Abstract
Although music is predominantly utilized for religious, enjoyment or entertainment purposes, it is gradually emerging as a promising non-pharmacological intervention for improving health outcomes in both healthy and diseased populations, especially in those with cardiovascular diseases. As such, music of various genres and types has been postulated to possess features that stimulate or inhibit the autonomic nervous system, which leads to variable effects on cardiovascular function. However, music intervention has not been adequately explored as a cardiovascular therapeutic modality due to the lack of extensive studies with quality methodology. Thus, the aim of this systematic review is to explore the available literature on the effect of music on the cardiovascular system, discuss the limitations of current research, and suggest future directions in this field.
Keywords: Music, Cardiovascular system, Cardiac rehabilitation, Heart rate variability, Blood pressure
Introduction
Music is a universal art form that is pervasive in every society globally and has mainly been a cultural tool used for entertainment and religious purposes. However, music does have its historical basis in medicine, dating back to the 6th century at least. Pythagoras, an ancient Greek philosopher, used music to treat bodily and psychological ailments. He proposed that by listening to music, one could comprehend and retrace the outer “physical” harmony of the universe, which would lead to a state of inner “mental” harmony, thus reestablishing balance in the body and helping to cure mental disorders [1]. He was thought to be the first person to prescribe music as medicine. Around 400 BC, Hippocrates, the father of clinical medicine, was known to play music for his patients with mental illness [2]. As far back as the pale-olithic ages, music was adopted for therapeutic purposes due to the belief that music would have positive effects on body systems, including the cardiovascular system [3]. These music therapies were mostly based on theory, rather than pragmatic evidence. The early 20th century advocated for the validation and implementation of music for therapeutic purposes using the same methodological rigor as any other clinical practice in modern medicine [4]. In 1914, the American Medical Association first acknowledged the possible benefits of music in hospital treatments through Dr. Evan O’Neill Kane’s letter in the Journal of the American Medical Association, documenting successful phonograph use in the operating room to calm patients before general and local anesthesia [5]. In 1918, Columbia University introduced the first course on music therapy, entitled “Musicotherapy” [6]. Because of its low cost, accessibility, ease of use, and minimal risk, music has the potential to be a universal mode of therapy. While music therapy has the potential to benefit all ages and a variety of disease processes, this review focuses on the cardiovascular system. It is thought that music may exert cardiovascular benefits through complex interactions between respiratory activity and autonomic cardiovascular control.
Heart rate variability (HRV) is the beat-to-beat variation in heart rate. HRV includes respiratory sinus arrhythmia (RSA), a normal phenomenon relating to the acceleration of heart rate during inhalation and the deceleration during exhalation. The HRV reflects the complex interplay of the sympathetic and parasympathetic branches of the autonomic nervous system, and measurements of HRV have proved to be powerful predictors of cardiac morbidity and mortality [7, 8]. Several studies we describe here assess changes in HRV as an outcome measure. Additional studies evaluate the impact of music on the electrocardiogram (ECG), blood pressure (BP), heart rate (HR) respiratory rate (RR), ventilatory efficiency, exercise performance, cortisol levels, and endothelial function. We will consider the subjects and outcomes studied, the types of music interventions and modalities (music listening, singing, instrument-playing) utilized, entrainment (synchronization of music tempo to biological variables such as heart rate), and the overall quality of the currently available evidence.
The aim of this systematic review is to explore the available literature on the effect of music on the cardiovascular system, discuss the limitations of current research, and suggest future directions in this field.
Methods
Search strategy
A search was conducted via the PubMed database for both randomized controlled trials and observational studies (including case-control and cohort studies) from January 1st, 1980 to December 31st, 2020. Only articles in English were considered. The key search phrase ‘music and cardiovascular’ was used to conduct the article search. Studies were required to include at least one music intervention and outcomes related to the cardiovascular system or cardiovascular diseases.
Study selection and inclusion criteria
Full-text, peer-reviewed published articles in scientific journals, which included music reception (listening), or performance (singing and playing instruments) interventions were included in this review. Studies in persons or populations of adult ages, conducted in individuals or groups, both in healthy and diseased populations, were included. Each study was required to evaluate at least one key biomarker or outcome related to cardiovascular physiology or health. This review includes music interventions in both healthy subjects and those with specific cardiovascular diseases (e.g., heart failure, myocardial infarction, hypertension, etc.). Articles were excluded if they were abstracts, supplements, reports, opinion articles, letters, reviews, commentaries, magazine articles, book chapters and presentations. However, we do incorporate and highlight major findings from previously published review articles related to this topic in the Discussion.
Article screening process
Our key search phrase through the PubMed database yielded 530 articles. This number was reduced to 149 full-text articles after the removal of 381 abstract-only publications. Further review led to the removal of 123 articles due to the following: unrelated topic (n = 13), review or meta-analysis (n = 16), lack of music intervention (n = 70), no cardiovascular outcome assessed (n = 6), pediatric study population (n = 1), non-English text only (n = 3), animal study (n = 3), supplement/letter or abstract-only (n = 9), and duplicates (n = 2). A total of 26 articles were included in this review (Figure 1).
Fig. 1.
