Abstract
Structural and intercultural competence approaches have been widely applied to fields such as medical training, healthcare practice, healthcare policies and health promotion. Nevertheless, their systematic implementation in epidemiological research is absent. Based on a scoping review and a qualitative analysis, in this article we propose a checklist to assess cultural and structural competence in epidemiological research: the Structural and Intercultural Competence for Epidemiological Studies guidelines. These guidelines are organised as a checklist of 22 items and consider four dimensions of competence (awareness and reflexivity, cultural and structural validation, cultural and structural sensitivity, and cultural and structural representativeness), which are applied to the different stages of epidemiological research: (1) research team building and research questions; (2) study design, participant recruitment, data collection and data analysis; and (3) dissemination. These are the first guidelines addressing structural and cultural competence in epidemiological inquiry.
Keywords: other diagnostic or tool, epidemiology, review, public health, other study design
Summary box.
Structural and cultural competence approaches have been widely applied to the health fields, but no systematic effort has been made to apply them to the epidemiological inquiry.
Organised as a 22-item checklist, the Structural and Intercultural Competence for Epidemiological Studies (SICES) guidelines are the first systematic attempt to bring these approaches into epidemiological research.
SICES provides new clues for reducing bias, interpreting the findings, and favours the commitment of populations to research results and their dissemination.
SICES encourages a more horizontal and dialogical relationship between researchers and the public.
SICES promotes the representativeness of minority groups and excluded population in epidemiological studies.
The challenge of intercultural and structural competence in epidemiological research
In recent decades, the intercultural competence approach and its sisters, such as cultural competence, cross-cultural competence and cultural humility, among others, have been widely applied to healthcare, healthcare policies and especially to training programmes for health professionals.1–6 Making policies and clinical practices more sensitive and effective in dealing with social diversity has become a purpose of healthcare systems of many countries, regardless of their policy models, as well as of international health agencies.7 In a globalised world, medical services and policies must face the challenge of multiculturalism.8 Everyday clinical practice presents a landscape that is expressed by patients with different demands, ethnic affiliations, languages and idioms of distress, as well as problems of exclusion and racism, experiences of migration, displacement and torture, and other difficulties arising from globalisation and its disruptions.9 10 In this context, culture matters for balancing the dominant cultural view of the healthcare agenda, for dealing with local worlds and popular medical systems, for promoting social participation in health, as well as for designing community-centred health initiatives, among many other fields.11
Following Fleckman et al,4 in this article we prefer the term intercultural competence rather than the more frequent cultural competence. The cultural competence notion can suggest the possibility of substantial or complete knowledge of a given culture and an emphasis on the culture of the patient, user or participant. Two implicit assumptions may be misleading, since (1) it is not possible to know a culture in its entirety and (2) any competence in this domain requires health professionals’ reflexivity regarding their cultural backgrounds, including the culture of their expert system. Alternatively, the intercultural competence model invites an understanding of competence as a movement from the personal to the interpersonal level of interactions.4 Intercultural competence values the impact of cultural factors on both lay participants and health professionals and can be defined, paraphrasing Fleckman et al,4 as ‘the ability to manage effectively and appropriately in intercultural situations on the basis of one’s own intercultural knowledge, skills and attitudes.’
Recent initiatives have sought to broaden the spectrum of intercultural competence to integrate social and economic dimensions, and issues such as structural violence and the naturalisation of inequality.12–16 Cultural diversity explains only part of the impact of social life on health. It is necessary to complement diversity with another ‘usual suspect’: inequality and its structural vulnerabilities. This is the case of some attempts to rethink cultural competence, such as Kirmayer’s,17 as well as of the so-called ‘structural competence’ that, according to some authors, attempts to rescue ‘five decades’ of studies on the social determinants of health.12 Following Metzl and Petty,18 we can define structural competence as a framework for addressing ‘health-related social justice issues that emphasises diagnostic recognition of economic and political conditions producing and racialising inequalities in health.’
Structural competence is closely related to other approaches such as the Critical Race Theory,19 which discusses structural racism and its impact in previous research studies and medical interventions in ethnic and sociocultural minorities. Structural vulnerabilities can be assessed through historical medical memories of the marginalised communities. The community’s trust in research and medicine and consequently their eagerness to participate, or not, in epidemiological studies is a main aspect to be addressed due to its impact on recruitment and thereby bias.
Structural competence includes some cultural dimensions, so it might seem that the proposal to maintain the dual structural and intercultural components may be redundant. Nevertheless, the focus of structural competence is mainly on how broad social systems and historical processes generate structural vulnerabilities and health inequalities. Bourgois et al12 define structural competence as ‘the ability for health professionals to recognise and respond with self-reflective humility and community engagement to the ways negative health outcomes and lifestyle practices are shaped by larger socioeconomic, cultural, political and economic forces.’ Culture is integrated in this definition as a ‘larger force,’ and implicitly in the idea of self-reflective humility and lifestyle practices. But culture as a factor is not widely included in this definition. Some elements are missing or receive meagre attention, especially the cultural and linguistic validation of tools and services and the ‘intercultural’ dimension, in the sense of the capacity of clinicians, researchers and policymakers to oscillate themselves ‘between’ a known culture and a culture to be known. We consider that a better balance between recognition of cultural diversity and awareness of inequality makes it possible to strengthen the analysis of both dimensions, since structural vulnerabilities take unique forms in specific cultural contexts. For example, ‘poverty’ takes on a different meaning in a culture where social status is not based on material wealth.17
The integration of structural and intercultural competencies into epidemiological study design is a real challenge not just for epidemiologists, but also for social scientists working on health issues, such as medical anthropologists. A look at the Lancet Commission on Culture and Health report is illuminating in this regard.11 In that detailed text, the word ‘epidemiology’ and its variants (ie, ‘epidemiological’) is used just twice, as are other close terms such as ‘cohort’. The relative omission of epidemiology in this text is symptomatic for us, especially considering its comprehensive and integrative purpose. In fact, no systematic effort has been made so far to apply the intercultural or structural competence perspectives to the epidemiological field.
