Abstract
The vision loss in the Traumatic Optic Neuropathy is the impact of deformational forces. This occurs due to direct or indirect injuries during trauma to skull. The use of high dose corticosteroids is the primary line of treatment in such injuries still remains a matter of debate. Traumatic Optic Neuropathy is yet an unexplored topic of study in Ayurveda. The Traumatic Optic Neuropathy can be correlated with Abhighatajanya Vataprakopaj Drishtinash. The treatment principles of Vataprakopaj Vyadhi are Snehan (massage), Swedan (sudation), Basti (enema) and Nasya (oleation through nasal route). A 50 year old male patient came to outpatient department suffered from motorcycle accident and had a forehead trauma followed by loss of vision in both eyes after 5 days and diagnosed as Traumatic Optic Neuropathy. An electrophysiological assessment showed absence of waveform in Visual Evoked Potential (VEP). According to Ayurveda patient was diagnosed primarily as Abhighatajanya Vataprakopaj Drishtinash and started to follow the protocol of Vataprakopaj Vyadhi. Patient received Ayurvedic formulations in morning, after meal and at night for 12 months and a course of Yapan Basti (medicated decoction enema) followed by Netratarpan (eye satiation), Nasya and Abhyanga (body and foot massage). Patient showed an improvement in the visual quality from no perception of light to perception of light and rays in right eye in 9 month. Patient had improvement in P100 latencies of right eye in VEP report and subjective improvement in quality of vision to perceive the images and objects. Application of Ayurvedic principles and Panchakarma therapy resulted in improvement of the case. An early management of Traumatic Optic Neuropathy with Ayurvedic treatment can have a significant impact on the clinical/visual outcome in terms of recovery in damaged optic nerve fibers.
Keywords: Traumatic Optic Neuropathy, Abhighatajanya Drishtinash, Basti, Nasya, Netratarpan, Visual Evoked Potential (VEP)
1. Introduction
Traumatic Optic Neuropathy (TON) is a result of head trauma which may be moderate or severe and mostly associated with little or no evidence of head injury. Traumatic Optic Neuropathy occurs in approximately 0.5–5% of closed head injury [1] and in 2.25% of patients with maxillofacial trauma and mid face fractures [2]. Loss of consciousness is associated with TON in 20–75% of cases [3,4]. Forehead and supraorbital injuries are the main contributing factors in causing blindness in closed head injuries while temporal region injuries are less common. Younger people between 20 and 50 years of age are the major sufferers of TON in major trauma population [5]. The prevalence of severe initial visual loss ranges from about 43 to 56%. Visual loss may present with no light perception (NLP) to 20/20 with an associated visual field defect. More severe visual loss is associated with optic canal fractures [6].
Deceleration injuries which are directed to ipsilateral forehead or mid face region from motor vehicle or bicycle accident is most common cause of TON in 17–63% cases. Among these motorcycle accidents is the most common followed by falls in 50% of cases. Assault, gunshot wound, falling objects, skateboarding and minor head injuries are the other causes of TON. The other iatrogenic causes are endoscopic sinus surgery or orbital surgery [7].
The treatment options are limited to the use of corticosteroids with variable doses, optic nerve decompression surgery, use of both corticosteroids as well as surgery or observation only without treatment [8]. Data regarding the randomized clinical trial for TON is deficient. The use of corticosteroids and optic nerve decompression does not shown any visual benefit instead add up to the risk in patients of TON [9]. A case series published recently showed a noticeable effect in visual outcome with intravenous erythropoietin in indirect TON [10]. The visual prognosis in cases of TON is mostly depend upon the time lost between trauma and treatment. So it is important for the patient to seek medical treatment at earliest in such cases [11].
Ayurveda is a traditional Indian system of medicine with holistic approach towards health and having a strong philosophical and empirical base. However, the role of Ayurveda always remained limited to chronic illness and lifestyle disorders in society. The subtle principles of Ayurveda certainly have potential in managing ophthalmic disorders. There are some clinical trials that evaluated the role of internal medication and local therapy for improvement of lost retinal sensitivity or delay in progression of neuropathy demonstrated in glaucoma [12,13]. TON is yet an unexplored topic of study in Ayurveda. According to Ayurveda, TON can be correlated with Abhighatajanya Vataprakopaj Drishtinash.
