Abstract
Introduction and importance
Ileosigmoid knotting is a surgical emergency. Common in Asian males, it is presented with signs and symptoms of diffuse peritonitis. Aggressive resuscitation with intravenous fluids and antibiotics followed by workup enable the patient hemodynamically stable. Explorative laparotomy followed by colo-colic anastomosis and double barrel ileostomy is curative.
Case presentation
A 32-year-old-male from Nepal with a chief complain of diffuse abdominal pain for a day and signs of peritonitis presented to Emergency room. After assessing and stabilizing the patient, explorative laparotomy was performed. Ileal and sigmoid resection followed by colo-colic anastomosis and double barrel ileostomy was done. On regular follow-up, he is in his usual state of health.
Discussion
The incidence of ileosigmoid knotting is reported to be about 1.6 cases per year. It is often misdiagnosed as non-specific intestinal obstruction which confers poor prognostic value to the patient. It should be identified promptly and intervened timely.
Conclusion
Ileosigmoid knotting is a rare but dangerous differential of acute abdomen not to be missed. Early assessment and quick decision making is the key to provide excellent prognosis to the patient in need, provided adequate surgical skills are demonstrated.
Keywords: Ileosigmoid, Knotting, Explorative laparotomy, Anastomosis, Resection
Highlights
-
•
Ileosigmoid knotting is a surgical emergency.
-
•
It is common in Asian males.
-
•
Patient presents with signs and symptoms of diffuse peritonitis.
-
•
Explorative laparotomy should be done.
-
•
Ileal and sigmoid resection followed by colo-colic anastomosis with double barrel ileostomy was performed.
1. Introduction
Ileosigmoid knotting (ISK), also known as compound volvulus or double volvulus, is an unusual surgical emergency causing intestinal obstruction [1], [2], [3]. Predominantly, it is a closed-loop intestinal obstruction that involves the sigmoid and ileum [4]. First described in the literature by Parker in 1845, it may promptly progress