Abstract
Background
Orthopaedic surgery training programs have lagged behind other surgical specialties in increasing their representation of women and people from under-represented minority (URM) groups. Comparative data between orthopaedic surgery and other specialties are needed to help identify solutions to closing the diversity gap.
Questions/purposes
(1) Which surgical specialties have the greatest representation of women residents and residents from URM groups? (2) How have the proportions of women residents and residents from URM groups changed across the surgical specialties during the past decade?
Methods
This was a retrospective evaluation of a large, longitudinally maintained survey database. Resident data by gender and ethnicity were retrieved from the Accreditation Council for Graduate Medical Education Data Resource Books for the 2011 to 2012 through 2019 to 2020 academic years. The Accreditation Council for Graduate Medical Education database is updated annually; thus, it is the most up-to-date and complete database available for gender and ethnicity data for all surgical residents. Data were obtained and analyzed for seven different surgical specialties: orthopaedic surgery, neurosurgery, ophthalmology, otolaryngology, plastic surgery, general surgery, and urology. No sampling was necessary, and thus descriptive statistics of the data were completed. Because the entire population of residents was included for the period of time in question, no statistical comparisons were made, and the reported differences represent absolute differences between the groups for these periods. Linear regression analyses were performed to estimate the annual growth rates of women residents and residents from URM groups in each specialty.
Results
Among the seven surgical specialties, representation of women residents increased from 28% (4640 of 16,854) of residents in 2012 to 33% (6879 of 20,788) in 2020. Orthopaedic surgery had the lowest representation of women residents every year, with women residents comprising 16% of residents (700 of 4342) in 2020. Among the seven surgical specialties, representation of residents from URM groups increased from 8.1% (1362 of 16,854) in 2012 to 9.7% (2013 of 20,788) in 2020. In 2020, the representation of residents from URM groups in orthopaedic surgery was 7.7% (333 of 4342). In 2020, general surgery had the highest representation of women residents (42%; 3696 of 8809) as well as residents from URM groups (12%; 1065 of 8809). Plastic surgery (1.46% per year) and general surgery (0.95% per year) had larger annual growth rates of women residents than the other specialties did. In each surgical specialty, the annual growth rate of residents from URM groups was insignificant.
Conclusion
During the past decade, there was only a small increase in the representation of women in orthopaedic surgery, while the representation of people from URM groups did not change. In contrast, by 2020, general surgery had become the most diverse among the seven surgical specialties. To increase diversity in our field, we need to evaluate and implement some of the effective interventions that have helped general surgery become the diverse surgical specialty that it is today.
Clinical Relevance
General surgery has substantially reduced gender and ethnic disparities that existed in the past, while those in orthopaedic surgery still persist. General surgery residencies have implemented a holistic review of resident applications and longitudinal mentoring programs to successfully address these disparities. Orthopaedic surgery programs should consider placing less emphasis on United States Medical Licensing Examination score thresholds and more weight on applicants’ non-academic attributes, and put more efforts into targeted longitudinal mentorship programs, some of which should be led by non-minority faculty.
Introduction
Having a diverse and balanced workforce in which populations of physicians generally represent the patients whom they serve in terms of gender, race, and ethnicity has been associated with improved clinical care and patient satisfaction [9, 27, 30]. Historically, women and people from under-represented minority (URM) groups have constituted a small percentage of practicing physicians relative to the demographic make-up of the general population. In 1970, 11% of students in medical schools were women, and an even smaller percentage of medical students were considered to be from URM groups [7]. There has been increased representation during the past five decades, with more women matriculating to medical school than men in 2020 and people from URM groups comprising approximately 22% of total matriculants [5]. However, this upward trend of women and URM representation in medicine has not been observed in many surgical specialties, particularly orthopaedic surgery [25].
Studies have found that women constitute less than 15% of orthopaedic surgery residents [7, 25]. Similarly, the percentage of residents in orthopaedic surgery who were from URM groups decreased between 2002 and 2016, although there was greater representation of people from URM groups among medical school graduates [4, 24]. There are clear gender and ethnic disparities in orthopaedic surgery, but no effective solution has been found [7, 24, 25]. Previous analyses evaluating orthopaedic surgery in terms of representation of women and people from URM groups have lacked comparative data with other surgical specialties and are not up to date. More detailed information that identifies which specialties have seen faster rates of growth in the number of women and people from URM groups may help guide solutions to this complex problem in orthopaedic surgery.