One of the reasons for this gap is undoubtedly the difficulty of integrating social and cultural factors into epidemiological inquiry. This difficulty arises from at least two challenges. The first is common to healthcare, as it lies in the very conceptualisation of health problems as realities dependent on social life.11 The second is more specific to epidemiological research and concerns the design and the use of tools and methods that are sensitive not just to cultural and social aspects, but also to political and structural vulnerabilities.
In relation to the first challenge, it is recognised that social and cultural factors overlap and there is no clear distinction between them. Generally, it is considered that culture refers to the ideational dimensions of social life: perceptions, symbolic representations, collective identities, religious customs, values, among other phenomena that often resist quantification.20 For their part, social factors have become more associated with the system of social organisation, status and classes, with social mobility, poverty, inequality and policies.21 However, cultural and social factors are related to each other in a holistic and interdependent mode in such a way that their isolation as variables can be artificial. For example, a cultural variable such as the process of acculturation of ethnic minorities is closely related to access to education and to upward social mobility and thus to social status.
But the more general problem arises concerning the second challenge: the application of structural and intercultural competence to the epidemiological design. The problem of cultural validation of some measurement instruments such as scales or diagnostic interviews is well known in the literature,22 23 but it is not the only issue. A competence approach in this matter presupposes a self-reflective practice on the researcher’s own cultural milieu, including biomedical culture. Table 1 includes some basic definitions that we have adapted to epidemiological inquiry to assist in this reflexivity process.
Table 1.
Basic definitions
| Term | Definition |
| Intercultural competence in epidemiology | The ability to effectively address cultural and intercultural factors in the study design, data collection, data management, analysis and dissemination. Intercultural competence values the impact of cultural factors on both participants and researchers. In this sense, it includes both lay and expert systems. |
| Culture | A culture is a set of values, meanings and lifestyles shared by a human group that is transmitted intergenerationally through a process of socialisation and learning. All human beings are cultural to the extent that we live in society. Each cultural system involves specific norms, values, canons, aesthetic forms and models of personhood, among other aspects, that shape a worldview. This particularity or specificity does not contradict the existence of an internal diversity in each culture. Culture is a dynamic reality, the result of historical developments, and therefore changing over time.11 36 |
| Biomedicine as culture | The ‘culture of biomedicine’ is the Westernised idea of care, analysis and perception of health, illness, the body and healing processes. Any medical system can be considered a cultural system. Biomedicine, also called Western medicine, scientific medicine or allopathic medicine, is the hegemonic medical system worldwide.37 38 |
| Race | Anthropology and population genetics indicate that the notion of race is not useful in accounting for human biological variation and that it results in reproducing non-existent biological differences.39–41 Alternative use of this term implies considering it a social construct, as a social variable related to discrimination and racism. |
| Racism | Racism can be understood as the exclusion of specific individuals and groups due to phenotypical and/or cultural traits (cultural racism). These traits may be imagined, but they have a real effect in the life of people. In this sense, it is a structural factor of vulnerability and vulnerabilisation. |
| Ethnicity | The notion of ethnicity or ethnic group refers to a set of individuals who share a sense of common origins, claim a common and distinctive history and destiny, and feel a sense of collective uniqueness and identity. This identity may be based on similarities in outward appearance (ie, phenotype), customs, language, religion or other identity elements. |
| Structural competence in epidemiology | The ability to recognise in the study design, data collection, management and analysis of data, and dissemination of the results the ways negative health outcomes and lifestyle practices are shaped by larger socioeconomic, cultural, political and economic forces. |
| Structural vulnerability | Bourgois et al12 define structural vulnerability as follows: ‘An individual’s or a population groups’ condition of being at risk for negative health outcomes through their interface with socioeconomic, political and cultural/normative hierarchies.’ Following these authors, some structural vulnerabilities are:
|
Certainly, in epidemiology there are different paradigms that focus on issues close to those considered in intercultural and structural competence. This would be the case of social epidemiology23 and sociocultural epidemiology,24 participatory epidemiology25 or critical epidemiology,26 in which we could even include the proposal of an ‘epidemiology without numbers’27 that takes the collective production of health as its horizon. However, these paradigms have not explicitly or clearly focused on the competence of researchers as a set of knowledge, skills and attitudes that can improve research design. Here we think that intercultural and structural competence should not be considered as a theoretical option, but as a transversal approach, in the same way as research ethics or the Responsible Research and Innovation (RRI) approach.28 The impact of local knowledge, difficulties in communicating with participants, or social and cultural biases arising from data collection,29 30 among many other factors, are challenges in epidemiological research that an intercultural and structural competence can help to address.
This article aims to develop some guidelines that can improve the structural and intercultural competence of epidemiological studies. When we speak of competence, we are referring to a horizon or an aspiration and not so much to a goal that can be achieved in its entirety. In this sense, this is not a proposal of maximums, but a first step that can help to strengthen the structural and intercultural competence of epidemiological studies.
