] | |
| WBLT Non-injured (cm) |
0.227 | 0.0455 | 0.136 | 0.227 | 0.364 | 0.182 | 0.864; 0.04 [−0.29 to 0.46] | |
| Pain (/10) |
0.545 | 0 | −0.182 | 0.545 | 0 | −0.227 | 0.008; 0.49 [0.12 to 0.94] | |
| Stiffness perception (/10) | −0.591 | −0.273 | −0.409 | −0.591 | −1 | −1.273 | 0.039; 0.46 [0.12 to 0.8] | |
| YBT (cm) |
2.909 | 1.682 | 1.364 | 2.909 | 5.227 | 5.364 | 0.063; 0.72 [0.25 to 1.26] | |
| Between group P value (Holm-Sidak); effect size [95% CI](group x session) for each session concerning WBLT injured variables | 0.032; 0.75 [<0.001 to 1.53] | 0.011; 0.82 [0.13 to 1.61] | 0.108; 0.59 [−0.11 to 1.47 | 0.032; 0.75 [<0.001 to 1.53] | 0.086; 0.47 [−0.19 to 0.97] | 0.001; 0.86 [0.25 to 1.59] | ||
| Mean Data are presented. WBLT = Weight-Bearing Lunge Test. | ||||||||
Secondary Outcomes
For the MWM group, post-hoc analysis (Holm–Sidak) revealed statistically significant differences for both pain and stiffness perception (respectively: p < 0.001, Cohen (d) 0.74 [0.06 to 1.41] and p = 0.003, Cohen (d) = 0.003, Cohen (d) = 0.66 [0.23 to 1.07]). Moreover, cumulative change scores for the YBT in the MWM group revealed a significant improvement from Session 1 to Session 3 (p = 0.001, Cohen (d) 0.62 [0.17 to 0.99]). In the Sham group, only the VAS for pain demonstrated a statistically significant improvement (p = 0.008, Cohen (d) = 0.49 [0.12 to 0.94]) from Session 1 to Session 3.
A two-way (group x session) ANOVA post-hoc analysis (Holm–Sidak) demonstrated no significant improvement in BESS in either group nor session or interaction factor (Table 4). However, FAAM 1 and 2 demonstrated a session factor (respectively: p = 0.017 and p = 0.043) between T6 and T1, without neither group nor interaction factor (Table 4). Kruskal–Wallis analysis of variance on ranks showed no difference for FSD between T6 and T1 for either the MWM or Sham group (p = 0.118).
Table 4.
Results of two-way ANOVA and Kruskal–Wallis analysis of rank for BESS, FAAM, and FSD
| MWM |
Sham |
|||||
|---|---|---|---|---|---|---|
| 1rst session (T1) | 3rd session (T6) | 1rst session (T1) | 3rd session (T6) | |||
| Two-way ANOVA | Within group (MWM) p-value (Holm-Sidak) from session 1 (T1) to Session 3 (T6) | Within group (Sham) p-value (Holm-Sidak) from session 1 (T1) to Session 3 (T6) | ||||
| BESS | 11.8 (6.1) | 8.4 (3.5) | 11.1 (5.2) | 13.5 (20.1) | 0.116 | 0.243 |
| FAAM [1] | 85.6 (12.32) | 89.7 (9.6) | 87.7 (9.46) | 92.9 (6.36) | 0.093 | 0.085 |
| FAAM [2] | 62.1 (25.2) | 71.9 (18.7) | 72.2 (18.7) | 80.3 (15.9) | 0.112 | 0.198 |
| Kruskal-Wallis | P-value | |||||
| FSD | 3 [2–3] | 3 [2.5–3] | 3 [2–3] | 3 [3–3] | 0.188 | |
| BESS: Balance Error Score System, FAAM: Foot and Ankle Ability Measurement, 1: for everyday life activities, 2: sports activity, FSD: Frontal Step Down. BESS and FAAM data were presented as MEAN (SD) while FSD data werepresented as MEDIAN [1rst-3rd quartile]; 1: poor, 2: medium, 3: good. | ||||||
Discussion
This study assessed the number of clinical responders to MWM in patients with subacute pain and disability following LAS. In addition, MWM efficacy was determined following a pragmatic treatment approach compared to a sham MWM in terms of dorsiflexion ROM, pain, stiffness perception, and functional outcomes. To our knowledge, this is the first study to apply a pragmatic clinical screening protocol in order to assess responses to a particular treatment in LAS patient. Based on our results, 84% of patients were found to respond to the MWM. In these responders, the most commonly effective treatment technique was an inferior tibiofibular joint MWM (58%) followed by the talocrural joint MWM (33%), while only 4% responded to the cubometatarsal joint MWM. The MWM group demonstrated a progression throughout the three sessions in dorsiflexion ROM and YBT measurements, whereas the Sham group only improved in the first session. In spite of a moderate effect size for pain and stiffness improvement, the MWM group was revealed to be below the required minimal detectable change (>2). This may possibly indicate that more treatment sessions would be required in an effort to reach the minimal detectable change in terms of these variables.