We therefore asked: (1) Which surgical specialties have the greatest representation of women residents and residents from URM groups? (2) How have the proportions of women residents and residents from URM groups changed across the surgical specialties during the past decade?
Materials and Methods
Study Design and Setting
This was a retrospective survey of a large, longitudinally maintained database retrieved from the Accreditation Council for Graduate Medical Education Data Resource Books for the 2011 to 2012 to 2019 to 2020 academic years [2]. The Accreditation Council for Graduate Medical Education database is updated annually as a requirement for institutions to maintain their accreditation status. We believe this database is ultimately the most comprehensive and up-to-date database available for gender and ethnicity data for residents in all surgical specialties.
Participants
All surgical residents attending an Accreditation Council for Graduate Medical Education–accredited institution were included in this study. Resident demographic information by gender and ethnicity was retrieved. Data were obtained for seven different surgical specialties: orthopaedics, neurosurgery, ophthalmology, otolaryngology, plastic surgery, general surgery, and urology. Residents from plastic surgery and plastic surgery–integrated programs were combined into one specialty for analysis.
Definitions and Observations
Gender was categorized dichotomously as either men or women. Ethnicity was classified into the following categories according to the Accreditation Council for Graduate Medical Education [2]: white, non-Hispanic; Asian or Pacific Islander; Hispanic; Black, non-Hispanic; Native American or Alaskan; other; and unknown. Residents who were from URM groups included those who were Hispanic, Black, or Native American or Alaskan. From 2011 to 2019, Asian and Pacific Islander residents were grouped together. During the 2019 to 2020 academic year, however, Asian and Pacific Islander residents were no longer combined into one ethnic group. Instead, a new ethnic group, Native Hawaiian or Pacific Islander, was created, which was also considered a URM in our study. Nonetheless, the number of residents in the Native Hawaiian or Pacific Islander group was very small and did not affect our analysis. Lastly, some ethnic data were categorized as “other” or “unknown” and were not included in our analysis. These represented a small proportion of the overall dataset.
Primary and Secondary Study Outcomes
The primary goal of our study was to assess which surgical specialties had the greatest representation of women residents and residents from URM groups during the study period. To achieve this, we determined the proportions of residents who were women or from URM groups in each surgical specialty.
Second, we aimed to assess how the proportions of women residents and residents from URM groups have changed during the past decade. To achieve this, we calculated the rates of change for residents who were women or from URM groups in each surgical specialty.
Ethical Approval
Per the policy of our institution, institutional review board approval is not required for data that are publicly available and deidentified. Thus, ethical approval for this study was not sought.
Statistical Analysis
Accreditation Council for Graduate Medical Education data contain the information of all surgical residents. Therefore, since no sampling was necessary, no direct statisical comparison was made between the two groups. The differences reported therefore represent the absolute differences between the groups for the periods we studied. Descriptive statistical analyses were performed using IBM SPSS Statistics for Windows, version 26 (IBM Corp.). Linear regression analyses were performed to estimate the annual growth rates of women residents and residents from URM groups in each specialty.
Results
Which Surgical Specialties Have the Greatest Representation of Women and People from URM Groups?