Searching for references
We conducted a scoping review to identify in the literature instruments, tools, and guidelines regarding structural and cultural competence in epidemiology and, in a second phase, in other health fields. In order to identify the available literature, we conducted several searches in the National Library of Medicine (PubMed) starting in April 2020; updated in September 2020. The searches included publications in any language with the following keyword search combinations (no Medical Subject Headings terms) limited to title and abstract:
First search: (“structural competence” OR “structural competency”) AND (epidemiolog* OR “epidemiological procedures” OR “epidemiological design” OR “epidemiological methods”).
Second search: (“cultural competence” OR “cultural competency OR intercultural competence OR intercultural competency OR cross-cultural competence OR cross-cultural competency) AND (epidemiolog* OR epidemiological procedures OR epidemiological design OR epidemiological methods).
Additionally, we searched in the Cochrane Database of Systematic Reviews using the same terms. No items met the sole inclusion criterion of being a tool, instrument, or guidelines for the application of structural and/or cultural competence in the design and/or implementation of epidemiological research.
Due to this gap in the literature, we proceeded in a second phase to review the instruments, tools and guidelines used in other fields, such as health professional training and education, healthcare, health promotion and healthcare policies. In this case, we used the following search strategies:
Third search: (“structural competence” OR “structural competency”) AND (“guideline” OR “tool” OR “instrument”).
Fourth search: (“cultural competence” OR “cultural competency” OR “intercultural competence” OR “intercultural competency” OR “cross-cultural competence” OR “cross-cultural competency”) AND (“guideline” OR “tool” OR “instrument”).
Only publications which reported tools, instruments or guidelines regarding structural and cultural competence were eligible for inclusion. Uncertainties about whether the publications met the inclusion criteria were resolved through discussion among the researchers. Additional references were added through cross-referencing.
Two researchers (DB and AM-H) conducted full-text reviews of the publications and independently analysed the most salient domains of the selected items using a hermeneutic and qualitative content methodology. The obtained domains were crossed with the tasks involved in epidemiological research. The examination of this intersection allowed us to propose a checklist of items that should be considered when designing, carrying out and analysing data in epidemiological studies with a structural and intercultural perspective. Finally, the different items were elaborated on the basis of a consensus exercise among all authors, which included both scholars with expertise in intercultural and structural competence and those with experience in designing and conducting epidemiological research.
Evaluating existing tools
The first and second searches yielded 55 articles (42 through PubMed and 13 identified through Cochrane Database of Systematic Reviews). No items met the inclusion criterion of being a tool, instrument or guidelines. The two articles closest to our goal were on the application of intercultural competence to public health,4 especially to the training of professionals, and on integrating epidemiological and ethnographic methodologies.31 The third and fourth searches yielded a total of 427 articles (11 and 416, respectively), and 10 documents were added through cross-referencing. After eliminating duplicates (two items), the remaining 435 articles were screened, of which 404 were excluded because they did not report on tools, instruments or guidelines, and 10 because they were a redundant use of a tool. A total of 21 tools were identified (figure 1).
Figure 1.
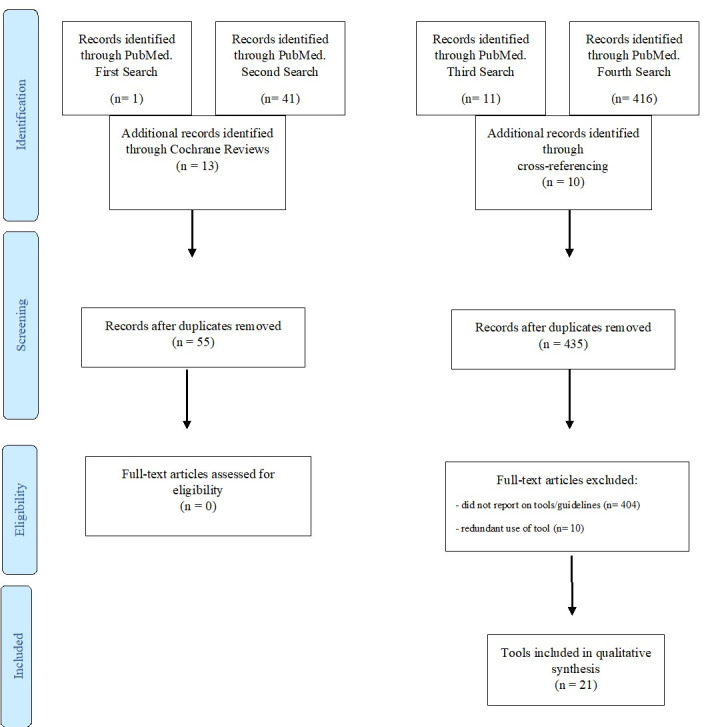
Flow diagram.
Table 2 shows the six domains that are covered by these tools and instruments. These six domains were reduced to four by merging both cultural and structural sensitivity, and cultural and structural representativeness.
Table 2.