Improvement in dorsiflexion ROM from the MWM and taping technique is assumed to be in part of biomechanical nature, with increased posterior gliding of the talus with respect to the tibia [28]. Hing et al. [29] previously described the efficacy of MWM therapy on peripheral joints concerning strength, pain, and function. Notably, several authors demonstrated that a single MWM session was able to improve dorsiflexion ROM. Collins et al. demonstrated a + 1.2 cm improvement following a single talocrural MWM session [14]. Similarly, Marron-Gomez et al. [8] demonstrated a 1.7 cm improvement and 2.2 cm improvement of WBLT directly and 48 hours after a single session of either talocrural MWM or high velocity and low amplitude manipulation (HVLA) compared to a placebo. However, it is worth noting that in the Marron-Gomez study, the placebo group did not undertake full ankle dorsiflexion during their talocrural MWM. In a similar study, Hidalgo et al. [15] demonstrated a + 1.1 cm change in the WBLT following a single talocrural MWM session, and +0.7 cm change following the HVLA technique. Based on our results, a single session (T1-T2) demonstrated an improvement of +1.7 cm in the MWM group versus +1.1 cm in the Sham group. It must be stressed that the minimal detectable change for the WBLT was previously from 1.5 cm; however, a new standard rise him to 1.9 cm [20]. Based on our results, non-injured ankles demonstrated an improvement of +0.4 cm after a single treatment session. This could be accounted for by repetitive active dorsiflexion during the session. Active dorsiflexion could induce viscoelastic property modifications in musculoskeletal tissues, i.e., conjunctive tissue, fascia, ligaments, etc. [30]. Reid et al. [31] suggested that the maximal dorsiflexion achieved during the WBLT might induce a stretching effect on the ankle. Moreover, a recent study demonstrated that a single session of inferior tibiofibular MWM was unable to improve the dorsiflexion ROM compared to a sham MWM [32]. In contrast, we demonstrated a + 2.7 cm improvement after three selected MWM sessions. Such a result is deemed clinically relevant compared to the Sham group (+1.4 cm). Furthermore, the MWM group cumulative change score for dorsiflexion ROM demonstrated a large effect size (0.85 [0.25 to 1.55]) whereas the Sham group demonstrated a Cohen (d) interval of confidence overlapping the null values (0.61 [−0.09 to 1.55]).
Similar to WBLT, YBT measurements improved in the MWM group (+8.85 cm). This could be explained by an improvement in dorsiflexion ROM, which enables a better YBT score. Moreover, manual therapy, e.g., spinal manipulation, demonstrated plastic changes in sensorimotor integration within the central nervous system [33]. On the other hand, static postural stability, as assessed with the BESS, failed to show signs of improvement. It has been reported that balance and strength training would improve BESS [34]. Therefore, it seemed logical to deduce that MWM therapy should be given along with other treatment modalities, including among others balance training and strengthening.
