Abstract
Background
Despite the growing number of studies reporting on periprosthetic joint infection (PJI), there is little information on one-stage exchange arthroplasty for the revision of infected rotating-hinge prostheses, which can be among the most difficult PJI presentations to treat.
Questions/purposes
After one-stage direct exchange revision for an infected rotating-hinge TKA prosthesis, and using a multimodal approach for infection control, we asked: (1) What is the survivorship free from repeat revision for infection and survivorship free from reoperation for any cause? (2) What is the clinical outcome, based on the Oxford Knee Score, of these patients at the latest follow-up?
Methods
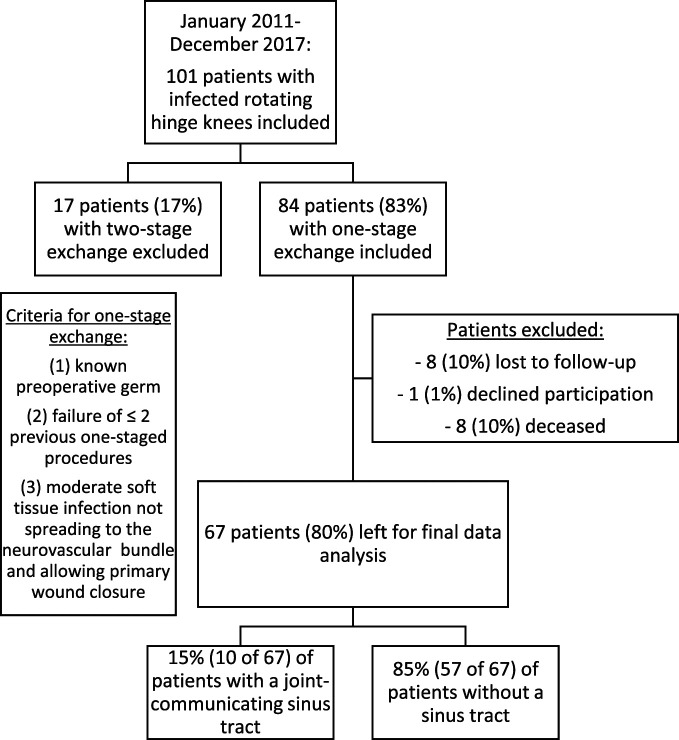
Between January 2011 and December 2017, we treated 101 patients with infected rotating-hinge knee prostheses at our hospital. All patients who underwent a one-stage exchange using another rotating-hinge implant were potentially eligible for this retrospective study. During that period, we generally used a one-stage approach when treating PJIs. Eighty-three percent (84 of 101) of patients were treated with one-stage exchange, and the remainder were treated with two-stage exchange. Of the 84 treated with one-stage exchange, eight patients died of unrelated causes and were therefore excluded, one patient declined to participate in the study, and another eight patients were lost before the minimum study follow-up of 2 years or had incomplete datasets, leaving 80% (67 of 84) for analysis in this study. The included study population consisted of 60% males (40 of 67) with a mean age of 64 ± 8 years and a mean (range) BMI of 30 ± 6 kg/m2 (21 to 40). The mean number of prior surgeries was 4 ± 2 (1 to 9) on the affected knee. Fifteen percent (10 of 67) of knees had a preoperative joint communicating sinus tract, and 66% (44 of 67) had experienced a prior PJI on the affected knee. The antimicrobial regimen was chosen based on the advice of our infectious disease consultant and individually adapted for the organism cultured. The mean follow-up duration was 6 ± 2 years. Kaplan-Meier survivorship analysis was performed using the endpoints of survivorship free from repeat revision for infection and survivorship free from all-cause revision. The functional outcome was assessed using the Oxford Knee Score (on a 12- to 60-point scale, with lower scores representing less pain and greater function), obtained by interviewing patients for this study at their most recent follow-up visit. Preoperative scores were not obtained.
Results
The Kaplan-Meier analysis demonstrated an overall survivorship free from reoperation for any cause of 75% (95% CI 64% to 87%) at the mean follow-up of 6 years postoperatively. Survivorship free from any repeat operative procedure for infection was 90% (95% CI 83% to 97%) at 6 years. The mean postoperative Oxford Knee Score was 37 ± 11 points.
Conclusion
With an overall revision rate of about 25% at 6 years and the limited functional results based on the poor Oxford Knee Scores, patients should be counseled to have modest expectations concerning postoperative pain and function level after one-stage exchange of an infected rotating-hinge arthroplasty. Nevertheless, patients may be informed about a reasonable chance of PJI eradication and might opt for this approach as a means to try to avoid high transfemoral amputation or joint arthrodesis, which in this population often is associated with the inability to ambulate at all. Regarding the relatively high number of patients with aseptic loosening, future studies might focus on implant design of revision knee systems as well. A longer course of oral antibiotics after such procedures may also be warranted to limit the chance of reinfection but requires further study.
Level of Evidence
Level IV, therapeutic study.
