Abstract
Rheumatoid arthritis (RA) is an autoimmune disease characterized by proliferative synovitis, which can cause cartilage and bone damage as well as functional limitations. Disease-modifying anti-rheumatic drugs have significantly improved the prognosis of RA patients. However, people with RA, when combined with hepatitis B virus (HBV) infection, may experience reactivation of HBV during treatment with anti-rheumatic drugs. The outcome of HBV reactivation (HBVr) varies from liver inflammation to liver failure, while insufficient HBV screening in RA patients has been reported in various countries. Therefore, it is necessary to identify patients at high risk before starting immunosuppressive therapy. The immune response plays an important role in anti-HBV infection. However, most anti-rheumatic drugs exert an inhibitory effect on the body’s immune system, resulting in HBVr. Therefore, it is necessary to conduct a comprehensive evaluation based on host factors, viral factors, and drug factors. In this paper, we summarize the mechanism of HBVr, the risk of HBVr caused by anti-rheumatic drugs, and the appropriate diagnosis and treatment process for RA patients so that clinicians can have a more comprehensive understanding of HBVr in RA patients.
Keywords: Rheumatoid arthritis, Hepatitis B virus reactivation, Disease-modifying antirheumatic drugs, Risk factors
Core Tip: The application of anti-viral drugs and anti-rheumatic drugs improves the prognosis of patients with hepatitis B virus (HBV) infection and rheumatoid arthritis (RA). However, the reactivation of HBV in RA patients has not attracted enough attention. Although the HBV infection rate in RA patients is not high, once HBV reactivation (HBVr) occurs, it will cause serious consequences. Therefore, patients with HBV infection should undergo comprehensive evaluation before anti-rheumatic drug treatment. This paper summarizes the mechanism of HBVr, the risk of HBVr caused by anti-rheumatic drugs, and the appropriate diagnosis and treatment process for RA patients.
INTRODUCTION
Chronic hepatitis B (CHB) is a prevalent disease worldwide, and it is also the main cause of cirrhosis and liver cancer[1,2]. The application of pegylated interferon (IFN), entecavir, tenofovir disoproxil fumarate (TDF), and other highly effective anti-viral drugs has significantly improved the prognosis of patients[3,4]. Some patients can even obtain hepatitis B surface antigen (HBsAg) clearance to achieve a “functional cure”[5]. However, for some special populations, such as cancer patients undergoing chemotherapy, biological agents are used to treat autoimmune diseases or for organ or tissue transplantation and so on. When combined with hepatitis B virus (HBV) infection, if there is no anti-viral prophylaxis, the use of immunosuppressive agents or chemotherapeutic agents may lead to liver injury or even death[6]. The cause of this condition is now known as HBV reactivation (HBVr). HBVr was first reported in 1975 in patients with lymphoproliferative and myeloproliferative disorders[7,8]. Subsequently, it was observed in various diseases[9,10]. However, there is currently no uniform definition of HBVr.
Rheumatoid arthritis (RA) is an autoimmune disease characterized by erosive arthritis as its main clinical manifestation. The incidence of disability and functional limitation increases with the course of disease[11]. Disease-modifying anti-rheumatic drugs (DMARDs) have significantly improved the clinical and radiographic outcomes in RA patients[12]. Epidemiological studies show that the distribution of RA is global, and the average incidence rate is 1%. The incidence rate of RA in China is 0.2% to 0.4% and in Japan, the prevalence is estimated at 0.6%-1.0%[13]. The Asia Pacific region has a high incidence of HBV infection. The relatively high prevalence of both HBV infection and various forms of RA will result in the coexistent diagnoses of both diseases in a substantial number of patients. For example, a study in Japan showed that approximately 20% or more of patients with rheumatic diseases are infected with HBV[14]. Insufficient HBV screening has been reported in various countries[15-17]. We know that most anti-rheumatic drugs work by downregulating the overactivated immune system. Several studies have reported that people with RA combined with HBV infection, especially those with occult HBV infection or resolved carriers, may reactivate HBV during treatment with anti-rheumatic drugs[18-21]. Due to different research populations, drugs, and definitions of HBVr, the reported rates of HBVr are significantly different, ranging from 0 to 100%[22,23]. The outcome of HBVr varies from liver inflammation to liver failure. Therefore, more attention should be given to the reactivation of HBV in RA patients.
MECHANISMS OF HBV REACTIVATION
The steps for HBV to achieve virus replication and cell infection include cell entry, relaxed circular DNA repair, covalently closed circular DNA (cccDNA) transcription and translation, pre-genomic RNA reverse transcription, and secretion of virus particles[24]. cccDNA is the template for replication. Nucleos(t)ide analogues (NAs) and IFN are the two main types of drugs for CHB anti-viral therapy. NAs can effectively reduce the HBV DNA load by inhibiting virus replication by acting on the retroviral process. IFN has the dual functions of direct anti-viral and immune regulation. However, neither drug has an effect on HBV replication template cccDNA. Therefore, the continuous existence of cccDNA in the hepatocyte nucleus is an important source of persistent HBV replication and infection. Studies have shown that even if HBV DNA in the peripheral blood of patients is lower than the detection threshold or even if HBsAg is cleared, the presence of cccDNA can still be detected in liver cells[25,26]. From the above information, it is very difficult to eradicate HBV, and the long-term existence of cccDNA is an important cause of HBVr.