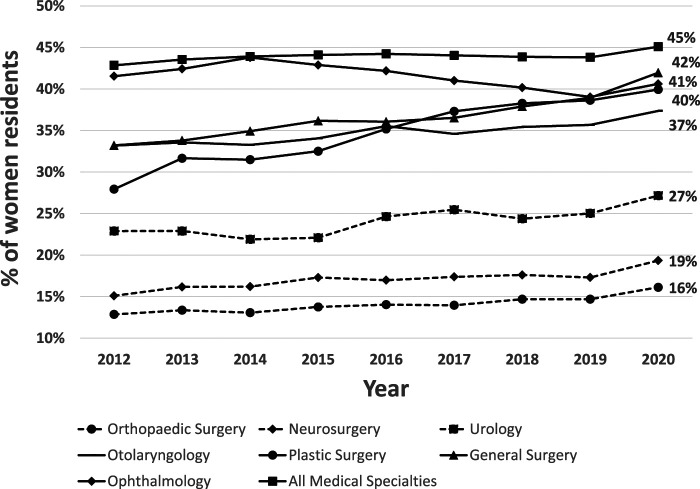
Orthopaedic surgery had the lowest mean representation of women residents over the 9-year study period (Fig. 1). Among the seven surgical specialties analyzed in this study, representation of women residents increased from 28% (4640 of 16,854 residents) to 33% (6879 of 20,788). In 2020, the representation of women residents in orthopaedic surgery was 16% (700 of 4342) (Fig. 2). Orthopaedic surgery only had a 3.3% increase in the representation of women residents from 2012 to 2020 (Fig. 2). In 2020, general surgery had the largest representation of women residents at 42% (3696 of 8809 residents), which was 8.7% higher than in 2012 (Fig. 2). Over the 9-year study period, representation of women residents among all medical specialties increased from 43% (49,403 of 115,293) to 45% (65,382 of 144,988) (Fig. 2). Plastic surgery had an increase of 12% in the representation of women residents during the study period (Fig. 2).
Fig. 1.
This graph shows the mean percentage of women residents by specialty from 2011 to 2020.
Fig. 2.
This graph shows the yearly growth rates from 2011 to 2020 for women residents across all surgical specialties.
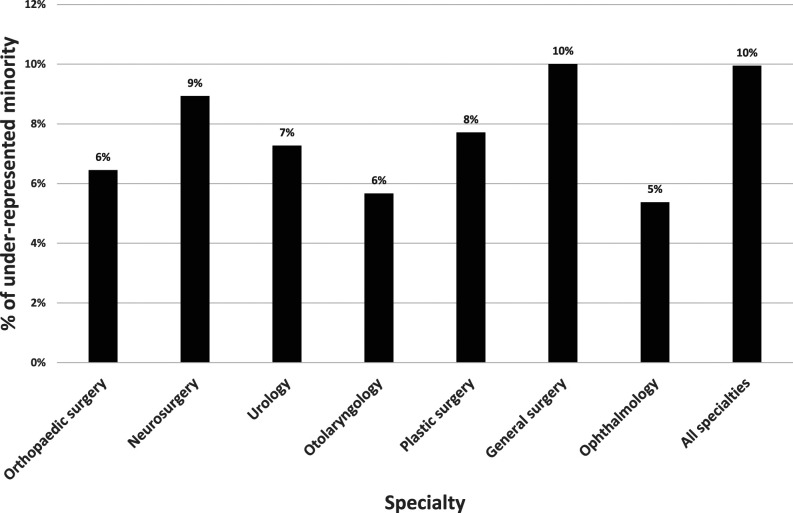
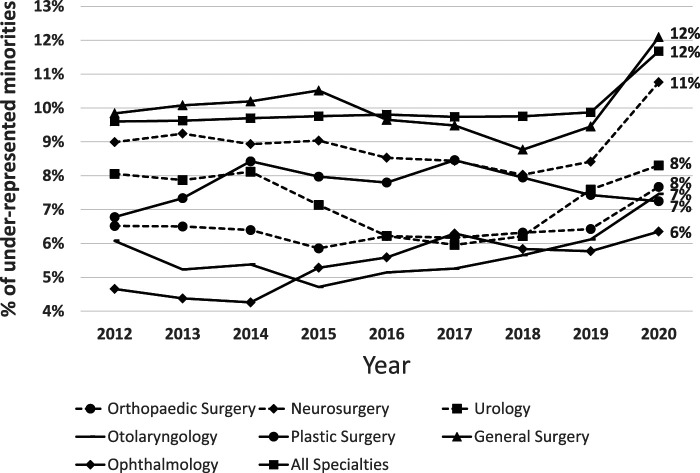
Orthopaedic surgery ranked fifth of the seven surgical specialties examined in the mean representation of residents from URM groups during the 9-year study period (Fig. 3). During this period, representation of residents from URM groups among all medical specialties increased from 9.6% (11,069 of 115,293) to 12% (16,926 of 144,988) (Fig. 4). Among the seven surgical specialties, representation of residents from URM groups increased from 8.1% (1362 of 16,854 residents) to 9.7% (2013 of 20,788). In 2020, the representation of residents from URM groups in orthopaedic surgery was 7.7% (333 of 4342) (Fig. 4). Orthopaedic surgery only had a 1.2% increase in the representation of residents from URM groups from 2012 to 2020 (Fig. 4). In 2020, general surgery had the largest representation of residents from URM groups (12%; 1065 of 8809 residents), which was 2.3% higher than in 2012 (Fig. 4).