Introduction
Periprosthetic joint infection (PJI) is one of the most common indications for early (< 2 years) revision in TKA [9, 38]. Treatment strategies include two-stage and one-stage exchange revision. Although we have observed that the two-stage procedure is in wider use worldwide, the one-stage exchange is the preferred management option in some specialized centers because of the advantages conferred by one procedure and hospitalization [11, 33, 44]. Both treatment methods begin with a radical surgical debridement. Because of the concomitant loss of bone stock and soft tissue defects, surgeons may choose hinged implants to reestablish joint stability and the anatomic leg axis as well as to preserve joint function [7, 10, 25, 29]. A growing number of studies have reported on good clinical outcomes after septic or aseptic revision TKA using rotating-hinge implants [1, 2, 7, 10, 25, 29, 37, 43]. These include studies on septic one-stage exchange TKA, with high eradication rates of 89% to 100% and long-term implant survival as high as 90% at 5 to 10 years [1, 9, 14, 24, 45]. Nevertheless, reinfection rates of 5% to 10% have been reported after aseptic revision TKA [2, 13]. In general, two-stage revision for PJI is associated with a lower risk of revision than one-stage treatment [18], although this has not consistently been found to be true [3, 19-21, 24]. In patients with a history of septic revisions, further reinfections can be especially devastating. Progressive bone loss makes implant fixation much more challenging, which increases the likelihood of subsequent aseptic loosening [7, 9, 30, 32, 35]. Furthermore, recurring PJIs are associated with a higher risk of death [5, 47]. Reducing the hospitalization time, the number of surgical interventions, total time on antibiotics, and patient mortality while managing PJI are all worthy goals [14, 17, 45].
Despite a considerable overall complication rate, revision of the infected hinged knee implant to another rotating-hinge construct may be the last chance for limb preservation for many patients [4, 15, 28]. Therefore, in our institution, after certain exclusion criteria are applied, exchange arthroplasty of infected rotating-hinge knee implants is performed in a one-stage fashion. However, little is known about the results with this approach, especially treating infected revision implants [9]. Since both the chance of reinfection and the level of pain and function influence patients’ postoperative satisfaction with such a procedure, we wanted to analyze the implant survival and functional outcome of patients with infected rotating-hinge knee implants undergoing one-stage revision surgery using the same type of hinged implant.
We therefore asked: After one-stage direct exchange revision for an infected rotating-hinge TKA prosthesis, and using a multimodal approach for infection control, (1) what is the survivorship free from repeat revision for infection and survivorship free from reoperation for any cause? (2) What is the clinical outcome, based on the Oxford Knee Score, of these patients at the latest follow-up?
Patients and Methods
Study Design and Setting
We performed a retrospective study in which we evaluated 101 patients with infected rotating-hinge knee prostheses who were treated at our hospital between January 2011 and December 2017. We did not have preoperative knee scores on these patients, and so we obtained Oxford Knee Scores by interviewing patients for this study at their most recent follow-up visit.
Participants
Exclusion criteria for this study were patients treated with two-stage revision, incomplete clinical records, or a knee prothesis that was different from the removed implant model (Endo-Model Rotating-Hinge Knee System, Waldemar Link). The indications for one-stage exchange in our institution during this study period included a known preoperative organism, a reinfection after not more than two previous one-stage procedures on the affected joint, moderate soft tissue infection not spreading to the neurovascular bundle, and sufficient soft tissue to allow primary wound closure (Fig. 1). In general, our indications for a two-stage approach were an unknown pathogen, more substantial soft tissue defects, or more than two reinfections after one-stage exchange on the affected joint. For this study, we only selected patients who were treated with the same type of knee system before and after one-stage exchange.
Fig. 1.
This flowchart shows patient recruitment (n = 67 patients).
We considered all patients treated with a one-stage exchange using rotating-hinge implants as potentially eligible; 17 patients were excluded because they received a two-stage approach. A further eight patients died, with no death directly attributable to PJI (according to family interview), one patient declined to participate in the study, and another eight patients were lost to follow-up before the minimum study follow-up duration (2 years) or had incomplete datasets, leaving 80% (67 patients) for analysis (Fig. 1).
Patients
The mean age was 64 ± 8 years, and 60% (40 of 67) of patients were males.
Sixty-six percent (44 of 67) of patients had a history of PJI in the affected joint and had undergone other surgical procedures before the one-stage exchange with the hinged implant used and analyzed here. Eleven percent (5 of 44) of these patients were treated with debridement, antibiotics, irrigation, and retention; 9% (4 of 44) of patients were treated with one-stage exchange, and 80% (35 of 44) were treated with two-stage exchange. Nine percent (4 of 44 patients with prior PJI on affected knee) of patients had a surgical lavage before one-stage exchange for the purpose of acute infection control and open biopsy. Implant history included 5% (2 of 44) of patients who underwent conversion from a unicondylar knee prothesis to a rotational hinge prosthesis and 95% (42 of 44 patients) whose implant was changed from a nonhinged (varus-valgus constrained posterior-stabilized) implant to a rotational hinge (Table 1).
Table 1.
