Abstract
Objectives:
We examined the association between multimorbidity and social participation and whether purpose in life and life satisfaction moderate this relationship.
Methods:
Participants were 12,825 Health and Retirement Study adults. We used multiple linear regression to examine the association between a cumulative-updated multimorbidity-weighted index (MWI) and social participation.
Results:
Among adults with average purpose in life or life satisfaction, MWI was associated with lower social participation. For those with above average purpose in life, each 1-point increase in MWI was associated with a 0.11-point (95%CI:0.07–0.14) better social participation score. Participants with above average life satisfaction experienced a 0.04-point (95%CI:0.02–0.07) better social participation score with each 1-point increase in MWI.
Discussion:
Multimorbidity was associated with worse social participation but this was reversed by above average purpose in life and life satisfaction. Interventions that improve well-being should be assessed to enhance social participation among older adults with any degree of multimorbidity.
Keywords: health-related quality of life, epidemiology, successful aging, leisure
INTRODUCTION
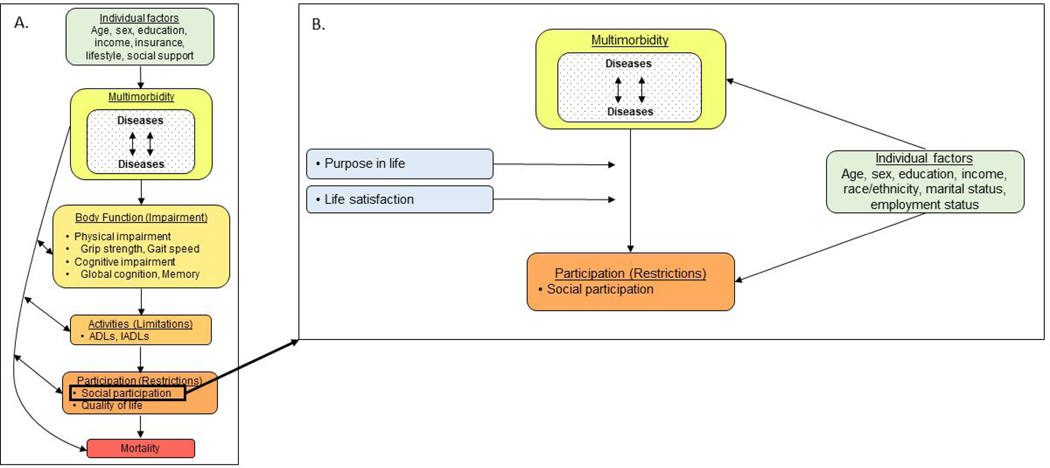
Multimorbidity, the coexistence of multiple chronic conditions, has an enduring and multifaceted impact on individuals. Its complications span several downstream components in the International Classification of Functioning, Disability, and Health (ICF) continuum of functioning and disability (World Health Organization, 2002), including worse physical and cognitive performance, disability, mental and physical health-related quality of life (HRQOL), and increased risk of all-cause mortality (Wei, Kabeto et al., 2019; Wei et al., 2018; Wei, Levine et al., 2019; Wei & Mukamal, 2019; Wei & Mukamal, 2018). In the ICF model, activities and participation have several upstream influences including multimorbidity (Figure 1). Physical functioning decline resulting from multimorbidity may hinder one’s ability to participate in social activities (Bowling, 1995). Further, multimorbidity compounded by poor physical health is associated with worse mental health (Fortin et al., 2004), which may reduce desire to engage in social activities. Environmental-level and individual factors such as low socioeconomic status may also limit access to social activities for multimorbid adults with disability (Galenkamp et al., 2016).
Figure 1.
Panel A: Adaptation of the ICF Continuum of Functioning and Disability to Include Multimorbidity; Panel B: Directed Acyclic Graph (DAG) of Variables in the Present Analysis
While several complications of multimorbidity have garnered attention (Wei, Kabeto et al., 2019; Wei et al., 2018; Wei & Mukamal, 2019; Wei & Mukamal, 2018), a perhaps overlooked dimension is social health, including participation and engagement in social activities. Social participation is dynamic, attainable, and has potential to provide deep personal connections and personal fulfillment. Prior studies report an association between social participation and better HRQOL (He et al., 2017), cognitive functioning (Bourassa et al., 2017), and decreased risk of cardiovascular disease and all-cause mortality (Glass et al., 1999; Hill et al., 2005). Greater social participation and activity engagement is predictive of improved measures of well-being (Smith et al., 2020). Engaging in social activities may also mitigate the adverse effects of loneliness and isolation on health (Fokkema & Knipscheer, 2007). Older adults are particularly susceptible to loneliness and isolation, as they may live alone, have fewer family ties, and experience functional decline that hampers their social engagement (Singh & Misra, 2009). Over half of adults aged 60 and older in a recent nationally representative sample reported being lonely (Gerst-Emerson & Jayawardhana, 2015). Quantifying the impact of multimorbidity on social participation could help identify an unfulfilled need and potential target for intervention to improve the HRQOL of older adults susceptible to both multimorbidity and loneliness.
While targeting social participation directly may positively impact HRQOL, it may also be improved by enhancing other adaptable characteristics. Particularly, purpose in life and life satisfaction are independently associated with social participation (Sano & Kyougoku, 2016; van Genderen et al., 2018). These psychosocial constructs are important dimensions of well-being (Musich et al., 2018) and may impact participation in activities. Low levels of both have been associated with symptomatic multimorbidity, poor self-rated health (Marques et al., 2018; Stålbrand et al., 2007), limitations in basic and instrumental activities of daily living (Tomioka et al., 2016), and mortality (Alimujiang et al., 2019). Further, each construct represents a distinct theoretical perspective of well-being. Life satisfaction is representative of subjective well-being, or hedonia, which emphasizes pleasure, happiness, and the absence of distress (Diener et al., 1985). Purpose in life represents psychological well-being, or eudaimonia, which defines well-being as living up to one’s perceived potential, or experiencing authenticity, meaning, and self-actualization (Ryff, 1989). Finally, purpose in life and life satisfaction are constructs that can be measured with validated tools.
We aimed to quantify the association between multimorbidity and social participation using a comprehensive measure of social participation that included the frequency of several cognitively, physically, and/or socially stimulating activities. We measured multimorbidity with a validated multimorbidity-weighted index (MWI) that weights self-reported physician-diagnosed chronic conditions by physical functioning. We hypothesized that multimorbidity was inversely associated with social participation, and that this was modified by both purpose in life and life satisfaction. We postulated that better purpose in life and life satisfaction both attenuated the association between multimorbidity and social participation through their positive influences on well-being.