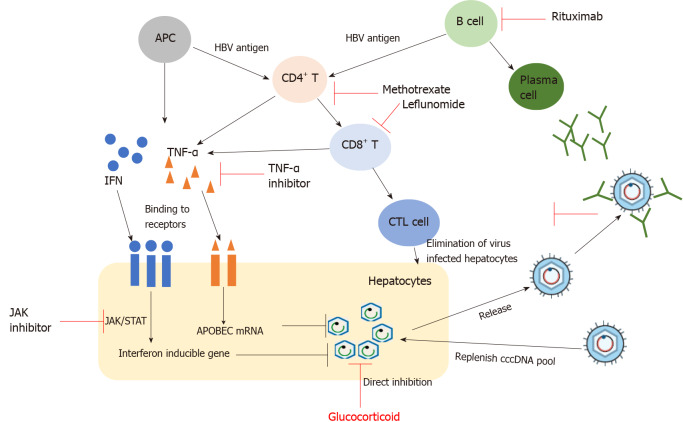
Studies have shown that the host immune response plays an important role in anti-HBV infection (Figure 1). After HBV infection, the release of antigenic substances induces B cells to produce corresponding antibodies, such as HBV surface antibody (anti-HBs), antibody to HBV core antigen (anti-HBc), and antibody to HBV envelope antigen (anti-HBe). They are important reference indicators for the clinical diagnosis of HBV infection stage. However, among these antibodies, only anti-HBs has a protective effect on the body. In addition to producing neutralizing antibodies, B cells also have the function of antigen presentation, which can present antigens to CD4+ T cells to exert anti-viral effects. CD4+ T cells can differentiate into helper T cells of different subtypes under antigen stimulation. These cells play an indirect anti-viral role by regulating the function of virus-specific CD8+ T cells and B cells. Cytotoxic T lymphocytes (CTL) play the most direct and critical anti-viral role in the anti-viral immune process. On the one hand, CTL directly kill infected hepatocytes by secreting substances such as granulomycin B and perforin, which promote cell lysis. On the other hand, CTL kill infected hepatocytes by secreting specific cytokines, including IFN-γ and tumour necrosis factor α (TNF-α), and then achieve the effect of clearing the virus, called the non-lysing pathway. Under normal circumstances, most adults with sound immune function can clear the virus through the coordination of the innate immune response and adaptive immune response and can obtain resistance to HBV re-infection. However, in HBV infection, CD8+ T cell function is exhausted under the combined action of multiple factors, which is one of the main causes of chronic infection[27].
Figure 1.
Hepatitis B virus life cycle and mechanisms associated with hepatitis B virus reactivation linked to immunosuppressive therapies. APC: Antigen presenting cell; CTL cell: Cytotoxic T lymphocyte cell; cccDNA: Covalently closed circular DNA; IFN: Interferon; TNF-α: Tumour necrosis factor α; JAK: Janus kinase; HBV: Hepatitis B virus.
The reactivation of HBV mainly occurs during the application of various immunosuppressive agents in specific populations, among which HBVr is the most common phenomenon in patients with chemotherapy-treated diffuse lymphoma. When treated with immunosuppressive drugs (ISDs), the body’s immune system is suppressed, and HBV replicates and infects more liver cells; when the ISDs are reduced or stopped, the body’s immunity will gradually recover and quickly start immune killing of HBV-infected hepatocytes, resulting in varying degrees of liver damage. When the body’s immune response is too strong, it will lead to necrosis of a large number of liver cells and even to liver failure and death. For example, corticosteroids (CSs) are commonly used in the treatment of RA. When RA with HBsAg- and/or anti-HBc-positive patients are treated with high-dose, long-course CSs, they are more likely to experience HBVr. This is mainly because CSs can directly act on the glucocorticoid response element that controls viral replication and transcriptional activity in HBV, thus promoting HBV replication and increasing the risk of HBVr[28].
RISK OF HBV REACTIVATION WITH DIFFERENT ANTI-RHEUMATIC DRUGS
ISDs, that is, conventional synthetic DMARDs (cDMARDs) and biologic DMARDs, target the synthesis of DMARDs and steroids used for RA and can cause HBVr (Table 1). Therefore, evaluating the risk of reactivation for each drug is very important.
Table 1.
Risk of hepatitis B virus reactivation with different immunosuppressants
|
Medication
|
Mechanism
|
Definition of HBV reactivation
|
Study population
|
Reactivation rate
|
| Methotrexate | Suppressive HBV specific cytotoxic T cell response and the production of proinflammatory cytokines | HBV DNA > 103 (copies/mL) | HBsAg-positive | Low risk[29,30] |
| HBsAg-negative | Low risk[30] | |||
| Leflunomide | Inhibition of the growth of activated lymphocytes by inhibition of dihydro-lactate dehydrogenase | 10-fold rise in HBV-DNA compared to baseline or a switch from undetectable to detectable | HBsAg-positive | High risk, contraindicated[31] |
| HBsAg-negative | No data | |||
| Corticosteroids | Immunomodulatory and anti-inflammatory | Switch from undetectable HBV DNA to detectable or a 10-fold increase compared with baseline[34] | HBsAg-positive | High risk (> 10 mg, > 4 wk); medium risk (< 10 mg, > 4 wk); low risk (< 10 mg, < 1 wk) |
| HBsAg-negative | 1%-1.8%[34,36] | |||
| TNF inhibitor | Dampening of the cytokine cascade and suppression of the cytotoxic CD8+ T-cell responses against HBV | An increase of serum HBV DNA levels by greater than 1 logs10 IU/mL or conversion from HBsAg- to HBsAg+ | HBsAg-positive | Medium-high risk (9.1%-75%)[23,38] |
| HBsAg-negative | Low risk (0-8.3%)[22,39] | |||
| Tocilizumab | Blocks IL-6 signaling by inhibiting its receptor | HBV-DNA level higher than 2.0 log copies/mL | HBsAg-positive | No data |
| HBsAg-negative | Low risk (8%)[40] | |||
| Tofacitinib | Inhibition of JAK signal pathway | An increase in HBV DNA by greater than 1 to 2 logs10 IU/mL or a reappearance of HBsAg | HBsAg-positive | High risk (100%)[41] |
| HBsAg-negative | Low risk (0) | |||
| Abatacept | Blocks co-stimulation of T lymphocytes | Conversion from HBsAg- to HBsAg+ | HBsAg-positive | Medium risk[34] |
| HBsAg-negative | Low risk[34] |
HBsAg: Hepatitis B surface antigen; HBV: Hepatitis B virus.
Methotrexate (MTX) is a folic acid antagonist that was initially used to treat tumors and has now become the most widely used drug for RA. MTX can suppress the HBV-specific cytotoxic T cell response and inhibit the production of proinflammatory cytokines such as TNF-α, interleukin (IL)-1, and IL-6. At present, insufficient data are available to identify the risk of cDMARD-related HBVr. In one study, only 3 (2 were HBsAg-positive and 1 was HBsAg-negative/anti-HBc-positive) of 211 patients (23 were HBsAg-positive and 188 were HBsAg-negative/anti-HBc-positive) had HBVr with MTX treatment[29]. Similarly, only one case of HBVr was reported in a cross-sectional study conducted in Thailand in HBsAg-positive patients[30]. For HBsAg-negative and anti-HBc-positive patients, although there have been a few case reports of HBVr using MTX alone or combined with other DMARDs, the risk of HBVr seems rather low in these patients and in a large cohort study conducted by Laohapand et al[30], HBVr was not detected in such patients[20,30]. In general, MTX is relatively safe in RA patients with chronic or past HBV infection.