Patient characteristics (n = 67)
| Parameter | Value |
| Males | 60 (40) |
| Age in years | 64 ± 8.3 |
| Affected side, left | 54 (36) |
| BMI, kg/m2 | 30 ± 5.7 |
| CRP level, mg/dL | 36 ± 51 |
| Smoking | 10 (7) |
| Diabetes, controlled | 12 (8) |
| Obesity (BMI > 30 kg/m2) | 55 (37) |
| Kidney insufficiency (GFR < 90 mL/min) | 5 (3) |
| Charlson Comorbidity Index score | 3.2 ± 1.6 |
| Number of prior surgical procedures on affected knee | 4.1 ± 1.5 |
| Prior PJI on affected knee | 66 (44) |
| Of whom had a prior treatment via DAIR | 11 (5 of 44) |
| Of whom had a prior treatment via one-stage exchange | 9 (4 of 44) |
| Of whom had a prior treatment via two-stage exchange | 80 (35 of 44) |
| Number of patients with prior joint lavage before current one-stage exchange | 9 (4 of 44) |
| Type of prior exchanged knee protheses before rotational-hinged implantation | |
| Unicondylar knee arthroplasty | 5 (2 of 44) |
| Nonhinged TKA | 95 (42 of 44) |
| Number of patients with preoperative sinus tract | 15 (10) |
| Time from prior surgery to one-stage exchange in months | 21 ± 20 |
| Patients with lavage before one-stage exchange | 13 (9) |
Data presented as % (n) or mean ± SD; CRP = C-reactive protein; GFR = glomerular filtration rate; DAIR = debridement, antibiotics, irrigation, and retention.
A joint-communicating sinus tract was not a contraindication to this approach during the study period. In 15% (10 of 67) of patients, a joint-communicating sinus tract was present (Fig. 1).
Diagnosis of PJI
PJI was diagnosed according to the criteria of the First International Consensus Meeting on PJI [27]. Preoperative joint aspirations were taken in all patients with PJI who had hinged knee implants. Additionally, the presence of a sinus tract communicating with the joint; intraoperative, visible purulence; or positive culture results of intraoperatively taken periprosthetic tissues were considered evidence of PJI. All cultures were incubated for at least 14 days for microbiologic analysis.
Microbiology
The most commonly isolated bacterium was Staphylococcus epidermidis (found in 40% [27 of 67] of knees), followed by Streptococci spp. (13% [9 of 67]) (Supplementary Table 1; http://links.lww.com/CORR/A600).
Among the study population, 66% (44 of 67) of patients had a history of PJI in the affected knee. In 84% (37 of 44) of these patients, the organism spectrum was identical between the previous and present PJI, while in 16% (7 of 44) of patients, a new organism was isolated. The median (range) period between prior septic exchange surgery and the current one-stage exchange in these 44 patients with a history of PJI in the involved knee was 21 months (4 to 85). Nine percent (4 of 44) of patients had a prior joint lavage before one-stage exchange.
Surgical Technique
A one-stage exchange protocol was used for all patients according to the standard ENDO-Klinik protocol [12]. In all patients, the old scar was excised throughout the surgical approach. Radical debridement and excision of the joint capsule and synovial tissue was performed, along with complete removal of all components and cement material. The entire surgical field was irrigated with approximately 1 L of 3% polyhexanide mixed with 3 L of saline solution using a high-pressure lavage system (Lavasept®, B. Braun). When there was severe loss of bone stock, femoral or tibial tantalum cones were used (Waldemar Link). Among the study population of 67 knees, tibial and/or femoral tantalum cones were used because of a loss of bone stock in 48% (32 of 67). Before reimplantation, the surgical gloves of all team members and the overhead light handles and electrocautery and suction tips were replaced. Furthermore, all surgical instruments were replaced and the operating area was redraped. The new implants were planted in antibiotic-loaded bone cement, selected with regard to the individual bacterial spectrum.
Antibiotic Treatment
Because we do not have a fixed general antimicrobial strategy for patients with PJI, the antibiotic treatment was chosen according to the advice of our infectious disease consultant and was adapted to the organism isolated from the prior knee aspiration as well as to patient characteristics such as known allergies and organism susceptibility. Antibiotic-loaded bone cement was intraoperatively prepared and based on the existing culture results and sensitivity patterns. Intravenous antibiotic administration was started intraoperatively, as soon as microbiological and histopathologic tissue samples were obtained. Antibiotics were continued for a mean of 15 ± 4 days. Subsequent oral therapy was prescribed individually. Seventy-two percent (48 of 67) of patients were discharged without any further oral antibiotic treatment. Among the remaining 19 patients, seven were treated with amoxicillin/clavulanacid, five were treated with rifampicin, and two were treated with either linezolid, clindamycin, or ciprofloxacin (two patients each) (Table 2). Regarding the duration of further oral antibiotic treatment after hospital discharge, most patients (11 of 19) received their medication for approximately 14 days. Three patients had a treatment period of 7 days, two had a treatment period of 21 days, and two were treated for more than 3 weeks. One patient was discharged with lifelong antibiotic suppression therapy (amoxicillin) because of a difficult-to-treat Enterobacter cloacae–associated PJI. The decision for duration of antibiotic treatment was made at the discretion of the operative surgeon and generally reflected a more difficult-to-treat organism or a compromised host.
Table 2.