METHODS
Study population
The Health and Retirement Study (HRS) is a longitudinal, nationally representative study of adults aged 51 years and older conducted in waves every 2 years (Sonnega et al., 2014). Biennially, participants report physician-diagnosed chronic conditions, functional status, health behaviors, living situation, household income, and other characteristics described previously (Sonnega et al., 2014).
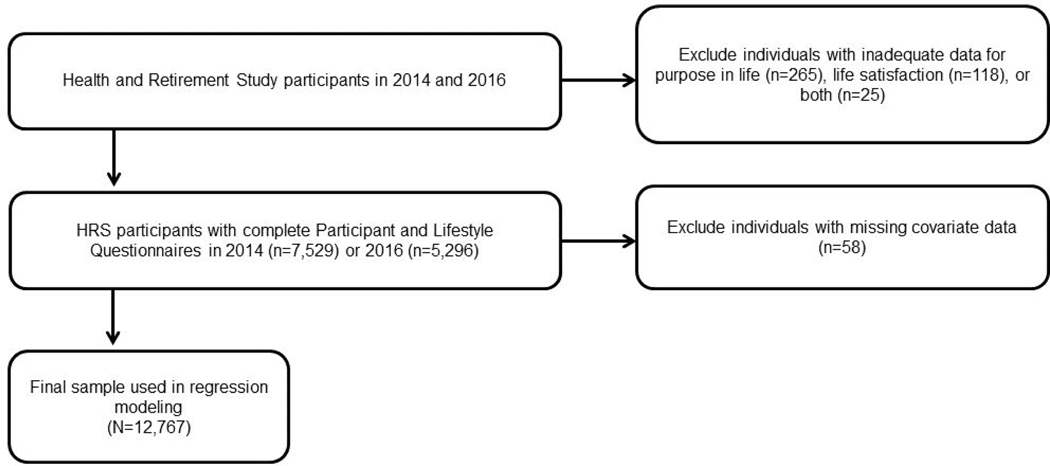
Alternating random halves of the HRS cohort completed a supplemental Participant Lifestyle Questionnaire (PLQ) following completion of the biennial core survey. The PLQ included questions about social participation, life satisfaction, purpose in life, and other related domains (Smith et al., 2017). The PLQ was administered to half of the cohort each study wave so that over time, each half completed the questionnaire every 4 years (Figure 2). In 2014, eligibility for the enhanced face-to-face PLQ included non-institutionalized self-respondents, nursing home residents, telephone interview, or proxy respondents. Proxies were used for participants with cognitive or visual impairment, disability resulting in inability to hold a pen, or illness prevenitng completion of the interview. About 1–2% of PLQs were completed using proxy respondents. In 2016, eligibility for the PLQ was revised to match the eligibility criteria for HRS physical measures and biomarkers, allowing only non-institutionalized self-respondents to complete the questionnaire in person. The PLQ response rate was 77.8% in 2014 and not yet available for 2016 (Smith et al., 2017).
Figure 2.
Participant Flow Diagram
For inclusion, participants must have completed both the core survey with self-reported physician-diagnosed conditions, from which their multimorbidity was computed biennially, and a subsequent PLQ. This study was approved by the University of Michigan Medical School Institutional Review Board.
Multimorbidity measurement
Multimorbidity was quantified through a validated MWI that weights self-reported physician-diagnosed chronic conditions by physical functioning. We used self-reported diseases starting in 2010, the first year a core set of chronic conditions in the index were consistently assessed, or 2012 (to precede date of PLQ completion) and updated every study wave until 2014 or 2016. The following conditions were included: diseases of the heart (myocardial infarction, angina, congestive heart failure, arrhythmia, other heart problems), stroke, hypertension, chronic lung disease, cancer (malignant tumor excluding skin), diabetes, joint disease (arthritis, connective tissue disease), joint replacement (hip, knee), dementia, glaucoma, and depression. Briefly, each condition was weighted by its impact on a 10-item physical functioning scale resembling the Short Form-36 (Ware, 1993; Wei et al., 2018). We summed the weighted chronic diseases to compute a MWI value for each participant (Wei et al., 2018). MWI was examined continuously and categorically in quartiles as a cumulative predictor over four years in the final model.
Social participation assessment
The dependent variable social participation was assessed using data from the 2014 (field interview dates March 2014-April 2015) and 2016 (field interview dates April 2016-April 2018) PLQs to ensure data collection took place after our exposure variable (multimorbidity from the core survey). We defined social participation as participation or engagement in activities that could be cognitively, physically, or socially stimulating. Social participation score was based on the frequency of participation in 21 specific activities including volunteering, fitness activities, social engagement such as social/community group attendance, and cognitive engagement such as educational course participation, writing, and reading (Table 1). These activities were part of the “Social Participation and Social Engagement” measure in the PLQ (Smith et al., 2017). The activities in this list follow the taxonomy of social participation proposed by Levasseur et al (Levasseur et al., 2010). The measure is comprehensive and includes activities done 1) in preparation for connecting with others, 2) alone but completed while being around others, 3) while making social contact with others but not doing a specific activity with them, 4) with others to reach a common goal, 5) to help others, and 6) to contribute to society (Levasseur et al., 2010).
Table 1.
Social Participation Activities Reported by Health and Retirement Study Participants, 2014 and 2016
| Activity | Categorization in Levasseur taxonomy1 | % Reporting regular participation2 N=12,825 |
|---|---|---|
| Watch television | 1 | 97.1 |
| Read books, magazines, or newspapers | 1 | 90.9 |
| Pray privately in a place other than a church or synagogue | 1 | 73.0 |
| Do home maintenance or gardening | 1 | 72.5 |
| Walk for 20 minutes or more | 2 | 69.9 |
| Bake or cook something special | 1 | 68.5 |
| Use a computer for e-mail, Internet, or other tasks | 3 | 65.4 |
| Play sports or exercise | 2 | 55.5 |
| Do activities with grandchildren, nieces/nephews, or neighborhood children | 4 | 52.1 |
| Do word games such as crossword puzzles or Scrabble | 4 | 48.4 |
| Work on a hobby or project | 1 | 45.9 |
| Play cards or games such as chess | 4 | 33.4 |
| Go to a sport, social, or other club | 6 | 32.8 |
| Do writing (such as letters, stories, or journal entries) | 1 | 32.4 |
| Do other volunteer or charity work | 5 | 26.6 |
| Care for sick or disabled adult | 5 | 19.1 |
| Attend meetings of non-religious organizations, such as political, community, or other interest groups |
6 | 16.5 |
| Volunteer work with children or young people | 5 | 14.0 |
| Attend an educational or training course | 3 | 12.7 |
| Make clothes, knit, embroider, etc. | 1 | 12.6 |
| Participate in a local community arts group such as a choir, dance, photography, theater, or music group | 4 | 10.0 |
Categories of Levasseur taxonomy: 1) Activity done in preparation for connecting with others; 2) Activity done alone but completed while being around others; 3) Activity done while making social contact with others but not doing a specific activity with them; 4) Activity done with others to reach a common goal; 5) Activity done to help others; and 6) Activity done to contribute to society
Regular participation defined as engaging in social activity at least once per month.
