Summary box.
Defining an accurate, representative service catchment area is important for computing population denominators for disease mapping and efficient public planning, including health, education and social care.
The growth in population settlement modelling techniques and provision of geocoded service databases has fuelled an increase in local and regional service access mapping to examine coverage and equity in much of sub-Saharan African countries.
However, metrics of service access and catchments are often implemented based on convenience, disregarding the implications on accuracy of the catchment population, complexities of service use and the likely implications for public service planning.
Lack of high spatial resolution geolocated data on residential locations of the service users has led to the use of rudimentary, inexact approaches to complex processes that define service catchment areas and should be used with caution.
The improved collection of residential addresses of service users and service providers has increased the ability to develop new innovative models of service catchment.
Improved data availability and data sharing must be accompanied by better models of service use.
In this commentary, we revisit the issue by considering common approaches, key issues and best practices in defining a reliable service catchment area.
We hope this will lead to further granular studies to populate and compare methods to improve the definition of service catchment areas in sub-Saharan Africa, ultimately improving efficiencies and equity in service use and more reliable interpretations of routine service use data.
Introduction
An accurate service catchment area—a geographical area delineated around a service point (such as a health facility or a school) describing the population that uses its services1—is important for robust and reliable estimation of population denominator used in planning, estimating commodity needs and mapping applications. In the literature, approaches used to define a service catchment area range from simple to complex approaches and are often presented as population to service ratios, use of administrative boundaries, proximity-based metrics and models accounting for utilisation rates. However, the implementation and choice of an approach are often based on convenience, disregarding the implications on accuracy of the catchment population, complexities of service use and the likely implications for planning. In this commentary, we highlight the common approaches, key issues and best practices in defining a reliable and representative service catchment area. We hope to create a dialogue within the geospatial community and allied stakeholders to evolve best-practice standards in defining service catchment areas for efficient and equitable planning.
The commentary is structured into four sections. We discuss the need for recording and geolocating user addresses followed by a summary of approaches used to define service catchment areas and conclude with the key characteristics of an ideal service catchment, best practices and key issues that require addressing.
Need for recording and geolocating service user addresses
The definition of a reliable service catchment area for health, education, social care and other local public services depends on the availability of spatially positioned residential addresses of those who seek services. In high-income countries, residential addresses (such as zip code, house number and street name) are part of well-defined registers that can be used to define service catchment areas. Conversely, most of sub-Saharan Africa (SSA) do not have the luxury of well-defined addresses or routine logging and geocoding of villages/estates of those seeking services.2 3 In cases where such data are available in SSA, there is heterogeneity between and within countries. For example, within health and demographic surveillance sites, addresses of households are well maintained. The absence of reliably defined service catchment areas challenges robust disease mapping, equitable provision of vaccines (eg, childhood immunisations), other preventive health commodities (such as bed-nets), and acute care, school needs, social care and the accurate compilation of health data. This is because such applications rely on a catchment population denominator, which is in turn derived by a spatial overlay of population density maps and the geographical extent of a service catchment area.4–7
Across SSA, population settlement and sites of service provision are often not mapped on a regular basis nor are always available at small administrative units for efficient planning. Disaggregating low-resolution census data to presumed high-resolution settlement patterns guided by satellite imagery and building footprints has increased in sophistication in recent years.8 The locations of schools, health facilities and other amenities have improved with crowd-sourced Global Positioning Systems initiatives, participatory mapping, improved national gazetteers, high-resolution satellite imagery and demand for such data sets.3 However, linking population to service delivery remains crude and ignores the complexities of service demand and/or supply mainly due to a lack of geocoded data on where the users of services reside in SSA.