Antibiotic treatment (n = 67 patients)
| Type of administration | Antibiotic drug | Prevalence |
| Local (ALBC) | G + C + V | 35 |
| G + V | 12 | |
| G + C | 10 | |
| G + M + V | 3 | |
| Other combinationsa | 7 | |
| Systemic (intravenous) Given for a mean of 15 ± 4 days |
Ampicillin/sulbactam | 12 |
| V + R | 11 | |
| V + F | 7 | |
| V + M | 4 | |
| Other combinations including V | 7 | |
| I | 6 | |
| Flucloxacillin | 4 | |
| Other combinationsa | 16 | |
| Systemic (oral) Given for a mean of 14 ± 11 days |
Amoxicillin/clavulanic acid | 7 |
| R | 5 | |
| L | 2 | |
| C | 2 | |
| Ciprofloxacin | 2 | |
| Levofloxacin | 1 |
None of these were used in more than one patient; ALBC = antibiotic-loaded bone cement; V = vancomycin; G = gentamycin; M = meropenem; C = clindamycin; R = rifampicin; I = imipenem; F = fosfomycin; L = linezolid.
Primary and Secondary Study Outcome
Our primary study outcome was survivorship free from repeat revision for infection and survivorship free from reoperation for any cause. The secondary outcome was clinical function, as measured via the Oxford Knee Score (on a 12- to 60-point scale, with lower scores representing less pain and greater function) at a minimum follow-up duration of 2 years. Given that we did not have preoperative knee scores on these patients, we obtained Oxford Knee Scores by interviewing patients for this study at their most recent follow-up visit.
Ethical Approval
This study was approved by the institutional review board of Hamburg University College of Medicine (number PV5647). All study procedures followed the tenets of the Declaration of Helsinki, and written informed consent was obtained from all participants. No patients younger than 18 years were included.
Statistical Analysis
Descriptive statistics are presented as the percentage and number, means, ranges, standard error, or SD. For relevant values, 95% confidence intervals were calculated. Kaplan-Meier survivorship analysis was performed using the endpoints of survivorship free from repeat revision for infection and survivorship free from all-cause revision. All data were processed using statistical analysis software (Statistica, Version 13.2).
Results
Survivorship
The Kaplan-Meier analysis demonstrated an overall survivorship free from revision because of PJI of 90% (95% CI 83% to 97%) and free from reoperation for any cause of 75% (95% CI 64% to 87%) at 6 years postoperatively (Fig. 2).
Fig. 2.
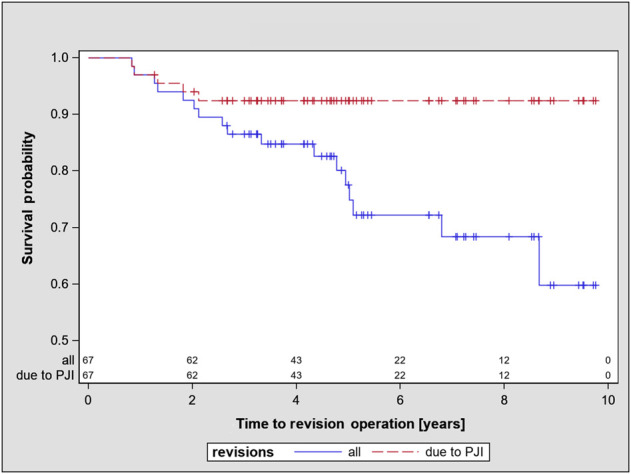
This graph shows the survivorship of overall revisions and revisions for infection (PJI, n = 67 patients).
Twenty-five percent (17 of 67) of patients were surgically revised. These included 9% (6 of 67) septic revisions because of PJI, 12% (8 of 67) aseptic revisions for implant loosening, and 3% (2 of 67) wound healing disorders requiring a superficial debridement followed by primary wound closure. One percent (1 of 67) suffered from recurring PJI, which eventually led to a proximal thigh amputation. Furthermore, 1% percent (1 of 67) were discharged from our hospital with a lifelong antibiotic suppression (amoxicillin) because of a difficult-to-treat E. cloacae–associated PJI. Seventy-five percent (50 of 67) did not undergo further surgical interventions.
Of the six postoperative reinfections throughout the follow-up period, the pathogens were Enterococci in three patients, Staphylococci in two, and Streptococci in one, which corresponded to the previously identified organism spectrum (organism persistence).
Functional Outcome
Since we did not have preoperative knee scores for these patients, we obtained Oxford Knee Scores by interviewing patients for this study at their most recent follow-up visit. Their mean postoperative Oxford Knee Score was 37 ± 11 points, which would be considered in the “poor” range.
Discussion
The treatment of infected revision knee implants is made difficult by the challenge inherent in debriding infected tissue and preventing recurrent infection while maintaining knee stability and gaining acceptable postoperative and patient satisfaction with the outcome. Established therapeutic strategies comprise one- and two-stage surgical procedures. Rotating-hinge prostheses offer improved stability in such settings, but little is known about the outcome of infected rotating-hinge prostheses. We therefore asked, (1) what is the survivorship free from repeat revision for infection and survivorship free from reoperation for any cause? (2) What is the clinical outcome, based on the Oxford Knee Score, of these patients at the latest follow-up?