Participants were instructed, “These first questions are about the activities in your life now. Please tell us how often you do each activity.” Response choices included 1) Daily, 2) Several times a week, 3) Once a week, 4) Several times a month, 5) At least once a month, 6) Not in the last month, 7) Never/Not Relevant. The score for each participant was calculated by summing the corresponding values of participation frequency for each activity. The continuous score ranged from 21 to 147, which we reverse coded so the worst score was 21 (no participation in any activities) and the best score was 147 (participation in 21 activities daily). Participants were required to report responses for at least 2 activities to have a score computed. Activities without responses were assigned the lowest value of 1 (never/not relevant).
Modifiers and covariates
Purpose in life and life satisfaction were evaluated as potential modifiers of the association between MWI and social participation. Both variables were based on responses to the PLQ. Purpose in life was measured with a 7-item scale from the Ryff Scales of Psychological Well-Being (Ryff, 1989). While Ryff’s original scale of psychological well-being measures six theory-driven dimensions, this subscale estimates only purpose in life. The subscale has acceptable internal consistency with α=0.77 in the 2014 HRS (Smith et al., 2017). Participants answered the prompt, “Please say how much you agree or disagree with each of the following statements: 1) I enjoy making plans for the future and working to make them a reality, 2) My daily activities often seem trivial and unimportant to me, 3) I am an active person in carrying out the plans I set for myself, 4) I don’t have a good sense of what it is I’m trying to accomplish in life, 5) I sometimes feel as if I’ve done all there is to do in life, 6) I live life one day at a time and don’t really think about the future, 7) I have a sense of direction and purpose in my life.” Response choices ranged from 1 (strongly disagree) to 6 (strongly agree). Items 2 and 4–6 were reverse coded. We calculated the average of item responses to create a purpose in life score (range 1–6, higher is better). We excluded 265 (2.1%) participants who responded to fewer than 4 of the 7 items per PLQ recommendations (Smith et al., 2017).
The PLQ life satisfaction questions aimed to measure subjective well-being among participants using Diener’s Satisfaction With Life Scale (Diener et al., 1985). This scale has favorable psychometric properties when tested in multiple age groups and populations, including high internal consistency and reliability over time (Diener et al., 1985). In the 2014 HRS, the Satisfaction with Life Scale had high internal consistency (α=0.89, (Smith et al., 2017)). Participants responded to the question, “Please say how much you agree or disagree with the following statements: 1) In most ways my life is close to ideal, 2) The conditions of my life are excellent, 3) I am satisfied with my life, 4) So far, I have gotten the important things I want in life, and 5) If I could live my life again, I would change almost nothing.” Response choices ranged from 1 (strongly disagree) to 7 (strongly agree). A life satisfaction score was calculated for each respondent by averaging the responses across all 5 statements (range 1–7, higher is better). We excluded 118 (0.9%) who responded to fewer than 3 of the 5 items per PLQ recommendations (Smith et al., 2017).
Potential confounders were selected a priori based on existing literature (Ang, 2018; Dong et al., 2014; Galenkamp & Deeg, 2016; Principi et al., 2016; Utz et al., 2002). These covariates were treated as simple updated variables evaluated in the 2014 or 2016 HRS core questionnaire and included age (continuous), sex, education (<12 years of school completed, 12 years, 13–15 years, and ≥16 years), income (household net worth in quartiles), race/ethnicity (white non-Hispanic, Black non-Hispanic, Hispanic, or other), marital status (married, annulled/separated/divorced, widowed, never married, or other), and employment status (working/not working, including those who were unemployed, laid off, homemakers, disabled, retired, on leave, or reported other non-working status). We excluded 57 participants missing covariate data. We intentionally did not adjust for social networks on the pathway between multimorbidity and social participation due to potential over-adjustment and limited evidence supporting an association between social networks and multimorbidity.
Statistical analysis
We calculated univariate statistics for MWI, social participation, purpose in life, life satisfaction, and demographic characteristics. We assessed MWI as a continuous and categorical variable and tested for non-linearity using fractional polynomials. The distribution of MWI with social participation was not significantly non-linear (p=0.38). We used multiple linear regression to examine the association between MWI and social participation. Regression models were adjusted for age, sex, race/ethnicity, education, household net worth, marital status, and employment status.
Purpose in life and life satisfaction were considered modifiers if the regression coefficient for the interaction between MWI and each was statistically significant. Purpose in life and life satisfaction were retained as continuous variables and centered around the mean in all models, allowing for the main effect of MWI to be interpreted at the average value of purpose in life and life satisfaction, respectively. The average purpose in life score was 4.6, and the average life satisfaction score was 5.0. We reported the interactions between MWI and purpose in life and MWI and life satisfaction in separate models and combined in one model. We also examined the simultaneous interaction between MWI, purpose in life, and life satisfaction.
To account for potential differences between respondents to the 2014 PLQ and 2016 PLQ, we tested for an interaction between multimorbidity adjusted for cohort year and calendar time. The interaction term was not significant (p=0.26) so both years of data were combined.
We reported regression coefficients of social participation score, 95% confidence intervals (CIs), and two-sided p-values for each 1-point increase in MWI as well as MWI quartiles. P-values less than 0.05 were considered statistically significant. We used the coefficient of determination (R2) to indicate the proportion of variance in social participation explained by multimorbidity in each model. All analyses were completed using SAS version 9.4 (SAS Institute, Cary, NC, 2013).
RESULTS
Study population
Our final sample included 12,825 participants with complete data on MWI and social participation (7,529 participants in 2014 and 5,296 in 2016). In 2014, 51% of HRS respondents were eligible to complete the PLQ and 49% were eligible in 2016. We excluded 2.8% (N=358) of individuals for completing less than half the questions needed to robustly compute scores for purpose in life (N=265), life satisfaction (N=118), and both (N=25).
The mean age was 69.3 (standard deviation (SD) 10.6) years. Most participants were white, non-Hispanic, married, and not working. The mean MWI was 8.1 (SD 6.6). Participants had a mean social participation score of 101.3 (SD 16.0), mean purpose in life score of 4.6 (SD 1.0), and mean life satisfaction score of 5.0 (SD 1.5) (Table 2).