Although pain scores and stiffness perception during ankle dorsiflexion decreased in both groups when comparing the final evaluation to baseline, it is must be noted that these values are still below the minimal detectable change of at least ±1.8 cm for a VAS [35]. Similarly, Collins et al. [14] concluded that there is no post-treatment hypoalgesia after applying MWM to the ankle, as their study did not produce any significant change in pressure pain threshold. One explanation for this is that in regard to our sample, MWM exerts a mainly mechanical effect on movement rather than a neurophysiological effect on pain in individuals suffering from ankle injuries. Another explanation could be that the lower pain reported at baseline in our studywas 2.4 and 1.9 for the MWM and Sham groups, respectively. Such pain levels are relatively low and could, thus, not be considered as a clinically relevant outcome.
The improvement in the Sham group (+1.1 cm after the first session; +1.4 cm after the third session) could be explained by the trial’s pragmatic nature. Each study participant received the real intervention as part of the responder identification prior to randomization. Our study design was focused on a pragmatic methodology rather than a standard research protocol. It is currently assumed that clinically reasoned, patient-centered care allows for the treatment to be modified so as to seek the best outcome for each individual [36]. The one-size-fits-all approach to therapy, which is often applied in clinical trials, may not be very relevant, given that the current literature reports on multiple factors able to influence the outcome, which are related to therapist, patient, and environment [37]. More specifically, the Hawthorne effect is not to be omitted [38]. The results of the present study indicate that the majority of people with an ankle dorsiflexion ROM deficit responded to MWM, whereas some did not. Furthermore, participants responded differently to each MWM technique. Based on the present study, the choice of any MWM technique, or any other manual therapy intervention, should be based on treatment response. According to our protocol, ITF-MWM demonstrated the best efficacy. One possible explanation would be that this was the first technique applied and, thus, statistically the most significant. A recent study supported, however, the anteriorization of the fibula in chronic ankle instability patients [39], and thus increase the order of the MWM proposed in the pragmatic trial. It could also be argued that this screening process should be done at each treatment session rather than only at the initial diagnostic session. The MWM screening protocol applied in the present study appeared to be quick to use and could, thus, be easily applied in clinical practice.
This study presents several limitations. Firstly, we included participants with subacute dorsiflexion ROM deficit and pain following LAS Grades I–II, with a mean time since injury of 2 months. Our population did not exhibit either substantial impairment or pain in the subacute condition. Therefore, it would be interesting to perform a similar protocol on subjects following acute LAS. In addition, we mostly recruited women and young participants. The study population were recruited in the university surrounding, including academic, student and administrative community. Extrapolation of our results to the general population should, thus, only be made with caution. Furthermore, we did not assess the intervention’s long-term effect. Moreover, the International Ankle Consortium recommended strength testing, which was not carried out in the present study due to logistical issues. However, strength rehabilitation is likely to be more relevant than MWM in terms of strength recovery. We used a sample of convenience. However, the primary outcome statistical power analysis demonstrated a power of 1.0 with a threshold significance of .05 and a large effect size (.84). Finally, we did not include a control group that received neither MWM nor sham treatment. Hence, it is not possible to conclude that the absence of treatment could also impact recovery following LAS. Further studies are required and should focus on the MWM screening protocol’s reliability. The impact of the MWM protocol should also be assessed on people suffering from acute LAS.
Conclusion
In people with dorsiflexion ROM deficit following subacute LAS, 84% responded well to a Mulligan MWM protocol comprising three different mobilization and taping techniques. A pragmatic clinical screening process was applied that permitted identifying potential responders to MWM. The MWM techniques provided clinically relevant benefits on dorsiflexion ROM, in addition to improvement on pain and stiffness after three treatment sessions, in comparison with sham. However, MWM did not demonstrate any effect on either static postural stability or functional activity impairment.