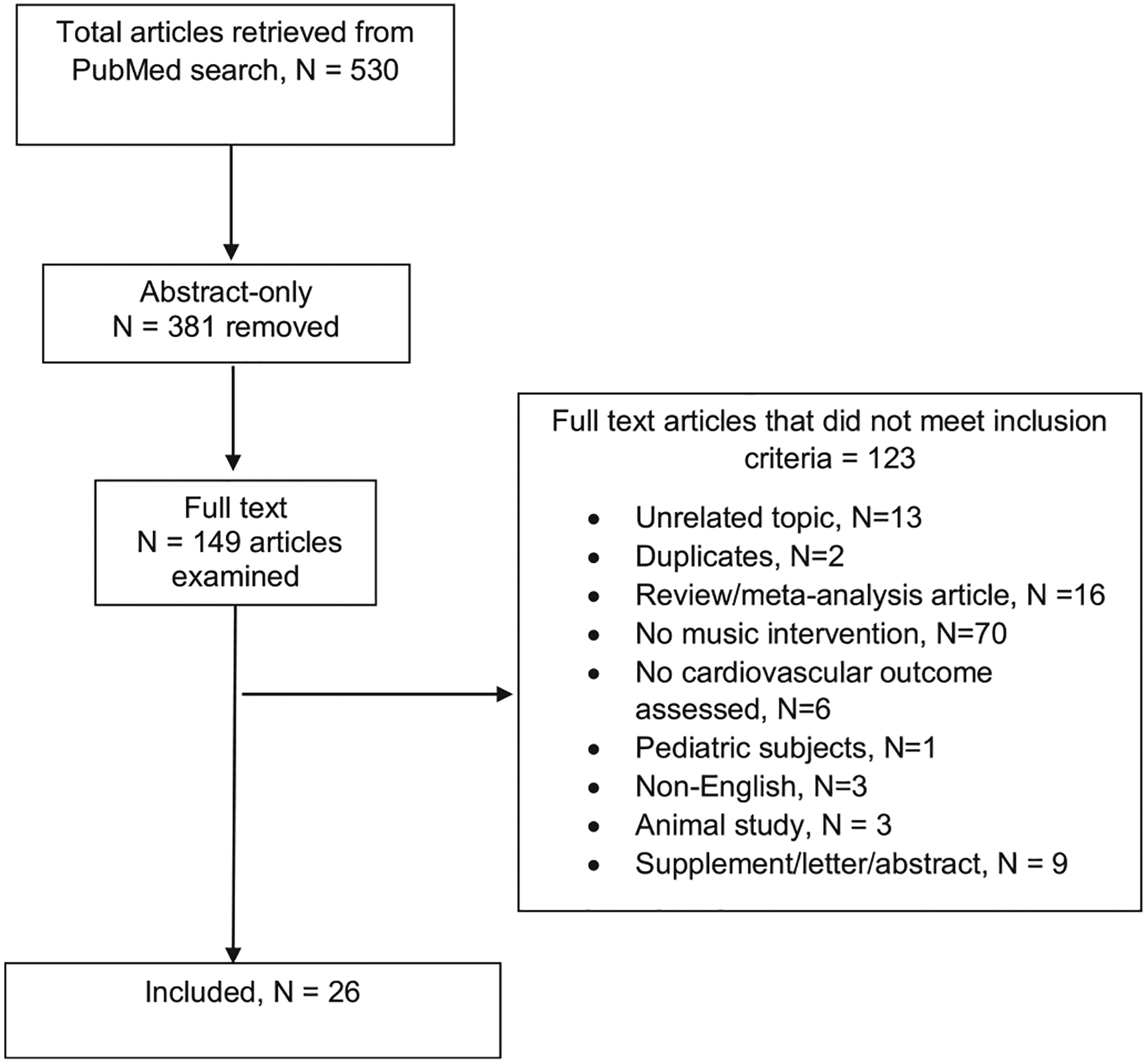
Flowchart of article search and screening results.
Quality assessments
Data extracted from all articles included the first author, year of publication, research design, sample size and study characteristics such as the mean age, sex distribution and health status of the studied population; the mode and duration of the music intervention; outcome measures assessed, and major findings, are displayed in Tables 1–3. All of these factors were considered during the quality assessment of each article.
Table 1.
Heart rate, blood pressure, and respiration outcomes of interest.
| Author | Study design | Intervention | Duration | Sample size | Subject demographics | Outcomes and major findings | Quality score |
|---|---|---|---|---|---|---|---|
| Bernardi et al. 2005 | pre-post intervention | music listening | 1 session with exposure to 6 different music styles and pauses | 24 | 12 practicing musicians and 12 age-matched controls, age 24±1, 50% females | (+) RR, minute ventilation, HR, BP, mid-cerebral artery flow velocity, and LF:HF ratio with faster tempos No change in end-tidal carbon dioxide |
15 |
| Kim et al 2018 | pre-post intervention | ocarina (wind instrument) playing | 5 to 10 weeks, twice weekly sessions of 1 hour each | 20 | elderly females without chronic lung or heart diseases, age 70±2 | (+) PFT, 6MWT, lower Borg PRE | 19 |
| Mir et al. 2020 | randomized with control | music listening +/− DASH diet | 30 minutes/day, 5 days/week, 4 weeks | 30 | pre-hypertensive, age 21±1, all males | (−) HR, SBP in music group; no change in DBP | 14 |
| Namdar et al. 2014 | pre-post intervention case-control | music listening | 1 session: 3 minutes of slow-beat music and 3 minutes of fast-beat music separated by 15 minutes of rest | 211 | 113 hypertensive males, 98 healthy males, ages 30 to 50 | (−) BP and HR in extraverts with slow music compared to introverts | 16 |
| Trappe & Voit 2016 | randomized with control | music listening | 25 minutes silent rest, Mozart, Strauss, ABBA | 120 | healthy, age 46±14, 50% females | (−) serum cortisol levels, (−) HR, BP Mozart & Strauss | 23 |
Ages in years shown as mean ± standard deviation.
RR: respiratory rate; HR: heart rate; BP: blood pressure; LF:HF is low frequency to high frequency HRV ratio; PFT: pulmonary function testing; 6MWT: 6-minute walk test; RPE: Borg rating of perceived exertion; SBP: systolic blood pressure; DBP: diastolic blood pressure.
Table 3.
ECG, cortisol, vascular function, and exercise performance outcomes of interest.
| Author | Study design | Intervention | Duration | Sample size | Subject demographics | Outcomes and major findings | Quality score |
|---|---|---|---|---|---|---|---|
| Abedi et al. 2017 | pre-post intervention | music listening | 10 minutes of Persian music over 1 visit | 22 | healthy, ages 20–24, 100% female | (−) mean P-wave, R-wave, and T-wave amplitudes | 15 |
| Alter et al. 2015 | randomized with control | music listening during cardiac rehab | 3 months | 34 | established cardiovascular disease, age 63, 30% females | (+) weekly volume of physical activity measured by accelerometers | 23 |
| Arazi et al. 2015 | pre-post intervention | exercise with and without music listening | 20 minutes of combined warm-up and resistance exercise per session | 12 | healthy, age 24±2, all male and strength-trained | lower RPE & shorter time to complete circuit with music | 14 |
| Dal Lin et al. 2018 | pre-post intervention case-control | meditation, music listening, or control | 20 minutes twice daily for 60 days | 40 | 30 with CAD after MI, 10 healthy controls, age 56±6, 23% female | Primary: (−) MAP, (−) inflammatory gene expression & mediators Secondary: (−) QT, (+) CFR, (−) CIMT, (−) stress hormones | 18 |
| Hou et al 2017 | randomized with control | music listening | 80 minutes/day, 3 times over 1 week | 99 | maintenance hemodialysis patients, age 73±3, 64% female | (−) cortisol, (−) mental stress, (+) 5-year cardiovascular survival with greater cortisol reductions |
22 |
| Maddigan et al. 2018 | randomized, cross-over design | exercise with and without music listening | 2 sessions separated by at least 2 days | 16 | healthy, ages 29±4, 50% females | (+) exercise duration, no change RPE, (+) HR, (+) RR | 19 |
| Orini et al. 2019 | pre-post intervention | music listening | 5 minutes per condition (pleasant, unpleasant, rest, tones) over 1 visit | 75 | healthy, age 25±3, 48% female | (−) QT interval | 12 |
| Rao and Kumar 2015 | pre-post intervention | exercise with and without music listening | 2 sessions separated by at least 1 week | 30 | healthy, ages 18–21, all male | (−) diastolic BP, (+) exercise time/distance, (+) METs | 15 |
| Ripley et al. | randomized with control | music listening | music listening during cardiac catheterization procedure | 70 | 70 patients undergoing LHC, age 62±8, 99% male | No change in endothelial function, as assessed by PAT | 19 |
| Sumpf 2015 | pre-post intervention | music listening | 2 self-selected and 2 control music pieces over 1 visit | 58 | healthy, age 28±5, 59% females | (+) Ek values, (+) HR, no change in RR during piloerection | 19 |
Ages in years shown as mean ± standard deviation.