to a gangrenous state in both the sigmoid and the ileum [1]. The aim of reporting this case is to increase understanding of the condition to promote earlier diagnosis and successful intervention for better patient outcome. Since endoscopic decompression is contraindicated in ISK, it is important to differentiate between simple sigmoid volvulus and ISK.
Less than 500 cases have been stated in the literature as of 2018 [5], [6]. It is interesting to note that the incidence of ISK is relatively high in eastern Anatolia [7], [8], [9].
We present a case report of a 32-year-old-male presented with acute abdomen in the Emergency room with signs of diffuse peritonitis. Erect abdominal X-ray demonstrated dilated loops. He was resuscitated with intravenous fluids and antibiotics. Explorative laparotomy was done. A diagnosis of ISK was established and segmental ileal and sigmoid resection was done. The patient was shifted to intensive care unit and discharged after sixth post-operative day.
This case report is reported in line with SCARE guidelines [10].
2. Case presentation
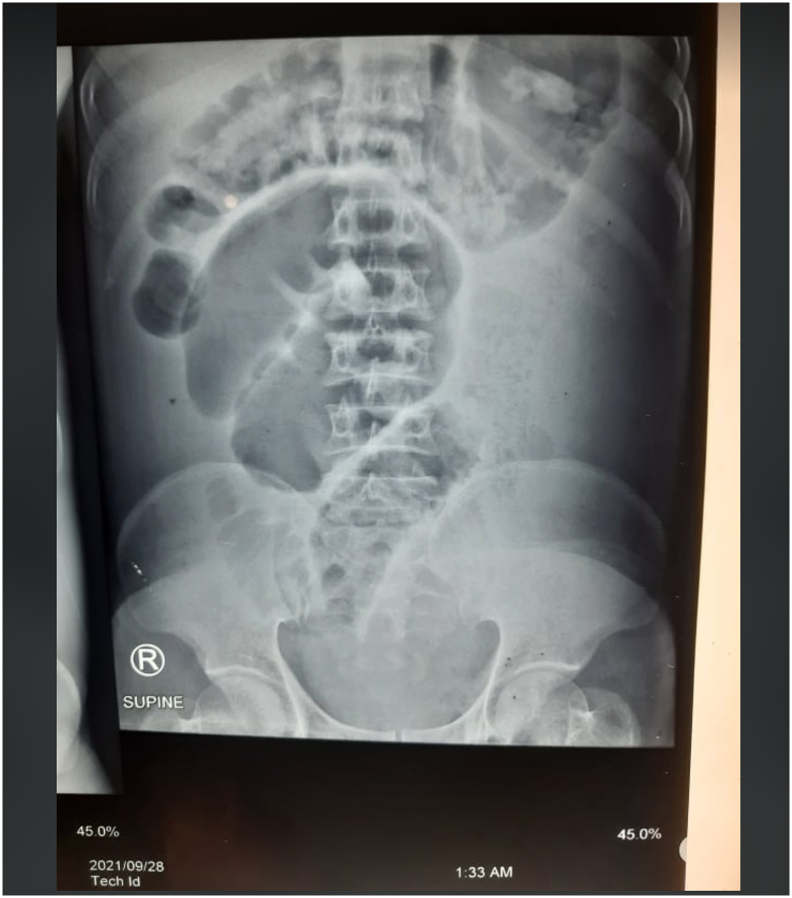
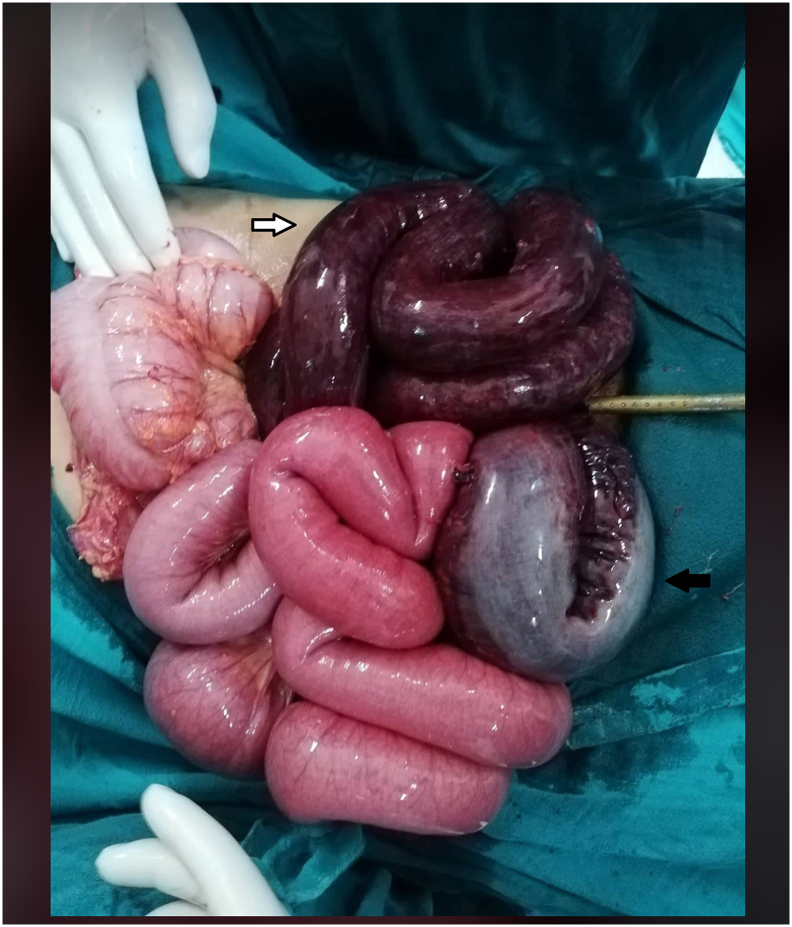
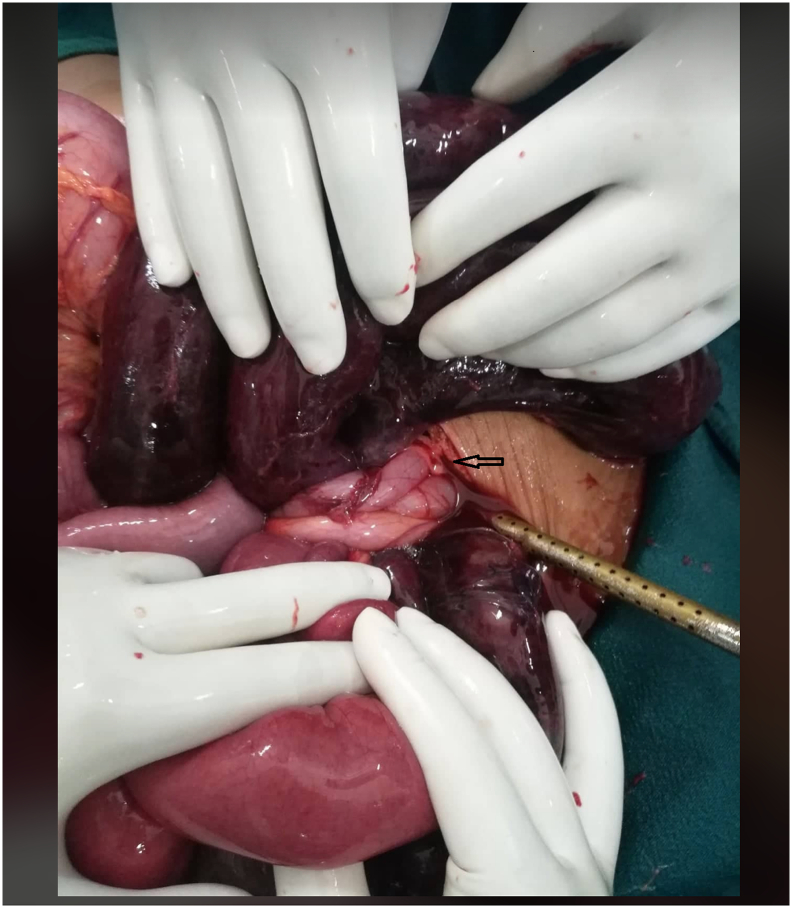
A 32-year-old male presented with diffuse abdominal pain of 1-day duration. The patient stated no history of blunt trauma or previous surgeries. On clinical examination, the patient was conscious, agitated and disoriented with vital signs including pulse 145 bpm, blood pressure 90/55 mm Hg, and saturation 99%. The chest examination was unremarkable. The patient's abdomen was distended and tense with signs of peritonitis. Laboratory investigations revealed a white blood count of 22 × 109 and Lactate 36.1 mmol/L. A chest x-ray revealed no signs of pneumonia or pneumothorax. An erect abdominal x-ray revealed a dilated bowel as shown in Fig. 1. The patient was resuscitated with aggressive intravenous fluid therapy and broad-spectrum antibiotics. An exploratory laparotomy was performed and revealed the distal ileum knotted around the base of the volvulus