The most important findings of this midterm follow-up study were that one-stage exchange of infected rotating-hinge knee arthroplasty with another rotating-hinge implant can lead to acceptable infection control, higher revision rates for aseptic loosening, and poor functional outcomes based on postoperative Oxford Knee Scores.
Limitations
The limitations of this study include its retrospective design and the lack of preoperative functional outcome measures. Unfortunately, we did not note the Oxford Knee Score of PJI patients preoperatively despite a thorough preoperative workup. Other scores were used in the past, but we believe the Oxford Knee Score best represents patient function in this setting. Still, the postoperative score alone can provide some valuable insight into the function of these patients. Additionally, 10% (8 of 84) of patients were lost to follow-up. These patients might bias the true outcome of all treated patients in our hospital because some of these patients might have undergone revision in a different hospital or have occult PJIs, lowering our perceived success rate. Furthermore, we have no objective information about posthospital treatment, such as antibiotic medication, in these patients. However, as a tertiary-care, specialized institution treating these difficult patients in our region, we believe most patients with recurring PJI would return to our institution. Finally, we recognize that our institution has specialized expertise in treating such infections with a one-stage approach in the multiply-revised patient, which might limit the generalizability of our results. However, many tertiary-care centers use both one- and two-stage approaches to eradicating infection with rotating-hinge implants, and these results would seem applicable at least in such settings.
Survivorship
In the present study, the infection-free survival rate was high, although survivorship free from reoperation for any cause was lower, at 75% (with a lower bound of 64% on the 95% CI). The varying results of surgical PJI treatment depend on several factors, including the underlying reason for revision, surgical approach, causative organism, and the institution’s infrastructure and experience in creating a multimodal infection protocol. When these factors are considered, one-stage exchange protocols of infected primary TKA can lead to results comparable with those of two-stage procedures in terms of infection control and implant survival [1, 12, 14, 17, 45]. No standardized management protocol for septic revision of rotating-hinge knee implants exists, and we are unaware of other studies that have followed a large number of patients with infected rotating-hinge implants who have undergone one-stage exchange. Our results may be attributed to the specific routines of a high-volume center that specializes in joint arthroplasty as well as perhaps the bacteria that predominated here. Most of the isolated pathogens were S. epidermidis (40% [27 of 67]). Although there are no pathogen-specific, long-term follow-up studies about S. epidermidis in PJI, coagulase-negative Staphylococci are generally considered “easier to handle” [34, 36, 41, 42, 46]. Nevertheless, there was a large percentage (84%) of organism persistence among patients with prior PJI. Organism persistence might be due to either an insufficient surgical debridement or an insufficient duration of the postoperative antibiotic treatment. At our institution, because surgical debridement is always performed by one of five surgeons who specialize in this area and use similar techniques, the antibiotic treatment might be the key factor. Three of six reinfected patients were discharged from our hospital without any further oral antibiotic treatment. These patients only received intravenous antibiotics for 14 days. Under these circumstances, perhaps the therapy for this special group of patients should be reconsidered. In this context, Chieffo et al. [8] recently reported on a postoperative antibiotic course of 6 weeks in patients undergoing one-stage exchange of THA and TKA, gaining an overall remission rate of 90% (44 of 49). In this study, patients were given intravenous antibiotics for a median of 11 days and then switched to a further oral treatment afterwards.
The associated loss of bone stock and compromise of stabilizing soft tissue during septic TKA revision often results in the use of hinged implants for sufficient stabilization [25, 45]. The use of these implants is associated with frequent complications, and a correspondingly lower survival rate [32]. In 40 primary and revision rotating-hinge knees, one study found a 2-year survival rate of 95%. However, in a subgroup of 28 aseptic revision rotating-hinge knees, 46% (13 of 28) experienced complications (of which 14% [4 of 28] underwent revision for infection) [32]. Another study found a 5-year survival rate of 72% (94) in 131 patients after rotating-hinge knee implantation for aseptic or septic revision. In a subgroup of 73 septic revisions, the reinfection rate was 16% (12 of 73) [37]. In a report on a subgroup of 58 implanted rotating-hinge knees after two-stage septic exchange, the 5-year survival rate was 71% (41 of 58) and the reinfection rate was 22% (13 of 58) [7].
When we considered all-cause revision to capture those patients experiencing aseptic loosening as well as repeat or persistent infection, we found that survivorship decreased considerably. This is consistent with the work of others on rotating-hinge TKA revisions. In rotating-hinge knee implants, aseptic loosening is one of the main sources of implant failure [10, 16, 22]. In two recent studies, Levent et al. [22, 23] identified several risk factors for aseptic loosening, including a higher BMI and smoking. One prior study found that larger femoral diaphyseal diameter was associated with a greater risk of aseptic loosening [23], but we did not measure or analyze these risk factors (femoral diaphyseal diameter, BMI, and smoking) in our study. To further reduce mechanical, implant-related causes of revision, the diameters of the femoral diaphysis and implant shaft should be considered more precisely in future studies.
