Abstract
Introduction: The best way to titrate the positive end-expiratory pressure (PEEP) in patients suffering from acute respiratory distress syndrome is still matter of debate. Electrical impedance tomography (EIT) is a non-invasive technique that could guide PEEP setting based on an optimized ventilation homogeneity.
Methods: For this study, we enrolled the patients with 2019 coronavirus disease (COVID-19)-related acute respiratory distress syndrome (ARDS), who required mechanical ventilation and were admitted to the ICU in March 2021. Patients were monitored by an esophageal catheter and a 32-electrode EIT device. Within 48 h after the start of mechanical ventilation, different levels of PEEP were applied based upon PEEP/FiO2 tables, positive end-expiratory transpulmonary (PL)/ FiO2 table, and EIT. Respiratory mechanics variables were recorded.
Results: Seventeen patients were enrolled. PEEP values derived from EIT (PEEPEIT) were different from those based upon other techniques and has poor in-between agreement. The PEEPEIT was associated with lower plateau pressure, mechanical power, transpulmonary pressures, and with a higher static compliance (Crs) and homogeneity of ventilation.
Conclusion: Personalized PEEP setting derived from EIT may help to achieve a more homogenous distribution of ventilation. Whether this approach may translate in outcome improvement remains to be investigated.
Keywords: ARDS, COVID-19, PEEP, electrical tomography impedance, mechanical ventilation
Introduction
Despite progresses in acute respiratory distress syndrome (ARDS) management, the best way to titrate a positive end-expiratory pressure (PEEP) is not straightforward (1). The “right” PEEP should allow for optimized lung recruitment while minimizing over-distention. To this aim, clinicians can use PEEP-FiO2 tables (2), transpulmonary pressure (PL) (3), or electrical impedance tomography (EIT).
The transpulmonary pressure is measured using an esophageal balloon catheter that approximates the pleural pressure. Using this technique, PEEP has to be set to maintain the end-expiratory PL above zero to avoid collapse of dependent dorsal lung regions, and the end-inspiratory PL below 20–25 cmH2O to decrease the risk of overdistension of non-dependent regions.
Electrical impedance tomography (EIT) is a non-invasive technique giving dynamic information on regional ventilation that can be embarked in modern ventilators. Regional hypoventilated lung units (“Silent spaces”) correspond to both collapsed areas in the dependent territories, and distended areas in the non-dependent regions. Using this technique, PEEP is set to minimize the percentage of total silent spaces.
We describe a case series of patients suffering from 2019 coronavirus disease (COVID-19)-related ARDS in whom we compared PEEP settings based on PEEP/FiO2 tables, PL/ FiO2 table, and EIT.
Methods
In March 2021, we enrolled some mechanically ventilated patients who were admitted to our Intensive Care Unit (ICU) because of a COVID-19-related moderate-to-severe ARDS. The diagnosis of COVID-19 relied upon positive result on polymerase chain reaction of sputum or nasal swab. The Ethic Committee of our University Hospital approved this study with a waiver of informed consent because of the use of routine procedures, as well as the use of de-identified data.
All patients were ventilated in volume control mode [tidal volume (Vt): 6–7 ml/kg ideal body weight (IBW)], with FiO2 set to achieve peripheral oxygen saturation (SpO2) between 92 and 95%, and respiratory rate (RR) set to reach PaCO2 between 38 and 45 mmHg. Transpulmonary pressures were measured with the use of an esophageal balloon catheter (Nutrivent; Sidam, Mirandola, Italy) after its correct positioning has been verified through passive chest compression during occlusion. As part of our routine monitoring, patients were also equipped with a 32-electrode soft-textile EIT belt (Sentec; Therwil, Switzerland), which was directly connected to the ventilator (ELISA 800 VIT, Lowenstein Medical; Kronberg, Germany). Some maneuvers were performed in supine position after 24–48 h of mechanical ventilation while the patients were still sedated (midazolam and sufentanyl) and paralyzed (cisatracurium or atracurium). Respiratory mechanics variables were recorded after 10 min at different PEEP levels while all the other parameters (FiO2, Vt, RR, flow rates, etc.) remained unchanged.
Positive end-expiratory pressure (PEEP) was first set according to the lower, then, to the higher PEEP/FiO2 ALVEOLI table (2). Next, PEEP as based upon end-expiratory PL/FiO2 table, was applied (3). Finally, an automated decremental PEEP trial was performed under EIT monitoring (Best-PEEP-Tool, Lowenstein Medical): PEEP was set at 24 cmH2O (corresponding to the maximum PEEP in the PEEP/FiO2 table) and was reduced by 2 cmH2O every 10 inspirations until 6 cm H2O, with a 3-s end-expiratory hold between decremental steps. For each PEEP values, percentages of relatively collapsed and overdistended lung regions were given by the EIT, and the “best” PEEP (PEEPEIT) was considered as the lowest level associated with the lowest total percentage of the lung silent spaces (collapsed + distended).
