BACKGROUND
The swiftness with which the coronavirus gripped the world presented unique challenges to both clinical practice and training in the medical field. Clinics across the nation (and the world) were forced to adapt drastically to a new medical reality, one that puts patients at unacceptable risk just by their physical presence in the clinic waiting room. Telemedicine (TM), the remote diagnosis and treatment of patients through telecommunications technology, quickly became the norm for medical care.
ROLE OF TM IN CLINICAL SLEEP MEDICINE
Sleep medicine is uniquely poised to leverage TM for patient care. Evidence exists that sleep disorders like insomnia and obstructive sleep apnea are increasing in prevalence1,2 and, for most patients with insomnia or obstructive sleep apnea, seamless TM models can deliver high-quality care.3 The options for TM include synchronous visits, consisting of telephone and video visits, and asynchronous care models (store and forward). Asynchronous care refers to the evaluation and management of patients by clinician review of patient symptoms, study results (ie, polysomnogram, multiple sleep latency test), patient generated data (ie, positive airway pressure compliance reports), and other relevant health-related data without real-time interaction. As TM becomes a mainstay in medical care, medical training must include education regarding this new method to deliver care. Efficiency in patient care, infection prevention, improved access and expeditious diagnostics, and care management are all potential gains of TM, which pave the way for change in the future of sleep medicine clinical practice and training in the aftermath of the current pandemic.
ROLE OF TM IN SLEEP EDUCATION
A dire need exists to better integrate and educate sleep medicine fellows in TM care. Recently, the Accreditation Council for Graduate Medical Education put out a statement broadly encouraging medical training sites to engage residents and fellows in patient care through the use of TM.4 The American Academy of Sleep Medicine has recommendations for TM visits;5 however the guidelines do not address the fellow’s inclusion. Sleep medicine fellowship curricula, specifically, have no guidelines for TM education.6 In a recent survey, 33% of sleep medicine fellowship program directors offered some TM experience to fellows.7 None had a standard TM curriculum for fellows. The lack of standardization places both fellows and supervisors in potentially uncomfortable positions without clear expectations, given that the use of virtual care models in training was less common prior to the onset of the pandemic.
MODEL OF VIRTUAL SLEEP EDUCATION IN THE CLINICAL LEARNING ENVIRONMENT
Here we provide the experience of our fellows with TM implementation at our training sites. Due to the urgent need for adaptation to virtual care, the clinical workflow was developed at each academic site according to local resources after leadership approval. The model gradually evolved after continuous monitoring and addressing the gaps. The goal was to increase the use of TM by fellows in a graded manner that allowed for increasing involvement and independence for fellows while allowing time for both the supervisors and fellows to become more comfortable with supervision of a virtual encounter. Expectations were set at the beginning with each supervisor regarding the mode of supervision, degree and timing of supervisor involvement, and feedback system. Our fellowship provides clinical training over three separate health organizations and thus implementation of TM varied between the sites. Additionally, the pandemic touched down in the latter half of the fellowship year, and our fellows had ample experience with sleep medicine clinic visits and were able to transition expediently to more independent TM visits. Basic training in TM techniques, including ethical, legal, and regulatory considerations, was provided through mandatory online learning modules. Remote access was granted after approval from the fellowship program director and the education office. Teaching regarding the technology platform, mode of communication, and workflow process was completed before fellows started providing virtual care. The pace and order of introduction of virtual modes varied at the different teaching sites.
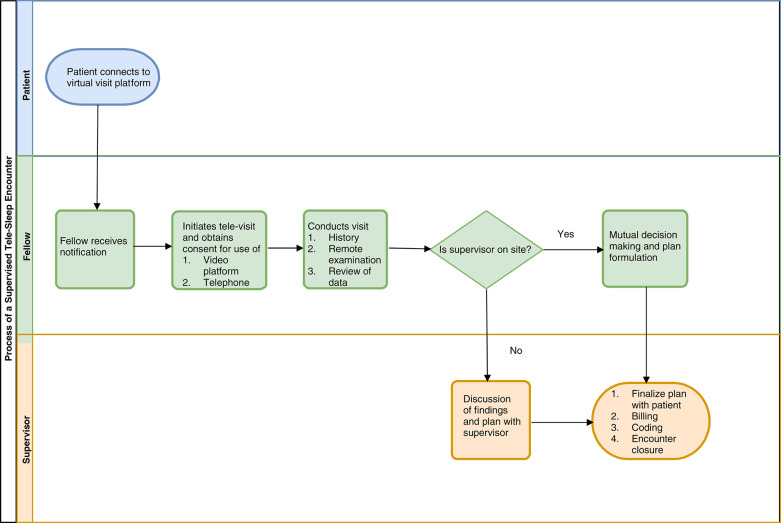