Biographies
Anh Phong Nguyen is a physiotherapist and PhD candidate at the Université Catholique de Louvain (UCLouvain) in Belgium. His time is divided between clinical work, teaching and research activities.
Prof. Laurent Pitance is a professor at the Université Catholique de Louvain (UCLouvain) in Belgium. His research is focused on pain, temporomandibular disorders and manual therapy and is an active member of the Mulligan Concept Teaching Association.
Prof. Philippe Mahaudens is a professor at the Université Catholique de Louvain (UCLouvain) in Belgium. His main focus are biomechanics and scoliosis.
Prof. Christine Detrembleur is a professor at the Université Catholique de Louvain (UCLouvain) in Belgium and is the head of the laboratory of NeuroMusculoSkeletal lab (IREC/UCLouvain). She is an expert in biomechanics and locomotion.
Yuval David is a physiotherapist based in Israel. He is an expert clinical and an active member of the Mulligan Concept Teaching Association.
Prof. Toby Hall is an internationally respected teacher of manual therapy. He is an Adjunct Associate Professor at Curtin University, Perth Western Australia, and is also Senior Teaching Fellow at the University of Western Australia. He also a member of the Mulligan Concept Teaching Association.
Ethic committee
The study protocol was approved by the local ethics’ committee, i.e.,, the ‘comité d’éthique hospitalo-facultaire’ (UCLouvain, Belgium) (B403201938921) and registered in ClinicalTrial.gov (NCT03948503).
Financial disclosure and conflict of interest
All authors affirm that they have no conflict of interest. No funding or grants from any public or private organization were used in the preparation of this manuscript.
Key points
Findings: More than 80% of dorsiflexion restricted from ankle sprains responded well to Mulligan's concept. Three MWM sessions were effective in clinically improving dorsiflexion, as compared to the sham therapy.
Implications: Mulligan's concept is easy to use in clinical trials, as well as in clinical practice, that assess the responsiveness of this concept to restricted dorsiflexion on account of ankle sprains. Clinicians should apply for selected therapy depending on the patient response.
Caution: The study population was relatively young and did not display any major functional impairment nor pain.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Gribble PA, Bleakley CM, Caulfield BM, et al. Evidence review for the 2016 international ankle consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016;50(24):1496–1505. [DOI] [PubMed] [Google Scholar]
- [2].Doherty C, Delahunt E, Caulfield B, et al. The incidence and prevalence of ankle sprain injury: A systematic review and meta-analysis of prospective epidemiological studies. Sport Med. 2014;44(1):123–140. [DOI] [PubMed] [Google Scholar]
- [3].Fong DT, Hong Y, Chan L, et al. Review on ankle injury and ankle sprain in sports. Sport Med. 2007;37(1):73–94. [DOI] [PubMed] [Google Scholar]
- [4].Delahunt E, Coughlan GF, Caulfield B, et al. Inclusion criteria when investigating insufficiencies in chronic ankle instability. Med Sci Sports Exerc. 2010;42(11):2106–2121. [DOI] [PubMed] [Google Scholar]
- [5].Delahunt E, Bleakley CM, Bossard DS, et al. Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement and recommendations of the international ankle consortium. Br J Sports Med. 2018;52(20):1304–1310. . [DOI] [PubMed] [Google Scholar]
- [6].Hertel J, Corbett RO.. An updated model of chronic ankle instability. J Athl Train. 2019;54(6):572–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Vicenzino B, Branjerdporn M, Teys P, et al. Initial changes in posterior talar glide and dorsiflexion of the ankle after mobilization with movement in individuals with recurrent ankle sprain. J Orthop Sports Phys Ther. 2006;36(7):464–471. [DOI] [PubMed] [Google Scholar]