Table 2.
Participant Characteristics in the Health and Retirement Study, 2014 and 2016
| N=12,825 | |||
|---|---|---|---|
| Characteristic | No. (%) | Mean | SD |
|
| |||
| Age, years | 69.3 | 10.6 | |
|
| |||
| Sex, female | 7693 (60.0) | ||
|
| |||
| Race/ethnicity | |||
| White, non-Hispanic | 8682 (67.7) | ||
| Black, non-Hispanic | 2180 (17.0) | ||
| Hispanic | 958 (7.47) | ||
| Other/unknown | 1005 (7.84) | ||
|
| |||
| Household net worth, $ | |||
| ≤14,000 | 2827 (22.0) | ||
| 14,001–113,000 | 3057 (23.8) | ||
| 113,001–323,700 | 3394 (26.5) | ||
| ≥323,701 | 3547 (27.7) | ||
|
| |||
| Education, years | |||
| <12 | 2257 (17.7) | ||
| 12 | 4087 (32.0) | ||
| 13–15 | 3163 (24.8) | ||
| ≥16 | 3261 (25.5) | ||
|
| |||
| Marital/living status | |||
| Married | 7544 (58.8) | ||
| Annulled/separated/divorced | 2030 (15.8) | ||
| Widowed | 2516 (19.6) | ||
| Never married | 713 (5.6) | ||
| Other | 22 (0.2) | ||
| Employment status | |||
| Working | 3927 (30.6) | ||
| Not working | 8897 (69.4) | ||
|
| |||
| Multimorbidity-Weighted Index quartile, 0–46.2 | 8.1 | 6.6 | |
| 0–3.01 | 2912 (22.7) | ||
| 3.02–6.62 | 3180 (24.8) | ||
| 6.63–11.74 | 3202 (25.0) | ||
| >11.74 | 3531 (27.5) | ||
|
| |||
| Social participation score, 21–147 | 101.3 | 16.0 | |
|
| |||
| Purpose in life score, 1–6 | 4.6 | 1.0 | |
|
| |||
| Life satisfaction score, 1–7 | 5.0 | 1.5 | |
Abbreviations: SD, standard deviation
Social participation
Respondents participated in an average of 9.5 (SD 3.5) activities regularly. Regular participation was defined as reporting participation in the activity at least once per month. Of these activities, the most common were watching television (97.1% of respondents), reading books, magazines, or newspapers (90.9%), praying privately in places other than a church or synagogue (73.0%), and doing home or car maintenance or gardening (72.5%) (Table 1). The least common activities reported regularly were participating in a local community arts group (10.0%), making clothes, knitting, embroidering, etc. (12.6%), attending an educational or training course (12.7%), and volunteering with children or young people (14.0%).
Multimorbidity and social participation
Each 1-point increase in MWI was associated with a 0.39 point (95% CI: −0.43, −0.34) lower social participation score in the unadjusted model (Table 3). After adjustment, each 1-point increase in MWI was associated with a 0.19 point (95% CI: −0.23, −0.14) lower social participation score. This was equivalent to the effect of one year of aging on social participation for the same participant in adjusted models.
Table 3.
Regression Coefficients Describing the Association Between Multimorbidity-Weighted Index and Social Participation Among Health and Retirement Study Participants, 2010–2014 and 2012–2016
| Models | Social Participation Score N=12,825 | |||
|---|---|---|---|---|
|
| ||||
| Regression coefficient | 95% CI | P-value | R2 | |
|
| ||||
| Unadjusted Model MWI, continuous | −0.39* | (−0.43, −0.34) | <0.001 | 0.025 |
| MWI, quartiles | 0.024 | |||
| Q4 | −6.39* | (−7.17, −5.62) | <0.001 | |
| Q3 | −3.07* | (−3.86, −2.28) | <0.001 | |
| Q2 Q1 (reference) |
−1.13* | (−1.93, −0.34) | 0.005 | |
|
| ||||
| Adjusted Model1 MWI, continuous |
−0.19* | (−0.23, −0.14) | <0.001 | 0.21 |
| MWI, quartiles | 0.21 | |||
| Q4 | −2.56* | (−3.33, −1.80) | <0.001 | |
| Q3 | −0.56 | (−1.31, 0.20) | 0.15 | |
| Q2 Q1 (reference) |
−0.03 | (−0.76, 0.70) | 0.93 | |
|
| ||||
| Adjusted Model1 with Purpose in Life MWI, continuous |
−0.09* | (−0.13, −0.05) | <0.001 | 0.27 |
| MWI*Purpose in life | 0.11* | (0.07, 0.14) | <0.001 | |
|
| ||||
| Adjusted Model1 with Life Satisfaction MWI, continuous |
−0.12* | (−0.16, −0.08) | <0.001 | 0.23 |
| MWI*Life satisfaction | 0.04* | (0.02, 0.07) | <0.001 | |
Abbreviations: MWI, multimorbidity-weighted index; CI, confidence interval; Q, quartile
Adjusted for age, sex, education, household net worth, race/ethnicity, marital status, employment status, and calendar time.
For MWI as a categorical variable, there was a monotonic gradient of worse social participation with higher MWI. In the unadjusted model, social participation score was poorer, on average, among participants in higher MWI quartiles: quartile 4 had worse social participation by 6.39 points (95% CI: −7.17, −5.62), quartile 3 by 3.07 points (95% CI: −3.86, −2.28), and quartile 2 by 1.13 points (95% CI: −1.93, −0.34) compared with quartile 1 (Table 3). In the adjusted model, the association of higher MWI with poorer social participation was statistically significant for quartile 4 vs. quartile 1 only (χ= −2.56, 95% CI: −3.33, −1.80). The effect of the highest quartile of MWI on social participation was approximately ten times greater than the effect of one year of age on social participation in the same participant in adjusted models (β=−0.24, 95% CI: −0.21, 0.27).
