Abstract
Background: Trans, gender diverse and non-binary (TGDNB) adults experience significant health disparities relative to their cisgender peers. While social support is a known health-protective factor within the general population, no systematic reviews of TGDNB experiences of social support exist.
Aim: To systematically review prior research of social support for TGDNB adults. We sought to assess the defining characteristics of the research, the participants and the research findings, mapping emerging trends across disciplines.
Methods: Six electronic databases (PubMed, MEDLINE, CINAHL, Web of Science, LGBT Life and PsycNet) were searched for literature pertaining to TGDNB adults, social support, and health or well-being published in the past decade.
Results: The findings illustrate a predominance of USA-based quantitative research that measures social support of friends, family and a singular intimate partner. The majority of participants were white, binary-identified transgender women and TGDNB people living in metropolitan settings. Social support was commonly reported as a protective factor, with TGDNB peer support the most frequently reported correlate of health and well-being for TGDNB adults.
Discussion: The results suggest standardized inventories do not capture the emic nature of social support for TGDNB adults. A key opportunity lies in an inductive, hypothesis-forming approach to the study of what is socially supportive for TGDNB adults. In turn, this knowledge will enable the appropriate measurement, implementation and interpretation of social support studies.
Keywords: Gender diverse, health, social support, transgender, well-being, systematic review
Introduction
In this study, we seek to counter the weight of studies that have focused on the deleterious social and physical effects of cissexism on gender diverse adults, by assessing the nature of research that has examined social support as a potential health protective factor. We examine studies of adults who defy or de-dichotomize the normative view of gender, who we refer to as trans, gender diverse and non-binary (TGDNB).
There is an increasing body of literature documenting the physical and mental health inequities of TGDNB adults(Brown & Peerapatanapokin, 2019; Hyde et al., 2014; Winter et al., 2016), including suicide attempts and ideation (Adams et al., 2017; Boza & Nicholson Perry, 2014). However, rather than view these outcomes as an inherent feature of TGDNB pathology, we conceptualize TGDNB health inequity as socially produced – and thus equally socially mitigated. Social support is one mechanism through which such outcomes may be mediated.
Social support is a multidimensional concept for which there is no agreed upon definition (Williams et al., 2004). As with previous scholars we conceptualize social support as relating to both the structure of an individual’s social life (e.g., kinship ties and friendship networks) and the support perceived to be available or actually provided from these social (non-professional) relationships (Cohen, 2000; Mclaren & Challis, 2009; Uchino, 2006). In this manner, we are interested in experiences at the individual rather than dyadic level (Gamarel et al., 2014) and how these experiences impact health and well-being.
Evidence for the utility of social support is well documented among cisgender men and women. Greater integration within social networks and perceived availability of social others is associated with better adjustment to – and recovery from – chronic disease in cross-sectional studies (Birkeland et al., 2017; Koch-Gallenkamp et al., 2016; Thomas et al., 2016). This buffering effect is similarly observed in the prospective studies, with social support associated with enhanced well-being, longevity and reduced all-cause mortality in the general population (Drageset et al., 2016; Holt-Lunstad et al., 2010; Tan & Wang, 2019).
For TGDNB people, sources of social support may exist outside of cisnormative models that typically locate social support as existing within the tripartite relations of family/friend/significant other (Frost et al., 2016). Indeed, TGDNB participants in cross-sectional studies consistently report ruptures in traditional networks of care, most notably one’s family of origin (Grant et al., 2011; Rotondi et al., 2011; Strauss et al., 2017). This was first observed by Factor and Rothblum (2007) in a systematic comparison of perceived family support among TGDNB adults and their cisgender siblings. Recent studies have sought to explore the meaning of alternate sites of social support for TGDNB adults (Hwahng et al., 2019; Sherman et al., 2020). TGDNB community connectedness, whether achieved in vivo (Hwahng et al., 2019) or online (Dowers et al., 2020), is increasingly recognized as an invaluable source of emotional, informational and instrumental support for TGDNB adults within Western settings.
Yet, within the TGDNB community, socially encoded patterns of difference delimit who may benefit from social support coping processes. Specifically, race/ethnicity and whether one holds a binary or non-binary identity are important determinants of TGDNB community engagement and subjective sense of belonging (Dowers et al., 2020; Kerry, 2014). Moreover, age-based norms of acceptance of TGDNB identities shape one’s willingness to disclose a TGDNB identity and subsequent access to TGDNB community (Gardner et al., 2014). Recent research suggests that the cultivation of social networks for TGDNB people is further complicated by place-based norms. In her analysis of trans men’s experiences across metropolitan and rural America, Abelson (2019) illuminated how social support is enabled through the ability to enact white, working-class heterosexuality for rural-dwelling trans men. These findings suggest that TGDNB social support experiences are shaped by personal, social and environmental factors.
Taken together, examining the contribution of social support to TGDNB health and well-being may be more complex than applying cisnormative models or measures and aggregating data from diverse TGDNB samples. However, at present there is no overview of how social support as a determinant of health and well-being has been studied within TGDNB samples, which constitutes these samples, and how the resultant findings may relate to each other. There is currently no clear path for reducing the socially mediated health inequities faced by TGDNB adults through interventions to enhance social support.
Therefore, this review investigates how social support has been studied in prior research with TGDNB adults. The research questions directing this review are as follows: (i) What are the defining characteristics of the research? (ii) what are the defining characteristics of the participants? and (iii) what are the key research findings? In completing this review, this article will consolidate what is known about social support as a determinant of TGDNB health and well-being and identify issues requiring future investigation.
Method
Systematic quantitative literature review
A systematic quantitative literature review (SQLR) was performed using the method of Pickering and Byrne (2014). The aim of SQLR, embedded in a positivist paradigm, is to produce a structured, quantitative summary of extant literature (Pickering & Byrne, 2014; Yang et al., 2017). This is achieved by charting and enumerating the number, proportion and type of papers dedicated to a specific research question. In doing so, researchers can assess which different combinations of, for example, locations, methods and participants have been examined by researchers and what has been observed. A key advantage of this method is that it is suitable for synthesizing a heterogeneous collection of research (Pickering & Byrne, 2014). Interest in TGDNB health and well-being spans a broad range of disciplines preferencing both qualitative and quantitative methods; hence, SQLR was deemed an appropriate method for mapping extant research.
Procedure
Six academic databases were identified from recently published TGDNB systematic reviews and included PubMed, MEDLINE, CINAHL, Web of Science, LGBT Life and PsycNet. Systematic searches were conducted from July 2019 until September 2019 using blocks of search strings that referred to the various study characteristics of social support, TGDNB and health and well-being (Table 1). Search terms within the blocks were combined using the Boolean phrase “or,” while the three blocks were combined using the Boolean phrase “and.”
Table 1.
Search terms.
| Search block | Terms |
|---|---|
| Social support | ‘social support’ OR ‘social network*’ OR ‘social integration’ OR ‘family’ OR ‘friends*’ OR ‘peers’ or ‘relationship*’ OR ‘community networks’ OR ‘community connect* |
| TGDNB | ‘transgender’ OR ‘transsexual*’ OR ‘gender minority’ OR ‘non-binary gender’ or ‘FTM’ OR ‘MTF’ OR ‘genderqueer’ |
| Health and well-being | ‘health’ OR ‘wellbeing’ OR ‘well-being’ OR ‘mental health’ OR ‘depression’ OR ‘anxiety’ OR ‘suicide’ |
Contemporary digital media environments have changed the way TGDNB adults seek and obtain social support (Sherman et al., 2020) and the way researchers access TGDNB samples (Miner et al., 2012). As such, a decision was made to focus our review on research from the past decade only, to ensure the findings reflected current typologies and methodologies used to study social support among TGDNB people. Therefore, inclusion criteria consisted of the following: (i) English-language, peer-reviewed articles with data collection and publication occurring between January 2009 and September 2019; (ii) studies of TGDNB adults (aged 18–65 years) and (iii) studies reporting quantitative or qualitative findings linking social support with a health or well-being outcome.