Leflunomide (LEF) is the world’s first recognized DMARD specifically for the treatment of RA and can effectively control the course of disease and prevent bone destruction. Its role is mainly to inhibit the growth of activated lymphocytes by inhibiting dihydrolactic dehydrogenase. Although both MTX and LEF can cause HBVr, Mo et al[31] showed that MTX can be used as a therapeutic drug for RA patients in the HBV carrier state at low doses, while LEF increases the risk of HBVr (P = 0.011), and it is best to prohibit its use. This may be related to the drug properties of LEF. Studies have shown that LEF may activate HBV replication through nucleoside reduction-related phosphorylation of mitogen-activated protein kinase P38[32]. In addition, liver damage may also occur during the application of LEF[33].
CSs can produce powerful anti-inflammatory effects and immunomodulatory effects, so they are widely used in the treatment of RA. They can not only reduce the number of monocyte-macrophages in the circulatory system but can also reduce the synthesis of inflammatory factors. The link between CSs and HBVr has been strongly established in the literature. Fujita et al[15] and Chen et al[18] showed that CSs alone or in combination with other drugs would significantly increase the risk of HBVr in RA patients who received immunosuppressive therapy. This may be related to the mechanism of CSs[28]. In addition, the risk of reactivation varies with the dosage and course. The American Gastroenterological Association (AGA) guidelines have proposed that the risk of HBVr in RA patients be divided into different levels according to the amount of CSs and the duration of treatment: High risk – dose > 10 mg and treatment duration > 4 wk; medium risk – dose < 10 mg and treatment duration > 4 wk; and low risk – dose < 10 mg and treatment course < 1 wk[34]. Wong et al[35] reported that among CHB patients, a peak daily dose > 40 mg vs < 20 mg CS was an independent risk factor for hepatitis flare, and under the same treatment dose, the risk of hepatitis flare was significantly higher in patients with a treatment course of > 7 d vs < 7 d (P < 0.001)[35]. At present, little data exist on HBVr in HBsAg-negative and anti-HBc-positive patients after using CSs. However, according to the 2015 AGA guidelines, HBsAg-negative and anti-HBc-positive patients are considered to be a low-risk group (< 1%) in terms of the occurrence of HBVr during CS therapy[34,36].
TNF-α is a protein that promotes inflammation of the joints and plays an important role in coordinating innate immunity and adaptive immunity against HBV infection. In particular, TNF-α can activate apolipoprotein B mRNA-editing enzyme catalytic polypeptide (APOBEC) proteins, which cause the degradation of cccDNA in HBV-infected cells[37]. Thus, blocking TNF-α signalling may lead to a higher HBV replication state and HBVr. Drugs or biological agents that block its pathway have been widely used in various inflammatory and autoimmune diseases. The association between TNF inhibitor (TNFi) use and HBVr has been well established. In general, the risk of HBVr is significantly increased in HBsAg-positive RA patients without antiviral treatment. Studies have shown that for HBsAg-positive RA patients treated with TNFi, the HBVr rate is 9.1%-75%[23,38]. When compared with HBsAg-positive patients, individuals who are HBsAg-negative and anti-HBc-positive appear to have a lower risk of HBVr when exposed to TNFi, and the HBVr rate is 0-8.3%[22,39]. The different reactivation rates of HBV may be related to the size of the study population, the definition of HBVr, and the different types of TNF-α inhibitors. For HBsAg-negative and anti-HBc-positive patients, the existing data show that the risk may be partly attributable to the concomitant use of other immune suppressive drugs that are in the low-risk category. In contrast, when high risk agents such as rituximab are used in HBsAg-negative, anti-HBc-positive patients, high rates of reactivation in excess of 10% occur and antiviral prophylaxis can be anticipated to result in similar absolute risk reduction as described for HBsAg-positive patients[34].
IL-6 is a key factor in the pathogenesis of RA. It promotes inflammatory cell aggregation, stimulates synovial pannus formation, and induces osteoclast activation, leading to joint inflammation and bone destruction. Tocilizumab (TCZ) is a humanized monoclonal antibody that blocks IL-6 signalling by inhibiting its receptor. However, there are currently insufficient data on the effect of TCZ on HBVr in RA patients with chronic HBV infection. Only one study reported that in RA patients with past HBV infection, the HBVr rate was 8%[40].
The JAK/STAT signalling pathway plays an important role in the pathophysiology of RA and has a regulatory effect on various cells and cytokines in the inflammatory process of RA. JAK inhibitors are a new kind of targeted synthetic DMARDs. The nonselective JAK inhibitor tofacitinib was the first approved treatment for RA. In a study, six HBsAg-positive RA patients were treated with JAK inhibitors, among which four were treated with antiviral prophylaxis and two were not, and the two who were not treated with antiviral prophylaxis showed HBVr[41]. However, in RA patients with previous HBV infection, no reactivation of HBV was observed.
Abatacept is a selective T cell costimulatory regulator. It is a fusion protein comprising the extracellular functional region of human cytotoxic T lymphocyte associated antigen-4 (CTLA-4, also known as CD152) and the FC segment of human immunoglobulin (Ig) G-1. It inhibits the activation of T cells by binding to CD80 and CD86 on the surface of antigen presenting cells. At present, abatacept has been approved for the treatment of active RA, including moderate and severe active patients with poor treatment effects of MTX and TNFi, which can be used alone or in combination with cDMARDs[42]. At present, there have been reports on HBVr in RA patients after the application of abatacept, but most of them come from case reports, and there are few relevant cohort studies. In one study, four inactive HBV carriers who received abatacept treatment developed HBVr within an average of 10 mo[43]. In contrast, in another study, none of the 38 inactive HBV carriers who received abatacept treatment developed HBVr[44]. At present, the only study collected 27 patients with HBsAg-negative and anti-HBC-positive RA treated with abatacept, of whom 19% received preventive antiviral drugs, and there were no cases of HBVr[45]. Although the current research data are limited, the AGA classifies abatacept as a medium-risk drug (1%-10%) for HBVr in HBsAg positive patients and a low-risk agent in HBsAg negative and anti-HBC positive RA patients (< 1%)[34].
RISK FACTORS FOR HBV REACTIVATION
HBVr is affected by many factors that can be roughly divided into three categories: Host factors, viral factors, and drug factors. Host factors, including male sex, advanced age, and the presence of cirrhosis, are risk factors for HBVr[9,15,46,47]. Different ISDs cause different risks of HBVr, as shown in Table 1.