- [8].Marrón-Gómez D, ÁL R-F, Martín-Urrialde JA. The effect of two mobilization techniques on dorsiflexion in people with chronic ankle instability. Phys Ther Sport [Internet]. 2015;161:10–15. [DOI] [PubMed] [Google Scholar]
- [9].Magerkurth O, Frigg A, Hintermann B, et al. Frontal and lateral characteristics of the osseous configuration in chronic ankle instability. Br J Sports Med. 2010;44(8):568–572. [DOI] [PubMed] [Google Scholar]
- [10].Hubbard TJ, Hertel J. Anterior positional fault of the fibula after sub-acute lateral ankle sprains. Man Ther. 2008;13(1):63–67. [DOI] [PubMed] [Google Scholar]
- [11].Denegar CR, Hertel J, Fonseca J. The effect of lateral ankle sprain on dorsiflexion range of motion, posterior talar glide, and joint laxity. J Orthop Sports Phys Ther. 2002;32(4):166–173. [DOI] [PubMed] [Google Scholar]
- [12].Aiken AB, Pelland L, Brison R, et al. Short-term natural recovery of ankle sprains following discharge from emergency departments. J Orthop Sports Phys Ther. 2008;38(9):566–571. [DOI] [PubMed] [Google Scholar]
- [13].Hudson R, Baker RT, May J, et al. Novel treatment of lateral ankle sprains using the Mulligan concept: an exploratory case series analysis. J Man Manip Ther [Internet]. 2017;255:251–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Collins N, Teys P, Vicenzino B. The initial effects of a Mulligan’s mobilization with movement technique on dorsiflexion and pain in subacute ankle sprains. Man Ther. 2004;9(2):77–82. [DOI] [PubMed] [Google Scholar]
- [15].Hidalgo B, Hall T, Berwart M, et al. The immediate effects of two manual therapy techniques on ankle musculoarticular stiffness and dorsiflexion range of motion in people with chronic ankle rigidity: A randomized clinical trial. J Back Musculoskelet Rehabil. 2018;31(3):515–524. [DOI] [PubMed] [Google Scholar]
- [16].Bialosky JE, Beneciuk JM, Bishop MD, et al. Unraveling the mechanisms of manual therapy: Modeling an approach. J Orthop Sports Phys Ther. 2018;48(1):8–18. . [DOI] [PubMed] [Google Scholar]
- [17].Malliaropoulos N, Papacostas E, Papalada A, et al. Acute lateral ankle sprains in track and field athletes: An expanded classification. Foot Ankle Clin. 2006;11(3):497–507. [DOI] [PubMed] [Google Scholar]
- [18].Bennell K, Talbot R, Wajswelner H, et al. Intra-rater and inter-rater reliability of a weight-bearing lunge measure of ankle dorsiflexion. Aust J Physiother. 1998;44(3):175–180. [DOI] [PubMed] [Google Scholar]
- [19].Cejudo A, Sainz de Baranda P, Ayala F, et al. A simplified version of the weight-bearing ankle lunge test: Description and test-retest reliability. Man Ther [Internet]. 2014;194:355–359. [DOI] [PubMed] [Google Scholar]
- [20].Powden CJ, Hoch JM, Hoch MC. Reliability and minimal detectable change of the weight-bearing lunge test: A systematic review. Man Ther [Internet]. 2015;20(4):524–532. [DOI] [PubMed] [Google Scholar]
- [21].Hawker GA, Mian S, Kendzerska T, et al. Measures of adult pain: visual analog scale for pain (VAS pain), numeric rating scale for pain (NRS pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP). Arthritis Care Res. 2011;63(SUPPL. 11):240–252. [DOI] [PubMed] [Google Scholar]
- [22].Gribble PA, Hertel J, Plisky P. Using the star excursion balance test to assess dynamic postural-control deficits and outcomes in lower extremity injury: A literature and systematic review. J Athl Train. 2012;47(3):339–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Docherty CL, Valovich McLeod TC, Shultz SJ. Postural control deficits in participants with functional ankle instability as measured by the balance error scoring system. Clin J Sport Med. 2006;16(3):203–208. [DOI] [PubMed] [Google Scholar]