RPE: Borg rating of perceived exertion; MAP: mean arterial pressure; ECG: electrocardiogram; CFR: coronary flow reserve; CIMT: carotid intima medial thickness; HR: heart rate; RR: respiratory rate; METs: metabolic equivalents where 1 MET is defined as 1 kcal/kg/hour); Ek value: resting ECG amplitude signature; PAT: peripheral arterial tonometry.
The assessment of the methodological quality of the studies was conducted for the 26 articles using the Downs and Black (1998) checklist for both randomized and non-randomized intervention studies [9]. The tool includes five sections with a total of 27 questions on study quality, external validity, study bias, confounding and selection bias, and study power. The total possible score was 28 for randomized and 25 for nonrandomized studies based on a previously published modification [10]. Downs and Black score ranges were given corresponding quality levels: excellent (26–28); good (20–25); fair (15–19); and poor (≤14) [10]. Two reviewers were assigned to each article for quality assessment. Any discrepancies in quality scores were resolved in consultation with a third reviewer. Quality scores are displayed in Tables 1–3.
Results
Twenty-six studies (1,342 subjects, 55% female) were included in this review, of which ten were randomized (8 with a control) and sixteen were non-randomized, pre-post intervention studies. Most studies (17/26) included predominantly younger, healthier subjects (mean age 26 ± 7, 61% females). The remaining nine studies included older individuals, often with cardiovascular disease (mean age 50 ± 19, 43% females) including: recent myocardial infarction or cardiac catheterization (n = 2); hypertension or pre-hypertension (n = 2); hemodialysis (n = 1); cardiac rehabilitation (n = 1); post- and peri-menopausal women (n = 1); elderly females enrolled from senior community centers (n = 1); and palliative care (n = 1). Music listening was the most studied type of intervention (21/26 studies), followed by music performance with playing instruments (n = 3) or singing (n = 2). Eighteen out of 26 studies were acute intervention studies with only a single study visit. Study outcome measures are described in detail below. Heart rate variability (HRV) was the most frequently studied outcome of interest (n = 11), followed by HR and/or BP (n = 8), exercise performance and/or Borg rating of perceived exertion (RPE, n = 5), ECG parameters (n = 4), among others. We were unable to pool the individual effect sizes given the inadequate number of RCTs included. A narrative synthesis of the evidence is presented below.
Six of the included studies were of good or excellent quality by modified Downs and Black scores ≥ 20). These 6 studies were either well-powered randomized studies or large observational cohort studies with adequate consideration or adjustment for potential confounders.
Heart rate, blood pressure, and respiration (Table 1)
Cardiorespiratory variables can be modified by musical structure (organization or composition of music by beats per minute, sequences, melody, and pauses). Vickhoff et al. [11] observed that musical structure determined RR, with a cascade or overarching effect on the HRV in group choir singing. Mantra singing demonstrated close alignment of RR and HR in terms of amplitude and frequency – resulting in the highest HRVwhen compared to hymn singing and humming. Higher HRV, a marker of greater vagal tone, is considered beneficial. Bernardi et al. [12] investigated the responses to six types of music in healthy musicians and non-musicians (age 24 ± 1) in random order both with and without intervening two-minute pauses of silence. Minute ventilation, BP, HR, and mid-cerebral artery flow increased with faster tempos and simpler rhythmic structures compared with baseline. BP, minute ventilation, and HR decreased during the silent two-minute pauses. Overall, there appeared to be an arousal effect proportional to the speed of the music, with slower rhythms inducing relaxation; silent pauses without music induced the greatest relaxation. Previous training in music enhanced the ability to respond to music rhythm (musicians breathed faster with faster tempi and had slower baseline breathing rates than non-musicians).
Mir et al. [13] randomized 30 pre-hypertensive males, ages 18 to 25, to 4 weeks of the Dietary Approaches to Stop Hypertension (DASH) diet with or without (control) music therapy. Music therapy listening sessions were 30 minutes five days per week, during which “The Best Relaxing Piano and Flute Music Ever,” was administered via recording. All participants received education on the DASH eating plan and sodium restriction with weekly reminders. Between-group comparisons showed statistically greater reductions in the mean systolic BP (by 8.73 mmHg, p < .001) and HR (by 6.42 beats/minute, p = .002) in the music group compared to the control group, with no differences in diastolic BP. The control group did not exhibit significant changes in any of these 3 outcomes from baseline to 4 weeks. This raises questions about dietary adherence (not directly assessed) in these subjects since there is excellent data that the DASH diet lowers blood pressure after just 2 weeks [14].
In a quasi-experimental research study, Namdar et al. [15] studied the impact of both slow-beat and fast-beat music listening on BP and HR in 98 healthy males and 113 hypertensive males based on introversion and extroversion personality characteristics. Extroverted, hypertensive patients showed greater reductions in systolic BP and HR after hearing slow-beat music, compared to introverts with hypertension. Healthy normotensive extroverts also showed greater reductions in HR after hearing slow-beat music, compared to introverts. In summary, personality traits may influence the impact of music stimuli on cardiovascular responses.
Trappe and Voit [16] randomized 120 healthy subjects (mean age 46, 50% female) to music listening or rest. The music group was further randomized to three arms (different sequences) of listening to various compositions by W.A. Mozart, J. Strauss, or the rock group ABBA for 25 minutes each per day over 3 days. Music by Mozart and Strauss lowered BP and HR, while music by ABBA did not. Mozart’s music had the strongest effects. Mozart’s music has previously been recommended as relaxation-inducing, [17–19] possibly related to the high degree of periodicity, repetitions, and effects of recognition of or familiarity with song. The observed effects were not correlated with the style of music individually preferred by the subjects. Men reacted to all 3 musical genres with a larger drop in cortisol concentrations than women. The lack of effect from ABBA’s music is unclear but may be related to emotional factors or use of spoken words.
Kim et al. [20] assigned 20 healthy elderly Korean females (mean age 70 ± 2) from senior community centers to 5 or 10 weeks of ocarina (a traditional flute-like wind instrument) playing. There were improvements in pulmonary function testing, 6-minute walk test, and Borg rating of perceived exertion (RPE). Larger improvements in these outcomes were seen at 10 weeks compared to 5 weeks of ocarina playing. One limitation of this study was the lack of randomization of participants or a control group. Th investigators also note that subjects were also participating in other programs at the center, such as yoga, dance, and singing. The effects of these other programs on observed results were not considered.