Modest approaches used to define service catchment areas
Population-to-service ratios are the most common metrics, ranging from wide subnational units to national estimates for international ranking. These metrics merely require an estimate of population size from national censuses and the number of facilities within a census-defined polygon. Smaller, subnational polygons can be used, for example, subcounties, wards, municipalities or parishes (figure 1), where service provision is decided by local health and education authorities. However, people residing along administrative boundaries will likely access the most proximal service which might be in the neighbouring administrative unit. Similarly, people in need of a particular service far away from the border might be attracted to a particular service point in a neighbouring unit due to preferred, desirable characteristics. For example, women bypassed the nearest facility in Tanzania,9 Ghana,10 Kenya,11 Mozambique, India and Pakistan.12 As a result, it is common practice to have childhood immunisation coverage from routine data greater than 100% in administrative units that attract many people from neighbouring administrative units.13 14 This is likely due to a challenge of assigning population denominators to an administrative area instead of a well-defined service catchment area based on the actual users of a particular service.
Figure 1.
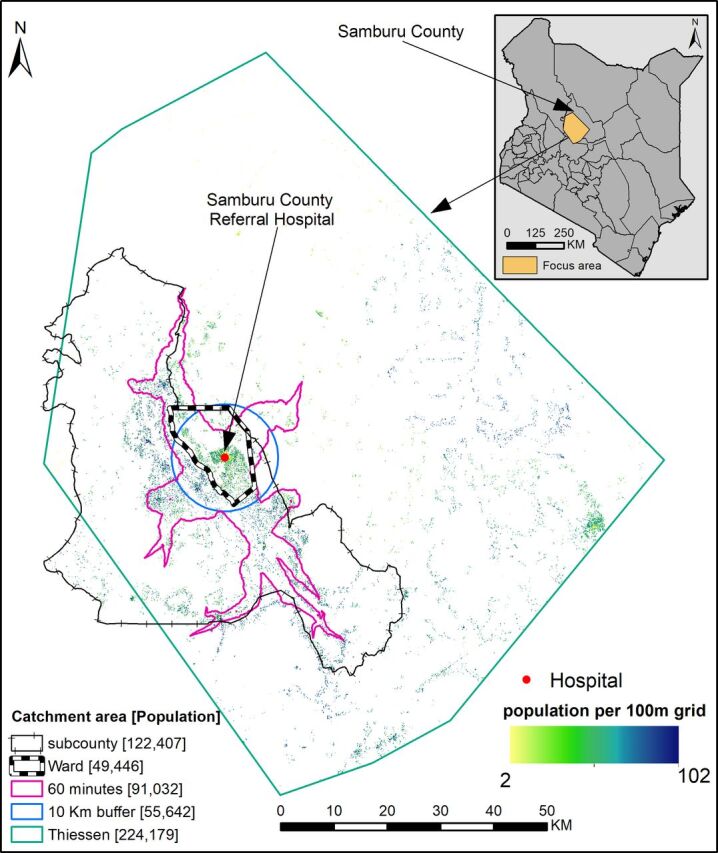
An illustration of several approaches used to define service catchment area, administrative unit (ward or subcounty), straight-line distance (10 km buffer and Thiessen polygon) and travel time (area within 60 min of a hospital). Illustration is based on 622 COVID-19 vaccination posts (https://medical.unon.org/node/169) approved in Kenya. If vaccine allocation was based on one of these catchment areas, there would be mismatches between those who attend a facility and the estimated population denominator in 20218 across methods due to lack of geolocated residential data of care seekers at a particular post. The top right corner shows the illustrated region within Samburu County, Kenya.
Where both the population (whether actual or modelled) and amenity locations (geocoded with a longitude and latitude) are available at high resolution and accuracy,8 15 service catchment areas can be empirically modelled. The most common and rudimentary approach is the use of an arbitrary radius (buffer) around a service point, for example, a 10 km buffer. The radius of the buffer can be variable depending on the capacity of the provider, type of services offered and the mode of transport used to access the service (figure 1). Related to the buffer is Thiessen polygon, where each catchment area incorporates all points that are closer to a given service provider than any other provider (figure 1). These two approaches rely on straight-line distance, which does not reflect actual distance and/or time travelled, which are in turn impacted by topography, land use/cover, road network, transport modes and associated transport speeds. Furthermore, service points are also weighted equally despite differences in the capacity and size.