- [24].Herman G, Nakdimon O, Levinger P, et al. Agreement of an evaluation of the forward-step-down test by a broad cohort of clinicians with that of an expert panel. J Sport Rehabil. 2016;25(3):227–232. [DOI] [PubMed] [Google Scholar]
- [25].Lebleu J, Mahaudens P, Pitance L, et al. Effects of ankle dorsiflexion limitation on lower limb kinematic patterns during a forward step-down test. Journal of Back and Musculoskeletal Rehabilitation -1 (2018) 1–12. [DOI] [PubMed] [Google Scholar]
- [26].Carcia CR, Martin RRL, Drouin JM. Validity of the foot and ankle ability measure in athletes with chronic ankle instability. J Athl Train. 2008;43(2):179–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Borloz S, Crevoisier X, Deriaz O, et al. Evidence for validity and reliability of a French version of the FAAM. BMC Musculoskelet Disord. 2011;12. 10.1186/1471-2474-12-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Vicenzino B, Paungmali A, Teys P. Mulligan’s mobilization-with-movement, positional faults and pain relief: current concepts from a critical review of literature. Man Ther. 2007;12(2):98–108. [DOI] [PubMed] [Google Scholar]
- [29].Hing W, Bigelow R, Bremner T. Mulligan’s mobilization with movement: A systematic review. J Man Manip Ther. 2009;17(2):39E–66E. [Google Scholar]
- [30].Lin CY, Shau YW, Wang CL, et al. Quantitative evaluation of the viscoelastic properties of the ankle joint complex in patients suffering from ankle sprain by the anterior drawer test. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1396–1403. [DOI] [PubMed] [Google Scholar]
- [31].Reid A, Birmingham TB, Alcock G. Efficacy of mobilization with movement for patients with limited dorsiflexion after ankle sprain: a cro. Physiother Canada [Internet]. 2007;59(3):166–172. [Google Scholar]
- [32].Nguyen AP, Mahaudens P, Detrembleur C, et al. Inferior tibiofibular joint mobilization with movement and taping does not improve chronic ankle dorsiflexion stiffness: a randomized placebo-controlled trial. J Man Manip Ther [Internet]. 2020;1–10. 10.1080/10669817.2020.1805690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Haavik H, Murphy B. The role of spinal manipulation in addressing disordered sensorimotor integration and altered motor control. J Electromyogr Kinesiol [Internet]. 2012;225:768–776. [DOI] [PubMed] [Google Scholar]
- [34].Hall EA, Chomistek AK, Kingma JJ, et al. Balance- and strength-training protocols to improve chronic ankle instability deficits, part I: Assessing clinical outcome measures. J Athl Train. 2018;53(6):568–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Todd KH, Funk JP. The minimum clinically important difference in physician-assigned visual analog pain scores. Acad Emerg Med. 1996;3(2):142–146. [DOI] [PubMed] [Google Scholar]
- [36].Zeppieri Jr G, Bialosky J, George SZ. Importance of outcome domain for patients with musculoskeletal pain: Characterizing subgroups and their response to treatment. Phys Ther. 2020;100(5):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Whyte J, It’s more ht.than a black box; it’s a Russian doll. Am J Phys Med Rehabil. 2003;82(8):639–652. [DOI] [PubMed] [Google Scholar]
- [38].Sedgwick P, Greenwood N. Understanding the Hawthorne effect. BMJ. 2015;351(September):1–2. [DOI] [PubMed] [Google Scholar]
- [39].Weerasekara I, Osmotherly PG, Snodgrass S, et al. Is the fibula positioned anteriorly in weight-bearing in individuals with chronic ankle instability? A case control study. J Man Manip Ther [Internet]. 2020:1–8. 10.1080/10669817.2020.1844852 [DOI] [PMC free article] [PubMed] [Google Scholar]