A case discussed here is of a patient, who met with road accident and as a result developed anterior visual pathway defect leading to secondary optic atrophy in both eyes. A thorough clinical history was taken according to Ayurvedic perspective and was diagnosed as Abhighatajanya Vataprakopaj Drishtinash. The treatment protocol for Vataprakopaj Vyadhi (diseases occur due to Vata vitiation) was initiated [14]. [Sutrasthana 13/1–3]. Patient received internal Ayurvedic medication for one year and a course of Yapana Basti, Netratarpan, Nasya and application of medicated oil body massage during the course of treatment.
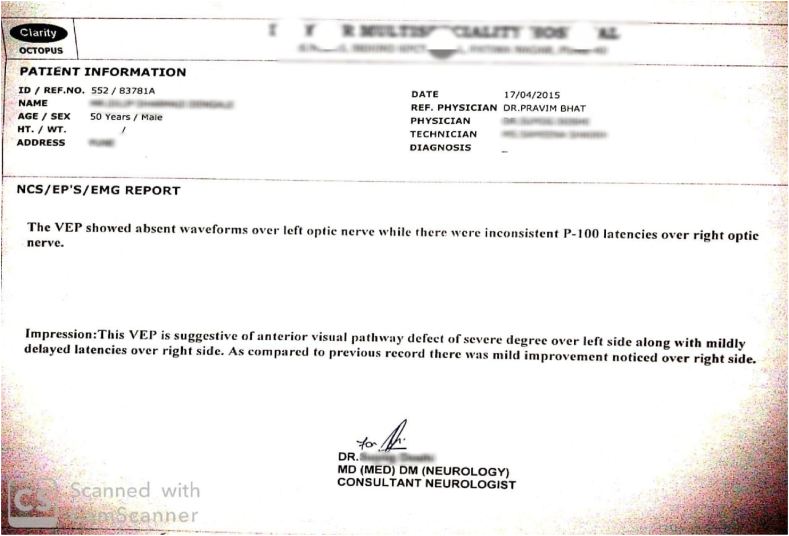
An improvement was observed in vision from no PL to perception of light and rays in right eye and VEP report which showed positive waveform in right eye and absence of waveform in the left eye. The main purpose of this case presentation is to report the impact of Ayurveda treatment with proper diagnosis in stimulating damaged nerve fibers.
1.1. Case report
A 50 years old male patient working as marketing executive visited to OPD with complaint of bilateral loss of vision since 10 days. Patient was having hypertension since 2 years and was prescribed Tab. Telmisartan 20 mg once in a day. He had a motorcycle accident on 25/06/2014. He visited to OPD for Ayurveda treatment on 10/07/2014 and was hospitalized for the same. He had closed lacerated wound on left side of forehead that was sutured during hospitalization. He had taken a course of antibiotics and analgesics for five days for CLW. Sutures were removed after 10 days and wound was healed.
2. Findings
2.1. General examination
Patient had no other major injury, no vomiting, and no unconsciousness after accident. His pulse was 80/minute and blood pressure was 130/80 mmhg. He was not having any addiction. He felt diminution of vision in both eyes from second day after accident which led to complete loss of vision after 5 days of injury.
2.2. Local examination
On local examination his both eye anterior segment was within normal limit but patent had rapid afferent pupillary pathway defect (RAPD) with sluggish pupillary reaction. There was no corneal abrasion (fluorescein test for corneal ulcer-negative) or apparent external injury noted in both eyes. Intraocular pressure of right eye was 14.6 mmHg while that of left eye was 17.3 mmHg taken with Schiotz tonometer (Riester, Germany). On mydriasis, direct ophthalmoscopy (Heine Beta 200, Germany) was conducted. Media from both eyes was clear with pale atrophic optic disc on both side.
2.3. Systemic examination
Patient was conscious and oriented about date, time and place. upon examination, his respiratory and cardiovascular system functioning was found to be normal. His Nadi (pulse) was Vata Pradhan and Pittanubandhi, Jivha (tongue) coated, Shabda (∼speech) was normal, Drik (vision) - loss of vision and Akriti (built) was medium.