Improved approaches to defining service catchment areas
The complexity of physical access, choice and demand characteristics can be tackled with more complex models of service use. Gravity models assume that the flow of people from residential areas to service providers is proportional to the demand for services and inversely proportional to physical access.16 The demand for services is defined by morbidity, age, and social structure and the capacity of a facility.16 To be more realistic, this physical access can be estimated by modelling the travel time to the nearest provider, by accounting for travel factors and barriers mainly through cost distance algorithms and network analysis.17 The travel time is then binned to define a service catchment area1 based on either an arbitrary time threshold (figure 1) or known cut-offs, where available (eg, 2 hours for obstetrical complications). A range of software including AccessMod,18 ArcMap (Esri, Redlands, CA, USA, 2021) and QGIS (QGIS.org, 2021. QGIS Association. QGIS Geographic Information System) can be used to estimate travel times and corresponding catchment areas.
The use of travel time is appealing, but it requires expert knowledge to implement. It also assumes travel time to the nearest facility, which is not always the case and often does not account for competition and user preferences.12 Furthermore, catchment boundaries might be highly permeable when arbitrarily defined thresholds are applied.4 The issue of arbitrarily defined time threshold can be minimised by combining travel time with utilisation rates typically from sample household survey data,19 to inform a reasonable threshold via the inflection point of a decay curve.20 The gravity models can be adapted with additional information and sophisticated models to account for competition between service points, variation in capacity, available equipment, quality and affordability of the service provided.21
Ideal service catchment area and best practices
An ideal service catchment area should meet a minimum set of conditions from both the supply and demand side: (a) capture a significant proportion of its activities, (b) exclude areas whose activity contribution is due to random variation (eg, service users who are not usual residents such as visitors), (c) account for geography (physical access and its barriers), (d) differentiate across specialty types (eg, vaccination sites, tuberculosis detection, snake antivenom availability, or primary and tertiary educational levels) and capacities (affordability, size, staffing and equipment), (f) competition from the network of neighbouring providers and (g) seasonal changes due to weather or population flows.22 23
The use of models to define a catchment area can, however, be bypassed if data needed to define an ideal catchment were available, enabling the use of simpler geospatial information systems techniques. Therefore, defining a representative catchment is premised on the availability of geocoded data at high spatial and/or temporal resolution, reflecting residential location of service users, service points, utilisation rates, service use and factors that affect travel and behavioural data on service choice. Future ambitions to define service catchment areas should be aligned to several key considerations listed in table 1.
Table 1.
Best practices and ambitions associated with defining reliable, accurate and representative service catchment areas for public services such as healthcare, education and social services
| Category | Ambitions and best practices |
| Data collection | Improving collection and geocoding of residential address (village/estate) data from service users by healthcare providers, educational institutions, local governments and national statistical agencies. This will enhance the definition of service catchment areas for effective planning. High-resolution population density maps and databases of road network, land use/cover, travel barriers, care-seeking behaviour, modes of transport and travel speeds also need a careful curation. |
| Data and software sharing | Important data sets to define service catchment areas should no longer be kept in silos. The culture of making open-access data analytical models and software should improve across researchers and organisations in SSA. With increasing model sophistication, there is a need for software that can easily be used to define realistic service areas especially for planners. |
| Community | Building a community of researchers, sharing best practices, identifying difference between services, different diseases, service interruptions (eg, COVID-19 or natural disasters), ecological contexts and demography will be useful. |
| Service use | With a growth in availability of geocoded data and spatial epidemiologists across SSA, there is a need for an increased investment in research aimed at mapping higher resolution data on service use. Studies should also consider different forms of service access such as vaccination, healthcare, education and social care. |
| Disease mapping | The use of spatial statistics to map diseases, health outcomes, and demographic and socioeconomic indicators has witnessed huge advancements. However, the use of data from routine services (such as disease registries) together with reliably defined catchment areas requires more attention and quantifying the role played by different approaches and their impact on the mapped quantities. |
| Sensitivity | Where modelling must be conducted due to inadequate data, authors should test the sensitivity and uncertainty of several models that are used to define a service area. Comparisons will tease out if there any gains in using complex geospatial approaches in lieu of simpler approaches (more accessible to non-experts) to define service areas. There is also a need to recognise limitations such as bypassing the nearest provider due to personal preferences, quality and capacity when results are being interpreted. |
SSA, sub-Saharan Africa.