Data are presented as median (interquartile range) and are compared using Wilcoxon signed-rank test. Bias and limits of agreement between different approaches were calculated with the Bland-Altman approach. Statistical analyses were performed by GraphPad software (La Jolla, CA, USA) with two-tailed p < 0.05 deemed as significant.
Results
Seventeen patients (15 men, 2 women) were enrolled. Median age was 65 (62–71) years, and body mass index was 31.1 (28.5–33.0). The ARDS was severe in 6 and moderate in 11 patients, while the PaO2/FiO2 was 136 (103–155), Vt 6.6 (6.2–7.0) mL/kg IBW, and RR 24 (22–27), respectively. Twelve patients were under high-flow oxygen therapy for a median of 1 (1, 2) day before intubation. All patients, except for one, were discharged alive.
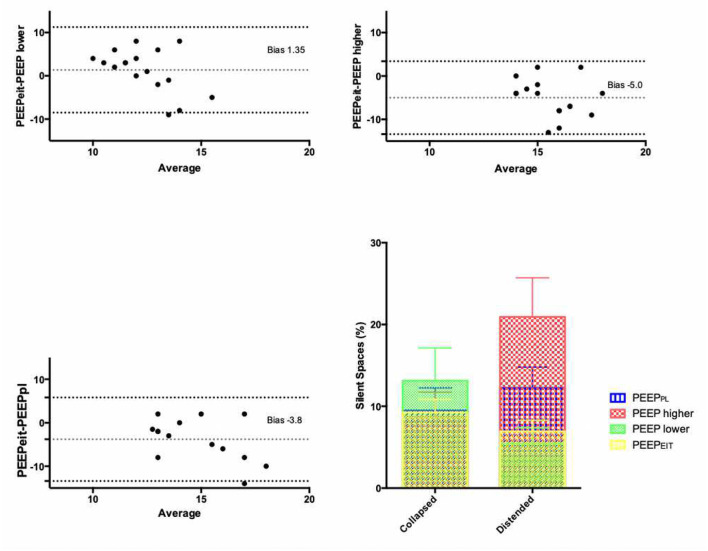
Positive end-expiratory pressure derived from EIT (PEEPEIT), corresponding to the lowest level of PEEP achieving the lowest percentage of total silent spaces (distended + collapsed), was significantly different from the other PEEP values. It was higher than the lower PEEP/FiO2 table, and lower than the higher PEEP/FiO2 or PL/FiO2 tables (Table 1). The Bland-Altman analysis showed that PEEPEIT was 1.3 cm H2O higher than the lower PEEP/FiO2 table with limits of agreement from −8.5 to 11.2 cm H2O. By contrast, PEEPEIT was 5 and 4 cm H2O lower, respectively, than higher PEEP/FiO2 and PL/FiO2 tables, with again wide limits of agreement (Figure 1).
Table 1.
Effect of positive end-expiratory pressure (PEEP) settings on respiratory mechanics.
| Variable | Lower PaO2/FiO2 table | Higher PaO2/FiO2 table | PL/FiO2 table | PEEPEIT |
|---|---|---|---|---|
| PEEP (cm H2O) | 10 (10 to 14) | 17 (16 to 20) | 15 (14 to 20) | 13 (12 to 14)*# |
| PPLAT (cm H2O) | 23 (20 to 26) | 33 (28 to 38) | 29 (24 to 37) | 25 (22 to 27)# |
| Driving Pressure (cm H2O) | 12 (10 to 14) | 14 (12 to 18) | 13 (11 to 16) | 12 (11 to 13) |
| CRS (mL/cm H2O) | 39 (34 to 48) | 30 (24 to 37) | 35 (26 to 43) | 38 (34 to 45)# |
| Mechanical Power (J/min) | 25.1 (22.7 to 34.3) | 34.4 (28.0 to 43.6) | 34.1 (26.0 to 40.7) | 28.4 (24.4 to 32.0)# |
| Inspiratory Transpulmonary pressure (cm H2O) | 6.6 (4.3 to 13.5) | 17.5 (9.9 to 21.6) | 14.7 (9.4 to 18.7) | 11.5 (6.4 to 14.3)# |
| Expiratory Transpulmonary pressure (cm H2O) | −0.3 (−2.8 to 3.6) | 5.0 (2.0 to 8.0) | 4.0 (1.5 to 6.5) | 1.3 (0.1 to 2.0)# |
| Silent spaces (%) | 18 (10 to 26) | 30 (13 to 48) | 23 (17 to 35) | 16 (9 to 23)# |
p < 0.05 PEEPEIT vs. Lower PaO2/FiO2 table.
p < 0.05 PEEPEIT vs. Higher PaO2/FiO2 and PL/FiO2 tables.
Figure 1.
Bland-Altman plots evaluating agreement between PEEP derived from EIT (PEEPEIT) and positive end-expiratory pressure (PEEP) values derived from lower and higher PEEP/FiO2 tables and PL/FiO2 table. Dotted lines: bias and its 95% confidence interval. Lower right panel: percentages of collapsed and distended lung regions measured by electrical impedance tomography (EIT) under different PEEP settings. Percentage of collapse was lower with PEEPEIT than with lower PEEP/FiO2 table (p = 0.04), while percentage of distended areas was reduced as compared to higher PEEP/FiO2 and PL/FiO2 tables (p < 0.01).