Studies where more than 5% of participants fell outside the included participant age range, and studies where participants were an additive subset of an LGBTQIA + cohort study or a study of sexual minorities, were excluded. While a body of literature considers the nature and quality of relationships between TGDNB people and their health care providers, this literature was excluded as the focus was on social, rather than therapeutic, relationships. As risk and protective factors of HIV have been the focus of previous systematic reviews of TGDNB adults (Brown & Peerapatanapokin, 2019; Herbst et al., 2008), studies that considered HIV as the principle outcome were excluded. Review articles and psychometric measurement analyses were also excluded.
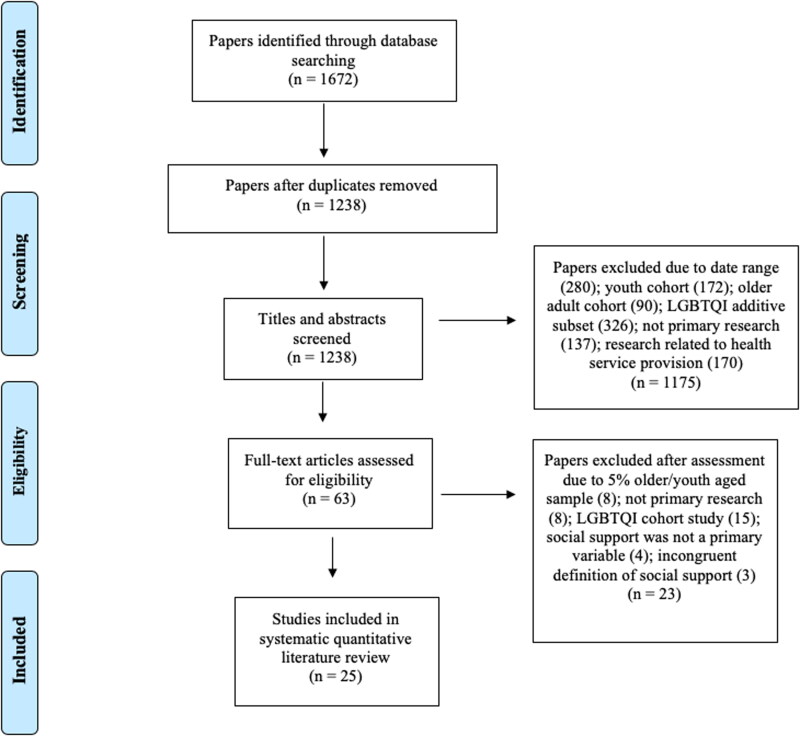
The PRISMA flowchart (Figure 1) outlines the number of studies screened and excluded at different stages of the review with reasons provided. The literature search resulted in 1672 records, which were exported to Endnote X9.2 for data management. After removing 434 duplicate references, the titles, abstracts and keywords of the remaining 1238 records were screened by the first author. Only articles that contained social support-related search terms in either the title, abstract or keywords were considered. The screening process yielded 63 records, of which full texts were retrieved and reviewed by the first author for eligibility in the final analysis. Twenty-three articles were identified as eligible, with the reference lists of these studies crosschecked to identify additional papers, resulting in two further inclusions, for a total of 25 studies.
Figure 1.
PRISMA flow diagram depicting search strategy and outcome.
(Adapted from Moher, Liberati, Tetzlaff & Altman, 2009).
Data extraction and synthesis
A personal database was created in Microsoft Excel where the bibliographic details of the 25 studies were populated. From each paper, the first author recorded the following information: author(s)/year, academic discipline, study location, aim, methods (qualitative/quantitative, reflexivity, reimbursement), sample size, participant details (gender identity, race/ethnicity, rural/metropolitan living status), social support variable(s), health and well-being outcome variables and findings relating social support to health and well-being.
For the purpose of data synthesis, articles were categorized as principally related to TGDNB health or well-being. This assessment was made based on a close reading of the aim(s), inventories and findings of each study. Health-related articles were those that examined pre-defined structural, functional or emotional states of being that shape TGDNB adults’ ability to function as both individuals and members of society (McCartney et al., 2019). For example, studies employing outcome measures of mental health morbidity were categorized as pertaining to health. Conversely, articles were categorized as relating to well-being when the emphasis of study was on the subjective, situated and socially constructed experience of being in the world (Germov, 2014). Studies of resilience were included within the well-being category.
Three studies were input and cross-checked by all authors to test how well the categories and subcategories of the database enabled the research team to answer the review questions. Categories were considered sufficient and, as such, details for the remaining articles input by the first author and cross-checked by the fourth. A summary table of data was produced (Table 2). As with previous application of the SQLR method (Guitart et al., 2012; Pickering & Byrne, 2014), studies were not appraised or ranked according to quality or relevance, as peer-reviewed article quality was assumed given that each was deemed suitable for publication within a given discipline.
Table 2.
Descriptions of included studies (N = 25).
| Author (year) | Location | Study design | Sample – size; mean age; gender (verbatim); race | Aim | Social support (measure used) | Outcome category (related measures) | Findings related to social support |
|---|---|---|---|---|---|---|---|
| Koken et al. (2009) | New York (USA) | Qualitative (SSI) | 20; 32 years; 60% TW, 40% female; 100% POC | Explore experiences with caregivers | Parent/primary caregiver experience post TW identity disclosure | Well-being | Majority experience hostility, aggression and neglect |
| Erich et al. (2010) | USA | Quantitative (PS) | 108; 41years; 80% MTF, 20% FTM, 58% white | Examine racial differences in social support | Satisfaction of support across multiple sources | Well-being (SWLS, ISE) | Main effect for total social support: positive correlation with SWLS and ISE |
| Singh et al. (2011) | USA | Qualitative (SSI, FG) | 20; 34 years; 55% MTF; 40% TM; 5% XX male; 71% POC | Explore strategies of resilience | Participant-derived experiences of resilience | Well-being | Connection to supportive communities is a source of resilience |
| Bethea and Mccollum (2013) | USA | Qualitative (SSI) | 7; age not reported; 100% MTF; 100% white | Explore social experiences | Social experiences post TW identity disclosure | Well-being | Social support and comfort through TW peer support groups |
| Boza and Nicholson Perry (2014) | Australia | Quantitative (OS) | 243; 38 years; 66% AMAB, 34% AFAB, 94% white | Examine correlations between social support and depression | MSPSS | Health (CES-D) | Main effect for total perceived support: negative correlation with depression |
| Davey et al. (2014) | Midlands (England) | Quantitative (PS) | 103; 36 years; 61% TW, 39% TM; 95% white | Examine correlations between social support and well-being | MSPSS | Well-being (SF, PWI, SCL) | Main effect for total perceived support: positive correlation with SF and PWI |
| Graham et al. (2014) | Detroit (USA) | Qualitative (UI) | 10; 21 years; 100% TW; 80% POC | Explore familial and peer social support | Social experiences post gender transition | Well-being | Fractious relationships with biological family, TW peer support enables identity affirmation and kinship |
| Budge et al. (2014) | USA | Quantitative (OS) | 64; 30 years; 100% GQ; 86% white | Examine correlations between social support, anxiety and depression | MSPSS | Health (CES-D, BA) | Main effect for total perceived support: negative correlation with CES-D and BA |
| Claes et al. (2015) | UK | Quantitative (PS) | 155; 34 years; 66.5% TW, 33.5% TM; no race data | Examine correlations between social support and non-suicidal self-injury (NSSI) | MSPSS | Health (SIQ) | Main effect for family: negative correlation with NSSI |
| Bauer et al. (2015) | Ontario (Canada) | Quantitative, (OS) | 380; 32 years; 53% FTM spectrum, 47% MTF spectrum; 77% white | Examine correlations between social support and suicidality | MOS | Health (suicidal ideation and attempts) | Main effect for total perceived support and support from parents: negative correlation with suicidality |