Evaluating existing tools
| Cultural awareness and reflexivity | Cultural and linguistic validation | Sensitivity to cultural diversity | Sensitivity to structural vulnerabilities | Representativeness of cultural minority groups | Representativeness of socially excluded populations | |
| Knowledge, Efficacy, and Practices Instrument42 | · | · | · | · | · | |
| Cross-Cultural Competence Instrument for Healthcare Professionals43 | · | · | · | |||
| Primary Care Assessment Tool44 | · | · | · | · | ||
| Clinical Cultural Competency Questionnaire45 | · | · | · | · | ||
| Tool for Assessing Cultural Competence Training46 | · | · | · | · | · | |
| Cultural Competence Scale47 | · | · | · | |||
| Intercultural Development Inventory48 | · | · | · | |||
| Standards for Transcultural Nursing49 | · | · | · | · | · | |
| The CAMHS Cultural Competence in Action Tool50 | · | · | · | · | ||
| Escala de Medición Competencia Cultural51 | · | · | · | · | * | * |
| The Cultural Competence Assessment Instrument52 | · | · | · | · | ||
| Inventory for Assessing Process of Cultural Competence Among Healthcare Professionals53 | · | |||||
| Healthcare Provider Cultural Competence Instrument54 | · | · | · | · | * | * |
| Structural Vulnerability Assessment Tool for the Clinical Encounter12 | * | * | · | · | ||
| Critical Race Theory (tool)19 | · | · | · | · | ||
| Structural Foundations of Health18 | · | · | · | · | ||
| Self-Assessment Checklist55 | · | · | · | · | ||
| Ethnic-Sensitive Inventory56 | · | · | · | · | · | |
| Agency Cultural Competence Checklist—Revised57 | · | · | · | · | · | |
| Multiculturally Competent Service System Assessment Guide58 | · | · | · | · | · | |
| Iowa Cultural Understanding Assessment—Client Form59 | · | · | · | · | · |
*When these domains were implicit throughout the tool/instrument, but did not have a specific section dedicated to these domains like in other tools/instruments.
CAMHS, Child and Adolescent Mental Health Services.
Domain 1: cultural awareness and reflexivity
In clinical care, this domain assesses whether health professionals are reflexively analysing how their cultural, ethnic, gender and social backgrounds, including the culture of their expert system, interact with the cultural background of patients and families and may affect clinical communication. In the field of health education and promotion, it is often aimed at raising awareness of the different perceptions among experts and lay systems. In this domain, the issue that is considered critical is an intangible attribute such as reflexivity. In our sample of 21 tools, this issue was clearly present in 19 of them. In one case,12 it was indirectly addressed through the idea of cultural humility. Applied to epidemiological research, this domain can be defined as the capacity of the research team to reflexively analyse how their cultural, ethnic, social and expert background interact with those of the participants, and can affect research questions, design, recruitment, data collection, data analysis and dissemination activities.
Domain 2: cultural and linguistic validation
This domain refers to the cultural and linguistic adaptation of instruments, tools, questionnaires, interviews, informed consents, health advice, prescriptions, and various interactions between health professionals or experts and patients and lay systems by extension. It also usually includes the adjustment of health services to the cultural and linguistic background of the users, for example, through the translation of information or the adaptation of protocols, settings and schedules. Among the 21 tools analysed, this domain was present in 18 of them. In the field of epidemiological research, this domain can be defined as the linguistic and cultural adaptation of instruments, tools, informed consents, and participant information sheets, questionnaires, interactions between researchers and participants, and dissemination outputs addressed to the participants.
Domain 3: sensitivity to cultural diversity and structural vulnerabilities
The idea of merging sensitivity to cultural diversities and to social inequalities responds here to the already mentioned complementarity between these perspectives. Cultural sensitivity refers to motivation and curiosity for diverse cultural realities, whether they come from patients, participants in a health promotion programme, users of a service, beneficiaries of a health policy or populations under study. Cultural knowledge can be understood as a result of cultural sensitivity. Similar reasoning can be applied to the case of sensitivity to structural vulnerabilities and social inequalities, and their correlates in knowledge on health disparities. Among the tools analysed, most contemplated some form of cultural sensitivity (19 clearly and 1 indirectly) or structural sensitivity (18). In the field of epidemiological research, this domain can be defined as the incorporation of variables and relevant information on cultural diversity and structural vulnerabilities of the groups under study in any of the phases of epidemiological research.
Domain 4: representativeness of minority groups and excluded populations
As in the previous domain, in this one we have merged the representativeness of minority groups and excluded populations, which may overlap since diversity and inequality often run together. Generally, this domain has to do with the inclusion of disadvantaged and hidden groups, especially in health policies and services, with the objectives of improving the health of these groups, making their unequal situation visible, favouring their empowerment and health literacy, and recognising their citizenship rights. In our analysis, we observed that this was the domain least present, as it was only included directly in half of the tools. Nevertheless, its inclusion can be considered strategic because of its capacity for social transformation of the most vulnerable populations. In the context of epidemiological research, this domain can be defined as the ability to favour the representativeness of minority groups and excluded populations throughout the different phases of the study, such as the composition of the research team, the selection of the sample, and the development of dissemination and RRI activities.
The Structural and Intercultural Competence for Epidemiological Studies guidelines
The four reported domains can be related to main stages of epidemiological research, such as (1) research team building and research questions; (2) study design, participant recruitment, data collection and data analysis; and (3) dissemination. Table 3 reveals the intersection between the cultural and structural domains and the epidemiological stages and a series of resulting items. Most of them relate to pre-existing instruments that account for intercultural and/or structural competence in other health fields. Other elements were obtained indirectly and were the result of a consensus among the different authors. One of them, item 14, has been expanded thanks to the valuable contribution of one of this article’s reviewers, who recommended including a second specific question already existing in the Bridging Research Integrity and Global Health Epidemiology (BRIDGE) guidelines.32 33 The result is a checklist of 22 items (see table 4) in which the items have been converted into questions that guide the researchers in their self-assessment.
