Abstract
Objectives/Hypothesis: To perform a systematic review and meta-analysis to compare the efficacy of and complications associated with antifungal drugs and traditional antiseptic medication for the treatment of otomycosis.
Data Sources: The PubMed, EMBASE, GeenMedical, Cochrane Library, CBM, CNKI, VIP and other databases were searched from January 1991 to January 2021.
Methods: The systematic literature review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Randomized controlled trials (RCTs) and non-randomized studies (case-control, cohort, and case series) were included to assess the topical use of antifungal drugs and traditional antiseptic medication in patients with otomycosis. The research subjects were patients who were clinically diagnosed with otomycosis and whose external auditory canal secretions were positive for fungi. Funnel plots were used to detect bias, and the Q test was used to assess heterogeneity. The random-effects model was used for meta-analysis. The t-test was used to assess significance.
Results: Of the 324 non-duplicate studies screened, 16 studies met the criteria for full-text review, and 7 were included in the meta-analysis. Four studies reported recovery conditions (P = 0.01). Six common complications after medication use were compared, and there were no significant differences. The authors further conducted subgroup analysis according to complications. The differences in the rates of ear distension (P = 0.007), earache (P = 0.03) and tinnitus (P = 0.003) were statistically significant.
Conclusion: The results of this meta-analysis and literature review showed that antifungal drugs and traditional antiseptic medication were effective in relieving symptoms in patients with otomycosis, and the two treatments were associated with different complications. Otolaryngologists have the option to use one medication or a combination of two drugs on the basis of the condition. Future research in this area should include RCTs with long-term follow-up to guide the development of otomycosis guidelines to overcome some of the weaknesses found in the literature.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/#myprospero.
Keywords: otomycosis, antifungal drug, traditional antiseptic medication, recovery rate, complication
Introduction
Otitis externa is a superficial fungal infection that can involve the middle ear, which is affected in more than 10% of all otitis externa cases (1). Bacterial infections of the ears are usually acute, while mycotic infections may be acute or subacute and cause inflammation and itching (2). Severe infections are generally caused by bacteria and may lead to the secretion of pus. As a chronic ear disease of the external auditory canal, the incidence of otomycosis is highest in the hot and humid seasons and lowest in the cold season. The most common pathogenic bacteria causing otomycosis are Candida, Aspergillus, Penicillium and so on, which lead to local histopathological changes (3). For example, in Aspergillus infections, bone invasion or tissue damage does not generally occur. The early stage of Candida infection is mainly characterized by exudation, and the late stage is characterized by granulomatous inflammation (4). Blastomyces and Actinomyces infections result in suppurative and granulomatous manifestations. Mucor invades blood vessels, causing thrombi, tissue infarction and leucocyte infiltration. Otomycosis can be asymptomatic, but fungi can multiply and accumulate to form masses that can block the external auditory canal, causing a sense of obstruction. Patients tend to experience a feeling of moisture in the external auditory canal because of fungal mass irritation, which causes a small amount of external auditory canal secretion. The blockage can worsen and invade the eardrum, leading to hearing impairment, tinnitus, and even dizziness (5). If the lesion increases in size, there may be local pain, and severe cases may cause facial paralysis (6).
For patients and physicians, otomycosis can be a very frustrating illness, although it is not a life-threatening ailment. Although otomycosis is not serious in most cases, immune compromise resulting from otomycosis is life-threatening to patients (7). The disease easily develops in patients in warm and humid environments, and it is difficult to obtain a good curative effect if patient treatment compliance is poor. Therefore, to ensure treatment adherence, topical drugs with simple application should be selected for treatment (8). Antifungal agents such as clotrimazole or terbinafine hydrochloride spray can be used, as well as traditional antiseptic medications such as povidone or boric acid alcohol (9). In general, systemic medication is unnecessary. In recent years, there have been great advances in antimicrobial therapy, though no widely accepted topical agent for the treatment of otomycosis has been developed.
Early detection of otomycosis and rapid intervention are important to reduce the negative effects of otomycosis on quality of life (10). Despite the availability of various interventions, their efficacy has rarely been compared, making it difficult to select an appropriate treatment. The authors conducted a systematic review incorporating pairwise and network meta-analyses (NMAs), with the objectives of assessing the relative effects of two medications in patients with otomycosis with regard to prognosis, complications and other key outcomes.
Materials and Methods
Search Strategy
The authors searched the PubMed, EMBASE, GeenMedical, Cochrane Library, CBM, CNKI, VIP and other databases using a combination of controlled vocabulary (e.g.,“Otomycosis,” “Fungus”) and keywords (e.g., “Therapeutic,” “Antifungal Drugs,” “Antiseptic Medication”). The databases were searched in May 2021, and articles related to drug treatment of fungal otomycosis that had been published or were in progress were extracted. In addition, the references of potentially relevant literature were screened.