RA patients with different HBV infection statuses have different risks of reactivation[48]. According to natural history, HBV infection can be divided into the following five phases (Table 2). Phase 1 is hepatitis B e antigen (HBeAg)-positive chronic HBV infection, characterized by HBsAg and HBeAg positivity and high levels of HBV DNA but continuous normal alanine aminotransferase (ALT); in the liver, there is minimal or no liver inflammation. This phase is the stage of “harmonious co-existence” between the virus and the immune system. Phase 2 is characterized by HBeAg-positive CHB, serum HBsAg positivity, HBeAg positivity, HBV DNA positivity, and sustained or repeated increase in ALT, with accompanying moderate or severe liver necroinflammation. In this phase, the immune system of the body is activated, and the virus is quickly eliminated, but at the same time, it also causes damage to liver tissue. Phase 3 is HBeAg-negative chronic HBV infection and was previously termed the “inactive carrier” phase; it is characterized by HBsAg positivity, HBeAg negativity, undetectable or low (< 2000 IU/mL) HBV DNA, and normal ALT. In this phase, HBV DNA is in a low replication stage, and the immune system returns to normal again. However, when the body’s immunity is reduced for any reason, it will also cause a large amount of virus replication, thus entering Phase 4, or HBeAg-negative CHB, characterized by serum HBsAg positivity, HBeAg negativity, HBV DNA positivity, sustained or repeated elevations in ALT, and liver histology showing necroinflammation and fibrosis. In Phase 5, the HBsAg-negative phase is characterized by serum-negative HBsAg and anti-HBc positivity, with or without anti-HBs, and ALT is within the normal range. This stage is currently the “optimal endpoint” for CHB treatment, but cccDNA can still be detected in most liver tissues. It is generally believed that CHB (HBeAg positive and negative) has the highest risk of reactivation, followed by inactive carriers. Although HBsAg clearance is currently called a “functional cure”, there is still a risk of reactivation, but compared with other phases, the risk of reactivation is relatively low. In the study of Cantini et al[49], 21 studies were included in a systematic review, and 10 were eligible for meta-analysis. The results showed that the pooled prevalence of reactivation was 3.0% for patients with occult infection and 15.4% for chronic HBV infection[49]. The study by Lin et al[50] also showed that the HBV reactivation rate in inflammatory arthritis patients was low in resolved patients and moderate in chronic HBV infection patients. Furthermore, lower rates were observed in chronic HBV infection patients who used anti-viral prophylaxis.
Table 2.
Characteristics of different phases of hepatitis B virus infection
|
|
|
|
|
HBsAg
|
Anti-HBs
|
HBeAg
|
Anti-HBe
|
Anti-HBc
|
HBV DNA
|
ALT
|
| HBV seronegative | - | +/- | - | - | - | - | Normal | |||
| HBV infection | Phase 1 | Chronic HBV infection | + | - | + | - | + | > 20000 IU/mL | Normal | |
| Phase 2 | CHB | HBeAg(+) | + | - | + | - | + | > 20000 IU/mL | > 2 ULN | |
| Phase 4 | CHB | HBeAg(-) | + | - | - | + | + | > 2000 IU/mL | > 2 ULN | |
| Phase 3 | Inactive HBsAg carrier | + | - | - | +/- | + | < 2000 IU/mL | Normal | ||
| Phase 5 | Resolved infection | - | +/- | - | + | + | - | Normal |
HBsAg: Hepatitis B surface antigen; anti-HBs: Antibody to hepatitis B surface antibody; HBeAg: Hepatitis B e antigen; anti-HBe: Antibody to hepatitis B envelope antigen; anti-HBc: Antibody to hepatitis B core antigen; CHB: Chronic hepatitis B; HBV: Hepatitis B virus; ALT: Alanine aminotransferase; ULN: Upper limit of normal.
Anti-HBs antibodies are protective antibodies produced by the body that can neutralize HBsAg. At present, many studies have found that anti-HBs levels affect HBVr in patients with RA treated with immunosuppressants[12,51,52]. In a retrospective study, 152 RA patients with resolved HBV were enrolled. During the observation period of 15 mo, 7 (4.6%) patients developed HBVr. Patients who were negative for anti-HBs showed a significantly higher incidence of HBVr (P = 0.013)[12]. Similarly, in the study by Tien et al[51], 380 patients with RA were treated with biologics, and compared with the anti-HBs < 100 mIU/mL group, the anti-HBs > 100 mIU/mL group had no HBVr[51]. Therefore, we should pay more attention to the detection of anti-HBs when using ISDs for RA patients with HBV infection. In addition, we also need to pay attention to special situation-HBV S region mutants. HBV is a virus with a high mutation rate. In particular, regarding the “α” antigenic determinant in the HBV S region, protein structure changes caused by amino acid changes at this site may cause HBsAg antigenic changes or even decrease the antibody neutralizing ability[53], resulting in the failure of reagent detection[54]. Therefore, only when anti-HBs produced by the body can neutralize HBsAg does it have a protective effect.
In addition, the application of different types of anti-rheumatic drugs also affects HBV reactivation. Lin et al[50] showed that TNF-α inhibitors significantly reduced the risk of HBV reactivation compared with other anti-rheumatic drugs (1.4% vs 6.1%), which was consistent with Cantini et al[49]’s report. However, in other studies, TNF-α inhibitors such as infliximab and adalimumab have a relatively high risk (62.5%) of HBVr in HBsAg-positive patients[39].
PREVENTION AND MANAGEMENT OF HBV REACTIVATION IN RA
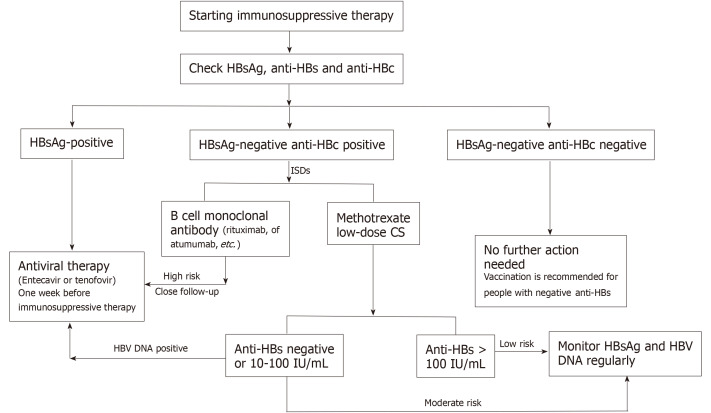
There is a risk of HBVr in RA patients when they are treated with ISDs. Therefore, it is necessary to identify patients at high risk before starting immunosuppressive therapy. We recommended that all RA patients be screened for HBsAg, anti-HBs, and anti-HBc when applying ISDs. According to the different detection results, the following three categories exist (Figure 2):
Figure 2.