sigmoid loop base as shown in Fig. 2, Fig. 3. Intraoperatively, the closed sigmoid loop and the knotted distal ileum were gangrenous. Ileum segment resection and sigmoid resection were performed followed by colo-colic anastomosis and double barrel ileostomy. The patient was shifted to intensive care unit. Immediately after first post-operative day, there was high stoma output (around 800 ml/day). He was then prescribed with Loperamide and bulk forming agent. Gradually his stoma output decreased and was discharged on the sixth post-operative day. He has been planned for reversal of stoma after six weeks. On regular follow-up, he is free of symptoms and in his usual state of health.
Fig. 1.
Erect abdominal X-ray revealing dilated bowel loops.
Fig. 2.
Intraoperative image showing dilated and gangrenous ileum (white arrow) and sigmoid colon (black arrow).
Fig. 3.
Intraoperative image showing ileo-sigmoid knotting.
3. Discussion
The pathogenesis of ISK is reliant on three factors: 1) a long small bowel mesentery with free mobile small bowel, 2) a long sigmoid with a narrow pedicle, and 3) a bulky diet with the presence of an empty small bowel [1], [11]. Some studies encourage the theory that a bulky diet may advance to the proximal jejunum and surge the mobility of the small bowel and fall in the left lower quadrant of the abdomen [11]. Loops of small bowel may rotate around the narrow pedicle of the sigmoid, and additionally peristalsis progresses the rotation to a closed loop of intestine [11]. Besides the anatomical factors mentioned above, several secondary factors such as late pregnancy, trans-mesenteric herniation, Meckel diverticulitis with band, and ileocecal intussusceptions also play a significant role in the pathogenesis [11]. It is reported that ISK is principally seen in certain African, Asian, and Middle-East nations and rarely in white populations [1], [3], [11].
Atamanalp has suggested a new classification based on the age of the patient, associated diseases, and the presence of gangrenous bowel as shown in Table 1 [12].
Table 1.