In conclusion, service choice will always depend on a complex array of social factors, quality (perceived or actual), previous experience, affordability and physical accessibility encompassing both the supply and the demand side.24 Such factors dictate how often lower level health facilities are by-passed, or the choice of an educational institution or social care programmes.25 26 The availability of well-curated and regularly updated service utilisation data and locations of service users will be important in accounting for such unique characteristics and defining reliable service catchment areas going forward.
Footnotes
Handling editor: Seye Abimbola
Twitter: @Pete_M_M
Contributors: PMM conceived and designed the commentary and was responsible for the production of the first draft. RWS contributed to the second draft. All authors provided scientific input and contributed to the writing of the commentary.
Funding: PMM is supported under the Royal Society Newton International Fellowship (NIF/R1/201418). NR acknowledges support from the Swiss National Science Foundation (project number 315130_176271). EG is supported by a Springboard grant (number SBF004/1009) of the Academy of Medical Sciences. EAO is supported as a Wellcome Trust Intermediate Fellow (number 201866). RWS is supported as a Wellcome Trust Principal Fellow (numbers 212176). PMM, EAO and RWS are grateful to the support of the Wellcome Trust to the Kenya Major Overseas Programme (number 203077).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Schuurman N, Fiedler RS, Grzybowski SCW, et al. Defining rational hospital catchments for non-urban areas based on travel-time. Int J Health Geogr 2006;5:43. 10.1186/1476-072X-5-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stresman GH, Stevenson JC, Owaga C, et al. Validation of three geolocation strategies for health-facility attendees for research and public health surveillance in a rural setting in Western Kenya. Epidemiol Infect 2014;142:1978–89. 10.1017/S0950268814000946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fornace KM, Surendra H, Abidin TR, et al. Use of mobile technology-based participatory mapping approaches to geolocate health facility attendees for disease surveillance in low resource settings. Int J Health Geogr 2018;17:21. 10.1186/s12942-018-0141-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Macharia PM, Odera PA, Snow RW, et al. Spatial models for the rational allocation of routinely distributed bed nets to public health facilities in Western Kenya. Malar J 2017;16:367. 10.1186/s12936-017-2009-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Okiro EA, Kazembe LN, Kabaria CW, et al. Childhood malaria admission rates to four hospitals in Malawi between 2000 and 2010. PLoS One 2013;8:e62214. 0062214-undefined8. 10.1371/journal.pone.0062214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kigozi SP, Kigozi RN, Sebuguzi CM, et al. Spatial-Temporal patterns of malaria incidence in Uganda using HMIS data from 2015 to 2019. BMC Public Health 2020;20:1913. 10.1186/s12889-020-10007-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodriguez-Segura D, Kim BH. The last mile in school access: mapping education deserts in developing countries. Development Engineering 2021;28:100064. 10.1016/j.deveng.2021.100064 [DOI] [Google Scholar]
- 8.Stevens FR, Gaughan AE, Linard C, et al. Disaggregating census data for population mapping using random forests with remotely-sensed and ancillary data. PLoS One 2015;10:e0107042. 10.1371/journal.pone.0107042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elewonibi B, Sato R, Manongi R, et al. The distance-quality trade-off in women's choice of family planning provider in North Eastern Tanzania. BMJ Glob Health 2020;5:e002149. 10.1136/bmjgh-2019-002149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amoro VA, Abiiro GA, Alatinga KA. Bypassing primary healthcare facilities for maternal healthcare in North West Ghana: socio-economic correlates and financial implications. BMC Health Serv Res 2021;21:545. 