Suggested process for screening, monitoring, and prevention of hepatitis B virus reactivation. HBsAg: Hepatitis B surface antigen; anti-HBs: Antibody to hepatitis B surface antibody; anti-HBc: Antibody to hepatitis B core antigen; ISDs: Immunosuppressive drugs; CS: Corticosteroid; HBV: Hepatitis B virus.
HBsAg-positive, anti-HBc-positive patients
HBsAg-positive patients have the highest risk of HBVr during immunosuppressive therapy. Timely antiviral therapy can effectively prevent HBVr[48]. Therefore, in HBsAg-positive RA patients, anti-viral prophylaxis is recommended before immunosuppressive therapy[55]. ETF and TDF can be used as the first choice[56].
HBsAg-negative, anti-HBc-positive patients
HBsAg-negative and anti-HBc-positive patients can be divided into different categories according to the level of antibodies and drugs. When RA patients are treated with rituximab, high-dose CS, or infliximab, HBVr is a high risk. Close follow-up, if necessary, is recommended before immunosuppressive treatment. For those who are treated with MTX or low-dose CS and have anti-HBs > 100 IU/L, the risk of HBVr is low. It is recommended that HBV DNA and ALT be regularly tested during therapy. If HBV DNA is elevated, it is also recommended that antiviral treatment be started. For those with negative or anti-HBs < 100 IU/L, there is a moderate risk of HBVr. Regular follow-up is also recommended.
HBsAg-negative, anti-HBc-negative patients
For RA patients who have not been infected with HBV but are anti-HBs positive (preferably ≥ 100 IU/mL), no additional operation is needed. However, if they are anti-HBs negative, a hepatitis B vaccine is recommended.
Finally, the ideal time interval between antiviral therapy and immunosuppressive therapy was determined. For people at high risk of HBVr (such as HBsAg-positive and anti-HBC-positive), antiviral therapy should be applied 1 wk before the start of ISDs treatment. For HBsAg-negative and anti-HBC-positive patients, if B-cell monoclonal antibodies are used, antiviral drugs can be considered[34,57]. After the cessation of immunosuppressant treatment, NAs treatment should be continued for at least 6 mo. If B cell monoclonal antibodies are used, NAs treatment should be continued for at least 12 mo after stopping immunosuppressive treatment. After NAs are stopped, there may be recurrence and even worsening of the disease. Follow-up and monitoring should be considered[58].
CONCLUSION
The application of anti-viral drugs and anti-rheumatic drugs improves the prognosis of patients with HBV and RA. However, the reactivation of HBV in RA patients has not attracted enough attention. Although the infection rate of RA patients with HBV is not high, once HBVr occurs, it will cause serious consequences. Therefore, patients with RA should undergo comprehensive evaluation before anti-rheumatic drug treatment, including patient age, sex, anti-HBs level, HBV DNA load, and ISDs. Patients who are at high risk of HBVr need to undergo regular testing for ALT and HBV DNA. Once they meet the treatment indications, anti-viral treatment should be carried out in a timely manner. Drugs with strong anti-viral effects and high drug resistance barriers are the best choice.
Footnotes
Conflict-of-interest statement: The authors declare that they have no actual or potential competing interest related to this article.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: June 7, 2021
First decision: September 1, 2021
Article in press: November 28, 2021
Specialty type: Infectious diseases
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kishida Y, Korkmaz P S-Editor: Yan JP L-Editor: Wang TQ P-Editor: Yan JP
Contributor Information
Ya-Li Wu, Center for Endocrine Metabolism and Immune Diseases, Beijing Luhe Hospital, Capital Medical University, Beijing 101149, China.
Jing Ke, Center for Endocrine Metabolism and Immune Diseases, Beijing Luhe Hospital, Capital Medical University, Beijing 101149, China.
Bao-Yu Zhang, Center for Endocrine Metabolism and Immune Diseases, Beijing Luhe Hospital, Capital Medical University, Beijing 101149, China.
Dong Zhao, Center for Endocrine Metabolism and Immune Diseases, Beijing Luhe Hospital, Capital Medical University, Beijing 101149, China. zhaodong@ccmu.edu.cn.