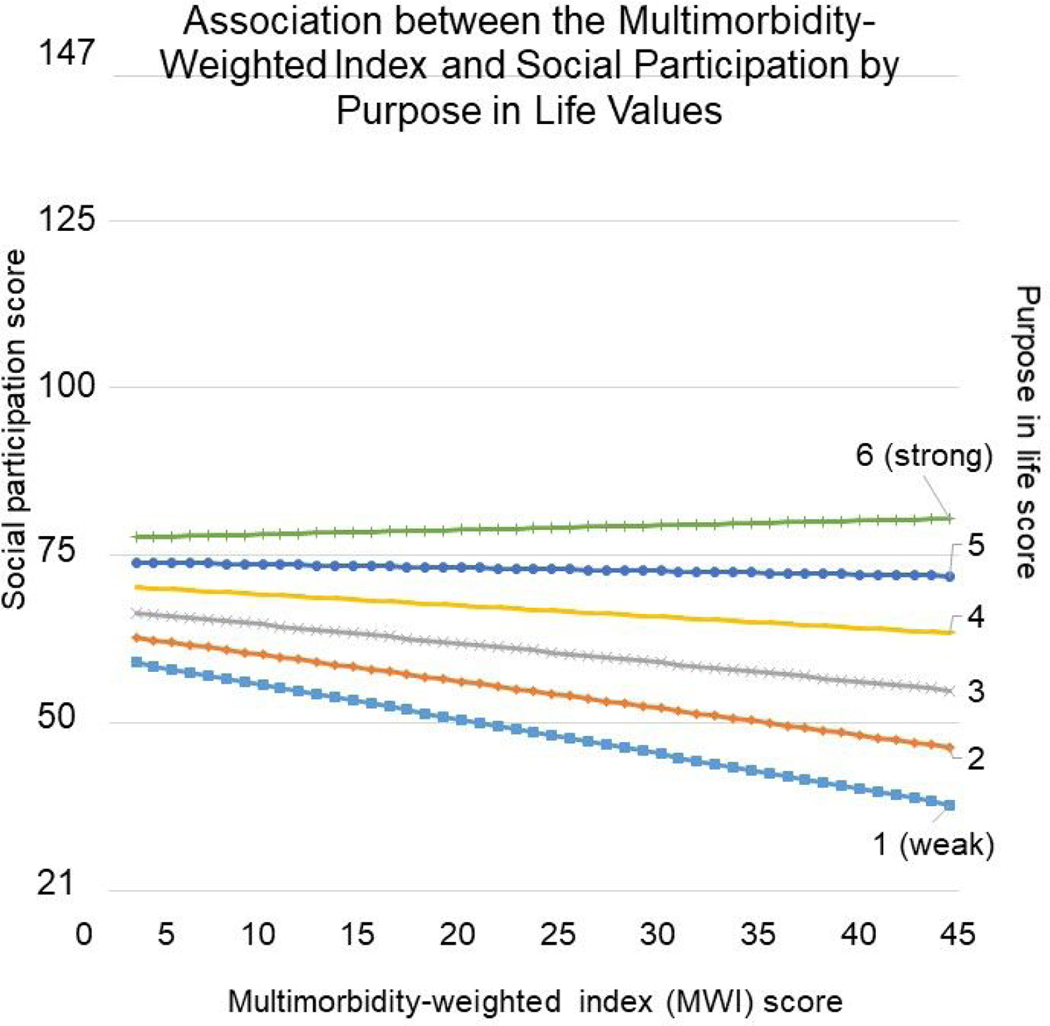
Effect modification: purpose in life and life satisfaction
Both purpose in life and life satisfaction independently modified the association between MWI and social participation. Among participants with average purpose in life, each point increase in MWI was associated with a 0.09 point (95% CI: −0.13, −0.05) worse social participation score. This was approximately equal to the effect of 0.5 years of aging on social participation in the same participant in adjusted models. Per 1-point increase in MWI, those with above average purpose in life experienced better social participation by 0.11 points (95% CI: 0.07, 0.14) compared to those with below average purpose in life (Figure 3).
Figure 3.
Association between the Multimorbidity-Weighted Index and Social Participation by Purpose in Life Values in the Health and Retirement Study, 2010–2014 and 2012–2016
*Among participants with above average purpose in life (>4.6), social participation score does not decrease with increased MWI. Among participants with average or below average purpose in life (<=4.6), social participation score is decreased with increased MWI.
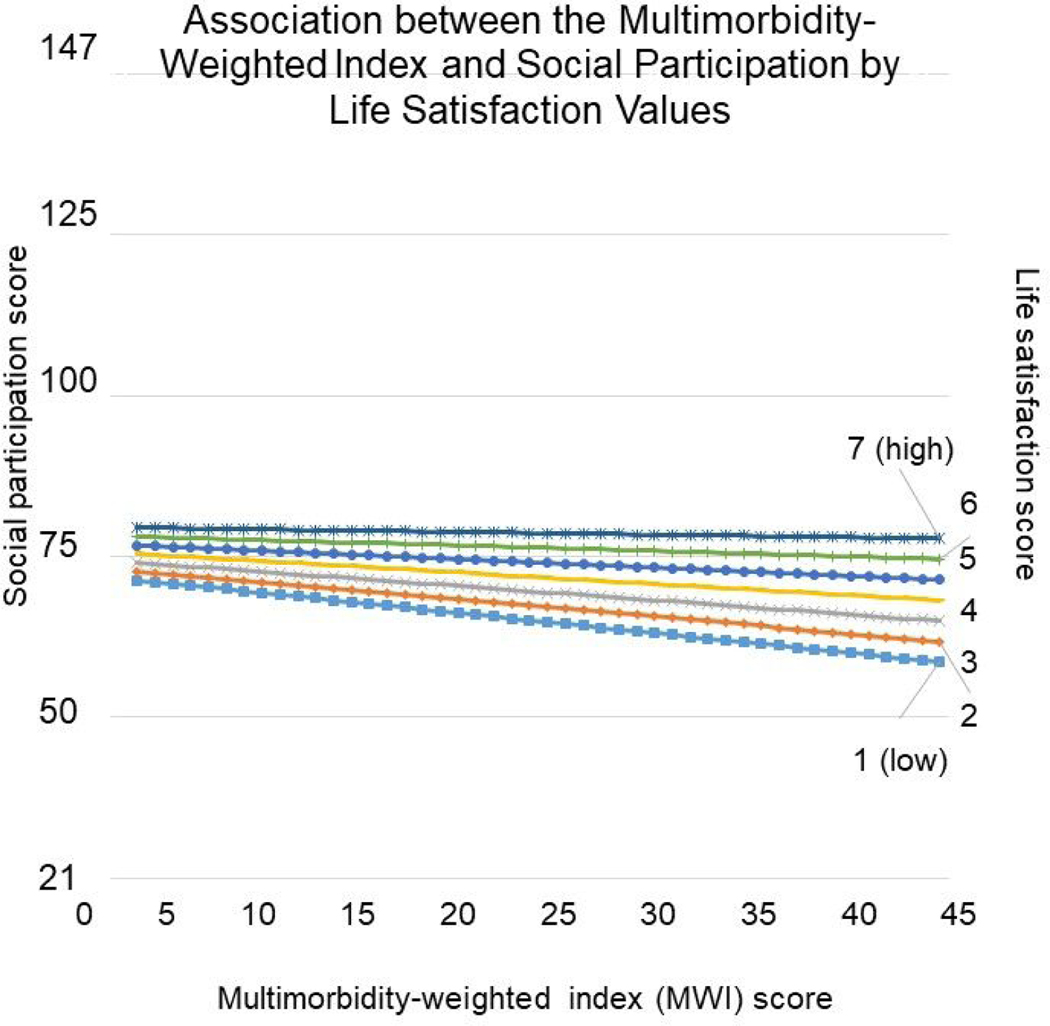
Similarly, the association between MWI and social participation differed depending on the level of life satisfaction. Among participants with average life satisfaction, each point increase in MWI was associated with a 0.12 point (95% CI: −0.16, −0.08) worse social participation score. As with purpose in life, this was equivalent to slightly less than the effect of 0.5 years of aging on social participation (β=−0.26, 95% CI: −0.23, −0.29). Conversely, among participants with above average life satisfaction, each 1-point increase in MWI was associated with a 0.04 point (95% CI: 0.02, 0.07) better social participation score (Figure 4) compared to participants with below average life satisfaction.