Table 3.
Structural and intercultural domains and criteria
| Research team building and research questions | Study design, recruitment, data collection and data analysis | Dissemination | |
| Cultural awareness and reflexivity | 1. Reflexivity on cultural and ethnic team composition compared with the populations under study. 2. Tools and instruments for ensuring team reflexivity. |
9. Awareness of cultural biases from previous research done on a similar topic/population. 10. Reflexivity on social and cultural sources of potential bias or imprecision. 11. Considering the association of missing data with sociocultural characteristics of populations under study. |
19. Inclusion of the groups under study in the dissemination plan through reflexivity and awareness on the potential linguistic, cultural and social gaps. |
| Cultural validation | 3. Awareness of the lay/expert decalages. 4. Adequate use of categories such as race, culture and ethnicity in the research questions. |
12. Cultural and linguistic validation of informed consent, and of instruments such as questionnaires and scales. 13. Integration of qualitative research (eg, in-depth interviews and focus groups) and/or mixed methods in the epidemiological design and the selection of instruments. |
20. Dissemination outputs addressed and culturally tailored to the population under study. |
| Sensitivity to cultural diversity and structural vulnerabilities | 5. Team training in intercultural and structural competence. 6. Cultural and social knowledge of populations under study, including ethnic minorities and marginalised groups, and lay perspectives on the topics of study. 7. Knowledge about the medical history of the country/community in which the research is taking place and the legacy that medical research has on ethnic minorities/hidden populations. |
14. Including cultural variables in the study design. Assessing causal mechanisms associated with these variables and the limitations of using these variables as proxies for more complex categories. 15. Including social determinants of health and structural vulnerability variables in the study design. 16. Use of local knowledge to interpret findings, for example, local ideas and beliefs regarding disease aetiology or transmission. |
21. Consideration of the cultural and social specificities of the population studied in the conclusions, recommendations and application of the results of the study. |
| Representativeness of minority groups and excluded populations | 8. Representativeness of cultural diversity and civil society in the team, including lay participants and/or minority and marginalised groups. | 17. Facilitating the participation of excluded groups and minorities through sample representativeness. 18. Assessing the social and cultural barriers to their participation in the study. |
22. Promoting the participation of excluded groups and minorities in the dissemination and RRI activities. |
RRI, Responsible Research and Innovation.
Table 4.
The Structural and Intercultural Competence for Epidemiological Studies guidelines
| Domains | Guide questions |
| Research team building and research questions | 1. Has the research team identified its ethnic, cultural, and social composition and compared it with that of the study population? Has the research team taken into account the potential impact that these differences or similarities may have on the research? 2. Does the research team have any tools or means to facilitate reflexivity, for example, fieldnotes or regular meetings for this purpose? 3. Does the research team consider the lay views on the topics of study? 4. Has the research team assessed whether the use of concepts such as race, ethnicity or culture (among others) in the study is adequate? 5. Have the research team’s training needs in intercultural and structural competence been assessed? 6. Does the research team have cultural and social knowledge of the populations under study, including ethnic minorities and marginalised groups and lay perspectives on the topics of study? 7. Has the research team considered the medical history of the country in which the research is taking place and the legacy that medical research has on ethnic minorities/hidden populations? 8. Has the research team established an advisory board which includes representatives of different cultural and/or ethnic groups, including lay participants representing civil society and/or minority collectives? |
| Study design, recruitment, data collection and data analysis | 9. Is the research team aware of cultural and social biases from previous research done on a similar topic/population that they are using as a research background? 10. Has the research team considered social and cultural sources of potential bias or imprecision? For example, if the research hypothesis, the objectives of the study, the theoretical–conceptual framework, or the sample gives rise to possible sensitive cultural issues or ethnocentric statements? 11. Has the association of missing data with sociocultural characteristics of populations under study been considered? 12. Are the informed consent and the questionnaires, scales, and instruments understandable to the participants and/or culturally validated or tailored to the population under study? 13. Has qualitative research or mixed methods been included in the design of the study, that is, for the selection of the instruments or for the collection of qualitative data on the research subject? 14. Have cultural variables been included in the study design such as ethnicity, cultural identity, religious beliefs or acculturation, among others? In addition, and following the Bridging Research Integrity and Global Health Epidemiology guidelines, have the different causal mechanisms associated with these variables been considered and the limitations of using these variables as proxies for more complex categories been acknowledged? 15. Does the study address how symptoms, clinical problems, diseases and/or attitudes toward patients, populations and/or health systems are influenced by social determinants of health and structural vulnerabilities? For example, but not limited to discrimination, lack of financial security, lacking safe/stable place, risk environments, difficulty in food access, lack of social network, problems with legal status and/or lack of formal education. 16. Has local knowledge been considered in interpreting the results of the study, that is, local ideas on aetiology and disease transmission? 17. Does the sample consider subsamples of cultural minority groups, groups subject to health disparities, and/or historically under-represented? And if so, in what way, that is, has the analysis been disaggregated for such variables or have they been considered as confounder/effect modifiers? 18. Have barriers to participation in the study arising from structural vulnerabilities been analysed? If so, has the inclusion of these participants been facilitated in any way? |
| Dissemination | 19. Does the dissemination plan include the groups under study? Does this plan include reflexivity and awareness on potential linguistic, cultural and social gaps? 20. As part of the dissemination of the results, has any output (ie, publication or audio-visual document) been addressed and culturally tailored to the population studied (ie, tested in a focus group)? 21. Have the cultural and social specificities of the studied groups been considered in the conclusions, recommendations and in the implementation of the results? 22. Is there a dissemination or Responsible Research and Innovation plan considering the active role of participants and stakeholders? If so, have barriers to participation been assessed and active participation been facilitated? |
Conclusion
To our knowledge, the Structural and Intercultural Competence for Epidemiological Studies (SICES) checklist is the first systematic attempt to bring the structural and intercultural competence into epidemiological research. Based on the selection and adaptation of a series of criteria developed for other health fields, we have proposed a checklist that should be understood as a starting point rather than as a destination. The methodology we followed was the same as the one used for the elaboration of the Consolidated Criteria for Reporting Qualitative Research34: data extraction and analysis of previous instruments and checklists, in this case on intercultural and structural competence. To this process, we have added a dimension of internal consensus, as the authors of this paper include both medical anthropologists specialising in intercultural and structural competence and epidemiologists with experience in designing and conducting epidemiological research. In this sense, and if we follow the Moher et al’s guidance for developers of health research reporting guidelines,35 SICES would be better defined as working guidelines, or even a guidance, whose purpose is to help promote a common language between epidemiology and structural and intercultural competence. SICES complements well with other guidelines and standards focused on related issues, such as the BRIDGE guidelines.
