Abstract
BACKGROUND
Laparoscopic cervical cerclage is performed for patients with abnormal cervical anatomy and/or transvaginal cervical cerclage failure. However, the method of removing the stitches to allow labour induction remains controversial. According to published literature, stitches are removed through laparoscopic or transvaginal methods. Herein, we report, for the first time, a case of a patient who had undergone laparoscopic cerclage, and then underwent removal of stitches by laparotomy and labour induction in the third trimester of pregnancy.
CASE SUMMARY
A patient who underwent laparoscopic cervical cerclage due to cervical insufficiency became pregnant naturally following the operation. At 31 wk of pregnancy, severe foetal malformations were found. To successfully induce labour, cerclage stitches were removed via laparotomy, and rivanol was injected directly into the uterus. Following successful induction of labour, the patient delivered a dead foetus.
CONCLUSION
This report provides a reliable scheme of removing cerclage stitches for patients who have undergone laparoscopic cerclage but experience severe foetal malformations.
Keywords: Laparoscopic cerclage, Pregnancy, Induced labour, Stitch removal, Case report
Core Tip: To the best of our knowledge, this is the first report of a case in which a patient, who had undergone laparoscopic cerclage, underwent removal of cerclage stitches via laparotomy and labour induction in the third trimester of pregnancy. This report highlights the advantages of this technique over other available methods. Moreover, this report presents the rarity of foetal abnormality or death in the third trimester in a woman who had laparoscopic cervical cerclage.
INTRODUCTION
Cervical incompetence is the main cause of late-term abortion and premature delivery, for which cervical cerclage is the primary treatment[1,2]. Cervical cerclage is a surgical intervention involving the placement of stitches around the uterine cervix to prevent the shortening and opening of the cervix. Transvaginal and laparoscopic cerclage are the main methods. Transvaginal cerclage is the most widely used[3], while laparoscopic cerclage is used for patients with abnormal cervical anatomy and/or transvaginal cerclage failure. Laparoscopic cerclage is primarily used before or during the early stages of pregnancy, and the stitches are usually removed during caesarean section[4]. However, for patients with foetal abnormalities or second- or third-trimester foetal death, the method of removing the stitches to allow for labour induction remains controversial. In all previous cases of laparoscopic cerclage, labour induction was implemented in the second trimester, and cerclage stitches were removed either laparoscopically or transvaginally[5-10].
Herein, we report, for the first time, a case in which the patient, who had undergone laparoscopic cerclage, underwent removal of stitches by laparotomy and labour induction in the third trimester of pregnancy.
CASE PRESENTATION
Imaging examinations
Foetal three-dimensional ultrasonography showed ‘tulip’-like external genitalia, external penis and scrotum transposition, single umbilical artery, disappearance of umbilical blood flow in the diastolic period, and foetal intrauterine growth restriction.
Laboratory examinations
No abnormal laboratory examinations.
Physical examination
No abnormal physical examination.
Personal and family history
No special personal and family history.
History of past illness
The patient experienced two miscarriages in the second trimester of pregnancy, one of which was caused by transvaginal cervical cerclage failure. Before the present pregnancy, laparoscopic cervical cerclage was performed under general anaesthesia, and the isthmus of the cervix was ligated with Mersilene tapes (RS22, Ethicon, NJ, United States).
History of present illness
During the routine obstetric examination, severe foetal malformations were identified through three-dimensional ultrasonography; thus, the patient requested for induced labour.
Chief complaints
A 31-year-old woman (gravida 4, abortus 3) was admitted for labour induction at 31 wk of gestation because of severe foetal malformations.
FINAL DIAGNOSIS
The final diagnosis was foetal malformations.