Figure 4.
Association between the Multimorbidity-Weighted Index and Social Participation by Life Satisfaction Values in the Health and Retirement Study, 2010–2014 and 2012–2016
*Among participants with above average life satisfaction (>5), social participation score does not decrease with increased MWI. Among participants with average or below average life satisfaction (<=5), social participation score is decreased with increased MWI.
The model including both pairs of interactions (MWI with purpose in life, and MWI with life satisfaction), and the simultaneous interaction between MWI, purpose in life, and life satisfaction yielded similar results to the model that assessed MWI with purpose in life separately (Supplemental Table 1).
DISCUSSION
In this nationally representative sample of 12,825 Americans ages ≥51 years, multimorbidity was associated with less participation in social activities. However, this was attenuated and even reversed among adults who reported above average purpose in life or life satisfaction. Those with above average purpose in life or life satisfaction had better social participation than those with below average purpose in life or life satisfaction for comparable values of multimorbidity.
Our study supports and extends existing literature about the association between multimorbidity and social participation and aligns with the ICF continuum of functioning and disability. Prior studies have reported that individuals with multimorbidity participated in fewer social activities, including formal learning (Golinowska et al., 2016) and social leisure activities outside the home (e.g., attending clubs/meetings and visiting friends) (Galenkamp et al., 2016; Qin et al., 2015), compared to those without multimorbidity. These studies measured multimorbidity in discrete categories (e.g., 2 or more chronic conditions vs. less than 2 chronic conditions) at one time point. Our analysis corroborates these findings and contributes further in three key ways. First, we measured cumulative multimorbidity over 4 years through a validated MWI that weights conditions by physical functioning to provide a more precise and patient-centered measure of disease burden. Second, our assessment of multimorbidity both linearly and categorically allowed us to see the effect of all values of multimorbidity on social participation, rather than only categorically like the prior studies. Third, our measurement of social participation was a composite score based on an inventory of cognitively, physically, and socially stimulating activities and their frequencies. The activities included in the measure are directly classified to Levasseur et al.’s taxonomy of social activities (Levasseur et al., 2010), providing a multidimensional picture of social participation among middle-aged and older adults. This is a more comprehensive measure of social participation compared with other studies.
Further, we provide new evidence that the association between multimorbidity and social participation is moderated by purpose in life and life satisfaction. Multiple pathways may explain the mechanism by which individuals with multimorbidity and above average purpose in life and/or life satisfaction maintain high social participation. First, strong purpose in life has been associated with healthier lifestyle behaviors, including disease treatment adherence (Hooker & Masters, 2016), which may better enable individuals to continue participating in social activities despite their multimorbidity burden. Second, strong purpose in life has also been associated with lower allostatic load (Zilioli et al., 2015) such that individuals with above average purpose in life may experience slower rates of progression in their multimorbidity, thereby allowing them to maintain and adapt to their current burden of multimorbidity and associated lifestyle. Third, above average purpose in life and/or life satisfaction may serve as a proxy for increased resilience or better coping with multimorbidity, therefore allowing continued social participation. Last, social participation is self-reported and potentially subject to bias. For example, adults with strong subjective and psychological well-being may more thoroughly report their participation in social activities than individuals who experience decreased well-being.
Simple interventions to improve subjective and psychological well-being have been successful among older adults. A program to increase older adults’ reminiscence ability, or activation of their autobiographical memories, significantly improved participants’ life satisfaction and psychological well-being. The treatment involved 2 hour per week group sessions for 10 weeks with a trained psychologist and the positive effects persisted for at least 3 months after program conclusion (Viguer et al., 2017). For older adults with low social participation, improved savoring ability, or ability to appreciate one’s positive life experiences, may also enhance satisfaction and enjoyment from their experiences (Smith et al., 2020). A 1-week savoring intervention requesting that participants think about something positive for 5 minutes twice per day improved measures of psychological well-being among older adults, including happiness and resilience (Smith & Hanni, 2019). Resilience is directly linked to life satisfaction, so this could be a useful intervention with mental health providers to foster greater social participation (Reyes et al., 2020). Similar programs could be easily implemented in long-term care facilities or community settings for older adults, allowing those with high multimorbidity to better experience the benefits of even minimal social participation.
This study has limitations. First, there are several possible ways to define social participation. While some use a strict definition that participation in social activities must be done in the presence of other people, we examined a more multifaceted definition of social participation that encompasses micro (personal) to macro (societal) levels (Levasseur et al., 2010). PLQ responses are also self-reported, so we are unable to verify actual levels of social participation among respondents. Second, multimorbidity was limited to only diseases assessed in the HRS and is likely an underestimate of multimorbidity, but this is a limitation of most national surveys. Third, the association between multimorbidity and social participation was assessed at one time. We were unable to use time-varying measures of social participation, life satisfaction, and purpose in life because PLQ data are only available longitudinally every 4 years; therefore, there were insufficient data to measure changes over time following our exposure of multimorbidity. However, we captured multimorbidity longitudinally over 4 years for two HRS waves. Future studies may examine the longitudinal association of multimorbidity and social participation with repeated measures of both. Fourth, the social participation measure from the PLQ did not explicitly include religious activities aside from praying privately, and religious participation is common among adults with multimorbidity (Sowa et al., 2016). Had we included religious participation, social participation may have been greater among those with multimorbidity. Lastly, data became sparse as MWI became greater than 30 so any conclusions about these participants should be drawn cautiously.