Functional Outcome
In the current study, the mean Oxford Knee Score was 37 points after a mean of 6 years, which may be considered a poor score. Given the complexity of these patients’ presentations, perhaps this is unsurprising, but since we did not have preoperative scores, it is difficult to put this in context. On one hand, some may consider that poor scores for pain and function do not justify major reconstructive surgery; however, given that the alternative in many patients might be a high transfemoral amputation, this may be acceptable to many patients and their surgeons. This is especially important given the age of these patients; patients older than 60 years often do not regain the ability to ambulate after transfemoral amputation [6, 31, 40]. Because of the variety of different scoring systems, comparing the functional results from our study with those of other studies that used other scoring systems [5, 7, 9, 11] is difficult. Tibrewal et al. [39] investigated 50 one-stage septic revision TKAs (nonhinged) and found an Oxford Knee Score of 20 of 60 possible points after 1 year (on the Oxford Knee Score 60-point scale, lower points indicate better function). A study of 70 patients who underwent one-stage exchange of infected TKA to rotating-hinge knee implants found a mean Hospital for Special Surgery score of 70 ± 23 points after a minimum follow-up of 9 years [45]. On the Hospital for Special Surgery scale, a higher point total represents better functional outcome, and 70 points would represent fair to good results. Cottino et al. [10] reported a Knee Society clinical score of 81 points (100-point scale, 81 points representing excellent results) and Knee Society functional score of 36 of 100 points (36 points corresponding to poor results) after a mean of 4 years after rotating-hinge knee implantation for revision (82% [334 of 408]) and primary (18% [74 of 408]) TKA in 408 patients, but only 11% (45 of 408) underwent revision for PJI. Another study found that the clinical outcome score at 5 years after two-stage rotating-hinge knee implantation was 71 for the Knee Society clinical score and 57 for the Knee Society functional score [7]. Most recently, Ohlmeier et al. [25] evaluated 52 patients who underwent aseptic (67% [35 of 52]) and septic (33% [17 of 52]) revision TKA and had extensive loss of bone stock. All patients received rotating-hinge knee implants and femoral and/or tibial cones. After 17 months, the functional outcome as measured with the Oxford Knee Score was 29 of 60 possible points. Almost half of the patients in our group also received tibial and/or femoral cones because of an extensive loss of bone stock.
Considering the limited expectations one should have based on the Oxford Knee Scores we observed, patients should be counseled not to expect high functional levels, and that moderate pain (or worse) may well persist. Still, patients may opt for this as a means to try to avoid high transfemoral amputation or knee arthrodesis, which in this population often is associated with the inability to ambulate [26, 31].
Conclusion
In light of an all-cause revision rate of about 25% at 6 years, and the limited expectations one should have based on the Oxford Knee Scores we observed, patients should be counseled that this may not be their last revision, and patient expectations should be managed realistically with shared decision-making. Still, patients may opt for this approach as a means to try to avoid high transfemoral amputation and maintain ambulatory ability. Regarding the relatively high percentage of aseptic loosening, future studies might focus on implant design of revision knee systems to gain higher long-term survival in these sclerotic bone situations. A longer oral antibiotic course after such procedures may also be warranted to limit the chance of reinfection, but this also requires further study.
Supplementary Material
Acknowledgments
We thank Silke Lange DSc, for the statistical analysis as well as Corona von Poehl MD, for identifying the patients records from our database. Furthermore, we thank Lars Frommelt MD for his long-time job as our infectious disease consultant, and we wish him a well-deserved annuity.
Footnotes
One of the authors (TG) reports personal fees in an amount more than USD 10,000 from Zimmer and personal fees in an amount more than USD 10,000 from Link, outside the submitted work. One of the authors (MC) reports personal fees in an amount less than USD 10,000 from Waldemar Link, outside the submitted work.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, or any drug or device before clinical use.
Ethical approval for this study was obtained from the Hamburg University College of Medicine, Hamburg, Germany (number PV5647).
This work was performed at ENDO-Klinik, Hamburg, Germany.
Contributor Information
Fadi Alrustom, Email: fadi.alrustom@gmail.com.
Mustafa Citak, Email: mcitak@gmx.de.
Jochen Salber, Email: jochen.salber@kk-bochum.de.
Thorsten Gehrke, Email: thorsten.gehrke@helios-gesundheit.de.
Jannik Frings, Email: j.frings@uke.de.