Eligibility Criteria
There were four criteria for inclusion. a. Research type: randomized controlled trial (RCT) or clinical Trial. b. Research subjects: patients who were clinically diagnosed with otomycosis and whose external auditory canal secretions were positive for fungi. c. Treatment method: topical drug treatment (the experimental group was treated with antifungal drugs, and the control group was treated with non-antifungal drugs). d. Research results: patient cure rate, symptom improvement, and complications after medication use (including ear itching, ear distension, ear pain, etc.).
The exclusion criteria were as follows. (a) Other diseases of the external auditory canal or middle ear with similar symptoms and imaging changes, such as external auditory canal osteoma, external auditory canal cholesteatoma, and middle ear spheroid tumor. (b) Surgical treatment or animal studies. (c) Duplicate studies. (d) Literature with incomplete data or no researchable indicators.
Data Extraction
Two researchers extracted data from the included literature, and differences were resolved through discussion or the opinion of a third researcher. Extracted data included general information (first author, publication time, and country, sex, age) and clinical data (sample size of each group and corresponding rates of cure, symptom improvement, and complications).
Risk of Bias Assessment
Since the included studies were mostly retrospective cohort studies, the Newcastle Ottawa Scale (NOS) was used to assess the risk of bias in the selection of study groups, comparability, and outcomes. A total of 7 items were evaluated, and each item received a score of “1” or “0.” The results are included in the basic research information and are displayed together.
Data Analysis
RevMan5.4 software was used for meta-analysis, and P < 0.05 indicated that a difference was statistically significant. Odds ratios (ORs) and corresponding 95% confidence intervals (Cis) were used to analyse dichotomous variables, and the I2 statistic was used to assess heterogeneity. If P > 0.05 and I2 <50%, the included studies had no obvious heterogeneity, and the fixed-effect model was used. If P < 0.05 and I2 > 50%, the included studies had obvious heterogeneity, and the random-effects models was used; subgroup and sensitivity analyses were performed to explore the source of the heterogeneity. The analysis results are presented as forest plots, and publication bias is shown in funnel plots.
Results
General Study Information
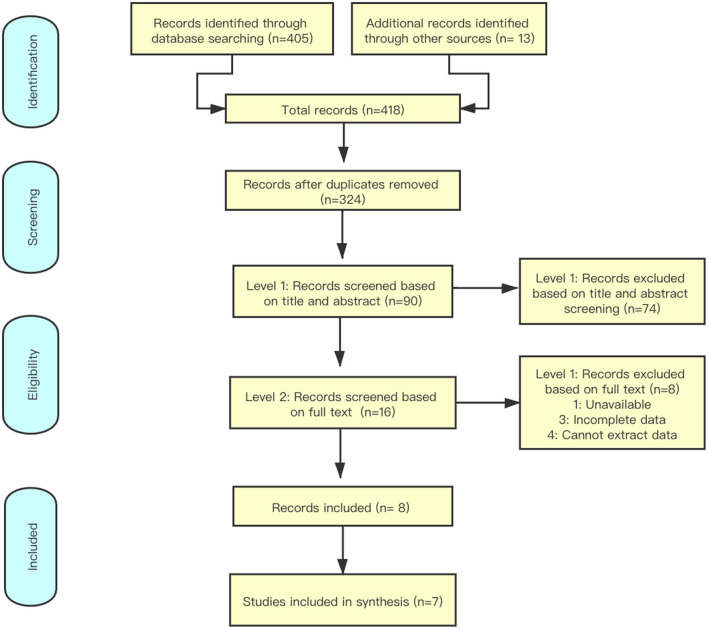
By searching the databases (Figure 1), 418 studies were identified, and 324 studies were selected for further screening. By reading the titles and abstracts of the literature, reviews, case reports or systematic reviews that did not meet the inclusion criteria were excluded. The remaining 16 articles were downloaded for full-text screening. Screening was strictly conducted according to the inclusion criteria. Studies with incomplete data or no research indicators were excluded, and 7 studies (Table 1) were finally included (11–17).
Figure 1.
Preferred reporting items for systematic reviews and meta-analyses search strategy.
Table 1.