2.4. Investigations
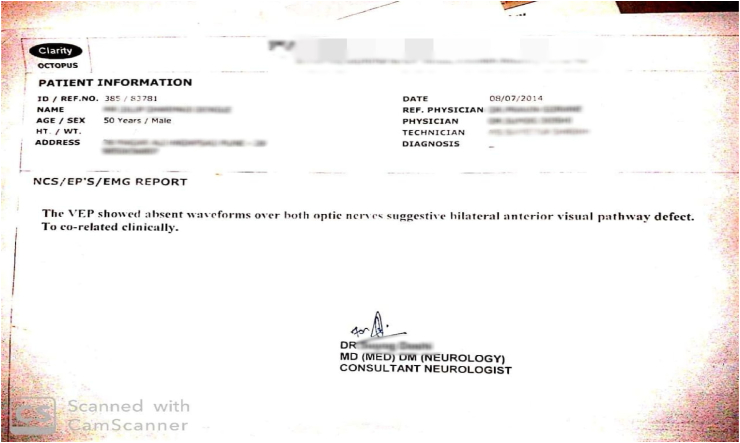
MRI- within normal limit. Visual Evoked Potential (VEP) was showing absent waveform over both optic nerves suggestive of bilateral anterior visual pathway defect. Blood and urine profile was within normal range.
2.5. Diagnosis
Diagnosis was done on the basis of VEP report as anterior visual pathway defect leading to optic atrophy. MRI ruled out other possibilities of optic neuritis, optic nerve avulsion, optic nerve inflammation, optic nerve sheath hematoma, orbital fractures, orbital hematoma, orbital tumors and sinusitis with orbital involvement. According to Ayurveda, patient was diagnosed as Abhighatajanya Vataprakopaj Drishtinash and given the treatment protocol of Vataprakopaj Vyadhi including Snehan (application of medicated oil on body), Swedan (steam bath).
-
•
Dosha: Vata
-
•
Dushya: Asthi, Majja
2.6. Therapeutic intervention
Patient received internal/oral medication (Table 1) along with Panchakarma and thereafter local treatment (Table 2). The internal medication treatment plan was initiated on patient's first visit to the OPD (10/07/2014). The follow up observations and outcomes are summarized in Table 3.
Table 1.
Internal medication- Treatment plan and rationale of formulation.
| Sr. No | Formulation with doses | Anupana (∼compliant) | Time of administration | Rationale of formulation |
|---|---|---|---|---|
| 1 |
Vasanta Kusumakar (125 mg), Roupyatapyadi Louha (250 mg), Vidari Churna (250 mg) |
Jeevanthyadi Ghrita 10 ml. | Pratah Kala (morning) | Santarpan (nourishment of tissue) and Rasayan (rejuvenation) |
| 2 |
Sitopaladi Churna (250 mg), Brihat Vata Chintamani (125 mg), Saptamrit Roupya (250 mg), Mahayogaraj Guggulu (125 mg), Punarnava Churna (250 mg) |
Pathyadi Kwath (20 ml). | Vyanodan Kala (after meal-afternoon & evening) | Vata pacifying, Deepan, Pachan (stimulate and enhance the digestive fire) |
| 3 |
Triphala (250 mg), Yashtimadhu Churna (125 mg), Saptamrit Louha (250 mg) |
Jeevantyadi Ghrita 10 ml | Nishakala (at night before sleep) | Chakshyushya (beneficial for sense organ) |
| 4 | Shatapaki Bala Taila (5 ml) | Mudga Yusha (soup of green gram) | Nishakala (at night before sleep) | Chakshyushya and Vata pacifying |
Panchakarma therapy was started simultaneously after 15 days of first visit. The details of Panchakarma therapy given as below:
Table 2.