SICES arranges a set of criteria that can be useful not just for strengthening the structural and intercultural competence, but also the self-reflection and self-evaluation of research teams. Reflexivity is an intangible domain that has to do with attitudes and predispositions and has an influence on the quality of research. For example, self-reflection on cultural and social gaps between the research team and the populations under study can provide new clues for reducing bias and interpreting the findings, favour the commitment of these populations to research results and their dissemination, and strengthen health literacy and empowerment among the most vulnerable groups. The impact of embracing a structural and intercultural competence perspective has different faces, but they all encourage a more dialogical relationship between researchers and the public. This is the purpose of these guidelines. We invite readers to improve this checklist with comments, critiques and suggestions.
Acknowledgments
We would like to thank the two anonymous reviewers for their excellent comments, criticisms and suggestions on an earlier version of this article.
Footnotes
Handling editor: Seye Abimbola
Contributors: AM-H and DB conceived the idea, designed the study and wrote the manuscript. DB and AM-H developed the review, the data extraction and analysis, and both verified the underlying data. AR-L, AS-N, CS, EV, JLA-M, JMH, LAR-U and LR-M reviewed the various drafts of the article. All authors discussed the results and contributed to the final manuscript.
Funding: This project has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement no 825884 (SYNergies for Cohorts in Health: integrating the ROle of all Stakeholders, SYNCHROS). AM-H acknowledges the financial support from Institut Català de la Recerca i Estudis Avançats (ICREA) under the ICREA Academia Award.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article.
References
- 1.Betancourt JR, Green AR. Commentary: linking cultural competence training to improved health outcomes: perspectives from the field. Acad Med 2010;85:583–5. 10.1097/ACM.0b013e3181d2b2f3 [DOI] [PubMed] [Google Scholar]
- 2.Martinez KM, Green CE, Sañudo FM. The CLAS challenge: promoting culturally and linguistically appropriate services in health care. International Journal of Public Administration 2004;27:39–61. 10.1081/PAD-120028652 [DOI] [Google Scholar]
- 3.Green AR, Miller E, Krupat E, et al. Designing and implementing a cultural competence OSCE: lessons learned from interviews with medical students. Ethn Dis 2007;17:344–50. [PubMed] [Google Scholar]
- 4.Fleckman JM, Dal Corso M, Ramirez S, et al. intercultural competency in public health: a call for action to incorporate training into public health education. Front. Public Health 2015;3:210. 10.3389/fpubh.2015.00210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tervalon M, Murray-García J. Cultural humility versus cultural competence: a critical distinction in defining physician training outcomes in multicultural education. J Health Care Poor Underserved 1998;9:117–25. 10.1353/hpu.2010.0233 [DOI] [PubMed] [Google Scholar]
- 6.Sue S. In defense of cultural competency in psychotherapy and treatment. Am Psychol 2003;58:964–70. 10.1037/0003-066X.58.11.964 [DOI] [PubMed] [Google Scholar]
- 7.Betancourt JR, Green AR, Carrillo JE, et al. Cultural competence and health care disparities: key perspectives and trends. Health Aff 2005;24:499–505. 10.1377/hlthaff.24.2.499 [DOI] [PubMed] [Google Scholar]
- 8.De Jong JTVM, Van Ommeren M. Mental health services in a multicultural society: interculturalization and its quality surveillance. Transcult Psychiatry 2005;42:437–56. 10.1177/1363461505055625 [DOI] [PubMed] [Google Scholar]
- 9.Agier M, Lecadet C. Un Monde de camps. Paris: La Découverte, 2014. [Google Scholar]
- 10.Gautier L, Sieleunou I, Kalolo A. Deconstructing the notion of "global health research partnerships" across Northern and African contexts. BMC Med Ethics 2018;19:49. 10.1186/s12910-018-0280-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Napier AD, Ancarno C, Butler B, et al. Culture and health. The Lancet 2014;384:1607–39. 10.1016/S0140-6736(14)61603-2 [DOI] [PubMed] [Google Scholar]
- 12.Bourgois P, Holmes SM, Sue K, et al. Structural vulnerability: Operationalizing the concept to address health disparities in clinical care. Acad Med 2017;92:299–307. 10.1097/ACM.0000000000001294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Petty J, Metzl JM, Keeys MR. Developing and evaluating an innovative structural competency curriculum for pre-health students. J Med Humanit 2017;38:459–71. 10.1007/s10912-017-9449-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Metzl JM, Petty J, Olowojoba OV. Using a structural competency framework to teach structural racism in pre-health education. Soc Sci Med 2018;199:189–201. 10.1016/j.socscimed.2017.06.029 [DOI] [PubMed] [Google Scholar]