| Pflum et al. (2015) | North America (77% urban) | Quantitative (OS) | 865; 33 years; 51% TMS; 49% TFS; 90% white | Examine correlations between social support, depression and anxiety | BSSS, GMSR | Health (CES-D, GAD-7) | Main effect for BSSS and GMSR (TFS only): negative correlation with CES-D and GAD-7 |
| Yang et al. (2015) | Shenyang (China) | Quantitative (I-PS) | 209; 26 years; 100% TW; 100% POC | Examine correlations between social support and depression | MSPSS | Health (SDS) | Main effect for total perceived support: negative correlation with SDS |
| Barr et al. (2016) | USA (87% urban) | Quantitative (OS) | 571; 30 years; 38% male, 37% female, 25% NB; 80% white | Examine correlation between TGDNB belongingness and well-being | LCBS (adapted as TGDNB belongingness) | Well-being (RSES, SWLS, SPWB) | Mediating effect for TGDNB belongingness: strength of TGDNB identity and well-being (RSES, SWLS, SPWB) |
| Başar & Öz (2016) | Ankara (Turkey) | Quantitative (PS) | 116; 25 years; 75% TM, 25% TW; no race data | Examine correlations between social support and resilience | MSPSS | Well-being (RSA) | Main effect for total and friend-support: positive correlation with RSA |
| Başar et al. (2016) | Ankara (Turkey) | Quantitative (I-PS) | 94; 27 years; 77% TM, 23% TW; no race data | Examine correlations between social support and quality of life | MSPSS | Well-being (WHOQOL-24) | Main effect for friend: positive correlation on three WHOQOL domains; main effect for family: positive correlation on one domain |
| Klein and Golub (2016) | USA | Quantitative (OS) | 3458; 36 years; 61% AMAB; 39% AFAB; 36% reported NB identity; 77.5% white | Examine correlations between interpersonal rejection and suicidality | Level of reported interpersonal rejection | Health (suicidality and substance use) | Main risk for interpersonal rejection: positive correlation with suicidality and substance use |
| Davey et al. (2016) | UK | Quantitative (PS) | 97; 35 years; 62% TW; 37% TM; 88.7% white | Examine correlations between social support and NSSI | MSPSS | Health (SIQ-TR) | Main effect for total perceived support: negative association with current NSSI |
| Budge et al. (2017) | USA | Qualitative (SSI) | 15; 40 years; 40% MTF; 27% FTM; 27% GQ/ NB, 7% ‘MFTS’; 66% POC | Exploration of facilitative coping | Participant derived facilitative coping processes | Well-being | Attending peer support groups and helping TGDNB others enables facilitative coping |
| Scandurra et al. (2017) | Italy (87% urban) | Quantitative (OS) | 149; 33 years; 33; 51% FTM; 49% MTF; 98% white | Examine correlations between social support and mental health | MSPSS | Health (CES-D; BAI) | Main effect for family support: negative correlation with BAI and CES-D; moderating effect for family: everyday discrimination and both CES-D and BAI |
| Trujillo et al. (2017) | USA | Quantitative (OS) | 78; 29 years; 33% TM, 37% TW; 30% gender other than the two; 62% white | Examine correlations between social support and mental health | MSPSS | Health (HSCL-25; SBQ; HHRDS) | Main effect for significant other: negative association with depression; moderating effect for friends and significant other: discrimination and SBQ |
| Clark et al. (2018) | Los Angeles (USA) | Quantitative (AS) | 271; 35 years; 100% TW; 72% POC | Examine correlations between social networks and hormone use | Social network dynamics | Health (hormone misuse) | Correlation between no. of friends using hormones and hormone misuse, using the Internet to find friends mitigates risk |
| Fuller and Riggs (2018) | USA | Quantitative (OS) | 345; 27 years; 32% male, 25% NB, 25% female, 13% another gender, 5% agenda; 75% white | Examine correlations between social support and resilience | MSPSS, gender-related family support (study specific) | Wellbeing (BRS, K10) | Main effect for total perceived support: negative correlations with psychological distress; main effect for family: positive correlation with resilience; main effect for gender-related family support: BRS, K10; mediating effect for gender-related family support: discrimination and K10 |
| Carter et al. (2019) | USA | Quantitative (OS) | 298; 48 years; 87% TW; 13% TM; 90% white | Examine social support as a moderator between discrimination and suicide | MSPSS (modified) | Health (suicidal ideation) | Main effect for friends (general and TGDNB-specific): negative association with suicidal ideation (SI); moderating effect for TGDNB friends: discrimination and SI |
| Hwahng et al. (2019) | New York (USA) | Qualitative (SSI, FG) | 13; 38 years; 100% TW; 100% POC | Exploration of resilience | Experiences within TW peer support groups | Well-being | Social bonds formed in TGDNB support groups enable resilience and health-promoting behavior |
| McDowell et al. (2019) | Boston (USA) | Quantitative (I-PS) | 150; 27 years; trans masculine (76.7% had a binary gender identity); 75% white | Examine correlations between social support and mental health | MOS | Health (PC-PTSD, BSI) | No significant effect in overall model for PTSD, anxiety or depression |
Notes: Acronyms used in the table:
Study design: AS: audio survey, FG: focus group, I-PS: in-person survey, OS: online survey, PS: posted survey, SSI: semi-structured interviews, UI: unstructured interviews.
Sample: AFAB: assigned female at birth, AMAB: assigned male at birth, FTM: female-to-male, GQ: gender queer, MTF: male-to-female, NB: non-binary, POC: people of color, TFS: trans feminine spectrum, TM: transgender men, TMS: trans masculine spectrum, TW: transgender women.
Measures: BA: Burns Anxiety Inventory, BAI: Beck Anxiety Inventory, BDI: Beck Depression Inventory, BRS: Brief Resilience Scale, BSI: Brief Symptom Inventory, BSSS: Berlin Social Support Scales, CES-D: Center for Epidemiological Studies Depression Scale, ETS: Experiences of Transphobia Scale; GAD-7: Generalized Anxiety Disorder 7-item Scale, GMSR: Gender Minority and Resilience Measure (community connectedness subscale), HHRDS: Heterosexist Harassment, Rejection and Discrimination Scale, HSCL-25: Hopkins Symptoms Checklist 25, ISE: Index of Self-Esteem, K10: The Kessler 10, LCBS: Lesbian Community Belongingness Scale, MOS: Medical Outcomes Study, MSPSS: Multidimensional Scale of Perceived Social Support, PC-PTSD: Primary Care PTSD Scale, PWI: Personal Wellbeing Index, RSA: Resilience Scale for Adults, RSES: Rosenberg Self-Esteem Scale, SBQ: Suicidal Behaviors Questionnaire, SCL: Symptom Checklist 90 Revised, SDS: Zung Self-Rating Depression Scale, SIQ-TR: Self Injury Questionnaire- Treatment Related, SF: Short Form 36 version 2, STIS: Strength of Transgender Identity Scale, SWLS: Satisfaction with Life Scale, SPWB: Scale of Psychological Wellbeing, TCB: Transgender Community Belongingness Scale, WHOQOL-24: World Health Organization’s Quality of Life (24 items).
Results
Characteristics of the research
Date range, geographic location and disciplinary scope
Twenty-five original research articles examining the impact of social support on the health and/or well-being of TGDNB adults were identified from the previous decade (Table 2).