Details of Panchakarma and local therapy.
| Sr.No | Procedure administered | Medication used | Timings |
|---|---|---|---|
| 1 | Abhyanga (∼whole body massage) | Bala Taila | Daily before bath |
| 2 | Swedan (∼Sudation) | Steam/sudation therapy of whole body in wooden box | During Yoga Basti administration daily for 8 days Duration- Till the sweating starts on forehead |
| 3 | Yoga Basti (3 sittings of Yapana Basti and 5 sittings of Anuvasan Basti) | Baladi Yapana (960 ml), Yashtisiddha Taila Anuvasan (120 ml) | Anuvasan Basti was administered on 1st, 2nd, 4th, 6th and 8th day while Yapana Basti administered on 3rd, 5th, 7th day. (Basti treatment started after 15 days of 1st visit) |
| 4 | Netratarpan (eye satiation) | Jeevantyadi Ghrita (10 ml in each eye) | Daily in evening for 15 days after Basti treatment Duration- 15 min (1000 Matra) |
| 5 | Nasya (oleation through nasal route) | Shatapaki Bala Taila [2 drops (1 ml) in each nostril- Pratimarsh Nasya] | After Netratarpan daily in morning for one month and thereafter thrice in a week for next 6 month. |
| 6 | Padabhyanga (foot massage) | Jeevantyadi Ghrita by Kansya Vati (bronze metal pot) from heel to toe | Daily at night for 10 min |
Patient continued oral medication and application of Bala Taila whole body massage for further 6 month.
Table 3.
Follow up & Treatment outcomes.
| Timeline | Treatment | Outcome |
|---|---|---|
| 10/07/2014 | Internal medication. Patient not taken any other medication | VEP report showed absent waveform over both optic nerve |
| 26/07/2014 | Internal medication followed by Basti treatment | Patient was able to see light perception in right eye |
| 11/08/2014 | Internal medication along with Basti treatment | Improvement in light perception in right eye |
| 13/10/2014 | Internal medication and completed treatment of Basti followed by Netratarpan and Nasya along with Padabhyanga | Along with light perception, patient was able to see projection of rays in right eye |
| 11/04/2015 | Internal medication | Symptomatically improvement noted in light perception and patient was able to do his own daily routine work of himself. Improvement in vision i.e.PL seen in right eye with delayed P100 latencies in VEP report of right eye. |
| 15/07/2015 | Internal medication | Vision stable with light perception of right eye and patient able to identify object in bright light |
2.7. Follow up and outcome
Shown in Table 3. Although, the VEP report of the left eye shown absent waveform after treatment the patient was able to perceive only mild light perception in left eye. There was no improvement seen in pupillary reaction (RAPD was same as the start of the treatment) and optic nerve/disc did not show any significant improvement but patient was satisfied with the visual outcome, patient was followed up monthly (only observation without medication) in clinic and did not show any aggravation in symptoms/visual loss (Till Oct.2015). Besides the improvement in vision, patient had also experienced an improvement in quality of life with normalized Agni (digestive fire), Nidra (sleep), Mala and Mutra (urine and bowel habit) leading to improved quality of health and well-being. Further, patient had advised to get regular body massage with Bala Taila and foot massage with Ghrita and bronze pot.
3. Discussion
Traumatic Optic Neuropathy is a clinical diagnosis which usually occurs after head trauma with or without loss of consciousness, decreased visual acuity and a relative afferent pupillary pathway defect (RAPD). Indirect posterior optic nerve injuries occuring naturaly are usually rarely show complete recovery. Most of the patients develop optic atrophy in later stage [15]. In different clinical circumstances, the pathogenesis of traumatic optic neuropathy is related to the variation in extent and rate of recovery and response to the treatment. In indirect TON, the prognosis of no recovery of visual acuity depends on a) loss of consciousness; b) presence of blood in posterior ethmoidal cells; c) absence of recovery after 48 hours of corticosteroid treatment and d) patient's age above 40 years [16]. Visual Evoked Potential (VEP) is the reliable method for assessment of visual pathway functions in severely injured patients. It is also a useful diagnostic tool in suspected bilateral optic nerve injuries. Visual recovery is difficult where VEP outcomes are not recordable. The electrophysiological assessment provides the diagnostic information for treatment selection.