Fig. 3.
This graph shows the mean percentage of under-represented minority residents by specialty from 2011 to 2020.
Fig. 4.
This graph shows the yearly growth rates from 2011 to 2020 for under-represented minority residents across all surgical specialties.
How Have the Proportions of Women and People from URM Groups Changed Across the Surgical Specialties During the Past Decade?
During the study period, among all medical specialties, the annual growth rate for women residents was 0.16%, and 0.15% for residents from URM groups. Among the seven surgical specialties combined, the annual growth rate for women residents was 0.60%, and 0.07% for residents from URM groups. Plastic surgery (1.46% per year) and general surgery (0.95% per year) had larger annual growth rates of women residents than the other specialties did. In each surgical specialty, the annual growth rate of residents from URM groups was insignificant (Table 1).
Table 1.
Annual growth rates for women residents and residents from URM groups
| Parameter | Women residents, % | Residents from URM groups, % |
| All medical specialties | 0.16 | 0.15 |
| All seven surgical specialties combined | 0.60 | 0.07 |
| Orthopaedic surgery | 0.34 | 0.08 |
| General surgery | 0.95 | 0.05 |
| Neurosurgery | 0.39 | 0.04 |
| Urology | 0.53 | -0.08 |
| Ophthalmology | -0.38 | 0.25 |
| Otolaryngology | 0.47 | 0.16 |
| Plastic surgery | 1.5 | 0.03 |
Discussion
The increase of women and people from URM groups entering medicine has not been observed in orthopaedic surgery. The need to improve gender and ethnic diversity in orthopaedic surgery is well supported by evidence showing improved patient care when there is physician-patient gender and ethnic concordance [9, 27, 30]. We found that the gender and ethnic makeup of orthopaedic surgery residencies has not changed substantially during the past decade and remains at or near the bottom in all categories examined. We found large differences among specialties, some of which have reduced disparities to a much larger degree than others. General surgery, through concrete actions that we will outline here, has increased its representation of women residents and residents from URM groups to be the highest among the surgical specialties.
Limitations
This study has several limitations. First, we did not have data in our study to longitudinally compare the applicant pool’s demographics and the demographics of applicants who have successfully matched. This would be of great utility in identifying whether the diversity gap is primarily driven by a bias in the application process. However, some research suggests that women match into orthopaedic surgery at higher rates than men do, suggesting that the better place to address the disparity may be during applicant recruiting rather than during the selection process [29]. Second, some ethnicity data were categorized as other or unknown, which were not included in our analysis. However, these represented a small proportion of the overall dataset and likely did not substantially affect our results. Finally, applicants were categorized as either men or women, and thus we were unable to collect information regarding residents who were nonbinary.
Representation and Change in the Proportion of Women in Surgical Specialties During the Past Decade
During the 9-year study period, orthopaedic surgery had the lowest representation of women residents, with little change over time. Consistent with our data, Acuña et al. [3] estimated that based on current rates of growth, gender parity between orthopaedic surgery and the overall medical profession (36% of practicing women orthopaedists) would not occur for 217 years. Examining the interventions that have helped general surgery to increase the representation of women may help shorten what has been a prolonged and as-yet incomplete course to parity for orthopaedic surgery. In fact, between 1994 and 2020, general surgery has more than doubled the proportion of women trainees, from 18.5% to 42% [1]. Performing a holistic review of applicants has been identified as a substantial contributor to closing the gender gap in general surgery [11, 22]. A holistic review focuses on selecting applicants with weight placed on experiences and personal attributes rather than academic metrics (United States Medical Licensing Examination scores, grades, and Alpha Omega Alpha honors society status) alone. Nehemiah et al. [22] implemented a holistic review of applicants that involved blinding selection committee members to United States Medical Licensing Examination scores, grades, and ethnicity, which resulted in an increase in the proportion of women ranked at their program by 19% compared with their previous formula for selection. Historically, orthopaedics has required some of the highest United States Medical Licensing Examination scores in order for an applicant to be considered competitive [21]. De-emphasizing standardized testing, which may be biased toward certain demographics [8, 26], and considering a holistic review would help improve the substantial gender gap currently present.