In terms of respiratory mechanics, PEEPEIT was associated with lower plateau pressure, mechanical power, transpulmonary pressures, and with a higher static compliance (Crs) than higher PEEP/FiO2 or PL/FiO2 tables (Table 1). Driving pressures were not significantly different.
A better distribution of ventilation was achieved with PEEPEIT: lung collapse was lower with PEEPEIT than with lower PEEP/FiO2 table (9 vs. 13%; p = 0.04), while lung distension was reduced as compared to higher PEEP/FiO2 and PL/FiO2 tables (6 vs. 20 and 13%, respectively; p < 0.01) (Figure 1).
Discussion
Personalized PEEP guided by EIT, with the aim to minimize relative alveolar distention and collapse, was different than PEEP based upon PEEP/FiO2 or PL/FiO2 tables. Although in terms of respiratory mechanics, PEEPEIT did not differ from lower PEEP/FiO2 table. There were very important individual variations as witnessed by the wide range of limit agreement in Bland-Altman analyses. Therefore, each patient exhibited different lung properties that cannot be ascertained by using global mechanics parameter such as driving or transpulmonary pressures, compliance, or pressure-volume curves. This may explain the negative results of important clinical trials, which compared low vs. high PEEP in ARDS patients (2, 4).
Several other recent studies evaluated EIT-guided PEEP titration. Van der Zee et al. (5) and Sella et al. (6) have compared PEEPEIT vs. PEEP/FiO2 tables in each of the 15 cases of COVID-19-related ARDS patients. In both studies, PEEP values differed with important individual variations. Interestingly, PEEPEIT was lower (12 cmH2O) in the Sella study than in the Van der Zee's (21 cm H2O). This highlights the huge variability between patients with ARDS, depending on weight, age, sex, or duration of mechanical ventilation.
When comparing PEEPEIT and PL/FiO2 table, Scaramuzzo et al. (7), in 20 patients under non-COVID-19 ARDS, found no correlation between the values given by the 2 techniques. As in our study, PEEPEIT achieved a more homogenous distribution of ventilation.
Our work has several limitations. First, we only included patients with COVID-19. Whether these patients behaved similarly to those suffering from non-COVID-19 ARDS in terms of respiratory mechanics is still matter of debate. Second, most of our patients were over-weighted. Hence, this may have contributed to the low agreement between techniques. Finally, only 17 patients have been enrolled, precluding any generalization. However, each patient was its own control, and we just wanted to underline the poor agreement between routinely used techniques at the patient level.
The use of EIT allows for a personalized PEEP titration with the aim to minimize the total amount of pulmonary silent spaces. Whether this approach could translate in outcome improvement remains to be investigated.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Comité d'éthique du CHRU de Nancy. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
SG designed the study, collected and analyzed data, and wrote the manuscript. MC, GC, and AC collected and analyzed data. All authors read and approved the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Sahetya SK, Golagher EC, Brower RG. Fifty years of research inn ARDS. Setting positive end-expiratory pressure in acute respiratory distress syndrome. Am J Respir Crit Care Med. (2017) 195:1429–38. 10.1164/rccm.201610-2035CI [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The The National Heart Lung and Blood Institute ARDS Clinical Trials Network . Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. (2004). 351:327–36. 10.1056/NEJMoa032193 [DOI] [PubMed] [Google Scholar]
- 3.Beitler JR, Sarge T, Banner-Goodspeed VM, Gong MN, Cook D, Novack V, et al. EPVent-2 study group: effect of titrating positive end-expiratory pressure (PEEP) with an esophageal pressure-guided strategy vs an empirical high PEEP-FiO2 strategy on death and days free from mechanical ventilation among patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. (2019) 321:846–57. 10.1001/jama.2019.0555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mercat A, Richard JC, Vielle B, Jaber S, Osman D, Diehl JL, et al. End-expiratory pressure (Express) study group. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. (2008) 299:646–55. 10.1001/jama.299.6.646 [DOI] [PubMed] [Google Scholar]
- 5.van der Zee P, Somhorst P, Endemann H, Gommers D. Electrical impedance tomography for positive end-expiratory pressure titration in COVID-19 related ARDS. Am J Respir Crit Care Med. (2020) 202:280–4. 10.1164/rccm.202003-0816LE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sella N, Zarantonello F, Andreatta G, Gagliardi V, Boscolo A, Navalesi P. Positive end-expiratory pressure titration in COVID-19 acute respiratory failure: electrical impedance tomography vs. PEEP/FiO2 tables. Crit Care. (2020) 24:540. 10.1186/s13054-020-03242-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scaramuzzo G, Spadaro S, Dalla Corte F, Waldmann AD, Böhm SH, Ragazzi R, et al. Personalized positive end-expiratory pressure in acute respiratory distress syndrome: Comparison between optimal distribution of regional ventilation and positive transpulmonary pressure. Crit Care Med. (2020) 48:1148–56. 10.1097/CCM.0000000000004439 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.