Acharya Sushruta described the traumatic loss of vision in Drishtigata Vyadhi (diseases affecting vision) [17]. [Uttartantra 7/45]. Trauma and shearing forces cause vitiation of Vata Dosha. These shearing forces can cause loss of visual acuity in most of the patients of TON. So we can compare TON with Abhighatajanya Vataprakopaj Drishtinash. Although, in Ayurvedic classics this terminology was not mentioned but we can consider the correlation on the basis of etiological factors and Doshaprakopa (vitiation of Vata and other body elements) [14]. [Sutrasthana 12/64]. The aggravation and vitiation of Vata seen in trauma is capable of causing damage to the surrounding structures in orbit like optic nerve and cause irreversible damage to vision. Shearing forces exert pressure to an extent that it leads to Drishtinash (complete loss or impaired vision). The diseases due to head trauma causing vision loss are difficult to treat. Hence it can be considered that aggravation of Vata, seen in trauma on head region is capable of causing Drishtinash. These type of causalities can be confirmed by future studies.
The plan of treatment in this case is based on Yuktivyapashray Chikitsa (rational therapy i.e. pharmacological) which mainly includes the Shaman (palliative care) and Shodhan (purificatory procedure). These are important in pacifying and eliminating the vitiated Dosha with medicine and balancing procedures. Shaman Chikitsa is intended to decrease, suppress and eliminate the disease. It pacifies and balance the body humor i.e. Vata, Pitta and Kapha and stops the aggravation of symptoms. Shaman Chikitsa is preferable when the patient is in physicaly or mentaly unable to bear the intensity of Shodhan [14]. [Sutrasthana 1/24]. This patient had a head trauma and a closed lacerated wound on forehead and was not in a mental state to bear the intensity of Shodhan procedure like Basti (medicated enema). So initially counselling was done and treatment started with internal medication. The aim of the treatment in this case was not only to treat the trauma or injury but to recover the vision loss occurred due to trauma and additional concerns of optic atrophy. The rationale of treatment shown in Table 4.
Table 4.
Properties and rationale of medicines used.
| Medicine used | Properties |
|---|---|
| Vasanta Kusumakar |
|
| Roupyayukta Tapyadi Louha |
|
| Vidari powder (Pueraria tuberosa Willd.) |
|
| Jeevanthyadi Ghrita |
|
| Sitopaladi Churna |
|
| Brihat Vata Chintamani |
|
| Saptamrit Roupya |
|
| Mahayogaraj Guggulu |
|
| Punarnava powder (Boerhavia diffusa) |
|
| Pathyadi Kwatha |
|
| Triphala powder (Combination of trio Haritaki, Amalaki and Bibhitak) |
|
| Yashtimadhu powder (Glycyrrhiza glabra L.) | |
| Saptamrit Louha |
|
The Bhaishajya Kala (time of administration of internal/oral medicine) plays an imperial role in treatment of a disease. The administration of medicine in Pratah Kala (morning) with empty stomach was prescribed as the disease condition was strong. The Vyanodan Kala is the time of administration of medicine after lunch (Vyana Kala) and after dinner (Udana Kala). Vyana and Udana are the types of Vata Dosha that play an important role in strengthening the color and normal action of tissue. Nishakala (night) is best to administer the medicine for the diseases above collar bone [14]. [Sutrasthana 13/37–41]. The Chakshyushya medicines are prescribed to administer at night time before sleeping.
Acharya Charaka has mentioned that the diseases which are confined to the bone needs Panchakarma [24]. Basti (medicated enema) is the prime Panchakarma treatment for Vata ailments [14]. [Sutrasthana 1/25]. In Vata predominant diseases Niruha or Yapana Basti is preferable. In present case, due to Marmabhighata (trauma to the vital points), Vata gets aggravated. Considering the physical and mental status of the patient, Baladi Yapana Basti was planned. It is indicated for immediate improvement in vision [14]. [Kalpasthana 4/5–6]. Basti process bypasses the hepatic first pass metabolism and gets absorbed rectally. It stimulates the enteric nervous system and ENS having synergistic working mechanism with CNS. ENS produces the same neurotransmitters found in brain. So Basti may activate the concerned part of CNS with chemo or mechano receptors and give results accordingly [25].