References
- 1.Abdelaziz H, Biewald P, Anastasiadis Z, et al. Midterm results after tantalum cones in 1-stage knee exchange for periprosthetic joint infection: a single-center study. J Arthroplasty. 2020;35:1084-1089. [DOI] [PubMed] [Google Scholar]
- 2.Abdelaziz H, Jaramillo R, Gehrke T, et al. Clinical survivorship of aseptic revision total knee arthroplasty using hinged knees and tantalum cones at minimum 10-year follow-up. J Arthroplasty. 2019;34:3018-3022. [DOI] [PubMed] [Google Scholar]
- 3.Belay ES, Danilkowicz R, Bullock G, al at. Single-stage versus two-stage revision for shoulder periprosthetic joint infection: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2020;29:2476-2486. [DOI] [PubMed] [Google Scholar]
- 4.Berend KR, Lombardi AV, Jr. Distal femoral replacement in nontumor cases with severe bone loss and instability. Clin Orthop Relat Res. 2009;467:485-492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berend KR, Lombardi AV, Jr, Morris MJ, et al. Two-stage treatment of hip periprosthetic joint infection is associated with a high rate of infection control but high mortality. Clin Orthop Relat Res. 2013;471:510-518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen AF, Kinback NC, Heyl AE, et al. Better function for fusions versus above-the-knee amputations for recurrent periprosthetic knee infection. Clin Orthop Relat Res. 2012;470:2737-2745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen MJ, Hung JF, Chang CH, et al. Periprosthetic knee infection reconstruction with a hinged prosthesis: implant survival and risk factors for treatment failure. Knee. 2020;27:1035-1042. [DOI] [PubMed] [Google Scholar]
- 8.Chieffo G, Corsia S, Rougereau G, et al. Six-week antibiotic therapy after one-stage replacement arthroplasty for hip and knee periprosthetic joint infection. Med Mal Infect. 2020;50:567-574. [DOI] [PubMed] [Google Scholar]
- 9.Citak M, Friedenstab J, Abdelaziz H, et al. Risk factors for failure after 1-stage exchange total knee arthroplasty in the management of periprosthetic joint infection. J Bone Joint Surg Am. 2019;101:1061-1069. [DOI] [PubMed] [Google Scholar]
- 10.Cottino U, Abdel MP, Perry KI, et al. Long-term results after total knee arthroplasty with contemporary rotating-hinge prostheses. J Bone Joint Surg Am. 2017;99:324-330. [DOI] [PubMed] [Google Scholar]
- 11.Gehrke T, Alijanipour P, Parvizi J. The management of an infected total knee arthroplasty. Bone Joint J. 2015;97:20-29. [DOI] [PubMed] [Google Scholar]
- 12.Gehrke T, Zahar A, Kendoff D. One-stage exchange: it all began here. Bone Joint J. 2013;95:77-83. [DOI] [PubMed] [Google Scholar]
- 13.Gudnason A, Milbrink J, Hailer NP. Implant survival and outcome after rotating-hinge total knee revision arthroplasty: a minimum 6-year follow-up. Arch Orthop Trauma Surg. 2011;131:1601-1607. [DOI] [PubMed] [Google Scholar]
- 14.Haddad FS, Sukeik M, Alazzawi S. Is single-stage revision according to a strict protocol effective in treatment of chronic knee arthroplasty infections? Clin Orthop Relat Res. 2015;473:8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kearns SM, Culp BM, Bohl DD, et al. Rotating hinge implants for complex primary and revision total knee arthroplasty. J Arthroplasty. 2018;33:766-770. [DOI] [PubMed] [Google Scholar]
- 16.Kienzle A, Walter S, von Roth P, et al. High rates of aseptic loosening after revision total knee arthroplasty for periprosthetic joint infection. JB JS Open Access. 2020;5:e20.00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kildow BJ, Della-Valle CJ, Springer BD. Single vs 2-stage revision for the treatment of periprosthetic joint infection. J Arthroplasty. 2020;35:S24-S30. [DOI] [PubMed] [Google Scholar]
- 18.Kunutsor SK, Whitehouse MR, Blom AW, et al. Re-infection outcomes following one- and two-stage surgical revision of infected hip prosthesis: a systematic review and meta-analysis. PloS One. 2015;10:e0139166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kunutsor SK, Whitehouse MR, Blom AW, et al. One- and two-stage surgical revision of peri-prosthetic joint infection of the hip: a pooled individual participant data analysis of 44 cohort studies. Eur J Epidemiol. 2018;33:933-946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kunutsor SK, Whitehouse MR, Lenguerrand E, et al. Re-infection outcomes following one- and two-stage surgical revision of infected knee prosthesis: a systematic review and meta-analysis. PloS One. 2016;11:e0151537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kunutsor SK, Wylde V, Beswick AD, et al. One- and two-stage surgical revision of infected shoulder prostheses following arthroplasty surgery: a systematic review and meta-analysis. Sci Rep. 2019;9:232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levent A, Suero EM, Gehrke T, et al. Risk factors for aseptic loosening in complex revision total knee arthroplasty using rotating hinge implants. Int Orthop. 2021;45:125-132. [DOI] [PubMed] [Google Scholar]
- 23.Levent A, Suero EM, Gehrke T, et al. Risk factors for aseptic loosening after total knee arthroplasty with a rotating-hinge implant: a case-control study. J Bone Joint Surg Am. 2021;103:517-523. [DOI] [PubMed] [Google Scholar]