New classification of ileosigmoid knot proposed by Atamanalp.
| C1 | C2 |
C3 |
C4 |
C5 | C6 | |||
|---|---|---|---|---|---|---|---|---|
| C2a | C2b | C3a | C3b | C4a | C4b | |||
| A0 D0 |
One of A,D1 Either older 60 years or present of associated disease |
Two of A,D1 Older 60 years and present of associated disease |
One of A,D1 Either older 60 years or present of associated disease |
Two of A,D1 Older 60 years and present of associated disease |
One of A,D1 Either older 60 years or present of associated disease |
One of A,D1 Either older 60 years or present of associated disease |
||
| S0 | S0 Shock absent |
S0 Shock absent |
S1 Shock present |
S0 Shock present |
S0 Shock absent |
S0 Shock absent |
S0 Shock present |
S0 Shock absent |
| G0 | G0 Bowel gangrene absent |
G0 bowel gangrene absent | G0 bowel gangrene absent | G0 bowel gangrene absent | G0 bowel gangrene absent | G1 bowel gangrene in ileum or sigmoid | G1 bowel gangrene in ileum or sigmoid | G2 bowel gangrene in ileum or sigmoid |
Notes: C (class). A (age): AO: under 60 years: Al: 60 years and older. (Associated disease): DO: absent. D I: present. S (Shock): SO: absent. SI: present. G (Bowel gangrene): GO: absent. GI: present in the ileum or sigmoid colon. G2: present in both segments.
Copyright ©2009 John Wiley and Sons. Adapted from S. Selcuk Atamanalp. Giirkan Ozturk. Biilent Aydinli. M. ilhan Yildirgan. Mahmut BASOCILU, Ourkaya Oren MK. A new classification for ileosigrnoid knotting. Turk J Med SO. 2009:39(4):54I—S45.
The diagnosis of ISK is difficult to ascertain due to its infrequent and rare presentation [3], [13]. Ileosigmoid knot can be misdiagnosed radiographically as simple sigmoid volvulus, which may lead to attempts to perform endoscopic decompression by a sigmoidoscope which may lead to perforation or injury [1]. The mortality rate of ileosigmoid knot usually may reach 48% [14].
Initial management of ISK begins with aggressive intravenous fluid resuscitation followed by acid-base imbalance correction [15]. Surgical intervention should be undertaken after the achievement of hemodynamic stability [15]. Antibiotic therapy with cephalosporin and aminoglycosides should be implemented in the pre- and post-operative periods for 5–7 days [15]. Various surgical procedures to accomplish ISK are mentioned in the literature [1]. The anatomical and pathological findings intraoperatively guide the surgical procedure [1]. The most common procedure performed is ileal and sigmoid resection with primary enteroenteric anastomosis and Hartmann's procedure/colostomy for descending colon, if both ileum and sigmoid are gangrenous [1].
In one of the largest single-centre series by Atamanalp SS, the incidence of ISK was 1.6 cases per year and 0.4 cases per 100,000 persons per year with mean age of 47.5 years. Of the patients, 72.5% were male. Abdominal pain, obstipation, distention and vomiting were the most common symptoms. Abdominal tenderness, distention, hypo/akinetic bowel sounds, empty rectum, guarding/rebound tenderness, hyperkinetic bowel sounds and melanotic stool were the most common signs. Plain abdominal X-ray findings, including a dilated sigmoid colon with multiple intestinal air-fluid levels, were observed in only 7.0% of patients. The preoperative precise diagnosis rate was 13.8%. Misdiagnoses, comprising non- specific intestinal obstruction and non-obstructive acute abdomen, were noted in 68.8% and 17.5% of patients respectively [16].
Our patient was male belonging to Asian community, presented with abdominal pain and signs of diffuse peritonitis, managed initially with empirical antibiotics and intravenous fluids, and after achieving hemodynamic stability, underwent explorative laparotomy followed by segmental ileal and sigmoid resection with colo-colic anastomosis and double barrel ileostomy.
4. Conclusion
Ileosigmoid knotting, a surgical emergency, should be kept in the back of our mind if patients present with symptoms and signs of diffuse peritonitis, thereby emphasizing an utmost necessary to distinguish it from sigmoid volvulus. Timely intervention can provide excellent prognosis to the patient, provided good surgical skills are demonstrated.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
Not required.
Funding
None.
Guarantor
Sushil Sharma Subedi.
Research registration number
Not applicable.