It is important to start the local treatment like Kriyakalpa only after Shodhan Procedure [17]. [Uttartantra 18/5]. Netratarpan was administered after Yoga Basti procedure. Kriyakalpa procedure is administered following the Shodhan procedure to pacify the remaining local Dosha. Netratarpan with Jeevantyadi Ghrita nourishes the internal structures by virtue of its action [26]. Since Ghritakalpana (clarified butter processed with medicinal plants) was used for Netratarpan, it has a lipid soluble property. Lipid soluble substances are have better permeability in the ocular tissue. As the cell membrane contains lipids, the transportation of the drug to the target cell is facilitated by the lipophilic nature of Ghrita. Jeevantyadi Ghrita contains the drug particles in the form of suspension and hence the tissue contact time and bioavailability is more to achieve the desired therapeutic effect in Vata Pitta predominant eye diseases [27]. Acharya Sushruta advocated to use the Tarpan Dravya in eyes by dipping the eyelashes in it [17]. [Uttartantra 18/8]. The required quantity for this purpose comes to approximately 10 ml in each eye and it may vary with the capacity of orbit of each individual.
After Netratarpan, Pratimarsha Nasya was administered with Shatapaki Bala Taila which is Indriyabodhak (nourishes all the five sense organ). Nasya plays an important role in diseases confined to head [14]. [Sutrasthana 20/1]. The drug administered through the nostrils, reaches the Shrigataka Marma, and spreads into Murdha (brain), Netra (eyes), Shrotra (ear), Kantha (throat), Siramukhas (opening of vessels) and snatches the morbid vitiated Doshas from these region and expel them from Uttamanga (region above collar bone). The olfactory nerve and the adjacent nerves are connected to the limbic system of brain including hypothalamus. The stimulation of olfactory nerve causes the stimulation of certain cells of hypothalamus and amygdaloidal complex. The instilled drug over olfactory mucosa are rapidly absorbed by olfactory neurons, supporting cells and capillary bed [28].
Abhyanga (whole body massage) and Shirobhyanga (head massage) with Bala Taila and Padabhyanga (foot massage) with Ghrita nourishes the Drishti and having Vata pacifying properties. Foot massage with metal like Kansya (bronze pot) is useful and reported to restore the balance between the two important neurotransmitters serotonin and norepinephrine which regulate a wide variety of neuropsychological processes [29]. Abhyanga (whole body massage) is useful in Drishti Prasadana (beneficial in improving vision) and specially can be applied in head region. It mitigates Vata Dosha and Jarahar (prevents aging) [14]. [Sutrasthana 2/8–9].
A complete Ayurvedic regime with Panchakarma showed a good subjective and objective outcome in the case of Traumatic Optic Neuropathy (Fig. 1, Fig. 2, Fig. 3, Fig. 4).
Fig. 1.
Pretreatment visual evoked potential (page 1).
Fig. 2.
Pretreatment visual evoked potential (page 2).
Fig. 3.
Visual Evoked Potential during treatment after 9 month (page 1).
Fig. 4.
Visual Evoked Potential during treatment after 9 month (page 2).
4. Conclusion
Presently neuroprotection is a trending topic for neurodegenerative diseases. In TON, if patient seek Ayurveda treatment at earliest, the chances of recovery of damaged nerve fiber increase. The classical Ayurveda principles along with Panchakarma therapy, local treatment and palliative care through Ayurveda can prevent the further damage of nerve fiber. The modern diagnostic tool like Visual Evoked potential (VEP) are useful to proove objective improvement in such cases. The subjective and objective effects observed in this case need corroboration from future studies to substantiate effectiveness of Ayurveda treatment with Panchakarma in Traumatic Optic Neuropathy (TON).