Heart rate variability (Table 2)
Table 2.
Heart rate variability as main outcome of interest.
| Author | Study design | Intervention | Duration | Sample size | Subject demographics | Outcomes and major findings | Quality score |
|---|---|---|---|---|---|---|---|
| Bernardi et al. 2017 | pre-post intervention | singing | 7 minutes per condition (resting, toning, singing, silent breathing, etc.) over 1 visit | 20 | healthy, age 24±4, 70% female | (+) SDNN in all conditions compared to baseline; (−) HF with singing & toning | 15 |
| Chanwimalueang et al. 2017 | pre-post intervention | playing instruments | 5 minutes of performance in low- and high-stress conditions over 2 visits | 16 | healthy musicians, age 23±2, 44% female | (+) SDNN, (+) RMMSD in low-stress compared to high-stress | 19 |
| da Silva et al. 2014 | pre-post intervention | music listening | 5 minutes per music style (baroque, heavy metal) over 1 visit | 12 | healthy, age 22±3, all males | (−) SDNN, (−) LF, (−) HF with heavy metal; (−) LF with baroque | 16 |
| do Amaral et al. 2016 | pre-post intervention | music listening | 5 minutes per music style (baroque, heavy metal) over 1 visit | 24 | healthy, age 21±2, 100% female | (−) SDNN, (−) LF with heavy metal; (−) LF with baroque | 17 |
| Fu et al. 2018 | randomized (no control group) | music listening v. breathing device | 15 minutes per day for 12 weeks |
121 | peri- and post- menopausal females, age 53±3 | no change in RSA from baseline or between groups | 27 |
| Kirk & Axelson 2020 | randomized with control group | music listening, mindfulness practice | 20–30 minutes daily for 10 days | 99 | healthy, age 37±11, 70% female | (+) RMSSD acutely in both intervention groups; (+) RMSSD after 10 days in mindfulness arm only | 23 |
| Ribeiro et al. 2018 | randomized with control group | music listening with music therapist | 30–45 minutes once weekly for 7±2 visits | 21 | mothers of preterm infants, age 26±6 | (+) RMSSD, (+) SDNN, (+) pNN50, (+) SD1 index | 18 |
| Shoda et al. 2016 | pre-post intervention | music listening | 70-minute live session and 50-minute recorded session separated by 10 weeks | 37 | healthy, age 21±2, 57% female | (−) LF/HF ratio in live session | 18 |
| Vickhoff et al. 2013 | pre-post intervention | group choir singing | 5 minutes per condition (hum, hymn, mantra, silent reading) over 1 visit | 15 | healthy choir singers, all 18 years old, mixed gender (percent female NA) | (+) RMSSD in all singing conditions, greatest in mantra | 15 |
| Warth et al. 2016 | randomized (no control group) | live music listening therapy v. prerecorded mindfulness exercise | 2 sessions, each 20 minutes | 84 | end-of-life palliative care patients, age 63±14, 71% female | (+) HF, (+) PBF in music therapy group | 23 |
| Wright & Palmer 2020 | pre-post intervention | playing instruments | 5 minutes per condition (familiar verses unfamiliar melodies) at 4 different times of the day over 1 day | 32 | healthy musicians, age 20, 78% females | (+) HR during unfamiliar melody; no changes in SDNN | 19 |
Ages in years shown as mean ± standard deviation.
SDNN: standard deviation of the NN (RR) interval; RMSSD: root mean square of the successive differences; pNN50: proportion of NN50s divided by total NNs; LF: low frequency domain; HF: high frequency domain; RSA: respiratory sinus arrhythmia; PBF: peripheral blood flow; HR: heart rate; HRV: heart rate variability; SD1 index: instantaneous beat-to-beat variability; QT: time from start of Q wave to end of T wave on ECG, encompassing ventricular depolarization and repolarization.
Eleven studies evaluated the effect of music intervention on HRV, of which nine studies were conducted in young (mean age 24), healthy subjects. Seven of eleven studies used music listening as the intervention, and two studies each examined playing instruments (in trained musicians) or singing (group choir singing in one study and individual singing in the other). Only four of these studies included randomization to specific interventions, of which two included a control or standard-of-care group.
Ribeiro et al. [21] studied the impact of weekly music therapy (MT) sessions (average number of sessions 7 ± 2 with one session/week) in 46 healthy mothers of preterm infants randomized to MT or usual care. The individual sessions were interactive with a trained music therapist for therapeutic music listening (songs selected by the participant based on personal preferences) and included reflection and verbal processing. There was a significant increase in HRV parameters (RMSSD: square root of the mean of the squares of differences between adjacent NN intervals; SDNN: standard deviation of all NN intervals; pNN50: percent of all NN intervals differing by more than 50 milliseconds in the recording period) and reductions in anxiety and depression in mothers in the MT group compared to the control group. However, data collection was completed for only 21 of the 46 mothers.
In a high-quality study, 99 healthy subjects (mean age: 37 ± 11, 70% female) were randomized to a daily 10-day intervention of one of three arms: music listening, mindfulness practice, or a non-intervention control [22]. The HRV (RMSSD) increased acutely during daily practice sessions in both the mindfulness and music listening groups compared to control. However, after the full ten days, HRV was improved only in the mindfulness practice group when compared to the baseline response. Self-reported stress was reduced over the ten days only in the mindfulness group. Differences in physical activity levels over the ten days did not appear to be a major contributor to observed findings.
Da Silva et al. [23] examined differences between listening to baroque or heavy metal music on HRV in 12 healthy men (mean age 22 ± 3). The main finding was a reduction in HRV (SDNN) while listening to heavy metal music with no significant change in HRV during exposure to baroque music. Heavy metal music decreased sympathetic (low frequency [LF]) and parasympathetic (high frequency [HF]) modulation of the heart, whereas baroque music reduced only sympathetic regulation (LF). Further, the authors found no differences in HRV with varying intensities (decibels) of music [24]. The duration of listening to each type of music was only 5 minutes, the study sample was small, and included no women. However, a similar study later undertaken in 24 healthy, young women (mean age 21 ± 2) observed similar reductions in HRV with heavy metal music at higher intensities [25].
Shoda et al. [26] sought to compare physiological responses in two listening contexts: live with a performer (pianists) and recorded music, in 37 young, healthy subjects. The LF/HF ratio was less in the live condition compared to the recorded condition, suggesting that the contribution of sympathetic versus parasympathetic activity tended to decrease in the live performance. In the live condition only, HR changed directionality in accordance with the tempo of music, a phenomenon called entrainment.