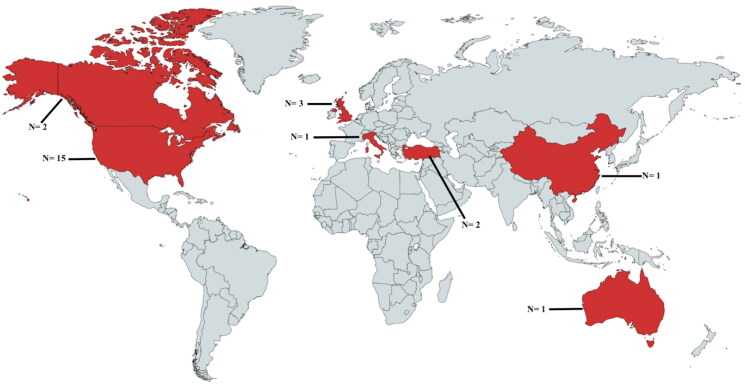
More than half of the identified articles (N = 13, 52%) were published between 2016 and 2019. Most studies took place in the USA (N = 15, 60%). Of the remaining 10 studies, three (12%) were conducted within the United Kingdom, two (8%) each within Canada and Turkey, with single studies in China, Australia and Italy (Figure 2).
Figure 2.
World map with locations of included studies (N = 25).
(Created with mapchart.net).
The studies were situated within a broad range of academic disciplines including medicine, science, public health and psychology. Studies were published in 21 different peer-reviewed journals, with multiple sources obtained from the International Journal of Transgenderism (N = 3, 12%), Journal of Sexual Medicine (N = 3, 12%), Journal of Counseling Psychology (N = 2, 8%) and LGBT Health (N = 2, 8%).
Study methods
All identified studies were cross sectional. Most studies (N = 19, 76%) sought to examine the relationship between researcher-derived measures of social support and participant self-rated health or well-being. Of the 19 studies that shared this objective, all employed quantitative, cross-sectional research methods. The primary method of data collection was online survey (N = 10, 53%), followed by posted survey (N = 5, 26%), in-person survey (N = 3, 16%) and administration by audio computer-assisted self-interview technology (N = 1, 5%). All remaining studies (N = 6, 24%) employed qualitative research methods. Of these, the most common form of data collection was a single semi-structured interview (N = 3, 50%), followed by a combined focus group/semi-structured interview method (N = 2, 33%). A single study employed an unstructured interview method. A majority of qualitative studies (N = 4, 67%) employed an inductive, rather than a deductive, approach to the study of social support. When an inductive method was employed, participants identified and explored sources of social support that were significant and meaningful to them.
Outcome measures were categorized as principally relating to health (N = 13, 52%) or well-being (N = 12, 48%). All qualitative studies were coded as the later. Self-reported health and well-being were assessed using a heterogeneous repertoire of standardized and study-specific scales with the highest degree of overlap recorded in use of the Center for Epidemiological Studies Depression Scale (CES-D) (N = 4, 16%). In the majority of studies (N = 21, 84%), social support was pre-defined by the research team and principally operationalized as perceived support (N = 20, 95%). Perceived support is a measure of the degree to which a person anticipates that the support they require will be available if needed. A single study (5%) assessed social support using social network analysis.
As with health and well-being outcome measures, multiple inventories were used to assess social support. The most common standardized instrument was the Multidimensional Scale of Perceived Social Support (MSPSS) employed in 48% of studies (N = 12). The MSPSS is a 36-item, self-report measure of the perceived quality of social support received from family, friends and a significant other from a subjective perspective. While the “friends” and “family” subscale are worded in the collective, the significant other subscale denotes a singular “special person” (Zimet et al., 1988). Or, put another way, the sub-scale assumes a monogamous relationship. Family, friend and support of a significant other were the most commonly studied sources of social support within the identified literature, which unsurprisingly granted the frequent use of the MSPSS.
Characteristics of participants
Gender
Approximately one quarter of samples included transgender women only (N = 6, 24%), compared to 4% of studies that focused exclusively on transgender men (N = 1) and genderqueer adults (N = 1). For the remaining studies, gender was reported as self-identification with a binary transgender identity (e.g., transgender men/transgender women) (N = 10, 40%), use of a tripartite classificatory system (e.g., transgender men, transgender women and other/non-binary) (N = 3, 12%), allocation along a male-to-female or female-to-male spectrum (N = 2, 8%) and the recording of participant’s self-described identity labels (N = 2, 8%). Notably, in those studies where a TGDNB spectrum was applied (Bauer et al., 2015; Pflum et al., 2015), gender-fluid and/or non-binary participants were categorized differently, suggesting the classifications were at odds.
Race
Twenty-two studies (88%) provided data on the racial/ethnic background of TGDNB participants. Of these, approximately two thirds (N = 17, 68%) involved majorly non-Hispanic, non-Indigenous, white participants. In contrast, less than one-fifth of studies (N = 5, 20%) involved the purposive sampling of TGDNB adults who self-identified as belonging to a racial/ethnicity minority group.
Study location and participant living environment
Geographical location data were reported for just over half of the included studies (N = 13, 52%). For these studies, either the name of the city/province (N = 10) or the proportion of urban and rural participants was provided (N = 3). Where location data were provided, studies typically occurred in large metropolitan settings such as San Francisco, New York City, Ontario, Ankara and Shenghan. Convergent with this metrocentric bias, when rurality data were reported, less than 12.8% of participants listed their place of residence as regional or rural.
Key research findings
Social support and TGDNB health
The frequency counts of the main and moderating effects of the 13 health-related articles are presented in Table 3. The main health-promoting effects were reported at a higher frequency than both moderating effects and risk factors. Perceived general social support was negatively correlated with depression (Boza & Nicholson Perry, 2014; Budge et al., 2014; Pflum et al., 2015; Yang et al., 2015), anxiety (Budge et al., 2014; Pflum et al., 2015), suicidality (Bauer et al., 2015) and non-suicidal self-injury (Davey et al., 2016). Conversely, interpersonal rejection (e.g., by parents, spouse and children) was associated with increased odds of suicide attempts and substance misuse (Klein & Golub, 2016). Regarding specific sources of support, health-promoting effects were commonly observed for family (including parent-specific support) and peer support.
Table 3.
Number and sources of articles reporting main and moderating health effects for social support.
| Operationalization of social support | Main health promoting effect | Moderating health promoting effect | Main health risk |
|---|---|---|---|
| General | 6 (Bauer et al., 2015; Boza & Nicholson Perry, 2014; Budge et al., 2014; Davey et al., 2016; Pflum et al., 2015; Yang et al., 2015) | 1 (Klein & Golub, 2016) | |
| Family | 2 (Claes et al., 2015; Scandurra et al., 2017) | 1 (Scandurra et al., 2017) | |
| Parent-specific | 1 (Bauer et al., 2015) | ||
| Significant other | 1 (Trujillo et al., 2017) | 1 (Trujillo et al., 2017) | |
| Friends | |||
| Non-specific | 1 (Carter et al., 2019) | 1 (Trujillo et al., 2017) | |
| TGDNB peer | 2 (Carter et al., 2019; Clark et al., 2018; Pflum et al., 2015) | 1 (Carter et al., 2019) |
Family and parental support was associated with significant health protective effects across four studies. The family sub-domain of the MSPSS was negatively correlated with non-suicidal self-injury (Claes et al., 2015), anxiety (Scandurra et al., 2017) and depression (Scandurra et al., 2017). Notably, in Claes et al.’s. (2015) study, transgender men reported significantly higher levels of social support from family than transgender women. An interaction effect was observed by Scandurra et al. (2017), with family support the only significant moderator between everyday discrimination and self-reported mental health, with transgender women reporting higher rates of discrimination than transgender men. Regarding specific familial relationships, parental support was inversely correlated with past-year suicidality in a single study (Bauer et al., 2015).