10.1186/s12913-021-06573-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Escamilla V, Calhoun L, Winston J, et al. The role of distance and quality on facility selection for maternal and child health services in urban Kenya. J Urban Health 2018;95:1–12. 10.1007/s11524-017-0212-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Makacha L, Makanga PT, Dube YP, et al. Is the closest health facility the one used in pregnancy care-seeking? A cross-sectional comparative analysis of self-reported and modelled geographical access to maternal care in Mozambique, India and Pakistan. Int J Health Geogr 2020;19:1. 10.1186/s12942-020-0197-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maina I, Wanjala P, Soti D, et al. Using health-facility data to assess subnational coverage of maternal and child health indicators, Kenya. Bull World Health Organ 2017;95:683–94. 10.2471/BLT.17.194399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gesicho MB, Were MC, Babic A. Data cleaning process for HIV-indicator data extracted from DHIS2 national reporting system: a case study of Kenya. BMC Med Inform Decis Mak 2020;20:293. 10.1186/s12911-020-01315-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maina J, Ouma PO, Macharia PM, et al. A spatial database of health facilities managed by the public health sector in sub Saharan Africa. Scientific Data 2019;6:1–8. 10.1038/s41597-019-0142-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones S, Wardlaw J, Crouch S, et al. Modelling catchment areas for secondary care providers: a case study. Health Care Manag Sci 2011;14:253–61. 10.1007/s10729-011-9154-y [DOI] [PubMed] [Google Scholar]
- 17.Ouma P, Macharia PM, Okiro E. Methods of measuring spatial accessibility to health care in Uganda. In: Practicing health geography. the African context. Springer, 2021: 77–90. 10.1007/978-3-030-63471-1_6 [DOI] [Google Scholar]
- 18.Ray N, Ebener S. AccessMod 3.0: computing geographic coverage and accessibility to health care services using anisotropic movement of patients. Int J Health Geogr 2008;7:63. 10.1186/1476-072X-7-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Corsi DJ, Neuman M, Finlay JE, et al. Demographic and health surveys: a profile. Int J Epidemiol 2012;41:1602–13. 10.1093/ije/dys184 [DOI] [PubMed] [Google Scholar]
- 20.Alegana VA, Wright JA, Pentrina U, et al. Spatial modelling of healthcare utilisation for treatment of fever in Namibia. Int J Health Geogr 2012;11:6. 10.1186/1476-072X-11-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alegana VA, Khazenzi C, Akech SO, et al. Estimating hospital catchments from in-patient admission records: a spatial statistical approach applied to malaria. Sci Rep 2020;10:1324. 10.1038/s41598-020-58284-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gilmour SJ. Identification of hospital catchment areas using clustering: an example from the NHS. Health Serv Res 2010;45:497–513. 10.1111/j.1475-6773.2009.01069.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adams EK, Wright GE. Hospital choice of Medicare beneficiaries in a rural market: why not the closest? J Rural Health 1991;7:134–52. 10.1111/j.1748-0361.1991.tb00715.x [DOI] [PubMed] [Google Scholar]
- 24.Alegana VA, Maina J, Ouma PO, et al. National and sub-national variation in patterns of febrile case management in sub-Saharan Africa. Nat Commun 2018;9:4994. 10.1038/s41467-018-07536-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ocholla IA, Agutu NO, Ouma PO, et al. Geographical accessibility in assessing bypassing behaviour for inpatient neonatal care, Bungoma County-Kenya. BMC Pregnancy Childbirth 2020;20:287. 10.1186/s12884-020-02977-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yaacob NA, Osman MM, Bachok S. Factors influencing parent's decision in choosing private schools. Procedia Soc Behav Sci 2014;153:242–53. 10.1016/j.sbspro.2014.10.058 [DOI] [Google Scholar]