A high-quality randomized study (n = 84) by Warth et al. [27] demonstrated higher HF HRV with listening to live music therapy (compared to prerecorded mindfulness exercise) in end-of-life, palliative care patients (mean age 63±14) regardless of age and sex. Fu et al. [28] randomized 121 post- and peri-menopausal women with a high burden of hot flashes to 12 weeks (15 minutes/day) of music listening or to a portable-guided breathing device to practice slowing respiratory rate to 10 breaths/minute. They found no between-group differences in HRV response. Furthermore, cardiac autonomic parameters, as measured by pre-ejection period (PEP) and RSA, were similar at baseline and at 12 weeks. In these patients, greater self-reported anxiety and depressive symptoms as measured by multiple validated questionnaires at baseline and 12 weeks, were associated with lower HRV (RSA), reflecting decreased parasympathetic activity.
In a crossover study, Bernardi et al. [29] showed that 7 minutes each of toning (a form of improvisation-based open vowel vocalization), singing, and breathing all increased HRV (SDNN) acutely (n = 20 healthy subjects, mean age: 24, 70% female). Silent breathing proved even more favorable than the matched vocal conditions, prompting a stronger increase in SDNN with a slower heart rate. The HF power decreased during singing, and decreased even further during toning, suggesting possible mild sympathetic stimulation compared to the non-vocal condition matched for breathing pattern. Vickhoff et al. [11] also observed that the musical structure determined RR, with a cascade effect on the HRV in group choir singing. Mantra singing or meditative vocal production such as chanting - demonstrated close alignment of HR and respiration amplitude and frequency, resulting in the highest HRV when compared to hymn singing and humming.
The effect of playing instruments on HRV was evaluated in 2 studies, both in trained musicians. Chanwimalueang et al. [30] specifically studied healthy musicians (mean age 23, 70% female, 11 violinists and 5 flutists) before and during performances in both low- and high-stress conditions. HRV (AVNN: average of the NN intervals; and RMMSD) during the low-stress condition was higher than those from the high-stress condition. There were no statistically significant changes in time-domain HRV variables from the pre-performance period (30 minutes) to the performance period (5 minutes) under either condition, though there was a shift from the HF to LF band suggesting higher sympathetic input. The stress responses in female participants appeared more parasympathetically driven than those of the male participants, as evidenced by an increase in the high-frequency domain of HRV only in the former. Wright and Palmer [31] studied 32 trained pianists to determine if the impact of music performance on cardiac activity is affected by time of day, as cardiac activity shows a circadian rhythm. Participants’ HR increased during the unfamiliar melody performance relative to a familiar performance earlier in the day, but not later in the evening; however, there were no significant effects of time of day or familiarity on HRV, as measured by SDNN. Thus, time of day and familiarity of music may influence music’s ability to modulate physiological systems.
ECG, cortisol, coronary flow reserve, and endothelial function (Table 3)
Music may influence the ECG signal. Dal Lin et al. [32] assigned 30 consecutive patients (23% females) after myocardial infarction (MI) to one of 3 groups: control, music listening, meditation – for 20 minutes twice daily over 60 days. Several outcomes were assessed. There was no difference in the corrected QT interval (QTc) between the intervention and non-intervention groups at 60 days. Even though the QT interval increased acutely in the intervention groups after a single 20-minute session, it was reduced after 60 days in the music and meditation groups compared to baseline; there was no difference compared to the control group. There were concordant reductions in vital signs, stress hormones, inflammatory mediators, carotid intimal medial thickness, and inflammatory gene expression with improvement in coronary flow reserve, as assessed by transthoracic echo doppler determination of coronary flow reserve. The latter improvement may be due in part to reduced resting coronary flow from lower resting HR and BP.
In a study of 75 young, healthy subjects (50% female), Orini et al. [33] found small, but significant increases in QTc interval during both unpleasant and pleasant music listening (for 5 minutes), suggesting that emotional arousal per se has a stronger effect on cardiovascular physiology than does emotional valence (positive versus negative feeling) associated with music listening. A prior review article arrived at similar conclusions [34]. This suggests that potentially clinically relevant changes in arrhythmogenic substrates may be triggered by emotions unrelated to dramatic events and warrants further investigation in persons with cardiovascular diseases, who may have a preexisting arrhythmogenic substrate.
The resting ECG amplitude signature, Ek has been shown to predict affectivity, or the ability to experience feelings and emotions. [35]. The Ek is calculated using a ratio of specific ECG waveform amplitudes from a resting ECG [36]. Values correlate with autonomic balance whereby individuals with lower Ek values exhibit lower HRV, higher LF and lower HF spectral HRV components than individuals with higher Ek values. Furthermore, lower Ek values predict flattened affectivity. Sumpf et al. [35] found that 25 of 58 healthy individuals had measurable piloerection during music and film exposure. The Ek values increased only with music listening causing chills with piloerection. Heart rate also increased during music-evoked chills and piloerection with no change in HR without piloerection. In a separate study using discrete waveform transform analysis, Abedi et al. [37] found reductions in mean amplitudes of ECG P-waves, R-waves, and T-waves in young, healthy females after 10 minutes of listening to Persian music. Heart rate and BP were not recorded. The clinical translation of these two studies is some-what unclear.
Hou et al. [38] randomized 99 hemodialysis (HD) patients (mean age 73±3, 64% female) to 1 week of music therapy or usual care. Music therapy sessions were 80 minutes long three times that week, coinciding with HD sessions. After 1 week, the music therapy group had reductions in mental stress, as assessed by validated scores. Furthermore, they demonstrated a significant reduction in salivary cortisol levels when compared to the control group. Changes in salivary cortisol correlated with reductions in self-reported stress, systolic BP, and RR. Although there was no difference in overall survival at 5 years between the groups, there was higher 5-year cardiovascular survival (81.6% vs 63.6%, p < 0.05) in subjects with > 0.6 pg/mL reductions in cortisol levels with the intervention.
Ripley et al. [39] randomized 70 subjects undergoing cardiac catheterization for suspected coronary artery disease to music therapy (listening to slow, relaxing contemporary music) or no music therapy. Vascular endothelial function, as assessed by peripheral arterial tonometry, was performed before and after catheterization. In this setting, music intervention did not elicit a vasodilator response, lower BP, or HR, and did not relieve anxiety or stress. Though fluoroscopic time (8 minutes) did not differ between the groups, there was no mention of procedure time and duration of music therapy, which may not have been long enough to impact cardiovascular function. Patient musical preferences were not considered, and effects of moderate sedation may have contributed to the null findings.