- 24.Masters JP, Smith NA, Foguet P, et al. A systematic review of the evidence for single stage and two stage revision of infected knee replacement. BMC Musculoskelet Disord. 2013;14:222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ohlmeier M, Lausmann C, Wolff M, et al. Preliminary clinical results of coated porous tibia cones in septic and aseptic revision knee arthroplasty. Arch Orthop Trauma Surg. 2021;141:555-560 [DOI] [PubMed] [Google Scholar]
- 26.Orfanos AV, Michael RJ, Keeney BJ, et al. Patient-reported outcomes after above-knee amputation for prosthetic joint infection. Knee. 2020;27:1101-1105. [DOI] [PubMed] [Google Scholar]
- 27.Parvizi J, Gehrke T, Chen AF. Proceedings of the International Consensus on Periprosthetic Joint Infection. Bone Joint J. 2013;95:1450-1452. [DOI] [PubMed] [Google Scholar]
- 28.Pasquier G, Ehlinger M, Mainard D. The role of rotating hinge implants in revision total knee arthroplasty. EFORT Open Rev. 2019;4:269-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Petis SM, Perry KI, Mabry TM, et al. Two-stage exchange protocol for periprosthetic joint infection following total knee arthroplasty in 245 knees without prior treatment for infection. J Bone Joint Surg Am. 2019;101:239-249. [DOI] [PubMed] [Google Scholar]
- 30.Pradhan NR, Bale L, Kay P, et al. Salvage revision total knee replacement using the Endo-Model rotating hinge prosthesis. Knee. 2004;11:469-473. [DOI] [PubMed] [Google Scholar]
- 31.Rodriguez-Merchan EC. Knee fusion or above-the-knee amputation after failed two-stage reimplantation total knee arthroplasty. Arch Bone Jt Surg. 2015;3:241-243. [PMC free article] [PubMed] [Google Scholar]
- 32.Rouquette L, Batailler C, Muller B, et al. Early complications and causes of revision after rotating-hinge TKA. Arch Orthop Trauma Surg. 2020;140:109-119. [DOI] [PubMed] [Google Scholar]
- 33.Rowan FE, Donaldson MJ, Pietrzak JR, et al. The role of one-stage exchange for prosthetic joint infection. Curr Rev Musculoskelet Med. 2018;11:370-379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schilcher K, Horswill AR. Staphylococcal biofilm development: structure, regulation, and treatment strategies. Microbiol Mol Biol Rev. 2020;84:e00026-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smith TH, Gad BV, Klika AK, et al. Comparison of mechanical and nonmechanical failure rates associated with rotating hinged total knee arthroplasty in nontumor patients. J Arthroplasty. 2013;28:62.e1. [DOI] [PubMed] [Google Scholar]
- 36.Stefansdottir A, Johansson D, Knutson K, et al. Microbiology of the infected knee arthroplasty: report from the Swedish Knee Arthroplasty Register on 426 surgically revised cases. Scand J Infect Dis. 2009;41:831-840. [DOI] [PubMed] [Google Scholar]
- 37.Theil C, Schmidt-Braekling T, Gosheger G, et al. Acceptable mid- to long-term survival rates and functional outcomes following a single design rotating hinge total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2020;28:1868-1875. [DOI] [PubMed] [Google Scholar]
- 38.Thiele K, Perka C, Matziolis G, et al. Current failure mechanisms after knee arthroplasty have changed: polyethylene wear is less common in revision surgery. J Bone Joint Surg. 2015;97:715-720. [DOI] [PubMed] [Google Scholar]
- 39.Tibrewal S, Malagelada F, Jeyaseelan L, et al. Single-stage revision for the infected total knee replacement: results from a single centre. Bone Joint J. 2014;96:759-764. [DOI] [PubMed] [Google Scholar]
- 40.Trouillez T, Faure PA, Martinot P, et al. Above-the-knee amputation versus knee arthrodesis for revision of infected total knee arthroplasty: recurrent infection rates and functional outcomes of 43 patients at a mean follow-up of 6.7 years. Orthop Traumatol Surg Res. 2021;107:102914. [DOI] [PubMed] [Google Scholar]
- 41.Ull C, Yilmaz E, Baecker H, et al. Microbial findings and the role of difficult-to-treat pathogens in patients with periprosthetic infection admitted to the intensive care unit. Orthop Rev. 2020;12:8867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Valour F, Trouillet-Assant S, Rasigade JP, et al. Staphylococcus epidermidis in orthopedic device infections: the role of bacterial internalization in human osteoblasts and biofilm formation. PloS One. 2013;8:e67240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yoon JR, Cheong JY, Im JT, et al. Rotating hinge knee versus constrained condylar knee in revision total knee arthroplasty: a meta-analysis. PloS One. 2019;14:e0214279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zahar A, Gehrke TA. One-stage revision for infected total hip arthroplasty. Orthop Clin North Am. 2016;47:11-18. [DOI] [PubMed] [Google Scholar]
- 45.Zahar A, Kendoff DO, Klatte TO, et al. Can good infection control be obtained in one-stage exchange of the infected TKA to a rotating hinge design? 10-year results. Clin Orthop Relat Res. 2016;474:81-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zeller V, Kerroumi Y, Meyssonnier V, et al. Analysis of postoperative and hematogenous prosthetic joint-infection microbiological patterns in a large cohort. J Infect. 2018;76:328-334. [DOI] [PubMed] [Google Scholar]
- 47.Zmistowski B, Karam JA, Durinka JB, et al. Periprosthetic joint infection increases the risk of one-year mortality. J Bone Joint Surg. 2013;95:2177-2184. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.