5. Scope for further study
Retinal Ganglion Cell death (apoptosis) is an important factor in loss of vision in ophthalmic neurodegenerative diseases. The study of Ayurveda medicines on molecular and cellular level is essential to substantiate the results obtained in clinical studies of neuro-ophthalmology. Basic understanding of biochemical mechanism in Traumatic Optic Neuropathy will give a future direction to Ayurveda clinical trials in TON.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
References
- 1.Steinsapir K.D., Goldberg R.A. Traumatic optic neuropathy: an evolving understanding. Am J Ophthalmol. 2011 Jun;151(6):928–933.e2. doi: 10.1016/j.ajo.2011.02.007. Epub 2011 May 6. PMID: 21529765. [DOI] [PubMed] [Google Scholar]
- 2.Urolagin S.B., Kotrashetti S.M., Kale T.P., Balihallimath L.J. Traumatic optic neuropathy after maxillofacial trauma: a review of 8 cases. J Oral Maxillofac Surg. 2012 May;70(5):1123–1130. doi: 10.1016/j.joms.2011.09.045. Epub 2011 Dec 16. PMID: 22177813. [DOI] [PubMed] [Google Scholar]
- 3.Rajiniganth M.G., Gupta A.K., Gupta A., Bapuraj J.R. Traumatic optic neuropathy: visual outcome following combined therapy protocol. Arch Otolaryngol Head Neck Surg. 2003 Nov;129(11):1203–1206. doi: 10.1001/archotol.129.11.1203. PMID: 14623751. [DOI] [PubMed] [Google Scholar]
- 4.Seiff S.R. High dose corticosteroids for treatment of vision loss due to indirect injury to the optic nerve. Ophthalmic Surg. 1990 Jun;21(6):389–395. PMID: 2381671. [PubMed] [Google Scholar]
- 5.Levin L.A., Joseph M.P., Rizzo J.F., 3rd, Lessell S. Optic canal decompression in indirect optic nerve trauma. Ophthalmology. 1994 Mar;101(3):566–569. doi: 10.1016/s0161-6420(94)31299-1. PMID: 8127578. [DOI] [PubMed] [Google Scholar]
- 6.Gupta D., Gadodia M. Transnasal endoscopic optic nerve decompression in post traumatic optic neuropathy. Indian J Otolaryngol Head Neck Surg. 2018 Mar;70(1):49–52. doi: 10.1007/s12070-017-1211-5. Epub 2017 Oct 16. PMID: 29456943; PMCID: PMC5807297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Steinsapir K.D., Goldberg R.A. In: Walsh and Hoyt's clinical neuro-ophthalmology. 5th ed. Miller N.R., Newman N.J., editors. Williams & Wilkins; Baltimore, MD: 1998. Traumatic optic neuropathies; pp. 715–740. [Google Scholar]
- 8.Sosin M., De La Cruz C., Mundinger G.S., Saadat S.Y., Nam A.J., Manson P.N., et al. Treatment outcomes following traumatic optic neuropathy. Plast Reconstr Surg. 2016 Jan;137(1):231–238. doi: 10.1097/PRS.0000000000001907. PMID: 26710028. [DOI] [PubMed] [Google Scholar]
- 9.Chaon B.C., Lee M.S. Is there treatment for traumatic optic neuropathy? Curr Opin Ophthalmol. 2015 Nov;26(6):445–449. doi: 10.1097/ICU.0000000000000198. PMID: 26448040. [DOI] [PubMed] [Google Scholar]
- 10.Entezari M., Esmaeili M., Yaseri M. A pilot study of the effect of intravenous erythropoetin on improvement of visual function in patients with recent indirect traumatic optic neuropathy. Graefes Arch Clin Exp Ophthalmol. 2014 Aug;252(8):1309–1313. doi: 10.1007/s00417-014-2691-6. Epub 2014 Jul 2. PMID: 24986593. [DOI] [PubMed] [Google Scholar]
- 11.Huang J., Chen X., Wang Z., Deng S., Duan J., Lu G., et al. Selection and prognosis of optic canal decompression for traumatic optic neuropathy. World Neurosurg. 2020 Jun;138:e564–e578. doi: 10.1016/j.wneu.2020.03.007. Epub 2020 Mar 10. PMID: 32169622. [DOI] [PubMed] [Google Scholar]