Physical performance/endurance (Table 3)
Music listening may enhance exercise performance. Thirty healthy male medical students underwent maximal exercise tread-mill testing with the well-accepted Bruce multi-stage protocol: both with and without listening to preferred music with earphones, with each exercise test separated by at least one week. While there were no changes in peak exercise HR or systolic BP responses with music listening, there were statistically significant decreases in diastolic BP, and increases in exercise time and distance, and metabolic equivalents (METs, where one MET is defined as 1 kcal/kg/min) [40]. In a high-quality, proof-of-concept study, Alter et al. [41] randomized 34 subjects (mean age 63, 70% males) with cardiovascular disease to standard therapy with cardiac rehabilitation (CR) or CR with music listening to tempo-pace synchronized personal music playlists, for 3 months. Music lists were matched to patient preferences, but selections were restricted to tempos approximating the patients’ prescribed exercise running or walking pace (steps/minute) to achieve tempo-pace synchrony. The music group underwent further randomization to music enhanced with rhythmic auditory stimulation (RAS), which accentuates tempo-pace synchrony. RAS-enhancement involved ‘sonic modification’ of audio files to accentuate and enhance quarter-notes using lower and/or higher frequency drum instruments without altering the total volume of the sound recording itself. The music listening patients achieved higher weekly volumes of exercise activity (as measured by accelerometer) than the usual care group (475.6 vs. 370.2 minutes, p < 0.001). These improvements were largely driven by the subjects randomized to RAS, in whom physical activity volumes were two-fold higher than those randomized to music without RAS.
Maddigan et al. [42] found that high tempo music (130 bpm) compared to a no-music condition during repeated high-intensity cycling bouts in young, healthy subjects (mean age 29, 50% female) increased exercise duration by 10.7% (approximately 1 minute). Furthermore, HR recovery at 5 minutes post-exercise was 13% greater following the music condition. Similarly, Arazi et al. [42] studied 12 healthy, strength-trained males (mean age 24) to find that during exercise with fast (130 bpm) tempo music, the men reported lower ratings of perceived exertion in addition to completing a circuit of resistance exercise in a shorter time.
Discussion
Main findings
The tempo of music may directly correlate with changes in HR, RR, and BP. These effects appear to depend on the speed of music rather than the style or musical preference of the subject. Music tempo may be used to synchronize or entrain body rhythms such as heart and respiratory rates. However, a 2015 review showed no evidence for entrainment of the heart rate to (non-live) music listening, at least without a visual performance [34]. Listening context is another contributing factor to be considered, and live listening could facilitate entrainment and merits further investigation.
Overall, there appears to be a positive impact of music listening on HRV, suggesting enhanced parasympathetic activity, similar to a previously published systematic review of 24 pre-post intervention studies and 5 RCTs [43]. However, included studies suffer from significant heterogeneity in terms of study design, population, and type and duration of musical intervention; differences in baseline characteristics were typically not controlled for. Few studies considered the role of sex in HRV (four of the eleven HRV studies in this review included only one sex). A comprehensive meta-analysis of 172 studies with data from over 63,000 participants (31,970 females) demonstrated significantly lower mean RR intervals and standard deviation of RR intervals (SDNN) in females [44]. The power spectral density of females was characterized by greater HF, suggesting greater vagal activity, and less LF power. In addition, meta-regression revealed significant effects of age, respiration, and length of HRV recording for analysis [44]. Studies in the present review suggest that changes in breathing pattern may be the key element mediating the effects of musical structure on HRV. Singing may have different effects on HRV compared to listening since it is an active rather than passive mode of music intervention; however, only two studies in this review studied singing and HRV, and both found improvements in the time domain measures of HRV with singing [11, 29].
Salivary cortisol levels decreased with music listening in two RCTs[16, 38]. In the study by Hou et al, larger reductions in cortisol correlated with improved 5-year cardiovascular survival [38]. However, the study population was narrow and included elderly patients (mean age 73) on maintenance hemodialysis. The contrasting effects of music on the QT interval in the two such studies reviewed may be related to the population studied (healthy versus those with coronary artery disease after MI) and/or duration of music listening sessions [32, 33]. Very few studies examined the impact of music on endothelial function or coronary flow reserve. Limitations of these studies include non-randomization design, lack of separation of results between meditation and music listening groups and multiple comparison testing. Thus, more research is needed to draw conclusions on these specific outcome variables.
This review supports the use of music listening to enhance physical performance; specifically, tempo-pace synchronous music can reduce exercise-perceived exertion, increase exercise endurance and adherence to physical activity. On the other hand, listening to slow-tempo music appears to induce relaxation. These ‘distracting effects’ may be related to the focus and release of attention, respectively [42, 45]. Furthermore, these effects may be greater when aligned with individual music preferences [41].
Several studies here included silent breathing, rest, or mindfulness control period or group when comparing to a music intervention or group. The sum of the findings is that slow, silent breathing and meditation or mindfulness may be equally if not more impactful than music, on specific outcome measures, such as HRV. Findings are similar to previous observations that silent, slow breathing yields effects on HRV that are at least comparable, and at times superior, to singing traditional songs [46]. This is an important consideration for the design of future clinical trials whereby an appropriate control may simply be usual care (rather than rest or meditation).
Whether or not musical preference matters may be dependent upon the outcome measured. Emotional arousal may have a stronger effect on cardiovascular physiology than does emotional valence (positive versus negative feeling) associated with music listening [33]. A prior review article arrived at similar conclusions [34]. Further research is needed to test the effect of emotional valence in patients with cardiac disorders, who may have preexisting arrhythmogenic substrates and to better understand how to translate these findings into strategies that can impact patients’ health.
Limitations
The major limitation of this review is the inability to comprehensively capture all relevant papers measuring cardiovascular variables due to the narrowed focus on cardiovascular variables and prespecified selection criteria. We were not able to include studies addressing the impact of music across the spectrum of cardiovascular diseases or on other important clinical outcomes such as depression, anxiety, and quality of life (QOL) [47, 48] because they did not use music as an intervention, examine cardiovascular variables, or were review articles or reports on a proposed methodology only. For example, in a multicenter, randomized, trial of 159 patients with heart failure, Burrai et al. [47, 48] found that listening to 30 minutes of recorded classical music per day for 3 months resulted in improved QOL; however, measures of cardiovascular function were not performed. In this review, most included studies used acute interventions during a single visit. As such, we cannot reliably conclude what duration of music intervention is sufficient to effect long-term changes in the cardiovascular system. The majority of studies in this review used music listening as the intervention. Singing and instrument playing, which are more active interventions, may have different effects on cardiovascular physiology. Furthermore, the emotional responses to a musical stimulus are not dependent only on the stimulus type, but also on how the subject interprets the stimulus, and his or her current mood state.