Study characteristics and details of interventions.
| Author | Year | Region | Design | Mode of administration | Total N | ||
|---|---|---|---|---|---|---|---|
| Antifungal drug | Traditional antiseptic medication | Male | Female | ||||
| Boncalon et al. | 2009 | Philippines | RCT | Clotrimazole cream 1% | Kalachuchi Bark Extract Ointment | 7 | 9 |
| Mgbor and Gugnani | 2001 | Nigeria | RCT | Clotrimazole | Mercurochrome/ Locacorten-Vioform | 38 | 34 |
| Mofatteh et al. | 2018 | Iran | RCT | Clotrimazole | Betadine | 86 | 118 |
| Philip et al. | 2013 | India | RCT | 1% Clotrimazole + Lignocaine | 7.5% Povidone Iodine | 17 | 17 |
| Romsaithong et al. | 2016 | Thailand | RCT | 1% Clotrimazole | 3% Boric acid in 70% Alcohol | 46 | 74 |
| Swain et al. | 2018 | India | RCT | Clotrimazole | Povidone Iodine | 19 | 25 |
| Xu et al. | 2020 | China | RCT | Terbinafine Hydrochloride Spray + 3%BAA | 3% Boric Acid Alcohol (BAA) | 162 | 136 |
RCT, randomized controlled trial.
Risk of Bias Assessment
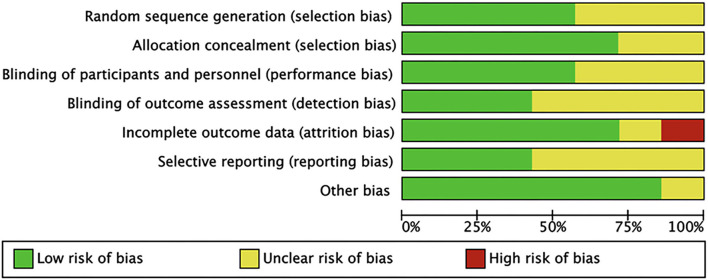
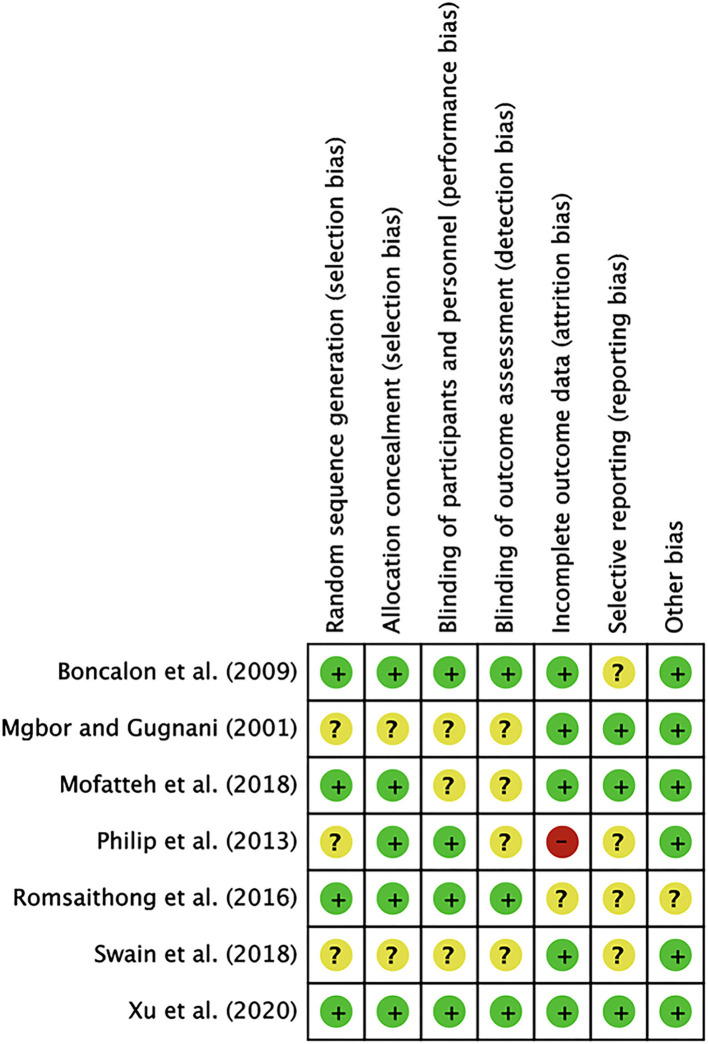
Based on 7 items, we estimated the quality of the literature. As summarized in Figure 1, only one study had a high risk of attrition bias. In this study, the follow-up patient data were incomplete, the number of people lost to follow-up was large, though the specific reasons were not explained. The last article was of higher quality because the information was more complete. Based on the above, all 7 articles were included in the meta-analysis (Figures 2, 3).
Figure 2.
Risk of bias graph. Review authors' judgements about each risk of bias item presented as percentages across all included studies.
Figure 3.
Findings of the risk of bias evaluation. Findings of the risk of bias evaluations using the Cochrane Scale are shown. Green, low risk of bias; red, high risk of bias; yellow, unclear risk of bias.