General friend and TGDNB peer support were further protective factors for TGDNB health. Trujillo et al. (2017) detailed an interaction effect for the MSPSS friend sub-domain. Accordingly, experiences of harassment and rejection were associated with suicidal ideation only when perceived social support from friends was low (Trujillo et al., 2017). In their adaptation of the MSPSS, Carter et al. (2019) introduced a TGDNB friend sub-domain, enabling comparison between general friend and TGDNB peer support. In the resulting analysis, only TGDNB peer support moderated the association between discrimination and suicidal ideation (Carter et al., 2019). Evidence for the specific utility of TGDNB peer support for mental health outcomes was similarly reported by Pflum et al. (2015). However, the negative relationship between trans community connectedness and symptoms of anxiety and depression was observed for trans feminine participants only. Finally, in an analysis of social networks, using the Internet to connect with TGDNB peers was associated with reduced risk of hormone misuse for transgender women (Clark et al., 2018). Here, a significance effect for age and race was observed: Being older and non-African-American/Black was a protective factor against hormone misuse.
Social support and well-being
In contrast to the exclusive use of quantitative research methods for health outcome studies, both qualitative (N = 6, 50%) and quantitative studies (N = 6, 50%) were categorized as relating to well-being. As such, well-being effects are recorded in Table 4 as either discussed within a paper, though not explicitly measured, or demonstrated statistically. General or overall perceived social support was positively correlated with well-being (Başar & Öz, 2016; Davey et al., 2014), satisfaction with life (Erich et al., 2010) and negatively correlated with psychological distress (Fuller & Riggs, 2018). In a phenomenological study, connection to a supportive community (e.g., spiritual, performance, racial or LGBT) was a significant source of resilience (Singh et al., 2011).
Table 4.
Number and sources of articles reporting main and moderating well-being effects for social support.
| Main well-being effect |
Mediating well-being effect |
Evidence of risk |
||||
|---|---|---|---|---|---|---|
| Operationalization of social support | Disc. | Dem. | Disc. | Dem. | Disc. | Dem |
| General | 1 (Singh et al., 2011) | 4 (Başar & Öz, 2016; Davey et al., 2014; Erich et al., 2010; Fuller & Riggs, 2018) | ||||
| Family | 2 (Başar et al., 2016; Fuller & Riggs, 2018) | 1 (Fuller & Riggs, 2018) | 1 (Graham et al., 2014) | |||
| Parent specific | 1 (Koken et al., 2009) | |||||
| Friends | ||||||
| Non-specific | 2 (Başar et al., 2016; Başar & Öz, 2016) | |||||
| TGDNB peer | 4 (Bethea & Mccollum, 2013; Budge et al., 2017; Graham et al., 2014; Hwahng et al., 2019) | 1 (Barr et al., 2016) | ||||
Disc., discussed in paper but not explicitly measured; Dem., demonstrated statistically in paper.
Four studies discussed or demonstrated the effects of family support (Başar et al., 2016; Fuller & Riggs, 2018; Graham et al., 2014; Koken et al., 2009). Fuller and Riggs (2018) observed a main effect for gender-related family support and the MSPSS family sub-domain. Both were correlated with resilience, with the study-specific measure of gender-related support negatively correlated with psychological distress. Notably, a significant effect for gender was observed, with non-binary participants reporting the lowest levels of gender-related family support. Social support from family was likewise associated with better psychological quality of life in the quantitative study by Başar et al. (2016). Conversely, Graham et al. (2014) and Koken et al. (2009) reported risk effects for connection to family. In Koken et al.’s (2009) study of transgender women’s experiences with their parents and primary caregivers, the majority discussed confronting hostility, aggression and neglect upon disclosing a transgender identity. This finding was similarly reported by Graham et al. (2014). Transgender women described family members as struggling with acceptance resulting in participants severing or severely limiting communication with – and instrumental reliance on – family.
Relative to the factious documented effects of family support, friend/peer support was a significant and meaningful source of well-being for TGDNB adults. Regarding generic friend support, higher perceived social support of friends was positively correlated with quality of life (Başar et al., 2016) and resilience (Başar & Öz, 2016). Notably, while Erich et al. (2010) did not report a main effect for support from friends in their overall analysis, TGDNB adults of color reported higher levels of perceived social support from friends compared to white participants.
Five studies documented the specific utility of TGDNB peer support as an important construct in well-being (Barr et al., 2016; Bethea & McCollum, 2013; Budge et al., 2017; Graham et al., 2014; Hwahng et al., 2019). Three of these studies (Bethea & McCollum, 2013; Budge et al., 2017; Graham et al., 2014) were not designed specifically to identify the influence of TGDNB peer support on well-being. Rather, TGDNB peer support was an inductively derived source of TGDNB adult resilience and facilitative coping across these studies, which predominately comprised transgender women participants. Deductive studies further attest to the importance of TGDNB peer support in promoting well-being. In a correlational study, transgender community belongingness mediated the positive relationship between strength of transgender identity and well-being (Barr et al., 2016). Hwahng et al. (2019) considered the meaning and significance of participating in a support group for transgender women of color. Participation was characterized by the development of alternate kinship structures that increase resilience and health-promoting behavior (Hwahng et al., 2019).
Discussion
The aim of this review was to illuminate the defining characteristics of TGDNB social support research, the participants and the findings as they relate to the health and well-being of TGDNB adults. This body of research is predominately conducted in North America and typically adheres to a positivist paradigm with cross-sectional survey designs commonly used. There is significant heterogeneity in the instruments used to assess health, well-being and TGDNB social support. The most frequently employed instrument was the MSPSS. Participants were typically binary-identified transgender women and people who self-identify as white. Moreover, a metrocentric bias of participants was observed, whereby most participants lived in major metropolitan and urban settings.
Although substantial heterogeneity exists in the design and outcomes of the included studies, some generalizations can be made. Overall, social support, typically operationalized as perceived social support, was a protective factor for health and well-being among TGDNB adults. The specific sources of support for which health and well-being effects were observed varied across studies. Social support of TGDNB peers and family (including parental support) was the most frequently reported health and well-being protective factor. However, critical intersections, most notably race/ethnicity and gender expression, shaped what was and what was not socially supportive to TGDNB adults.
The reported health and well-being effects for social support among TGDNB adults align with studies of the general population. A previous systematic review of 36 studies, which did not purposively sample for TGDNB adults, reported a protective function of social support for depression (Gariépy et al., 2016). More recently, Wang et al. (2018) replicated this finding in a systematic review of 34 prospective studies of perceived social support and outcomes of mental health problems, thereby enabling statements of inference. Lower levels of perceived social support at baseline resulted in poorer outcomes in terms of depressive symptoms, recovery and social functioning (Wang et al., 2018). However, upon closer examination, support from a spouse was the most consistently reported protective factor (Gariépy et al., 2016). This finding was not replicated in the current review of TGDNB social support experiences. Indeed, Carter et al. (2019) removed the “significant other” sub-domain from their application of the MSPSS, owing to the low number of TGDNB participants reporting having a spouse.
The finding that TGDNB adults do not obtain social support from the same sources as members of the general population raises questions regarding how social support is operationalized. While the MSPSS was used in almost half of the reviewed studies, the factorial structure of this inventory does not align with the meaning of social support prescribed by TGDNB adults. When TGDNB adults were asked to speak to their subjective experience of well-being, TGDNB peer support was the most frequently discussed determinant (Bethea & McCollum, 2013; Budge et al., 2017; Graham et al., 2014). However, the MSPSS “friend” sub-domain limits investigation into general friend and TGDNB peer specific effects. A similar critique extends to the “family” and “significant other” sub-domains. As both studies of this review (Graham et al., 2014; Hwahng et al., 2019) and research of partnership experiences suggest (Bauer et al., 2013; Scheim et al., 2019), the expectation of biological kinship and monogamy is not reflected in intimate affective and behavioral bonds that characterize TGDNB relationships.