Directions for future research
Music interventions of longer duration (weeks to months) are clearly needed, as are more studies in subjects with preexisting cardiovascular diseases. Future studies measuring HRV should not only be stratified by sex but should consider other confounders, especially age and comorbidities. Furthermore, HRV is a complex signal, and analyses should include both time and frequency HRV domains to disentangle the relative contributions of the parasympathetic and sympathetic nervous systems. The HRV response may be further complicated by existing cardiovascular disease and medication use, both of which must be considered in the study design [49]. To understand mechanisms by which music may impact cardiovascular health, it will also be important to consider studying other important biomarkers, such as inflammatory and cardiac injury markers, natriuretic peptides, and vascular endothelial function, an excellent surrogate of coronary endothelial function [50] and valuable predictor of future cardiovascular health [51]. Clinical outcome measures, such as hospitalizations, hospital length of stay and medication needs, would also be valuable.
In future studies, it will be important to characterize the emotional impact of music stimuli regarding felt valence and arousal or relaxation, at a minimum. Personal music preferences, genres, and tempos should also be tracked. An appropriate control group should be included, keeping in mind that quiet rest or meditation may also favorably impact cardiovascular physiology. Therefore, either a usual care control or control with other audio stimuli (such as audiobooks or nature sounds) [34], should be considered. Additional studies of more active musical interventions such as singing and instrument playing, should also be conducted.
Conclusion
Listening to music is a complex phenomenon, involving psychological, emotional, cardiorespiratory, and likely other body system changes. Individual responses to music can be influenced by personal preferences, familiarity with music, environment, prior music experience, and other health factors. This review highlights the need for well-controlled randomized clinical trials in subjects with preexisting medical conditions and appropriate controls. Comparison of individualized music sessions to preferred or random music selections, and duration of therapies needed for therapeutic benefit, are important variables for future studies. The promising effects of music interventions on cardiovascular physiology, coupled with their low cost and a high degree of safety, warrant further exploration in both healthy populations and especially those with cardiovascular disease.
Funding
This publication was supported in part by the National Center for Complementary & Integrative Health of the National Institutes of Health under Award Number R61AT010680.
Footnotes
Publisher's Disclaimer: Disclaimer
Publisher's Disclaimer: The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the National Heart, Lung, and Blood Institute, the National Institutes of Health, or the United States Department of Health and Human Services.
Declaration of Competing Interest
The Authors declare that there is no conflict of interest.
References
- [1].Thaut MH. Chapter 8 - Music as therapy in early history. In: Progress in Brain Research. 217. Elsevier; 2015. p. 143–58. [DOI] [PubMed] [Google Scholar]
- [2].Babikian T, Zeltzer L, Tachdjian V, Henry L, Javanfard E, Tucci L, et al. Music as medicine: a review and historical perspective. Alternat Complement Therapies 2013;19:251–4. [Google Scholar]
- [3].Montinari MR, Giardina S, Minelli P, Minelli S. History of music therapy and its contemporary applications in cardiovascular diseases. South Med J 2018;111(2):98–102. [DOI] [PubMed] [Google Scholar]
- [4].Taylor DB. Music in general hospital treatment from 1900 to 1950. J Music Ther 1981;18(2):62–73. [DOI] [PubMed] [Google Scholar]
- [5].Kane EON. Phonograph in operating-room. J Am Med Ass 1914;LXII(23):1829. [Google Scholar]
- [6].de L’Etoile S The history of the undergraduate curriculum in music therapy. J Music Ther 2000;37(1):51–71. [DOI] [PubMed] [Google Scholar]
- [7].Tsuji H, Venditti FJ Jr, Manders ES, Evans JC, Larson MG, Feldman CL, et al. Reduced heart rate variability and mortality risk in an elderly cohort. The Framingham Heart Study. Circulation 1994;90(2):878–83. [DOI] [PubMed] [Google Scholar]
- [8].Vaishnav S, Stevenson R, Marchant B, Lagi K, Ranjadayalan K, Timmis AD. Relation between heart rate variability early after acute myocardial infarction and long-term mortality. Am J Cardiol 1994;73(9):653–7. [DOI] [PubMed] [Google Scholar]
- [9].Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52(6):377–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Hooper P, Jutai JW, Strong G, Russell-Minda E. Age-related macular degeneration and low-vision rehabilitation: a systematic review. Can J Ophthalmol 2008;43(2):180–7. [DOI] [PubMed] [Google Scholar]
- [11].Vickhoff B, Malmgren H, Astrom R, Nyberg G, Ekstrom SR, Engwall M, et al. Music structure determines heart rate variability of singers. Front Psychol 2013;4:334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Bernardi L, Porta C, Sleight P. Cardiovascular, cerebrovascular, and respiratory changes induced by different types of music in musicians and non-musicians: the importance of silence. Heart 2006;92(4):445–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Mir IA, Chowdhury M, Islam RM, Ling GY, Chowdhury A, Hasan ZM, et al. Relaxing music reduces blood pressure and heart rate among pre-hypertensive young adults: A randomized control trial. J Clin Hypertens (Greenwich) 2021;23(2):317–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Juraschek SP, Miller ER 3rd, Weaver CM, Appel LJ. Effects of sodium reduction and the dash diet in relation to baseline blood pressure. J Am Coll Cardiol 2017;70(23):2841–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Namdar H, Taban Sadeghi M, Sabourimoghaddam H, Sadeghi B, Ezzati D. Effects of music on cardiovascular responses in men with essential hypertension compared with healthy men based on introversion and extraversion. J Cardiovasc Thorac Res 2014;6(3):185–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Trappe HJ, Voit G. The cardiovascular effect of musical genres. Dtsch Arztebl Int 2016;113(20):347–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Smith JC, Joyce CA. Mozart versus new age music: relaxation states, stress, and ABC relaxation theory. J Music Ther 2004;41(3):215–24. [DOI] [PubMed] [Google Scholar]
- [18].Bangerter A, Heath C. The Mozart effect: tracking the evolution of a scientific legend. Br J Soc Psychol 2004;43(Pt 4):605–23. [DOI] [PubMed] [Google Scholar]
- [19].Thompson WF, Schellenberg EG, Husain G. Arousal, mood, and the Mozart effect. Psychol Sci 2001;12(3):248–51. [DOI] [PubMed] [Google Scholar]