Representation and Change in the Proportion of URM Groups in Surgical Specialties During the Past Decade
Orthopaedic surgery, similar to the other surgical specialties we studied, had low representation of residents from URM groups. There was little change in the proportion of residents from URM groups in any surgical specialty during the study period. Similar to its success with recruiting women through methods such as using a holistic review of applicants and less reliance on objective measures, general surgery had the highest representation of residents from URM groups [10, 12, 22]. Outside surgery, a holistic review of applicants from URM groups in pediatrics has garnered a large increase in representation in a short time period [18]. Therefore, to ensure similar success in achieving parity among women and people from URM groups in orthopaedic surgery, we believe similar changes are needed at the residency recruitment level. We recommend these four steps, which have worked for other specialties, in order to increase recruitment and retainment of women and people from URM groups in orthopaedic surgery (Table 2):
Revise scoring rubrics to reduce reliance on objective measures (grades, United States Medical Licensing Examination Step 1 and 2 scores, and Alpha Omega Alpha membership) and discrete score cutoffs because these reinforce structural inequities that benefit those who are primarily white or come from more affluent backgrounds [8, 10, 12, 14].
Have residency program directors create explicit goals for recruitment such as “1/3 of recruitment members to be women or be from URM groups in 5 years, with success being 50/50 in 10 years,” because group leaders are the most important source of normative change [13]. A similar concept has been applied to the National Football League under the “Rooney Rule,” which requires league teams to interview ethnic minority candidates for head coaching positions. In the first 4 years since its implementation in 2002, the National Football League saw the number of Black coaches increase from 6% to 22% [17].
Institute mandatory unconscious bias training for those involved in resident recruitment as outlined by the Association of American Medical Colleges, because most faculty members are white men and this group (white faculty men) were found to display substantial levels of implicit white preference at the medical school admissions level [6].
Implement a longitudinal mentorship program for women and URM medical students that provides early exposure to orthopaedics, specialty immersion, and ongoing mentorship, as demonstrated in the Nth Dimension Pipeline Initiative Curriculum. This final recommendation primarily targets fostering interest in orthopaedics rather than improving the application selection process. Although the design of this study, by definition, included some selection bias (it was limited to medical students who chose to participate), Mason et al. [20] found that people from URM groups and women who participated in the Nth Dimension were 15 and 51 times more likely, respectively, to apply to orthopaedic surgery than the national average. The Nth Dimension has proven to be effective in recruiting people from URM groups and women to other surgical specialties as well [19]. However, these programs can require substantial time and funding, and they might be underused. We believe that future research identifying the highest yield components of these programs, in term of cost-effectiveness, would be of great importance for our specialty. These mentorship programs often place a disproportionate burden on faculty from URM groups by asking them to play leadership roles [23]. Faculty belonging to majority groups should be tasked with leading at least some of these initiatives to remove the burden from a group that is already burdened [15].
Table 2.
Summary of actionable items to decrease the gender and diversity gap in orthopaedic surgery
| Level of change | Immediate actionable items |
| Medical student interest | 1. Longitudinal mentorship program implementation. Have greater involvement of orthopaedic faculty who belong in the majority group (white men) in longitudinal mentorship programs such as Nth Dimensions and the Perry Initiative so that the burden does not fall solely on faculty from URM groups 2. Required orthopaedic surgery rotation during core third year clerkships. Implement mandatory musculoskeletal clerkships, which were found to create a relative 81% increase in women and 101% increase in people from URM groups into orthopaedic surgery [16] |
| Department optics/faculty representation | 1. Publicize diversity and inclusion efforts on residency program websites. Include visions of diversity and inclusion on residency program websites, because this has a correlation with an increase in the proportion of women residents [28] 2. Explicit goals and visions. Encourage residency program directors to direct normative change through creating public and explicit diversity and inclusion goals 3. Rooney Rule. Adopt the Rooney Rule from the National Football League, in which residency programs must interview at least one minority or woman candidate when choosing a new faculty member [17] |
| Application review process | 1. Holistic review. Create a holistic review process with new scoring rubrics that de-emphasizes the importance of discrete United States Medical Licensing Examination Step 1 and 2 cutoffs and Alpha Omega Alpha status during the residency application review process, and places greater weight on experiences and personal attributes 2. Implicit bias training. Require unconscious bias training in order to decrease the significant levels of implicit white preference in application review processes [6] |
Conclusion
During the past decade, orthopaedic surgery had the lowest representation of women residents compared with six other surgical specialties. In addition, the representation of residents from URM groups in orthopaedic surgery did not change from 2012 to 2020. The annual growth rate of women residents in each surgical specialty was small, while the annual growth rate of residents from URM groups did not change. By 2020, general surgery had become the most diverse surgical specialty. General surgery provides an example of how it is possible to substantially improve the representation of women, primarily through a holistic review of resident applications. Orthopaedic surgery would benefit from implementing a more holistic review of resident applications, with less emphasis on academic achievement and United States Medical Licensing Examination screening thresholds, which can be ethnically biased. More time and financial investment in longitudinal mentorship programs aimed to recruit students who are women or from URM groups into orthopaedics should be implemented. Further research is needed to identify which components of holistic review and longitudinal mentorship provide the most effective (and cost effective) increases in women and people from URM groups entering orthopaedic surgery.