References
- 1.Chen YC, Chu CM, Yeh CT, Liaw YF. Natural course following the onset of cirrhosis in patients with chronic hepatitis B: a long-term follow-up study. Hepatol Int. 2007;1:267–273. doi: 10.1007/s12072-007-5001-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fattovich G, Bortolotti F, Donato F. Natural history of chronic hepatitis B: special emphasis on disease progression and prognostic factors. J Hepatol. 2008;48:335–352. doi: 10.1016/j.jhep.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 3.Bahardoust M, Mokhtare M, Barati M, Bagheri-Hosseinabadi Z, Karimi Behnagh A, Keyvani H, Agah S. A randomized controlled trial of pegylated interferon-alpha with tenofovir disoproxil fumarate for hepatitis B e antigen-negative chronic hepatitis B: A 48-week follow-up study. J Infect Chemother. 2020;26:1265–1271. doi: 10.1016/j.jiac.2020.07.005. [DOI] [PubMed] [Google Scholar]
- 4.European Association for the Study of the Liver. EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection. J Hepatol. 2017;67:370–398. doi: 10.1016/j.jhep.2017.03.021. [DOI] [PubMed] [Google Scholar]
- 5.Meng Z, Chen Y, Lu M. Advances in Targeting the Innate and Adaptive Immune Systems to Cure Chronic Hepatitis B Virus Infection. Front Immunol. 2019;10:3127. doi: 10.3389/fimmu.2019.03127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guo L, Wang D, Ouyang X, Tang N, Chen X, Zhang Y, Zhu H, Li X. Recent Advances in HBV Reactivation Research. Biomed Res Int. 2018;2018:2931402. doi: 10.1155/2018/2931402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yeo W, Johnson PJ. Diagnosis, prevention and management of hepatitis B virus reactivation during anticancer therapy. Hepatology. 2006;43:209–220. doi: 10.1002/hep.21051. [DOI] [PubMed] [Google Scholar]
- 8.Wands JR, Chura CM, Roll FJ, Maddrey WC. Serial studies of hepatitis-associated antigen and antibody in patients receiving antitumor chemotherapy for myeloproliferative and lymphoproliferative disorders. Gastroenterology. 1975;68:105–112. [PubMed] [Google Scholar]
- 9.Loomba R, Liang TJ. Hepatitis B Reactivation Associated With Immune Suppressive and Biological Modifier Therapies: Current Concepts, Management Strategies, and Future Directions. Gastroenterology. 2017;152:1297–1309. doi: 10.1053/j.gastro.2017.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou K, Terrault N. Management of hepatitis B in special populations. Best Pract Res Clin Gastroenterol. 2017;31:311–320. doi: 10.1016/j.bpg.2017.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chinese Rheumatology Association. [2018 Chinese guideline for the diagnosis and treatment of rheumatoid arthritis] Zhonghua Nei Ke Za Zhi. 2018;57:242–251. doi: 10.3760/cma.j.issn.0578-1426.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 12.Watanabe T, Fukae J, Fukaya S, Sawamukai N, Isobe M, Matsuhashi M, Shimizu M, Akikawa K, Tanimura K, Atsumi T, Koike T. Incidence and risk factors for reactivation from resolved hepatitis B virus in rheumatoid arthritis patients treated with biological disease-modifying antirheumatic drugs. Int J Rheum Dis. 2019;22:574–582. doi: 10.1111/1756-185X.13401. [DOI] [PubMed] [Google Scholar]
- 13.Zhang Z, Deng W, Wu Q, Sun L. Tuberculosis, hepatitis B and herpes zoster in tofacitinib-treated patients with rheumatoid arthritis. Immunotherapy. 2019;11:321–333. doi: 10.2217/imt-2018-0113. [DOI] [PubMed] [Google Scholar]
- 14.Watanabe R, Ishii T, Kobayashi H, Asahina I, Takemori H, Izumiyama T, Oguchi Y, Urata Y, Nishimaki T, Chiba K, Komatsuda A, Chiba N, Miyata M, Takagi M, Kawamura O, Kanno T, Hirabayashi Y, Konta T, Ninomiya Y, Abe Y, Murata Y, Saito Y, Ohira H, Harigae H, Sasaki T. Prevalence of hepatitis B virus infection in patients with rheumatic diseases in Tohoku area: a retrospective multicenter survey. Tohoku J Exp Med. 2014;233:129–133. doi: 10.1620/tjem.233.129. [DOI] [PubMed] [Google Scholar]
- 15.Fujita M, Sugiyama M, Sato Y, Nagashima K, Takahashi S, Mizokami M, Hata A. Hepatitis B virus reactivation in patients with rheumatoid arthritis: Analysis of the National Database of Japan. J Viral Hepat. 2018;25:1312–1320. doi: 10.1111/jvh.12933. [DOI] [PubMed] [Google Scholar]
- 16.Hwang JP, Fisch MJ, Zhang H, Kallen MA, Routbort MJ, Lal LS, Vierling JM, Suarez-Almazor ME. Low rates of hepatitis B virus screening at the onset of chemotherapy. J Oncol Pract. 2012;8:e32–e39. doi: 10.1200/JOP.2011.000450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Visram A, Chan KK, McGee P, Boro J, Hicks LK, Feld JJ. Poor recognition of risk factors for hepatitis B by physicians prescribing immunosuppressive therapy: a call for universal rather than risk-based screening. PLoS One. 2015;10:e0120749. doi: 10.1371/journal.pone.0120749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen MH, Chen MH, Liu CY, Tsai CY, Huang DF, Lin HY, Lee MH, Huang YH. Hepatitis B Virus Reactivation in Rheumatoid Arthritis Patients Undergoing Biologics Treatment. J Infect Dis. 2017;215:566–573. doi: 10.1093/infdis/jiw606. [DOI] [PubMed] [Google Scholar]
- 19.Tien YC, Yen HH, Chiu YM. Incidence and clinical characteristics of hepatitis B virus reactivation in HBsAg-negative/HBcAb-positive patients receiving rituximab for rheumatoid arthritis. Clin Exp Rheumatol. 2017;35:831–836. [PubMed] [Google Scholar]
- 20.Tamori A, Koike T, Goto H, Wakitani S, Tada M, Morikawa H, Enomoto M, Inaba M, Nakatani T, Hino M, Kawada N. Prospective study of reactivation of hepatitis B virus in patients with rheumatoid arthritis who received immunosuppressive therapy: evaluation of both HBsAg-positive and HBsAg-negative cohorts. J Gastroenterol. 2011;46:556–564. doi: 10.1007/s00535-010-0367-5. [DOI] [PubMed] [Google Scholar]