CONCLUSION
In this large, nationally representative sample, high multimorbidity was associated with lower participation in social activities, but this was attenuated and even reversed by above average purpose in life and life satisfaction. This study contributes to growing evidence of the detrimental and far-reaching impact of multimorbidity on middle-aged and older adults. Despite the high prevalence and morbidity and mortality associated with multimorbidity, successful interventions to delay the onset and progression of multimorbidity and its complications are lacking. We report that greater purpose in life and life satisfaction may be protective of the impact of increased multimorbidity on decreased social participation. Small-scale, positive psychological interventions that improve subjective and psychological well-being should be assessed to enhance the benefits of social participation among older adults with any degree of multimorbidity.
Supplementary Material
Acknowledgements:
These findings were presented at the Society of General Internal Medicine Annual Meeting, May 2019.
Funding statement: This work was supported by K23AG056638 and U01AG009740 from the National Institutes of Health.
Abbreviations:
- HRS
Health and Retirement Study
- HRQOL
Health-related quality of life
- PLQ
Psychosocial and Lifestyle Questionnaire
- MWI
Multimorbidity-Weighted Index
Footnotes
IRB name and approval number: University of Michigan Medical School IRB, HUM00128383. Informed consent was not required.
Conflict of Interest: None to declare.
REFERENCES
- Alimujiang A, Wiensch A, Boss J, Fleischer NL, Mondul AM, McLean K, Mukherjee B, & Pearce CL (2019). Association Between Life Purpose and Mortality Among US Adults Older Than 50 Years. JAMA Network Open, 2(5), e194270–e194270. 10.1001/jamanetworkopen.2019.4270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ang S. (2018). Social participation and health over the adult life course: Does the association strengthen with age? Social Science and Medicine, 206, 51–59. 10.1016/j.socscimed.2018.03.042 [DOI] [PubMed] [Google Scholar]
- Bourassa KJ, Memel M, Woolverton C, & Sbarra DA (2017). Social participation predicts cognitive functioning in aging adults over time: comparisons with physical health, depression, and physical activity. Aging & Mental Health, 21(2), 133–146. 10.1080/13607863.2015.1081152 [DOI] [PubMed] [Google Scholar]
- Bowling A. (1995). What things are important in people’s lives? A survey of the public’s judgements to inform scales of health related quality of life. Social Science and Medicine, 41(10), 1447–1462. 10.1016/0277-9536(95)00113-L [DOI] [PubMed] [Google Scholar]
- Diener E, Emmons RA, Larsen RJ, & Griffin S. (1985). The Satisfaction With Life Scale. Journal of Personality Assessment, 49(1), 71–75. 10.1207/s15327752jpa4901_13 [DOI] [PubMed] [Google Scholar]
- Dong X, Li Y, & Simon MA (2014). Social engagement among U.S. Chinese older adults--findings from the PINE Study. Journals of Gerontology. Series A: Biological Sciences and Medical Sciences, 69 Suppl 2, S82–89. 10.1093/gerona/glu152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fokkema T, & Knipscheer K. (2007). Escape loneliness by going digital: A quantitative and qualitative evaluation of a Dutch experiment in using ECT to overcome loneliness among older adults. Aging & Mental Health, 11(5), 496–504. 10.1080/13607860701366129 [DOI] [PubMed] [Google Scholar]
- Fortin M, Lapointe L, Hudon C, Vanasse A, Ntetu AL, & Maltais D. (2004). Multimorbidity and quality of life in primary care: a systematic review. Health Qual Life Outcomes, 2, 51–51. 10.1186/1477-7525-2-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galenkamp H, & Deeg D. (2016). Increasing social participation of older people: are there different barriers for those in poor health? Introduction to the special section. Eur J Ageing, 13(2), 87–90. 10.1007/s10433-016-0379-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galenkamp H, Gagliardi C, Principi A, Golinowska S, Moreira A, Schmidt A, Winkelmann J, Sowa A, van der Pas S, & Deeg D. (2016). Predictors of social leisure activities in older Europeans with and without multimorbidity. Eur J Ageing, 13(2), 129–143. 10.1007/s10433-016-0375-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerst-Emerson K, & Jayawardhana J. (2015). Loneliness as a public health issue: the impact of loneliness on health care utilization among older adults. Am J Public Health, 105(5), 1013–1019. 10.2105/AJPH.2014.302427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass TA, de Leon CM, Marottoli RA, & Berkman LF (1999). Population based study of social and productive activities as predictors of survival among elderly Americans. BMJ, 319(7208), 478–483. 10.1136/bmj.319.7208.478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golinowska S, Sowa A, Deeg D, Socci M, Principi A, Rodrigues R, Ilinca S, & Galenkamp H. (2016). Participation in formal learning activities of older Europeans in poor and good health. Eur J Ageing, 13(2), 115–127. 10.1007/s10433-016-0371-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Q, Cui Y, Liang L, Zhong Q, Li J, Li Y, Lv X, & Huang F. (2017). Social participation, willingness and quality of life: A population-based study among older adults in rural areas of China. Geriatr Gerontol Int, 17(10), 1593–1602. 10.1111/ggi.12939 [DOI] [PubMed] [Google Scholar]
- Hill TD, Angel JL, Ellison CG, & Angel RJ (2005). Religious attendance and mortality: an 8-year follow-up of older Mexican Americans. Journals of Gerontology. Series B: Psychological Sciences and Social Sciences, 60(2), S102–109. 10.1093/geronb/60.2.s102 [DOI] [PubMed] [Google Scholar]
- Hooker SA, & Masters KS (2016). Purpose in life is associated with physical activity measured by accelerometer. Journal of Health Psychology, 21(6), 962–971. 10.1177/1359105314542822 [DOI] [PubMed] [Google Scholar]
- Levasseur M, Richard L, Gauvin L, & Raymond E. (2010). Inventory and analysis of definitions of social participation found in the aging literature: proposed taxonomy of social activities. Social Science and Medicine, 71(12), 2141–2149. 10.1016/j.socscimed.2010.09.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques A, Peralta M, Gouveia ER, Chavez FG, & Valeiro MG (2018). Physical activity buffers the negative relationship between multimorbidity, self-rated health and life satisfaction. J Public Health (Oxf), 40(3), e328–e335. 10.1093/pubmed/fdy012 [DOI] [PubMed] [Google Scholar]