Telephone encounters, being the most rudimentary of the options, were introduced first. The fellow would initiate and conduct the visit with inclusion of the supervisor through a conference call to finalize the medical decision making for new patients. For follow-up patients, supervisors were included in the visit if deemed necessary by the supervisor and fellow; in some cases the supervisor would call the patient separately to complete the encounter. Video conference visits were more complex for a variety of reasons, including the technology required, the choice of platform options, and varying degrees of comfort and knowledge with the technology, and as such were introduced into the learning environment later. Clinic staff were instrumental in assisting patients in preparation for visits, obtaining consent, use of software, and awareness of appointment times. Video visits required patients to click on a link sent to their email allowing them to connect to the provider in a virtual medical room. Different videoconferencing platforms (Microsoft Teams, Virtual Care Manager, Zoom, Amwell [Redmond, WA; VHA Office of Connected Care, Washington, DC; Tokyo, Japan; Boston, MA; respectively]) compatible with desktop, laptop, and mobile phone, and approved by local institutional authorities and HIPAA compliant, were used at each institution. Conduct and supervision of the video encounter varied by institution. Rarely, the fellow and supervisor would attend in the same physical room. In these instances, the fellow would conduct most of the visit and the supervisor would join at the end. The discussion between fellow and supervisor, as well as completion of the visit, would be carried out with both providers keeping as much physical distance as possible and wearing personal protective equipment as recommended at the institutional level. At one institution, the TM visits for new patients were initiated and led by the fellow with the supervisor’s audio muted and video disconnected, allowing the supervisor to observe the encounter. Supervisors would then engage in the visit at the end to finalize the plan and decision making. For complex cases, the fellow and supervisor would have a separate discussion by telephone if needed. At another institution, the video visits were performed by both the supervisor and fellow co-participating in the virtual visit while physically distanced. Figure 1 provides a process map for virtual clinical encounters involving a fellow.
Figure 1. Process of a supervised tele-sleep encounter.
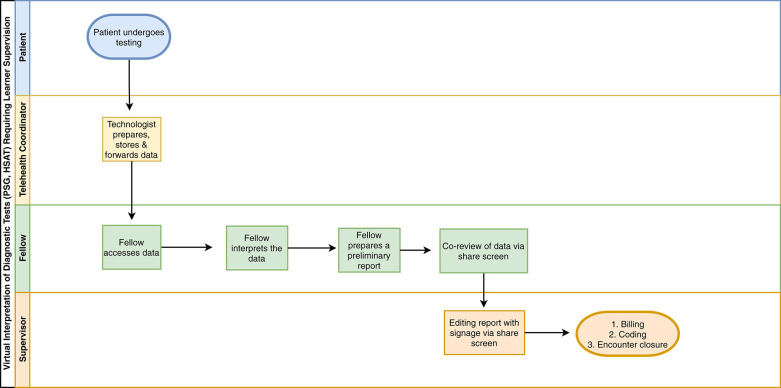
Another important aspect of sleep medicine education is the interpretation of various diagnostic tests. At one institution, polysomnogram interpretation was done synchronously using the “share screen” function via the video conference platform with the supervisor and fellow discussing the findings in real time. In another institution, both the fellow and supervisor reviewed the polysomnogram independently followed by joint interpretation and discussion prior to finalization. Similar methods were used regarding home sleep apnea tests, actigraphy evaluation, and continuous positive airway pressure (CPAP) monitoring. Figure 2 provides a process map for virtual diagnostic learning.
Figure 2. Virtual interpretation of diagnostic tests (PSG, HSAT) requiring learner supervision.
HSAT = home sleep apnea test, PSG = polysomnography.
Sleep medicine is a specialty that accepts fellows from all the primary medical fields, and there is inconsistent exposure to sleep medicine at the medical school and postgraduate training level. Thus, an individual’s comfort with the practice of sleep medicine at the onset of fellowship varies considerably. A benefit of TM is that it is possible to tailor the supervisor’s level of involvement in a nuanced fashion, from full participation, to passive observation, and eventual limited engagement. In our experience, being closer to the end of fellowship, independence in clinical assessment and decision making on the fellow’s part was of high importance, and supervisor involvement was scaled back as soon as was comfortable. Importantly, the methods used above should be tailored based on fellow experience, clinical workflow, and organizational regulations.
STRATEGIES TO ENHANCE TELE-SLEEP EDUCATION
Areas in sleep medicine education pertaining to TM that are worthy of a concerted effort include comprehensive curriculum development compliant with ethical and legal regulations and standardized assessment of the fellows for measurable milestones of professional growth.
Developing and enhancing current education models to address these facets would be beneficial and, arguably, critical for positive outcomes. The following strategies may be helpful to achieving the goal of training fellows in tele-sleep medicine:
Collaboration between the education department and clinical leadership is key to developing a concrete plan that will facilitate a multidirectional relationship between the fellow, supervisor, and patient without hindering workflow. This will lead to an environment where all participants of the visit benefit.
Fellows should undergo required orientation and standardized training modules regarding TM professional conduct, ethical considerations, technical operations, documentation, and after-care/follow-up.
TM training protocols for supervisors must also be established to provide a framework for tele-sleep education and virtual precepting.
Interval monitoring and feedback processes should be in place to ensure that fellows and supervisors can identify areas of improvement.