TREATMENT
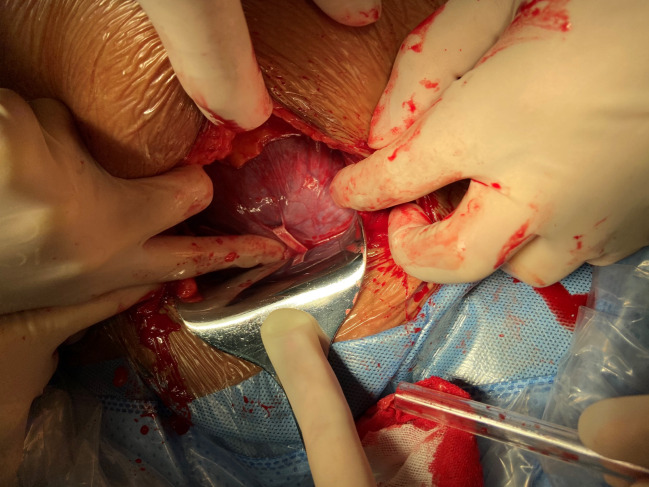
After relevant examinations, cerclage stitches were removed, and rivanol amniocentesis was performed for labour induction via laparotomy under combined spinal-epidural anaesthesia. A mini horizontal incision was made in the middle of the abdomen, and the cerclage stitches were separated carefully from the cervix and surrounding tissue to which they were closely adhered (Figure 1). The stitches were clipped and removed. Amniocentesis was then performed, and 0.2 g rivanol was injected into the uterine cavity. Finally, the abdominal incision was sutured routinely.
Figure 1.
A mini horizontal incision was made and the cerclage stitches were exposed.
OUTCOME AND FOLLOW-UP
Two days following labour induction, the patient delivered a dead foetus and was discharged 2 days later.
DISCUSSION
Laparoscopic cerclage is a type of trans-abdominal cervical cerclage. The isthmus of the cervix is sutured under laparoscopic guidance before or during early pregnancy. Compared with transvaginal cerclage, laparoscopic cerclage causes less trauma and has a lower risk of infection[11]. In addition, laparoscopic cerclage stitches are placed closer to the internal cervix, which more closely conforms to the normal physiological anatomy. Laparoscopic cerclage is effective not only in reducing the risk of cervical tear and infection but also in maintaining the expansion of the amniotic cavity[12,13]. In clinical practice, several obstetricians have performed this technique in women with cervical defects to extend the gestational age of the foetus, as well as in cases where transvaginal cerclage was not possible and in cases with repeated transvaginal cerclage failure.
Laparoscopic cerclage stitches can be removed by laparotomic, laparoscopic, and transvaginal approaches. For pregnant women with normal foetuses at full term or near term, caesarean section is commonly performed for delivery, and cerclage stitches were removed during the procedure[14]. For pregnancies that should be terminated because of foetal abnormalities or third-trimester foetal death, the methods of removing cerclage stitches and inducing labour remain controversial. Burger et al[6] reported three cases of removing transvaginal cerclage stitches in the second trimester. Carter et al[7-10] and other authors have reported laparoscopic removal of cerclage stitches in pregnancies terminated due to premature rupture of membranes or foetal abnormalities in the second trimester (Table 1). However, in the present study, the patient was already at 31 wk of pregnancy. She was informed of the risks of labour induction and caesarean delivery. Subsequently, she requested for induction of labour, but not caesarean section, to maintain the integrity of the uterus for future pregnancy. Therefore, we considered removing the stitches for a vaginal delivery. The enlarged uterus limited the surgical space in the abdominal cavity; therefore, laparoscopic removal of the stitches was not feasible. In addition, given the abundant pelvic blood supply during pregnancy, the stitches may be adhered to the surrounding tissue, and transvaginal stitch removal may cause injury to the surrounding tissue or intra-abdominal bleeding. Therefore, stitches were removed by laparotomy and rivanol was injected directly into the uterus to induce labour.
Table 1.