- 15.Neff J, Holmes SM, Knight KR, et al. Structural competency: curriculum for medical students, residents, and interprofessional teams on the structural factors that produce health disparities. MedEdPORTAL 2020;16:10888. 10.15766/mep_2374-8265.10888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hansen H. Metzl JM editors. Structural competency in mental health and medicine. A case-based approach to treating the social determinants of health. Cham, Switzerland: Springer, 2019. [Google Scholar]
- 17.Kirmayer LJ. Rethinking cultural competence. Transcult Psychiatry 2012;49:149–64. 10.1177/1363461512444673 [DOI] [PubMed] [Google Scholar]
- 18.Metzl JM, Petty J. Integrating and assessing structural competency in an innovative prehealth curriculum at Vanderbilt university. Acad Med 2017;92:354–9. 10.1097/ACM.0000000000001477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Freeman R, Gwadz MV, Silverman E, et al. Critical race theory as a tool for understanding poor engagement along the HIV care continuum among African American/Black and Hispanic persons living with HIV in the United States: a qualitative exploration. Int J Equity Health 2017;16:54 https://dx.doi.org/10.1186%2Fs12939-017-0549-3 10.1186/s12939-017-0549-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Geertz C. The interpretation of cultures. New York: Basic Books, 1973. [Google Scholar]
- 21.Giddens A. The constitution of society: outline of the theory of Structuration. Berkeley, CA: Univ of California Press, 1984. [Google Scholar]
- 22.Sousa VD, Rojjanasrirat W, Translation RW. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: a clear and user-friendly guideline. J Eval Clin Pract 2011;17:268–74. 10.1111/j.1365-2753.2010.01434.x [DOI] [PubMed] [Google Scholar]
- 23.Berkman LF, Kawachi I, Glymour MM, eds. Social epidemiology. Oxford: Oxford University Press, 2014. [Google Scholar]
- 24.Hersch-Martínez P. Epidemiología sociocultural: Una perspectiva necesaria. Salud Pública de México 2013;55:512–8. [PubMed] [Google Scholar]
- 25.Bach M, Jordan S, Hartung S, et al. Participatory epidemiology: the contribution of participatory research to epidemiology. Emerg Themes Epidemiol 2017;14:1–5. 10.1186/s12982-017-0056-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prussing E. Critical epidemiology in action: research for and by Indigenous peoples. SSM - Population Health 2018;6:98–106 https://dx.doi.org/10.1016%2Fj.ssmph.2018.09.003 10.1016/j.ssmph.2018.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Almeida Filho N. Epidemiologia SEM números. Rio de Janeiro: Campus, 1989. [Google Scholar]
- 28.Owen R, Macnaghten P, Stilgoe J. Responsible research and innovation: from science in society to science for Society, with Society. Science and Public Policy 2012;39:751–60. 10.1093/scipol/scs093 [DOI] [Google Scholar]
- 29.Adams V, Burke NJ, Whitmarsh I. Slow research: thoughts for a movement in global health. Med Anthropol 2014;33:179–97. 10.1080/01459740.2013.858335 [DOI] [PubMed] [Google Scholar]
- 30.Kingori P, Gerrets R. The masking and making of fieldworkers and data in postcolonial Global Health research contexts. Crit. Public Health 2019;8;29:494–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bourgois P, Martinez A, Kral A, et al. Reinterpreting ethnic patterns among white and African American men who inject heroin: a social science of medicine approach. PLoS Med 2006;3:e452. 10.1371/journal.pmed.0030452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alba S, Verdonck K, Lenglet A, et al. Bridging research integrity and global health epidemiology (bridge) statement: guidelines for good epidemiological practice. BMJ Global Health 2020;5:e003236. 10.1136/bmjgh-2020-003236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alba S, Lenglet A, Verdonck K, et al. Bridging research integrity and global health epidemiology (bridge) guidelines: explanation and elaboration. BMJ Glob Health 2020;5:e003237. 10.1136/bmjgh-2020-003237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 35.Moher D, Schulz KF, Simera I, et al. Guidance for developers of health research reporting guidelines. PLoS Med 2010;7:e1000217. 10.1371/journal.pmed.1000217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pelto PJ, Pelto GH, knowledge S. Culture, and behavior in applied medical anthropology. Med Anthropol Q 1997;11:147–63. [DOI] [PubMed] [Google Scholar]
- 37.Hahn RA, Kleinman A. Biomedical practice and anthropological theory: frameworks and directions. Annu Rev Anthropol 1983;12:305–33 https://www.jstor.org/stable/2155650 10.1146/annurev.an.12.100183.001513 [DOI] [Google Scholar]
- 38.Hahn RA. Sickness and healing: an anthropological perspective. New Haven: Yale University Press, 1995. [Google Scholar]
- 39.Board American anthropological association (AAA) . AAA statement on race. Am Anthropol 1998;100:712–3. 10.1525/aa.1998.100.3.712 [DOI] [Google Scholar]