- [20].Kim BS, Kim JH, Park SH, Seo HS, Lee HS, Lee MM. Effect of a respiratory training program using wind instruments on cardiopulmonary function, endurance, and quality of life of elderly women. Med Sci Monit 2018;24:5271–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ribeiro MKA, Alcantara-Silva TRM, Oliveira JCM, Paula TC, Dutra JBR, Pedrino GR, et al. Music therapy intervention in cardiac autonomic modulation, anxiety, and depression in mothers of preterms: randomized controlled trial. BMC Psychol 2018;6(1):57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Kirk U, Axelsen JL. Heart rate variability is enhanced during mindfulness practice: a randomized controlled trial involving a 10-day online-based mindfulness intervention. PLoS One 2020;15(12):e0243488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].da Silva SA, Guida HL, Dos Santos Antonio AM, de Abreu LC, Monteiro CB, Ferreira C, et al. Acute auditory stimulation with different styles of music influences cardiac autonomic regulation in men. Int Cardiovascular Res J 2014;8(3):105–10. [PMC free article] [PubMed] [Google Scholar]
- [24].Amaral JA, Nogueira ML, Roque AL, Guida HL, De Abreu LC, Raimundo RD, et al. Cardiac autonomic regulation during exposure to auditory stimulation with classical baroque or heavy metal music of different intensities. Turk Kardiyoloji Dernegi arsivi 2014;42(2):139–46. [DOI] [PubMed] [Google Scholar]
- [25].do Amaral JA, Guida HL, de Abreu LC, Barnabe V, Vanderlei FM, Valenti VE. Effects of auditory stimulation with music of different intensities on heart period. J Tradit Complement Med 2016;6(1):23–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Shoda H, Adachi M, Umeda T. How Live Performance Moves the Human Heart. PLoS One 2016;11(4):e0154322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Warth M, Kessler J, Hillecke TK, Bardenheuer HJ. Trajectories of terminally ill patients’ cardiovascular response to receptive music therapy in palliative care. J Pain Symptom Manage 2016;52(2):196–204. [DOI] [PubMed] [Google Scholar]
- [28].Fu P, Gibson CJ, Mendes WB, Schembri M, Huang AJ. Anxiety, depressive symptoms, and cardiac autonomic function in perimenopausal and postmenopausal women with hot flashes: a brief report. Menopause 2018;25(12):1470–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Bernardi NF, Snow S, Peretz I, Orozco Perez HD, Sabet-Kassouf N, Lehmann A. Cardiorespiratory optimization during improvised singing and toning. Sci Rep 2017;7(1):8113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Chanwimalueang T, Aufegger L, Adjei T, Wasley D, Cruder C, Mandic DP, et al. Stage call: Cardiovascular reactivity to audition stress in musicians. PLoS One 2017;12(4):e0176023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Wright SE, Palmer C. Physiological and Behavioral Factors in Musicians’ Performance Tempo. Front Hum Neurosci 2020;14:311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Dal Lin C, Marinova M, Rubino G, Gola E, Brocca A, Pantano G, et al. Thoughts modulate the expression of inflammatory genes and may improve the coronary blood flow in patients after a myocardial infarction. J Tradit Complement Med 2018;8(1):150–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Orini M, Al-Amodi F, Koelsch S, Bailón R. The effect of emotional valence on ventricular repolarization dynamics is mediated by heart rate variability: a study of qt variability and music-induced emotions. Front Physiol 2019;10:1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Koelsch S, Jancke L. Music and the heart. Eur Heart J 2015;36(44):3043–9. [DOI] [PubMed] [Google Scholar]
- [35].Sumpf M, Jentschke S, Koelsch S. Effects of Aesthetic Chills on a Cardiac Signature of Emotionality. PLoS One 2015;10(6):e0130117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Koelsch S, Remppis A, Sammler D, Jentschke S, Mietchen D, Fritz T, et al. A cardiac signature of emotionality. Eur J Neurosci 2007;26(11):3328–38. [DOI] [PubMed] [Google Scholar]
- [37].Abedi B, Abbasi A, Goshvarpour A, Khosroshai HT, Javanshir E. The effect of traditional Persian music on the cardiac functioning of young Iranian women. Indian Heart J 2017;69(4):491–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Hou YC, Lin YJ, Lu KC, Chiang HS, Chang CC, Yang LK. Music therapy-induced changes in salivary cortisol level are predictive of cardiovascular mortality in patients under maintenance hemodialysis. Ther Clin Risk Manag 2017;13:263–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Ripley L, Christopoulos G, Michael TT, Alomar M, Rangan BV, Roesle M, et al. Randomized controlled trial on the impact of music therapy during cardiac catheterization on reactive hyperemia index and patient satisfaction: the Functional Change in Endothelium After Cardiac Catheterization, With and Without Music Therapy (FEAT) study. J Invasive Cardiol 2014;26(9):437–42. [PubMed] [Google Scholar]
- [40].Rao NS, Kumar JV. Role of Perceptual Factors on Endurance Profiles on Tread-mill Exercise. J Clin Diagn Res 2015;9(6):CC13–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Alter DA, O’Sullivan M, Oh PI, Redelmeier DA, Marzolini S, Liu R, et al. Synchronized personalized music audio-playlists to improve adherence to physical activity among patients participating in a structured exercise program: a proof-of-principle feasibility study. Sports Med Open 2015;1(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Maddigan ME, Sullivan KM, Halperin I, Basset FA, Behm DG. High tempo music prolongs high intensity exercise. PeerJ 2019;6:e6164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Mojtabavi H, Saghazadeh A, Valenti VE, Rezaei N. Can music influence cardiac autonomic system? A systematic review and narrative synthesis to evaluate its impact on heart rate variability. Complement Ther Clin Pract 2020;39:101162. [DOI] [PubMed] [Google Scholar]
- [44].Koenig J, Thayer JF. Sex differences in healthy human heart rate variability: A meta-analysis. Neurosci Biobehav Rev 2016;64:288–310. [DOI] [PubMed] [Google Scholar]
- [45].Arazi H, Asadi A, Purabed M. Physiological and psychophysical responses to listening to music during warm-up and circuit-type resistance exercise in strength trained men. J Sports Med (Hindawi Publ Corp) 2015;2015:389831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Olsson E, von Schéele B, Theorell T. Heart rate variability during choral singing. Music Med 2013;5:52–9. [Google Scholar]
- [47].Lin ZW, Huang ST, Xu N, Cao H, Chen LW, Chen Q. Effect of music therapy on the chronic pain and midterm quality of life of patients after mechanical valve replacement. Ann Thorac Cardiovasc Surg 2020;26(4):196–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Burrai F, Sanna GD, Moccia E, Morlando F, Cosentino ER, Bui V, et al. Beneficial effects of listening to classical music in patients with heart failure: a randomized controlled trial. J Card Fail 2020;26(7):541–9. [DOI] [PubMed] [Google Scholar]
- [49].Butta C, Tuttolomondo A, Casuccio A, Petrantoni R, Miceli G, Cuttitta F, et al. Relationship between HRV measurements and demographic and clinical variables in a population of patients with atrial fibrillation. Heart Vessels 2016;31(12):2004–13. [DOI] [PubMed] [Google Scholar]
- [50].Yeboah J, McClelland RL, Polonsky TS, Burke GL, Sibley CT, O’Leary D, et al. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA 2012;308(8):788–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Son Y, Kim K, Jeon S, Kang M, Lee S, Park Y. Effect of exercise intervention on flow-mediated dilation in overweight and obese adults: meta-analysis. Int J Vasc Med 2017;2017:7532702. [DOI] [PMC free article] [PubMed] [Google Scholar]