Cases of inducing labour in the second trimester after laparoscopic cerclage
|
Author
|
Gestational age (wk)
|
Reason of removal
|
Method of removal
|
| Nicole B. Burger[6] | 16 + 5 | Rupture of membranes | Posterior colpotomy |
| 19 | Intrauterine infection | Posterior colpotomy | |
| 23 + 3 | Intrauterine infection | Anterior colpotomy | |
| James F. Carter[7,8] | 17 | Feotal death | Laparoscope |
| 19 | Rupture of membranes | Laparoscope | |
| S E Scarantino[9] | 16 | Rupture of membranes | Laparoscope |
| Mohammed Agdi[10] | 19 | Oligohydramnios | Laparoscope |
To the best of our knowledge, no study has reported the removal of laparoscopic cerclage stitches via laparotomy simultaneously with labour induction in the third trimester. The method of terminating a pregnancy is usually restricted by trans-abdominal stitches, especially in cases with premature rupture of the membrane or foetal abnormality in the second or third trimester. Obstetricians should comprehensively assess the methods of removing cerclage stitches to reduce the risk of injury to the patients; this indicates the need to develop new laparoscopic cerclage techniques. Sukur and Saridogan[15] sutured cerclage stitches behind the cervical isthmus, allowing the removal of these stitches through the vagina. Shaltout et al[16] designed an improved laparoscopic cerclage, which involved opening the peritoneum folding between the uterus and the bladder, puncturing the needle through the posterior fornix of the vagina, and placing the suture knot in the posterior fornix. Among the 15 patients who underwent this new surgical method, 12 underwent induced vaginal delivery after the stitches were removed through the vagina. Wang et al[17] performed ‘vaginal removal’ of laparoscopic cervical cerclage without opening the peritoneum folding, through which the cerclage stitches can be sutured to the posterior fornix of the vagina. Procedures were performed on 13 patients, of which four underwent vaginal delivery after 36 wk of pregnancy. The improved laparoscopic cerclage enabled the removal of the stitches through the vagina and avoided potential traumas caused by transabdominal surgery.
CONCLUSION
Foetal abnormality or death in the third trimester of pregnancy in patients who have undergone laparoscopic cerclage is extremely rare. In the present case, cerclage stitches were removed by laparotomy and vaginal delivery was possible following successful induction of labour, which maintained the integrity of the patient’s uterus. This is an alternative method for patients undergoing induced labour in the third trimester. In addition, obstetricians should improve prenatal examinations of patients who have undergone laparoscopic cervical cerclage during pregnancy to detect pregnancy-related complications as early as possible and thereby avoid adverse events. More laparoscopic cerclage techniques should be developed, and existing techniques should be improved to increase the number of options available for removal of stitches.
Footnotes
Informed consent statement: Informed written consent was obtained from the patient for publication of this report.
Conflict-of-interest statement: The authors declare that they have no conflict of interest.
CARE Checklist (2016) statement: The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: May 22, 2021
First decision: October 18, 2021
Article in press: November 24, 2021
Specialty type: Obstetrics and gynecology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: De Carolis S, Tolunay HE S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
Contributor Information
Xin-Ni Na, Department of Obstetrics and Gynecology, Shengjing Hospital of China Medical University, Shenyang 110004, Liaoning Province, China.
Ben-Shuo Cai, Department of Obstetrics and Gynecology, Shengjing Hospital of China Medical University, Shenyang 110004, Liaoning Province, China. caibenshuo_sj@vip.163.com.