Footnotes
Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval for this study was not sought.
Contributor Information
Benjamin W. Van, Email: bwvan@ucdavis.edu.
Joseph B. Wick, Email: jbwick@ucdavis.edu.
Hai V. Le, Email: haile@ucdavis.edu.
References
- 1.Abelson JS, Chartrand G, Moo TA, Moore M, Yeo H. The climb to break the glass ceiling in surgery: trends in women progressing from medical school to surgical training and academic leadership from 1994 to 2015. Am J Surg. 2016;212:566-572.e1. [DOI] [PubMed] [Google Scholar]
- 2.Accreditation Council for Graduate Medical Education. Data resource book archives. Available at: https://www.acgme.org/About-Us/Publications-and-Resources/Graduate-Medical-Education-Data-Resource-Book. Accessed April 1, 2021.
- 3.Acuña AJ, Sato EH, Jella TK, et al. How long will it take to reach gender parity in orthopaedic surgery in the United States? An analysis of the National Provider Identifier Registry. Clin Orthop Relat Res. 2021;479:1179-1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adelani MA, Harrington MA, Montgomery CO. The distribution of underrepresented minorities in U.S. orthopaedic surgery residency programs. J Bone Joint Surg Am. 2019;101:e96. [DOI] [PubMed] [Google Scholar]
- 5.American Association of Medical Colleges. 2020. facts: applicants and matriculants data. 2020. Available at: https://www.aamc.org/data-reports/students-residents/interactive-data/2020-facts-applicants-and-matriculants-data. Accessed April 1, 2021.
- 6.Capers Q, 4th, Clinchot D, McDougle L, Greenwald AG. Implicit racial bias in medical school admissions. Acad Med. 2017;92:365-369. [DOI] [PubMed] [Google Scholar]
- 7.Chambers CC, Ihnow SB, Monroe EJ, Suleiman LI. Women in orthopaedic surgery: population trends in trainees and practicing surgeons. J Bone Joint Surg Am. 2018;100:e116. [DOI] [PubMed] [Google Scholar]
- 8.Edmond MB, Deschenes JL, Eckler M, Wenzel RP. Racial bias in using USMLE Step 1 scores to grant internal medicine residency interviews. Acad Med. 2001;76:1253-1256. [DOI] [PubMed] [Google Scholar]
- 9.Fink M, Klein K, Sayers K, et al. Objective data reveals gender preferences for patients' primary care physician. J Prim Care Community Health. 2020;11:2150132720967221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gardner AK, Cavanaugh KJ, Willis RE, Dunkin BJ. Can better selection tools help us achieve our diversity goals in postgraduate medical education? Comparing use of USMLE Step 1 scores and situational judgment tests at 7 surgical residencies. Acad Med. 2020;95:751-757. [DOI] [PubMed] [Google Scholar]
- 11.Hemal K, Reghunathan M, Newsom M, Davis G, Gosman A. Diversity and inclusion: a review of effective initiatives in surgery. J Surg Educ. 2021;S1931-7204(21)00063-5. [DOI] [PubMed] [Google Scholar]
- 12.Jarman BT, Kallies KJ, Joshi ART, et al. Underrepresented minorities are underrepresented among general surgery applicants selected to interview. J Surg Educ. 2019;76:e15-e23. [DOI] [PubMed] [Google Scholar]
- 13.Kang SK, Kaplan S. Working toward gender diversity and inclusion in medicine: myths and solutions. Lancet. 2019;393:579-586. [DOI] [PubMed] [Google Scholar]
- 14.Kassam AF, Cortez AR, Winer LK, et al. Swipe right for surgical residency: exploring the unconscious bias in resident selection. Surgery. 2020;168:724-729. [DOI] [PubMed] [Google Scholar]