- 12.Dhiman K.S., Adhoor V.S., Agarwal R., Mehta A.J. Adjuvant effect of Chakshushya Rasayana with beta-blocker eye drops in the management of progressive glaucomatous optic neuropathy: an open-label randomized controlled trial. Ayu. 2016 Apr-Jun;37(2):125–134. doi: 10.4103/ayu.AYU_30_16. PMID: 29200751; PMCID: PMC5688835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agrawal S., Rajagopala M. Clinical study on primary open-angle glaucoma with Ashchyotana, Tarpana and oral medication. Ayu. 2017 Jan-Jun;38(1–2):33–38. doi: 10.4103/ayu.AYU_155_16. PMID: 29861590; PMCID: PMC5954260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kunte A., Paradkar H., editors. Ashtang Hridaya of Vagbhata. 6th ed. Nirnay Sagar Press; Bombay: 1939. [Google Scholar]
- 15.Chan J. 2nd ed. Springer Science; New York: 2014. Optic nerve disorders. Chapter 5: traumatic optic neuropathies; p. 161. [DOI] [Google Scholar]
- 16.Carta A., Ferrigno L., Salvo M., Bianchi-Marzoli S., Boschi A., Carta F. Visual prognosis after indirect traumatic optic neuropathy. J Neurol Neurosurg Psychiatr. 2003 Feb;74(2):246–248. doi: 10.1136/jnnp.74.2.246. PMID: 12531960; PMCID: PMC1738266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Acharya Jadavaji T. 2nd ed. Nirnay Sagar Press; Bombay: 1931. Sushrut Samhita by Sushruta. [Google Scholar]
- 18.Gangadharshastry Gune. Vaidyak Grantha Bhandar; Pune: 2001. Ayurvediy Aushadhigunadharmashastra. Part 1-4. (edition reprint) [Google Scholar]
- 19.Chunekar K., Gangasahay Pandey. Bhavaprakash Nighantu. 1st ed. Choukhambha Bharati Academy; Varanasi: 2010. [Google Scholar]
- 20.Murthy K. 4th ed. Choukhambha Orientalia; Varanasi: 2001. Sharagdhara Samhita. Madhyamkhanda 6/134-135; p. 98. [Google Scholar]
- 21.Tripathi P., Koushik G. 3rd ed. Tejkumar Press; Lucknow: Muralidhar Mishra: 1957. Bhaishajyaratnavali, Vayurogadhikar; p. 491. [Google Scholar]
- 22.Murthy K. 4th ed. Choukhambha Orientalia; Varanasi: 2001. Sharagdhara Samhita. Madhyamkhanda 2/143-145; p. 73. [Google Scholar]
- 23.Tripathi P., Koushik G. Lucknow: Muralidhar Mishra. 3rd ed. Tejkumar Press; 1957. Bhaishajyaratnavali, Shoolarogadhikar; p. 351. [Google Scholar]
- 24.Acharya Jadavaji T., editor. Charaka Samhita by Agnivesh, Sutrasthana; Vividhashitpitiya: chapter 28, verse 27. Nirnay Sagar Press; Bombay: 1941. p. 180. [Google Scholar]
- 25.Yogita B., Lekurwale P., Mekhale S., Rathode S., K D., Gulhane C. A critical review on pharmacodynamics of Basti Chikitsa and its action on enteric nervous system. Int J Ayurvedic Med. 2015;6(4) https://www.ijam.co.in/index.php/ijam/article/view/06412015 Retrieved from. [Google Scholar]
- 26.Bhat P. A Review on Kriyakalpa: The modern approach to Ayurvedic ocular therapeutics. Int J Res Ayurveda Pharm. 2016;7(5):12–16. [Google Scholar]
- 27.Poonam, Manjusha R., Vaghela D.B., Shukla V.J. A clinical study on the role of Akshi Tarpana with Jeevantyadi Ghrita in Timira (myopia) Ayu. 2011 Oct;32(4):540–545. doi: 10.4103/0974-8520.96130. PMID: 22661851; PMCID: PMC3361932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kar P. 1st ed. Chaukhamba Sanskrit Pratishthan; Delhi: 2013. Mechanism of Panchakarma & its module of investigation; pp. 119–122. [Google Scholar]
- 29.Rashmi K., Deshpande S. Role of Padabhyanga as preventive aspect w.s.r to eye disorders: A conceptual study. Int J Ayurveda Pharma Res. 2015;3(10):80–82. [Google Scholar]