- Musich S, Wang SS, Kraemer S, Hawkins K, & Wicker E. (2018). Purpose in Life and Positive Health Outcomes Among Older Adults. Popul Health Manag, 21(2), 139–147. 10.1089/pop.2017.0063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Principi A, Galenkamp H, Papa R, Socci M, Suanet B, Schmidt A, Schulmann K, Golinowska S, Sowa A, Moreira A, & Deeg DJH (2016). Do predictors of volunteering in older age differ by health status? Eur J Ageing, 13(2), 91–102. 10.1007/s10433-016-0377-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin J, Theis KA, Barbour KE, Helmick CG, Baker NA, & Brady TJ (2015). Impact of arthritis and multiple chronic conditions on selected life domains - United States, 2013. MMWR: Morbidity and Mortality Weekly Report, 64(21), 578–582. [PMC free article] [PubMed] [Google Scholar]
- Reyes MF, Satorres E, & Meléndez JC (2020). Resilience and Socioeconomic Status as Predictors of Life Satisfaction and Psychological Well-Being in Colombian Older Adults. J Appl Gerontol, 39(3), 269–276. 10.1177/0733464819867554 [DOI] [PubMed] [Google Scholar]
- Ryff CD (1989). Happiness is everything, or is it? Explorations on the meaning of psychological well-being. Journal of Personality and Social Psychology, 57(6), 1069–1081. 10.1037/0022-3514.57.6.1069 [DOI] [Google Scholar]
- Sano N, & Kyougoku M. (2016). An analysis of structural relationship among achievement motive on social participation, purpose in life, and role expectations among community dwelling elderly attending day services. PeerJ, 4, e1655. 10.7717/peerj.1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh A, & Misra N. (2009). Loneliness, depression and sociability in old age. Ind Psychiatry J, 18(1), 51–55. 10.4103/0972-6748.57861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J, Ryan L, Sonnega A, & Weir D. (2017). HRS Psychosocial and Lifestyle Questionnaire 2006–2016. https://hrs.isr.umich.edu/publications/biblio/9066
- Smith JL, Bihary JG, O’Connor D, Basic A, & O’Brien CJ (2020). Impact of Savoring Ability on the Relationship Between Older Adults’ Activity Engagement and Well-Being. J Appl Gerontol, 39(3), 323–331. 10.1177/0733464819871876 [DOI] [PubMed] [Google Scholar]
- Smith JL, & Hanni AA (2019). Effects of a Savoring Intervention on Resilience and Well-Being of Older Adults. J Appl Gerontol, 38(1), 137–152. 10.1177/0733464817693375 [DOI] [PubMed] [Google Scholar]
- Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, & Weir DR (2014). Cohort Profile: the Health and Retirement Study (HRS). International Journal of Epidemiology, 43(2), 576–585. 10.1093/ije/dyu067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sowa A, Golinowska S, Deeg D, Principi A, Casanova G, Schulmann K, Ilinca S, Rodrigues R, Moreira A, & Gelenkamp H. (2016). Predictors of religious participation of older Europeans in good and poor health. Eur J Ageing, 13, 145–157. 10.1007/s10433-016-0367-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stålbrand IS, Svensson T, Elmståhl S, Horstmann V, Hagberg B, Dehlin O, & Samuelsson G. (2007). Subjective health and illness, coping and life satisfaction in an 80-year-old swedish population-implications for mortality [journal article]. International Journal of Behavioral Medicine, 14(3), 173–180. 10.1007/bf03000189 [DOI] [PubMed] [Google Scholar]
- Tomioka K, Kurumatani N, & Hosoi H. (2016). Relationship of Having Hobbies and a Purpose in Life With Mortality, Activities of Daily Living, and Instrumental Activities of Daily Living Among Community-Dwelling Elderly Adults. Journal of Epidemiology, 26(7), 361–370. 10.2188/jea.JE20150153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Utz RL, Carr D, Nesse R, & Wortman CB (2002). The effect of widowhood on older adults’ social participation: an evaluation of activity, disengagement, and continuity theories. Gerontologist, 42(4), 522–533. 10.1093/geront/42.4.522 [DOI] [PubMed] [Google Scholar]
- van Genderen S, Plasqui G, van der Heijde D, van Gaalen F, Heuft L, Luime J, Spoorenberg A, Arends S, Lacaille D, Gignac M, Landewe R, & Boonen A. (2018). Social Role Participation and Satisfaction With Life: A Study Among Patients With Ankylosing Spondylitis and Population Controls. Arthritis Care & Research, 70(4), 600–607. 10.1002/acr.23304 [DOI] [PubMed] [Google Scholar]
- Viguer P, Satorres E, Fortuna FB, & Meléndez JC (2017). A Follow-Up Study of a Reminiscence Intervention and Its Effects on Depressed Mood, Life Satisfaction, and Well-Being in the Elderly. J Psychol, 151(8), 789–803. 10.1080/00223980.2017.1393379 [DOI] [PubMed] [Google Scholar]
- Ware JE Jr. (1993). SF-36 health Survey Manual and Interpretation Guide. The Health Institute, New England Medical Center Hospitals, Inc. [Google Scholar]
- Wei M, Kabeto M, Galecki A, & Langa K. (2019). Physical Functioning Decline and Mortality in Older Adults With Multimorbidity: Joint Modeling of Longitudinal and Survival Data. Journals of Gerontology. Series A: Biological Sciences and Medical Sciences, 74(2), 226–232. 10.1093/gerona/gly038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei M, Kabeto M, Langa K, & Mukamal K. (2018). Multimorbidity and physical and cognitive function: performance of a new multimorbidity-weighted index. Journals of Gerontology. Series A: Biological Sciences and Medical Sciences, 73(2), 225–232. 10.1093/gerona/glx114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei M, Levine D, Zahodne L, Kabeto M, & Langa K. (2019). Multimorbidity and cognitive decline over 14 years in older Americans. Journals of Gerontology. Series A: Biological Sciences and Medical Sciences 10.1093/gerona/glz147 [DOI] [PMC free article] [PubMed]
- Wei M, & Mukamal K. (2019). Multimorbidity and Mental Health-Related Quality of Life and Risk of Completed Suicide. Journal of the American Geriatrics Society, 67(3), 511–519. 10.1111/jgs.15678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei M, & Mukamal KJ (2018). Multimorbidity, Mortality, and Long-Term Physical Functioning in 3 Prospective Cohorts of Community-Dwelling Adults. American Journal of Epidemiology, 187(1), 103–112. 10.1093/aje/kwx198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2002). Towards a Common Language for Functioning, Disability and Health: The International Classification of Functioning, Disability and Health. Retrieved 2020 August from http://www.who.int/classifications/icf/icfbeginnersguide.pdf?ua=1
- Zilioli S, Slatcher RB, Ong AD, & Gruenewald TL (2015). Purpose in life predicts allostatic load ten years later. Journal of Psychosomatic Research, 79(5), 451–457. 10.1016/j.jpsychores.2015.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.