It is not our intention to suggest the use of alternate inventories that, as with the MSPSS, are based on cisnormative operationalizations of social support. To address limitations in the current evidence base, we argue for an inductive hypothesis-forming approach to TGDNB social support research. The lack of a TGDNB-specific definition of social support presents a fundamental challenge to social support research. As an extension of this, there is no TGDNB standardized inventory for the assessment of perceived social support for TGDNB adults. Use of qualitative research methods, specifically phenomenology and grounded theory, would make it possible to develop a context-specific definition of what is social support from the perspectives of TGDNB adults. This can only be achieved by asking TGDNB adults what social support means to them (Creswell, 2018). Explicating the nature and process of social support, in turn, would allow for confident measurement, interpretation and synthesis of TGDNB social support literature.
While there is merit in identifying the core features and process of TGDNB social support, the current findings suggest that any attempt to define TGDNB social support must be sensitive to intra-group differences. In the current review, social support experiences were shaped by gender expression. Relative to transgender men, transgender women reported higher rates of discrimination (Scandurra et al., 2017) and lower levels of perceived family support (Claes et al., 2015). Qualitative findings of family rejection were also evident in studies comprising transgender women only (Graham et al., 2014; Koken et al., 2009). These findings are consistent with scholarship suggesting that transgender women are “policed” differently based on cultural presumptions about gender (Serano, 2009; Westbrook & Schilt, 2014). Data from this review suggest that delimited opportunity for social support may be one such manifestation of transmisogyny.
Race and place are additional intersections that must be acknowledged in the development of a TGDNB-specific understanding of social support. In the current review, differences in satisfaction of support were reported between TGDNB people of color and TGDNB people who identify as white (Erich et al., 2010). Specifically, TGDNB adults of color reported higher levels of satisfaction of support from friends and significant others. What this finding suggests is that race shapes experiences of social support for TGDNB adults. Abelson (2019) similarly observed this in her qualitative analysis of rural American masculinities. The ability of transgender men to integrate within rural communities was enabled through whiteness and an ability to enact rural working-class heterosexual masculinity (Abelson, 2019). In sum, a TGDNB-specific definition of social support must attend to the extra-local conditions that shape opportunity for – and experiences of – social support.
Future directions
With this complexity in mind, future TGDNB social support research must enable exploration of intersectionalities. Attending to how people understand their gender, as well as their race/ethnicity, and how this shapes situated and subjective experiences of social support is one avenue for future TGDNB research. For example, while transgender women were observed to benefit most from TGDNB–community connection (Pflum et al., 2015), it is unclear to what extent race/ethnicity shapes perception of – and experiences – with TGDNB peers. While this subject remains unexamined within adult TGDNB research, Singh (2013) conducted a USA-based phenomenological study of TGDNB youth of color. Validation of participants’ experiences of racism and affirmation of their “whole” self was uniquely enabled by racial/ethnic concordant TGDNB peers (Singh, 2013). This finding suggests the need to attend to the complexity of social support for people with diverse lived experiences. A key question to ask is how might the intersectionality of race and gender shape experiences of trans community connectedness for TGDNB adults?
A second research opportunity pertains to place. No study inquired into the meaning and significance of social support for TGDNB adults living exclusively within regional and/or rural settings. Neglecting the specificity of TGDNB experiences of the rural has led to what critical trans scholar Jack Halberstam termed a “meteronormative” bias of TGDNB research (Halberstam, 2005, p. 36). This narrative implicitly frames TGDNB identity practices outside metropolitan settings as exceptional, different or as some form of mimicry (Knopp & Brown, 2003). What is needed is research that explicitly centers the social support experiences of TGDNB adults living in regional or rural settings. As Abelson (2019) observed in her study of trans men from West, South and Midwest USA, gendered, racialized, classed and sexualized notions of what, exactly, is a man, creates systemic inequalities in place. Consideration of how these dynamics operate and potentially complicate experiences of social support among samples of regional and rural dwelling TGDNB adults is a recommended avenue for future research.
Limitations of the review
Despite the utility of this review for illuminating current trends in research, knowledge gaps and opportunities for knowledge production, there are several limitations. Firstly, this review did not assess the rigor of included studies nor rank these through the use of a standardized appraisal tool. Due to the inter-disciplinary nature of included studies and the heterogeneity of research methods employed, there was a lack of accepted appraisal criteria for achieving this (Pickering & Byrne, 2014). The results presented simply map the breadth of the literature, a critical function of the SQLR, rather than evaluating its depth, a function achieved through more traditional review methods. A second limitation pertains to potential biases in searching for relevant literature. We did not review research published in languages other than English, nor did we include research studies that were not accessible via electronic databases. The authors recognize that there is an under-representation of “negative” or “neutral” research findings in published journals, a potential limitation of this review. Finally, the search criteria demanded that a minimum of one search term appears in the title, abstract or keywords of an article. As a result, studies that have considered proximal social determinants of TGDNB health but did not mention an included term for social support in any of the three sections may have been overlooked. It is recommended that future researchers are prudent in achieving a balance between comprehensiveness and precision when conducting future systematic reviews on this topic.
Conclusion
This is the first study to systematically review TGDNB adult’s experiences of social support. This review has demonstrated the significance of social support as a protective factor for TGDNB health and well-being, most notably support provided by TGDNB peers. A key opportunity for future research lies in the development of a context-specific definition of social support. This definition must maintain sensitivity to both intersectionality and the significance of place in determining what is socially supportive to TGDNB adults. Ultimately, a context-specific definition of social support will enable greater insight into the dynamics of social support as a determinant of health and well-being for TGDNB adults and the subsequent development of TGDNB-specific social support inventories.
Disclosure statement
The authors have no conflict of interest to declare.
References
- Abelson, M. (2019). Men in place: Trans masculinity, race and sexuality in America. University of Minnesota Press. [Google Scholar]
- Adams, N., Hitomi, M., & Moody, C. (2017). Varied reports of adult transgender suicidality: Synthesizing and describing the peer-reviewed and gray literature. Transgender Health, 2(1), 60–75. 10.1089/trgh.2016.0036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barr, S. M., Budge, S. L., & Adelson, J. L. (2016). Transgender community belongingness as a mediator between strength of transgender identity and well-being. Journal of Counseling Psychology, 63(1), 87–97. 10.1037/cou0000127 [DOI] [PubMed] [Google Scholar]
- Başar, K., & Öz, G. (2016). Resilience in individuals with gender dysphoria: Association with perceived social support and discrimination. Turk Psikiyatri Dergisi = Turkish Journal of Psychiatry, 27(4), 225–234. 10.5080/u17071 [DOI] [PubMed] [Google Scholar]
- Başar, K., Öz, G., & Karakaya, J. (2016). Perceived discrimination, social support, and quality of life in gender dysphoria. The Journal of Sexual Medicine, 13(7), 1133–1141. 10.1016/j.jsxm.2016.04.071 [DOI] [PubMed] [Google Scholar]