CRediT authorship contribution statement
Sushil Sharma Subedi (SSS), Rakesh Kumar Gupta (RKG), Durga Neupane (DN), Sunit Agrawal (SA), Bhawani Khanal (BK), Lokesh Shekher Jaiswal (LSJ) = Study concept, Data collection, and surgical therapy for the patient.
Sushil Sharma Subedi (SSS), Durga Neupane (DN), Lokesh Shekher Jaiswal (LSJ) = Writing- original draft preparation.
Sushil Sharma Subedi (SSS), Durga Neupane (DN), Sunit Agrawal (SA), Bhawani Khanal (BK) = Editing and writing.
Sushil Sharma Subedi (SSS), Durga Neupane (DN), Lokesh Shekher Jaiswal (LSJ) = senior author and manuscript reviewer.
All the authors read and approved the final manuscript.
Declaration of competing interest
None.
Acknowledgment
None.
References
- 1.Mandal A., Chandel V., Baig S. Ileosigmoid knot. Indian J. Surg. 2012;74(2):136–142. doi: 10.1007/s12262-011-0346-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adili W., Jm M., Bm N. The ileosigmoid knot: a case report. Ann. Afr. Surg. 2014;11(2):1. [Google Scholar]
- 3.Lee S., Park Y.H., Won Y.S. Case report the ileosigmoid knot: ct findings. AJR. 2000;174(3):685–687. doi: 10.2214/ajr.174.3.1740685. [DOI] [PubMed] [Google Scholar]
- 4.Al-qahtani J., Faidah A., Yousif M., Kurer M.A., Ali S.M. Ileosigmoid knotting, rare cause of intestinal obstruction and gangrene. Open Access J. Surg. 2017;7(3):8–11. doi: 10.19080/OAJS.2017.07.555712. [DOI] [Google Scholar]
- 5.Web of Science. Ileosigmoid knotting. [Accessed January 2018]. Accessible via: http://apps.webofknowledge.com/ WOS_GeneralSearch_input.do?product=WOS&search_ mode=GeneralSearch.
- 6.Pubmed Central. Ileosigmoid knotting. [Accessed January 2018]. Accessible via: https://www.ncbi.nlm.nih.gov/pub med/?term=Ileosigmoid knotting.
- 7.Atamanalp S.S. Ileosigmoid knotting: clinical appearance of 73 cases over 45.5 years. ANZ J. Surg. 2013;83(1–2):70–73. doi: 10.1111/j.1445-2197.2012.06146.x. [DOI] [PubMed] [Google Scholar]
- 8.Atamanalp S.S. Treatment for ileosigmoid knotting: a single-center experience of 74 patients. Tech. Coloproctol. 2014;18(3):233–237. doi: 10.1007/s10151-013-1046-3. [DOI] [PubMed] [Google Scholar]
- 9.Atamanalp S.S., Korkut E., Karadeniz E., Aksungur N. Ileosigmoid knotting: changing trends over 50 years. Indian J Surg. 2017 doi: 10.1007/s12262-017-1636-9. [DOI] [Google Scholar]
- 10.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 11.Machado N.O. Ileosigmoid knot: a case report and literature review of 280 cases. Ann. Saudi Med. 2009;29(5):402–406. doi: 10.4103/0256-4947.55173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Atamanalp S.S., Oeztuerk G., Aydinli B., et al. A new classification for ileosigmoid knotting. Turk. J. Med. Sci. 2009;39(4):541–545. doi: 10.3906/sag-0810-1. [DOI] [Google Scholar]
- 13.Mungazi G.S., Mutseyekwa B., Sachikonye M. A rare occurrence of viability of both small and large bowel in ileosigmoid knotting: a case report. Int. J. Surg. Case Rep. 2018;49:1–3. doi: 10.1016/j.ijscr.2018.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nagappan R.N. A rare case of ileo-sigmoid knotting compound vol-vulus case report. Univ. J. Surg. Surg Spec. 2019;5(5):4–7. [Google Scholar]
- 15.Tokta O., Çim N. Ileosigmoid knot as a cause of acute abdomen at 28 weeks of pregnancy: a rare case report. East J. Med. 2017;22(3):110–113. doi: 10.5505/ejm.2017.35220. [DOI] [Google Scholar]
- 16.Atamanalp S.S. Ileosigmoid knotting: one of the largest single-center series. Pak J Med Sci. 2018;34(3):671–675. doi: 10.12669/pjms.343.14893. May-Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]