- 21.Chen YM, Yang SS, Chen DY. Risk-stratified management strategies for HBV reactivation in RA patients receiving biological and targeted therapy: A narrative review. J Microbiol Immunol Infect. 2019;52:1–8. doi: 10.1016/j.jmii.2017.10.002. [DOI] [PubMed] [Google Scholar]
- 22.Kuo MH, Tseng CW, Lu MC, Tung CH, Tseng KC, Huang KY, Lee CH, Lai NS. Risk of Hepatitis B Virus Reactivation in Rheumatoid Arthritis Patients Undergoing Tocilizumab-Containing Treatment. Dig Dis Sci. 2021;66:4026–4034. doi: 10.1007/s10620-020-06725-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zingarelli S, Frassi M, Bazzani C, Scarsi M, Puoti M, Airò P. Use of tumor necrosis factor-alpha-blocking agents in hepatitis B virus-positive patients: reports of 3 cases and review of the literature. J Rheumatol. 2009;36:1188–1194. doi: 10.3899/jrheum.081246. [DOI] [PubMed] [Google Scholar]
- 24.Mitra B, Thapa RJ, Guo H, Block TM. Host functions used by hepatitis B virus to complete its life cycle: Implications for developing host-targeting agents to treat chronic hepatitis B. Antiviral Res. 2018;158:185–198. doi: 10.1016/j.antiviral.2018.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brahmania M, Feld J, Arif A, Janssen HL. New therapeutic agents for chronic hepatitis B. Lancet Infect Dis. 2016;16:e10–e21. doi: 10.1016/S1473-3099(15)00436-3. [DOI] [PubMed] [Google Scholar]
- 26.Durantel D. New treatments to reach functional cure: Virological approaches. Best Pract Res Clin Gastroenterol. 2017;31:329–336. doi: 10.1016/j.bpg.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 27.Rehermann B, Lau D, Hoofnagle JH, Chisari FV. Cytotoxic T lymphocyte responsiveness after resolution of chronic hepatitis B virus infection. J Clin Invest. 1996;97:1655–1665. doi: 10.1172/JCI118592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chou CK, Wang LH, Lin HM, Chi CW. Glucocorticoid stimulates hepatitis B viral gene expression in cultured human hepatoma cells. Hepatology. 1992;16:13–18. doi: 10.1002/hep.1840160104. [DOI] [PubMed] [Google Scholar]
- 29.Tan J, Zhou J, Zhao P, Wei J. Prospective study of HBV reactivation risk in rheumatoid arthritis patients who received conventional disease-modifying antirheumatic drugs. Clin Rheumatol. 2012;31:1169–1175. doi: 10.1007/s10067-012-1988-2. [DOI] [PubMed] [Google Scholar]
- 30.Laohapand C, Arromdee E, Tanwandee T. Long-term use of methotrexate does not result in hepatitis B reactivation in rheumatologic patients. Hepatol Int. 2015;9:202–208. doi: 10.1007/s12072-014-9597-6. [DOI] [PubMed] [Google Scholar]
- 31.Mo YQ, Liang AQ, Ma JD, Chen LF, Zheng DH, Schumacher HR, Dai L. Discontinuation of antiviral prophylaxis correlates with high prevalence of hepatitis B virus (HBV) reactivation in rheumatoid arthritis patients with HBV carrier state: a real-world clinical practice. BMC Musculoskelet Disord. 2014;15:449. doi: 10.1186/1471-2474-15-449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hoppe-Seyler K, Sauer P, Lohrey C, Hoppe-Seyler F. The inhibitors of nucleotide biosynthesis leflunomide, FK778, and mycophenolic acid activate hepatitis B virus replication in vitro. Hepatology. 2012;56:9–16. doi: 10.1002/hep.25602. [DOI] [PubMed] [Google Scholar]
- 33.Emery P, Breedveld FC, Lemmel EM, Kaltwasser JP, Dawes PT, Gömör B, Van Den Bosch F, Nordström D, Bjorneboe O, Dahl R, Horslev-Petersen K, Rodriguez De La Serna A, Molloy M, Tikly M, Oed C, Rosenburg R, Loew-Friedrich I. A comparison of the efficacy and safety of leflunomide and methotrexate for the treatment of rheumatoid arthritis. Rheumatology (Oxford) 2000;39:655–665. doi: 10.1093/rheumatology/39.6.655. [DOI] [PubMed] [Google Scholar]
- 34.Perrillo RP, Gish R, Falck-Ytter YT. American Gastroenterological Association Institute technical review on prevention and treatment of hepatitis B virus reactivation during immunosuppressive drug therapy. Gastroenterology. 2015;148:221–244.e3. doi: 10.1053/j.gastro.2014.10.038. [DOI] [PubMed] [Google Scholar]
- 35.Wong GL, Yuen BW, Chan HL, Tse YK, Yip TC, Lam KL, Lui GC, Wong VW. Impact of dose and duration of corticosteroid on the risk of hepatitis flare in patients with chronic hepatitis B. Liver Int. 2019;39:271–279. doi: 10.1111/liv.13953. [DOI] [PubMed] [Google Scholar]
- 36.Wong GL, Wong VW, Yuen BW, Tse YK, Yip TC, Luk HW, Lui GC, Chan HL. Risk of hepatitis B surface antigen seroreversion after corticosteroid treatment in patients with previous hepatitis B virus exposure. J Hepatol. 2020;72:57–66. doi: 10.1016/j.jhep.2019.08.023. [DOI] [PubMed] [Google Scholar]
- 37.Lucifora J, Xia Y, Reisinger F, Zhang K, Stadler D, Cheng X, Sprinzl MF, Koppensteiner H, Makowska Z, Volz T, Remouchamps C, Chou WM, Thasler WE, Hüser N, Durantel D, Liang TJ, Münk C, Heim MH, Browning JL, Dejardin E, Dandri M, Schindler M, Heikenwalder M, Protzer U. Specific and nonhepatotoxic degradation of nuclear hepatitis B virus cccDNA. Science. 2014;343:1221–1228. doi: 10.1126/science.1243462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ryu HH, Lee EY, Shin K, Choi IA, Lee YJ, Yoo B, Park MC, Park YB, Bae SC, Yoo WH, Kim SI, Lee EB, Song YW. Hepatitis B virus reactivation in rheumatoid arthritis and ankylosing spondylitis patients treated with anti-TNFα agents: a retrospective analysis of 49 cases. Clin Rheumatol. 2012;31:931–936. doi: 10.1007/s10067-012-1960-1. [DOI] [PubMed] [Google Scholar]
- 39.Lan JL, Chen YM, Hsieh TY, Chen YH, Hsieh CW, Chen DY, Yang SS. Kinetics of viral loads and risk of hepatitis B virus reactivation in hepatitis B core antibody-positive rheumatoid arthritis patients undergoing anti-tumour necrosis factor alpha therapy. Ann Rheum Dis. 2011;70:1719–1725. doi: 10.1136/ard.2010.148783. [DOI] [PubMed] [Google Scholar]