- 40.Fuentes A, Ackermann RR, Athreya S. The American association of physical Anthropologists (AAPA) statement on race and racism. Am J Phys Anthropol 2019;169:400–2. [DOI] [PubMed] [Google Scholar]
- 41.Norton HL, Quillen EE, Bigham AW. Human races are not like dog breeds: refuting a racist analogy. Evolution: Education and Outreach 2019;12:1–20. [Google Scholar]
- 42.Garvan GJ, Garvan CW, Behar-Horenstein LS. Developing and testing the short-form knowledge, efficacy, and practices instrument for assessing cultural competence. J Dent Educ 2016;80:1245–52. 10.1002/j.0022-0337.2016.80.10.tb06208.x [DOI] [PubMed] [Google Scholar]
- 43.Bernhard G, Knibbe RA, von Wolff A, et al. Development and psychometric evaluation of an instrument to assess cross-cultural competence of healthcare professionals (CCCHP). PLoS One 2015;10:e0144049. 10.1371/journal.pone.0144049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Berra S, Hauser L, Audisio Y, et al. Validez Y fiabilidad de la versión Argentina del PCAT-AE para evaluar La atención primaria de salud. Rev Panam Salud Publica 2013;33:30–9. 10.1590/S1020-49892013000100005 [DOI] [PubMed] [Google Scholar]
- 45.Betancourt JR. Cultural competency: providing quality care to diverse populations. The Consultant Pharmacist 2006;21:988–95. 10.4140/TCP.n.2006.988 [DOI] [PubMed] [Google Scholar]
- 46.Lie D, Boker J, Cleveland E. Using the tool for assessing cultural competence training (TACCT) to measure faculty and medical student perceptions of cultural competence instruction in the first three years of the curriculum. Acad Med 2006;81:557–64. 10.1097/01.ACM.0000225219.53325.52 [DOI] [PubMed] [Google Scholar]
- 47.Perng S-J, Watson R. Construct validation of the nurse cultural competence scale: a hierarchy of abilities. J Clin Nurs 2012;21:1678–84. 10.1111/j.1365-2702.2011.03933.x [DOI] [PubMed] [Google Scholar]
- 48.Kruse JA, Didion J, Perzynski K. Utilizing the Intercultural development Inventory® to develop intercultural competence. Springerplus 2014;3:334. 10.1186/2193-1801-3-334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Leuning CJ, Swiggum PD, Wiegert HMB, et al. Proposed standards for transcultural nursing. J Transcult Nurs 2002;13:40–6 https://doi.org/10.1177%2F104365960201300107 10.1177/104365960201300107 [DOI] [PubMed] [Google Scholar]
- 50.Papadopoulos I, Tilki M, Ayling S. Cultural competence in action for CAMHS: development of a cultural competence assessment tool and training programme. Contemp Nurse 2008;28:129–40. 10.5172/conu.673.28.1-2.129 [DOI] [PubMed] [Google Scholar]
- 51.Pedrero V, Bernales M, Chepo M, et al. Development of an instrument to measure the cultural competence of health care workers. Rev. saúde pública 2020;54:29. 10.11606/s1518-8787.2020054001695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schim SM, Doorenbos AZ, Miller J, et al. Development of a cultural competence assessment instrument. J Nurs Meas 2003;11:29–40. 10.1891/jnum.11.1.29.52062 [DOI] [PubMed] [Google Scholar]
- 53.Associates TCAR . Inventory for assessing the process of cultural competence among healthcare professionals (IAPCC), 2020. Available: http://transculturalcare.net/iapcc-r/
- 54.Schwarz JL, Witte R, Sellers SL, et al. Development and psychometric assessment of the healthcare provider cultural competence instrument. Inquiry 2015;52. 10.1177/0046958015583696. [Epub ahead of print: 24 04 2015]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Goode TD. Self-Assessment checklist for personnel providing services and supports in early intervention and early childhood settings. promoting cultural competence and cultural diversity in early intervention and early childhood settings. Washington DC: National Center for Cultural Competence. Georgetown University Child Development Center, 2000. https://nccc.georgetown.edu/assessments/. (accessed May 10, 2020). [Google Scholar]
- 56.MK H. Use of ethnic-sensitive inventory (ESI) to enhance practitioner skills with minorities. J Multicult Soc Work 1990;1:57–68. [Google Scholar]
- 57.Dana R. Understanding cultural identity in intervention and assessment. Thousand Oaks (CA): SAGE publications, 1998. [Google Scholar]
- 58.The Connecticut Department of Children and Families Office of Multicultural Affairs . Developing a Multiculturally competent service system for an organization or program, 2002. Available: https://portal.ct.gov/-/media/dcf/Multicultural_Affairs/pdf/MCAservicesystempdf.pdf?la=en
- 59.White K, Clayton R, Arndt S. Culturally competent substance abuse treatment project: annual report. Iowa City, Ia: Iowa Consortium for substance abuse research and evaluation, 2009. https://icsa.uiowa.edu/sites/icsa.uiowa.edu/files/projects/Culturally%20Competent%20Substance%20Abuse%20Treatment%20Project%20-%20Evaluation%20Report%202009.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article.