- 15.Leopold SS. Editorial: Fears about #MeToo are no excuse to deny mentorship to women in orthopaedic surgery. Clin Orthop Relat Res. 2019;477:473-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.London DA, Calfee RP, Boyer MI. Impact of a musculoskeletal clerkship on orthopedic surgery applicant diversity. Am J Orthop (Belle Mead NJ). 2016;45:E347-E351. [PubMed] [Google Scholar]
- 17.Madden JF, Ruther M. Has the NFL's Rooney Rule efforts "leveled the field" for African American head coach candidates? J Sports Econom. 2010;12:127-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marbin J, Rosenbluth G, Brim R, Cruz E, Martinez A, McNamara M. Improving diversity in pediatric residency selection: using an equity framework to implement holistic review. J Grad Med Educ. 2021;13:195-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mason BS, Ross W, Chambers MC, Grant R, Parks M. Pipeline program recruits and retains women and underrepresented minorities in procedure based specialties: a brief report. Am J Surg. 2017;213:662-665. [DOI] [PubMed] [Google Scholar]
- 20.Mason BS, Ross W, Ortega G, Chambers MC, Parks ML. Can a strategic pipeline initiative increase the number of women and underrepresented minorities in orthopaedic surgery? Clin Orthop Relat Res. 2016;474:1979-1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Residency Match Program. NRMP report archives. Available at: https://www.nrmp.org/report-archives/. Accessed April 1, 2021.
- 22.Nehemiah A, Roberts SE, Song Y, et al. Looking beyond the numbers: increasing diversity and inclusion through holistic review in general surgery recruitment. J Surg Educ. 2021;78:763-769. [DOI] [PubMed] [Google Scholar]
- 23.Pololi L, Cooper LA, Carr P. Race, disadvantage and faculty experiences in academic medicine. J Gen Intern Med. 2010;25:1363-1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Poon S, Kiridly D, Mutawakkil M, et al. Current trends in sex, race, and ethnic diversity in orthopaedic surgery residency. J Am Acad Orthop Surg. 2019;27:e725-e733. [DOI] [PubMed] [Google Scholar]
- 25.Rohde RS, Wolf JM, Adams JE. Where are the women in orthopaedic surgery? Clin Orthop Relat Res. 2016;474:1950-1956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rubright JD, Jodoin M, Barone MA. Examining demographics, prior academic performance, and United States Medical Licensing Examination scores. Acad Med. 2019;94:364-370. [DOI] [PubMed] [Google Scholar]
- 27.Shah RF, Mertz K, Gil JA, et al. The importance of concordance between patients and their subspecialists. Orthopedics. 2020;43:315-319. [DOI] [PubMed] [Google Scholar]
- 28.Smith JB, Chiu AG, Sykes KJ, Eck LP, Hierl AN, Villwock JA. Diversity in academic otolaryngology: an update and recommendations for moving from words to action. Ear Nose Throat J. Published online May 18, 2020. doi: 10.1177/0145561320922633. [DOI] [PubMed] [Google Scholar]
- 29.Sutherland M, Sanchez C, Baroutjian A, Ali A, McKenney M, Elkbuli A. Gender, race, age, allopathic degree, board score, and research experience among applicants matching to general and orthopedic surgery residencies, 2015-2019. Am Surg. Published online February 8, 2021. doi: 10.1177/0003134821991982. [DOI] [PubMed] [Google Scholar]
- 30.Takeshita J, Wang S, Loren AW, et al. Association of racial/ethnic and gender concordance between patients and physicians with patient experience ratings. JAMA Netw Open. 2020;3:e2024583. [DOI] [PMC free article] [PubMed] [Google Scholar]