- Bauer, G. R., Redman, N., Bradley, K., & Scheim, A. I. (2013). Sexual health of trans men who are gay, bisexual, or who have sex with men: Results from Ontario, Canada. The International Journal of Transgenderism, 14(2), 66–74. 10.1080/15532739.2013.791650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer, G. R., Scheim, A. I., Pyne, J., Travers, R., & Hammond, R. (2015). Intervenable factors associated with suicide risk in transgender persons: A respondent driven sampling study in Ontario, Canada. BMC Public Health, 15(1), 525. 10.1186/s12889-015-1867-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bethea, M. S., & McCollum, E. E. (2013). The disclosure experiences of male-to-female transgender individuals: A systems theory perspective. Journal of Couple & Relationship Therapy, 12(2), 89–112. 10.1080/15332691.2013.779094 [DOI] [Google Scholar]
- Birkeland, M. S., Nielsen, M. B., Hansen, M. B., Knardahl, S., & Heir, T. (2017). Like a bridge over troubled water? A longitudinal study of general social support, colleague support, and leader support as recovery factors after a traumatic event. European Journal of Psychotraumatology, 8(1), 1302692. 10.1080/20008198.2017.1302692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boza, C., & Nicholson Perry, K. (2014). Gender-related victimization, perceived social support, and predictors of depression among transgender Australians. International Journal of Transgenderism, 15(1), 35–52. 10.1080/15532739.2014.890558 [DOI] [Google Scholar]
- Brown, T., & Peerapatanapokin, W. (2019). Evolving HIV epidemics: The urgent need to refocus on populations with risk. Current Opinion in HIV and Aids, 14(5), 337–353. 10.1097/COH.0000000000000571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budge, S. L., Chin, M. Y., & Minero, L. P. (2017). Trans individuals' facilitative coping: An analysis of internal and external processes. Journal of Counseling Psychology, 64(1), 12–25. 10.1037/cou0000178 [DOI] [PubMed] [Google Scholar]
- Budge, S. L., Rossman, H. K., & Howard, K. A. S. (2014). Coping and psychological distress among genderqueer individuals: The moderating effect of social support. Journal of LGBT Issues in Counseling, 8(1), 95–117. 10.1080/15538605.2014.853641 [DOI] [Google Scholar]
- Carter, S., Allred, K., Tucker, R., Simpson, T., Shipherd, J., & Lehavot, K. (2019). Discrimination and suicidal ideation among transgender veterans: The role of social support and connection. LGBT Health, 6(2), 43–50. 10.1089/lgbt.2018.0239 [DOI] [PubMed] [Google Scholar]
- Claes, L., Bouman, W. P., Witcomb, G., Thurston, M., Fernandez‐Aranda, F., & Arcelus, J. (2015). Non-suicidal self-injury in trans people: Associations with psychological symptoms, victimization, interpersonal functioning, and perceived social support. The Journal of Sexual Medicine, 12(1), 168–179. 10.1111/jsm.12711 [DOI] [PubMed] [Google Scholar]
- Clark, K., Fletcher, J. B., Holloway, I. W., & Reback, C. J. (2018). Structural inequities and social networks impact hormone use and misuse among transgender women in Los Angeles county. Archives of Sexual Behavior, 47(4), 953–962. 10.1007/s10508-017-1143-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, S. (2000). Social support measurement and intervention: A guide for health and social scientists. Oxford University Press. [Google Scholar]
- Creswell, J. W. (2018). Qualitative inquiry & research design: Choosing among five approaches (4th ed.). SAGE. [Google Scholar]
- Davey, A., Arcelus, J., Meyer, C., & Bouman, W. P. (2016). Self-injury among trans individuals and matched controls: Prevalence and associated factors. Health & Social Care in the Community, 24(4), 485–494. 10.1111/hsc.12239 [DOI] [PubMed] [Google Scholar]
- Davey, A., Bouman, W. P., Arcelus, J., & Meyer, C. (2014). Social support and psychological well-being in gender dysphoria: a comparison of patients with matched controls. The Journal of Sexual Medicine, 11(12), 2976–2985. 10.1111/jsm.12681 [DOI] [PubMed] [Google Scholar]
- Dowers, E., White, C., & Kingsley, J. (2020). Virtually trans: An Australian Facebook group supporting gender diverse adults’ health and wellbeing . Manuscript Submitted for Publication. [DOI] [PubMed]
- Drageset, S., Lindstrøm, T. C., Giske, T., & Underlid, K. (2016). Women’s experiences of social support during the first year following primary breast cancer surgery. Scandinavian Journal of Caring Sciences, 30(2), 340–348. 10.1111/scs.12250 [DOI] [PubMed] [Google Scholar]
- Erich, S., Tittsworth, J., & Kersten, A. S. (2010). An examination and comparison of transsexuals of color and their white counterparts regarding personal well-being and support networks. Journal of GLBT Family Studies, 6(1), 25–39. 10.1080/15504280903472493 [DOI] [Google Scholar]
- Factor, R., & Rothblum, E. (2007). A study of transgender adults and their non-transgender siblings on demographic characteristics, social support, and experiences of violence. Journal of LGBT Health Research, 3(3), 11–30. 10.1080/15574090802092879. [DOI] [PubMed] [Google Scholar]
- Frost, D. M., Meyer, I. H., & Schwartz, S. (2016). Social support networks among diverse sexual minority populations. The American Journal of Orthopsychiatry, 86(1), 91–102. 10.1037/ort0000117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller, K. A., & Riggs, D. W. (2018). Family support and discrimination and their relationship to psychological distress and resilience amongst transgender people. International Journal of Transgenderism, 19(4), 379–388. 10.1080/15532739.2018.1500966 [DOI] [Google Scholar]
- Gamarel, K. E., Reisner, S. L., Laurenceau, J.-P., Nemoto, T., & Operario, D. (2014). Gender minority stress, mental health, and relationship quality: A dyadic investigation of transgender women and their cisgender male Partners. Journal of Family Psychology, 28(4), 437–447. 10.1037/a0037171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner, A. T., de Vries, B., & Mockus, D. S. (2014). Aging out in the desert: Disclosure, acceptance, and service use among midlife and older lesbians and gay men. Journal of Homosexuality, 61(1), 129–144. 10.1080/00918369.2013.835240 [DOI] [PubMed] [Google Scholar]
- Gariépy, G., Honkaniemi, H., & Quesnel-Vallée, A. (2016). Social support and protection from depression: Systematic review of current findings in Western countries. The British Journal of Psychiatry: The Journal of Mental Science, 209(4), 284–293. https://doi.org/.1192/bjp.bp.115.169094 [DOI] [PubMed] [Google Scholar]
- Germov, J. (2014). Second opinion: An introduction to health sociology (5th ed.). Oxford University Press. [Google Scholar]
- Graham, L. F., Crissman, H. P., Tocco, J., Hughes, L. A., Snow, R. C., & Padilla, M. B. (2014). Interpersonal relationships and social support in transitioning narratives of black transgender women in Detroit. International Journal of Transgenderism, 15(2), 100–113. 10.1080/15532739.2014.937042 [DOI] [Google Scholar]
- Grant, J. M., Mottet, L. A., Tanis, J., Harrison, J., Herman, J., & Keisling, M. (2011). Injustice at every turn: A report of the national transgender discrimination survey. National Center for Transgender Equality and National Gay and Lesbian Task Force. [Google Scholar]
- Guitart, D., Pickering, C., & Byrne, J. (2012). Past results and future directions in urban community gardens research. Urban Forestry & Urban Greening, 11(4), 364–373. 10.1016/j.ufug.2012.06.007 [DOI] [Google Scholar]
- Halberstam, J. (2005). In a queer time and place. University of California Press. [Google Scholar]
- Herbst, J. H., Jacobs, E. D., Finlayson, T. J., McKleroy, V. S., Neumann, M. S., Crepaz, N., & HIV/AIDS Prevention Research Synthesis Team . (2008). Estimating HIV prevalence and risk behaviors of transgender persons in the United States: A systematic review. AIDS and Behavior, 12(1), 1–17. 10.1007/s10461-007-9299-3 [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad, J., Smith, T. B., & Layton, J. B. (2010). Social relationships and mortality risk: A meta-analytic review. PLoS Medicine, 7(7), e1000316. 10.1371/journal.pmed.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwahng, S. J., Allen, B., Zadoretzky, C., Barber, H., Mcknight, C., & Des Jarlais, D. (2019). Alternative kinship structures, resilience and social support among immigrant trans Latinas in the USA. Culture, Health & Sexuality, 21(1), 1–15. 10.1080/13691058.2018.1440323 [DOI] [PubMed] [Google Scholar]
- Hyde, Z., Doherty, M., Tilley, P., McCaul, K., Roonery, R., & Jancey, J. (2014). The first Australian national trans mental health study: Summary of results. Curtin University. [Google Scholar]
- Kerry, S. C. (2014). Sistergirls/Brotherboys: The status of Indigenous transgender Australians. International Journal of Transgenderism, 15(3–4), 173–186. 10.1080/15532739.2014.995262 [DOI] [Google Scholar]
- Klein, A., & Golub, S. (2016). Family rejection as a predictor of suicide attempts and substance misuse among transgender and gender nonconforming adults. LGBT Health, 3(3), 193–202. 10.1089/lgbt.2015.0111 [DOI] [PubMed] [Google Scholar]
- Knopp, L., & Brown, M. (2003). Queer cultural geographies- we're here! We're queer! We're over there, too! In K. Anderson (Ed.), Handbook of cultural geography (pp. 313–324). SAGE.