Relevant milestones in core competencies should be developed and standardized to assess the fellow’s competency in tele-sleep education.
Annual program evaluation should include tele-sleep education to allow for ongoing improvement in seamless patient care and fellow education.
Additionally, further opportunities for research and educational activities will undoubtedly be forthcoming. Areas of future clinical research should include comparisons between TM and clinic visits (health outcomes, show rates, patient satisfaction, etc), as well as evaluation of learning outcomes achieved through tele-education compared to traditional training. The analysis of such data will be instrumental in updating sleep medicine fellowship guidelines.
LIMITATIONS OF TM
While the gains attributable to TM are profound, there are some inherent challenges and concerns regarding its use. General limitations to TM include equitability (technology may not be available to all patients equally), potential for diminished patient engagement (lack of a “captive audience”), variable technological capability of patients and providers, potential for technological malfunction, need for technical and administrative support, and limitation of the physical exam. From a training perspective, an intangible benefit to the physical clinic experience is the potential for interactions among providers, co-fellows, and other learners, such as residents and medicals students, that often leads to spontaneous opportunities for learning, discussion, and collaboration. A specific limitation to TM practice in sleep relates to CPAP therapy for obstructive sleep apnea. This common sleep condition presents a unique challenge to virtual visits as data from the CPAP machine is an important component of providing effective care. At our training sites, each institution has handled the data monitoring differently. One institution has invested in integration of CPAP data into the electronic medical record. Another institution continues to monitor all of the CPAP users through a cloud-based service, replacing older models when feasible (this is the local Veterans Administration hospital where patient-wide changes can be implemented). The third institution has had to rely heavily on clinic staff to obtain CPAP data from the durable medical equipment companies via fax or by the patient sending the CPAP data card through the mail. This presents a comparative challenge to virtual visits, as otherwise patients can bring their devices in and the data can be accessed directly. While this is a current barrier, the reality is that this is rapidly changing as virtually all new CPAP machines have cloud-based data storage, and internet services continue to be expanded to reach more rural areas. It is important to recognize these barriers so conscious efforts can be directed toward mitigating them.
CONCLUSIONS
As coronavirus infections spread in the country it was paramount to first ensure the safety of patients and health care workers as much as possible, while putting all efforts into containment and management of the disease. Nevertheless, the tragedy has accelerated the adoption of technological advancements in medicine. Here, we outlined and emphasized the importance of advancing medical training in TM for sleep medicine fellowships across the country. As medical stewards, it is incumbent upon us to improve upon the areas of weakness made bare through circumstance. This is true for every cross-section in health care, from the individual patient encounter to health care at the population and policy level. Similarly, this must also hold true at the training level within the field of medicine.
DISCLOSURE STATEMENT
All the authors have seen and approved the manuscript. The authors report no conflicts of interest.
ABBREVIATIONS
- CPAP
continuous positive airway pressure
- TM
telemedicine
Citation: Ryba-White B, Gupta S, Khalil W, Irfan M. Integrating telemedicine into sleep medicine: a learner’s perspective. J Clin Sleep Med. 2021;17(12):2573–2576.
REFERENCES
- 1.Calem M, Bisla J, Begum A, et al . Increased prevalence of insomnia and changes in hypnotics use in England over 15 years: analysis of the 1993, 2000, and 2007 National Psychiatric Morbidity Surveys . Sleep. 2012. ; 35 ( 3 ): 377 – 384 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Franklin KA, Lindberg E . Obstructive sleep apnea is a common disorder in the population-a review on the epidemiology of sleep apnea . J Thorac Dis. 2015. ; 7 ( 8 ): 1311 – 1322 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murase K, Tanizawa K, Minami T, et al . A randomized controlled trial of telemedicine for long-term sleep apnea continuous positive airway pressure management . Ann Am Thorac Soc. 2020. ; 17 ( 3 ): 329 – 337 . [DOI] [PubMed] [Google Scholar]
- 4.White S . ACGME Response to the Coronavirus (COVID-19). Accreditation Council for Graduate Medical Education website. Published March 8, 2020. . https://acgme.org/Newsroom/Newsroom-Details/ArticleID/10111/ACGME-Response-to-the-Coronavirus-COVID-19 . Accessed August 3, 2020.
- 5.Singh J, Badr MS, Diebert W, et al . American Academy of Sleep Medicine (AASM) Position Paper for the Use of Telemedicine for the Diagnosis and Treatment of Sleep Disorders . J Clin Sleep Med. 2015. ; 11 ( 10 ): 1187 – 1198 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Accreditation Council for Graduate Medical Education . ACGME Program Requirements for Graduate Medical Education in Sleep Medicine. Updated July 1, 2020. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/520_SleepMedicine_2020.pdf?ver=2020-06-29-164058. Accessed August 3, 2020.
- 7.Fields BG, Dholakia SA, Ioachimescu OC . Sleep telemedicine training in fellowship programs: a survey of program directors . J Clin Sleep Med. 2020. ; 16 ( 4 ): 575 – 581 . [DOI] [PMC free article] [PubMed] [Google Scholar]