References
- 1.Korb D, Marzouk P, Deu J, Oury JF, Sibony O. Effectiveness of elective cervical cerclage according to obstetric history. J Gynecol Obstet Hum Reprod. 2017;46:53–59. doi: 10.1016/j.jgyn.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 2.Černohorská P, Vitásková H, Kokrdová Z, Hájek Z, Koucký M, Pařízek A. Cervical cerclage - history and contemporary use. Ceska Gynekol. 2019;84:55–60. [PubMed] [Google Scholar]
- 3.Sun X, Ding XP, Shi CY, Yang HX, Jin YZ. Analysis of clinical effect of McDonald cervical cerclage and the related risk factors. Zhonghua Fu Chan Ke Za Zhi. 2016;51:87–91. doi: 10.3760/cma.j.issn.0529-567X.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Clark NV, Einarsson JI. Laparoscopic abdominal cerclage: a highly effective option for refractory cervical insufficiency. Fertil Steril. 2020;113:717–722. doi: 10.1016/j.fertnstert.2020.02.007. [DOI] [PubMed] [Google Scholar]
- 5.Marchand GJ, Masoud AT, Galitsky A, Sainz K, Azadi A, Ware K, Vallejo J, Anderson S, King A, Ruther S, Brazil G, Cieminski K, Hopewell S, Syed M. Complications of Laparoscopic and Transabdominal Cerclage in Patients with Cervical Insufficiency: A Systematic Review and Meta-analysis. J Minim Invasive Gynecol . 2021;28:759–768. doi: 10.1016/j.jmig.2020.11.014. [DOI] [PubMed] [Google Scholar]
- 6.Burger NB, van 't Hof EM, Huirne JAF. Removal of an Abdominal Cerclage by Colpotomy: A Novel and Minimally Invasive Technique. J Minim Invasive Gynecol. 2020;27:1636–1639. doi: 10.1016/j.jmig.2020.05.022. [DOI] [PubMed] [Google Scholar]
- 7.Carter JF, Savage A, Soper DE. Laparoscopic removal of abdominal cerclage at 19 wk' gestation. JSLS. 2013;17:161–163. doi: 10.4293/108680812X13517013317194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carter JF, Soper DE. Laparoscopic removal of abdominal cerclage. JSLS. 2007;11:375–377. [PMC free article] [PubMed] [Google Scholar]
- 9.Scarantino SE, Reilly JG, Moretti ML, Pillari VT. Laparoscopic removal of a transabdominal cervical cerclage. Am J Obstet Gynecol. 2000;182:1086–1088. doi: 10.1067/mob.2000.105404. [DOI] [PubMed] [Google Scholar]
- 10.Agdi M, Tulandi T. Placement and removal of abdominal cerclage by laparoscopy. Reprod Biomed Online. 2008;16:308–310. doi: 10.1016/s1472-6483(10)60590-1. [DOI] [PubMed] [Google Scholar]
- 11.Chen Y, Liu H, Gu J, Yao S. Therapeutic effect and safety of laparoscopic cervical cerclage for treatment of cervical insufficiency in first trimester or non-pregnant phase. Int J Clin Exp Med. 2015;8:7710–7718. [PMC free article] [PubMed] [Google Scholar]
- 12.Xia E, Huang X. Laparoscopic Cerclage for Prevention of Recurrent Pregnancy Loss Due to Cervical Incompetence. J Minim Invasive Gynecol. 2015;22:S201. doi: 10.1016/j.jmig.2015.08.727. [DOI] [PubMed] [Google Scholar]
- 13.Tian S, Zhao S, Hu Y. Comparison of laparoscopic abdominal cerclage and transvaginal cerclage for the treatment of cervical insufficiency: a retrospective study. Arch Gynecol Obstet . 2021;303:1017–1023. doi: 10.1007/s00404-020-05893-9. [DOI] [PubMed] [Google Scholar]
- 14.Vigueras Smith A, Cabrera R, Zomer MT, Ribeiro R, Talledo R, Kondo W. Laparoscopic Transabdominal Cerclage for Cervical Incompetence: A Feasible and Effective Treatment in 10 Steps. J Minim Invasive Gynecol. 2020;27:1025–1026. doi: 10.1016/j.jmig.2019.10.019. [DOI] [PubMed] [Google Scholar]
- 15.Şükür YE, Sarıdoğan E. Tips and tricks for laparoscopic interval transabdominal cervical cerclage; a simplified technique. J Turk Ger Gynecol Assoc. 2019;20:272–274. doi: 10.4274/jtgga.galenos.2019.2019.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shaltout MF, Maged AM, Elsherbini MM, Elkomy RO. Laparoscopic transabdominal cerclage: new approach. J Matern Fetal Neonatal Med. 2017;30:600–604. doi: 10.1080/14767058.2016.1181165. [DOI] [PubMed] [Google Scholar]
- 17.Wang YY, Duan H, Zhang XN, Wang S, Gao L. A Novel Cerclage Insertion: Modified Laparoscopic Transabdominal Cervical Cerclage with Transvaginal Removing (MLTCC-TR) J Minim Invasive Gynecol. 2020;27:1300–1307. doi: 10.1016/j.jmig.2019.09.774. [DOI] [PubMed] [Google Scholar]