- Koch-Gallenkamp, L., Bertram, H., Eberle, A., Holleczek, B., Schmid-Höpfner, S., Waldmann, A., Zeissig, S. R., Brenner, H., & Arndt, V. (2016). Fear of recurrence in long-term cancer survivors-Do cancer type, sex, time since diagnosis, and social support matter? Health Psychology, 35(12), 1329–1333. 10.1037/hea0000374 [DOI] [PubMed] [Google Scholar]
- Koken, J. A., Bimbi, D. S., & Parsons, J. T. (2009). Experiences of familial acceptance-rejection among transwomen of color. Journal of Family Psychology, 23(6), 853–860. 10.1037/a0017198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCartney, G., Popham, F., McMaster, R., & Cumbers, A. (2019). Defining health and health inequities. Public Health, 172, 22–30. 10.1016/j.puhe.2019.03.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDowell, M., Hughto, J., & Reisner, S. (2019). Risk and protective factors for mental health morbidity in a community sample of female-to-male trans-masculine adults. BMC Psychiatry, 19(16), 1–12. https://doi/org.10.1186/s12888-018-2008-0 [DOI] [PMC free article] [PubMed]
- Mclaren, S., & Challis, C. (2009). Resilience among men farmers: The protective roles of social support and sense of belonging in the depression-suicidal ideation relation. Death Studies, 33(3), 262–276. 10.1080/07481180802671985 [DOI] [PubMed] [Google Scholar]
- Miner, M. H., Bockting, W. O., Romine, R. S., & Raman, S. (2012). Conducting internet research with the transgender population: Reaching broad samples and collecting valid data. Social Science Computer Review, 30(2), 202–211. 10.1177/0894439311404795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med, 6(7), e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed]
- Pflum, S., Testa, R., Balsam, K., Goldblum, P., & Bongar, B. (2015). Social support, trans community connectedness, and mental health symptoms among transgender and gender nonconforming adults. Psychology of Sexual Orientation and Gender Diversity, 2(3), 281–286. 10.1037/sgd0000122 [DOI] [Google Scholar]
- Pickering, C., & Byrne, J. (2014). The benefits of publishing systematic quantitative literature reviews for PhD candidates and other early-career researchers. Higher Education Research & Development, 33(3), 534–548. 10.1080/07294360.2013.841651 [DOI] [Google Scholar]
- Rotondi, N. K., Bauer, G. R., Travers, R., Travers, A., Scanlon, K., & Kaay, M. (2011). Depression in male-to-female transgender Ontarians: Results from the trans PULSE project. Canadian Journal of Community Mental Health, 30(2), 113–133. 10.7870/cjcmh-2011-0020 [DOI] [Google Scholar]
- Scandurra, C., Amodeo, A. L., Valerio, P., Bochicchio, V., & Frost, D. M. (2017). Minority stress, resilience, and mental health: A study of Italian transgender people. Journal of Social Issues, 73(3), 563–585. 10.1111/josi.12232 [DOI] [Google Scholar]
- Scheim, A. I., Adam, B. D., & Marshall, Z. (2019). Gay, bisexual, and queer trans men navigating sexual fields. Sexualities, 22(4), 566–586. 10.1177/1363460717716426 [DOI] [Google Scholar]
- Serano, J. (2009). Whipping girl: A transsexual woman on sexism and the scapegoating of femininity. Seal Press. [Google Scholar]
- Sherman, A. D. F., Clark, K. D., Robinson, K., Noorani, T., & Poteat, T. (2020). Trans* community connection, health, and wellbeing: A systematic review. LGBT Health, 7(1), 1–13. 10.1089/lgbt.2019.0014 [DOI] [PubMed] [Google Scholar]
- Singh, A. A. (2013). Transgender youth of color and resilience: Negotiating oppression and finding support. Sex Roles, 68(11–12), 690–702. 10.1007/s11199-012-0149-z [DOI] [Google Scholar]
- Singh, A. A., Hays, D. G., & Watson, L. S. (2011). Strength in the face of adversity: Resilience strategies of transgender individuals. Journal of Counseling & Development, 89(1), 20–27. 10.1002/j.1556-6678.2011.tb00057.x [DOI] [Google Scholar]
- Strauss, P., Cook, A., Winter, S., Watson, V., Wright-Toussaint, D., & Lin, A. (2017). Trans pathways: The mental health experiences and care pathways of trans young people. Summary of results. Telethon Kids Institute. [Google Scholar]
- Tan, J., & Wang, Y. (2019). Social integration, social support, and all-cause, cardiovascular disease and cause-specific mortality: A prospective cohort study. International Journal of Environmental Research and Public Health, 16(9), 1498. 10.3390/ijerph16091498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas, E. C., Muralidharan, A., Medoff, D., & Drapalski, A. L. (2016). Self-efficacy as a mediator of the relationship between social support and recovery in serious mental illness. Psychiatric Rehabilitation Journal, 39(4), 352–360. 10.1037/prj0000199 [DOI] [PubMed] [Google Scholar]
- Trujillo, M. A., Perrin, P. B., Sutter, M., Tabaac, A., & Benotsch, E. G. (2017). The buffering role of social support on the associations among discrimination, mental health, and suicidality in a transgender sample. International Journal of Transgenderism, 18(1), 39–52. 10.1080/15532739.2016.1247405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino, B. N. (2006). Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine, 29(4), 377–387. 10.1007/s10865-006-9056-5 [DOI] [PubMed] [Google Scholar]
- Wang, J., Mann, F., Lloyd-Evans, B., Ma, R., & Johnson, S. (2018). Associations between loneliness and perceived social support and outcomes of mental health problems: A systematic review. BMC Psychiatry, 18(1), 156. 10.1186/s12888-018-1736-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westbrook, L., & Schilt, K. (2014). Doing gender, determining gender: Transgender people, gender panics, and the maintenance of the sex/gender/sexuality system. Gender & Society, 28(1), 32–57. 10.1177/0891243213503203 [DOI] [Google Scholar]
- Williams, P., Barclay, L., & Schmied, V. (2004). Defining social support in context: A necessary step in improving research, intervention, and practice. Qualitative Health Research, 14(7), 942–960. 10.1177/1049732304266997 [DOI] [PubMed] [Google Scholar]
- Winter, S., Diamond, M., Green, J., Karasic, D., Reed, T., Whittle, S., & Wylie, K. (2016). Transgender people: Health at the margins of society. The Lancet, 388(10042), 390–400. 10.1016/S0140-6736(16)00683-8 [DOI] [PubMed] [Google Scholar]
- Yang, E. C. L., Khoo-Lattimore, C., & Arcodia, C. (2017). A systematic literature review of risk and gender research in tourism. Tourism Management, 58, 89–100. 10.1016/j.tourman.2016.10.011 [DOI] [Google Scholar]
- Yang, X., Wang, L., Hao, C., Gu, Y., Song, W., Wang, J., Chang, M. M., & Zhao, Q. (2015). Sex partnership and self-efficacy influence depression in Chinese transgender women: A cross-sectional study. PLoS One, 10(9), e0136975. 10.1371/journal.pone.0136975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet, G. D., Dahlem, N. W., Zimet, S. G., & Farley, G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30–41. 10.1207/s15327752jpa5201_2 [DOI] [PubMed] [Google Scholar]