- 40.Nakamura J, Nagashima T, Nagatani K, Yoshio T, Iwamoto M, Minota S. Reactivation of hepatitis B virus in rheumatoid arthritis patients treated with biological disease-modifying antirheumatic drugs. Int J Rheum Dis. 2016;19:470–475. doi: 10.1111/1756-185X.12359. [DOI] [PubMed] [Google Scholar]
- 41.Chen YM, Huang WN, Wu YD, Lin CT, Chen YH, Chen DY, Hsieh TY. Reactivation of hepatitis B virus infection in patients with rheumatoid arthritis receiving tofacitinib: a real-world study. Ann Rheum Dis. 2018;77:780–782. doi: 10.1136/annrheumdis-2017-211322. [DOI] [PubMed] [Google Scholar]
- 42.Blair HA, Deeks ED. Abatacept: A Review in Rheumatoid Arthritis. Drugs. 2017;77:1221–1233. doi: 10.1007/s40265-017-0775-4. [DOI] [PubMed] [Google Scholar]
- 43.Kim PS, Ho GY, Prete PE, Furst DE. Safety and efficacy of abatacept in eight rheumatoid arthritis patients with chronic hepatitis B. Arthritis Care Res (Hoboken) 2012;64:1265–1268. doi: 10.1002/acr.21654. [DOI] [PubMed] [Google Scholar]
- 44.Padovan M, Filippini M, Tincani A, Lanciano E, Bruschi E, Epis O, Garau P, Mathieu A, Celletti E, Giani L, Tomietto P, Atzeni F, Sarzi Puttini P, Zuliani F, De Vita S, Trotta F, Grilli A, Puoti M, Govoni M. Safety of Abatacept in Rheumatoid Arthritis With Serologic Evidence of Past or Present Hepatitis B Virus Infection. Arthritis Care Res (Hoboken) 2016;68:738–743. doi: 10.1002/acr.22786. [DOI] [PubMed] [Google Scholar]
- 45.Nagashima T, Minota S. Long-term tocilizumab therapy in a patient with rheumatoid arthritis and chronic hepatitis B. Rheumatology (Oxford) 2008;47:1838–1840. doi: 10.1093/rheumatology/ken384. [DOI] [PubMed] [Google Scholar]
- 46.Fukuda W, Hanyu T, Katayama M, Mizuki S, Okada A, Miyata M, Handa Y, Hayashi M, Koyama Y, Arii K, Kitaori T, Hagiyama H, Urushidani Y, Yamasaki T, Ikeno Y, Suzuki T, Omoto A, Sugitani T, Morita S, Inokuma S. Incidence of hepatitis B virus reactivation in patients with resolved infection on immunosuppressive therapy for rheumatic disease: a multicentre, prospective, observational study in Japan. Ann Rheum Dis. 2017;76:1051–1056. doi: 10.1136/annrheumdis-2016-209973. [DOI] [PubMed] [Google Scholar]
- 47.Cheng J, Li JB, Sun QL, Li X. Reactivation of hepatitis B virus after steroid treatment in rheumatic diseases. J Rheumatol. 2011;38:181–182. doi: 10.3899/jrheum.100692. [DOI] [PubMed] [Google Scholar]
- 48.Erratum for the Research Article: "Squalene epoxidase drives NAFLD-induced hepatocellular carcinoma and is a pharmaceutical target" by D. Liu, C. C. Wong, L. Fu, H. Chen, L. Zhao, C. Li, Y. Zhou, Y. Zhang, W. Xu, Y. Yang, B. Wu, G. Cheng, P. B.-S. Lai, N. Wong, J. J. Y. Sung, J. Yu. Sci Transl Med. 2018;10 doi: 10.1126/scitranslmed.aap9840. [DOI] [PubMed] [Google Scholar]
- 49.Cantini F, Boccia S, Goletti D, Iannone F, Leoncini E, Panic N, Prignano F, Gaeta GB. HBV Reactivation in Patients Treated with Antitumor Necrosis Factor-Alpha (TNF-α) Agents for Rheumatic and Dermatologic Conditions: A Systematic Review and Meta-Analysis. Int J Rheumatol. 2014;2014:926836. doi: 10.1155/2014/926836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lin TC, Yoshida K, Tedeschi SK, de Abreu MM, Hashemi N, Solomon DH. Risk of Hepatitis B Virus Reactivation in Patients With Inflammatory Arthritis Receiving Disease-Modifying Antirheumatic Drugs: A Systematic Review and Meta-Analysis. Arthritis Care Res (Hoboken) 2018;70:724–731. doi: 10.1002/acr.23346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tien YC, Yen HH, Li CF, Liu MP, Hsue YT, Hung MH, Chiu YM. Changes in hepatitis B virus surface antibody titer and risk of hepatitis B reactivation in HBsAg-negative/HBcAb-positive patients undergoing biologic therapy for rheumatic diseases: a prospective cohort study. Arthritis Res Ther. 2018;20:246. doi: 10.1186/s13075-018-1748-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schwaneck EC, Krone M, Kreissl-Kemmer S, Weißbrich B, Weiss J, Tony HP, Gadeholt O, Schmalzing M, Geier A. Management of anti-HBc-positive patients with rheumatic diseases treated with disease-modifying antirheumatic drugs-a single-center analysis of 2054 patients. Clin Rheumatol. 2018;37:2963–2970. doi: 10.1007/s10067-018-4295-8. [DOI] [PubMed] [Google Scholar]
- 53.Ding F, Miao XL, Li YX, Dai JF, Yu HG. Mutations in the S gene and in the overlapping reverse transcriptase region in chronic hepatitis B Chinese patients with coexistence of HBsAg and anti-HBs. Braz J Infect Dis. 2016;20:1–7. doi: 10.1016/j.bjid.2015.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Golsaz Shirazi F, Amiri MM, Mohammadi H, Bayat AA, Roohi A, Khoshnoodi J, Zarnani AH, Jeddi-Tehrani M, Kardar GA, Shokri F. Construction and expression of hepatitis B surface antigen escape variants within the "a" determinant by site directed mutagenesis. Iran J Immunol. 2013;10:127–138. [PubMed] [Google Scholar]
- 55.Koutsianas C, Thomas K, Vassilopoulos D. Hepatitis B Reactivation in Rheumatic Diseases: Screening and Prevention. Rheum Dis Clin North Am. 2017;43:133–149. doi: 10.1016/j.rdc.2016.09.012. [DOI] [PubMed] [Google Scholar]
- 56.Zhang MY, Zhu GQ, Zheng JN, Cheng Z, Van Poucke S, Shi KQ, Huang HH, Chen FY, Zheng MH. Nucleos(t)ide analogues for preventing HBV reactivation in immunosuppressed patients with hematological malignancies: a network meta-analysis. Expert Rev Anti Infect Ther. 2017;15:503–513. doi: 10.1080/14787210.2017.1309291. [DOI] [PubMed] [Google Scholar]
- 57.Hwang JP, Lok AS. Management of patients with hepatitis B who require immunosuppressive therapy. Nat Rev Gastroenterol Hepatol. 2014;11:209–219. doi: 10.1038/nrgastro.2013.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chinese Society of Hepatology Chinese Society of Infectious Diseases of CMA. The guideline of prevention and treatment for chronic hepatitis B (2015 version) Zhonghua Ganzangbing Zazhi . 2015;23:888–905. doi: 10.3760/cma.j.issn.1007-3418.2015.12.002. [DOI] [PubMed] [Google Scholar]