Patient Population
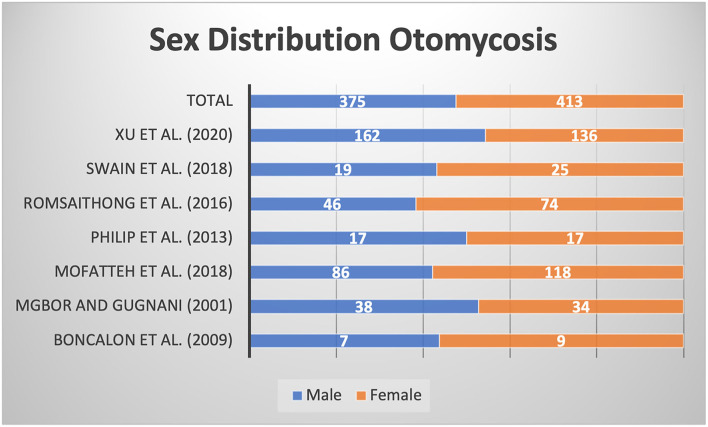
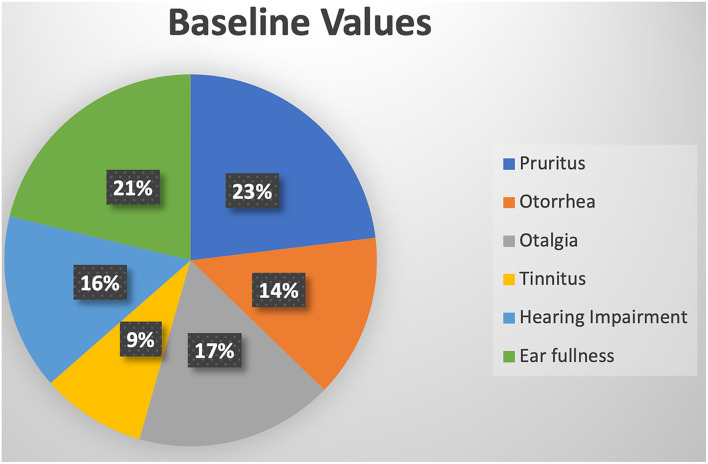
The research areas included India, the Philippines, Nigeria, Iran, Thailand, and China. Most patients were located in hot and humid areas and economically underdeveloped areas. A total of 788 patients were included, including 375 males and 413 females. As shown in Figure 4, there was a female predominance, but there was a certain error due to the small sample size. After baseline ear symptom data were converted using the standard ratio, it was observed that the symptoms of ear itching and ear swelling in patients with external auditory canal mycosis were most common, and the symptom of tinnitus was relatively rare (Figure 5).
Figure 4.
Sex ratios in the included studies.
Figure 5.
Ear symptoms before medication in the included studies.
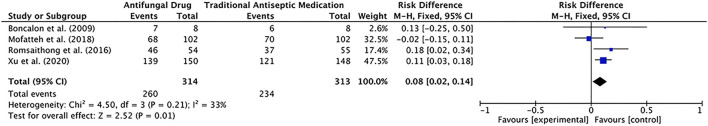
Efficacy and Complications
Four of the included studies described the relief of symptoms by two types of drugs. The antifungal group included 314 patients, of which 260 patients had complete or partial relief of symptoms after treatment. In contrast, the traditional antiseptic medication group included 313 patients, of which 234 patients had complete or partial relief of symptoms after treatment. The data were analyzed with a fixed-effects model (P = 0.21, I2 = 33%), and the results showed the following: total effect Z = 2.52, P = 0.01, RD = 0.08, 95% CI [0.02, 0.14]. The difference was statistically significant, suggesting that antifungal drugs were relatively effective (Figures 6, 7).
Figure 6.
Forest plot of the efficacy of the two drug regimens analyzed in the meta-analysis.
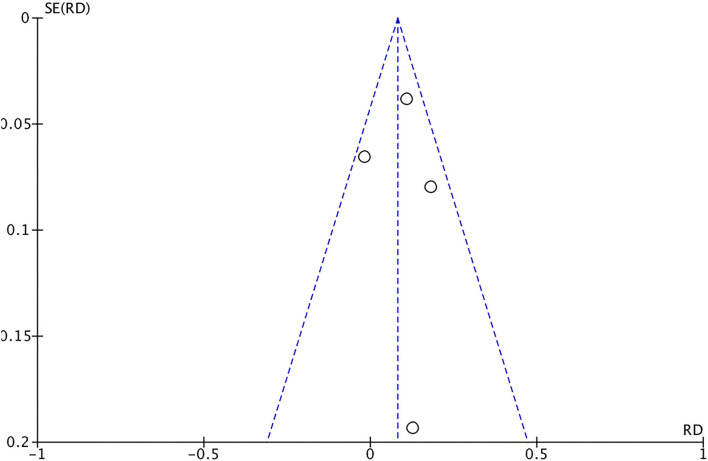
Figure 7.
Funnel plot of the efficacy of the two drug regimens analyzed in the meta-analysis.
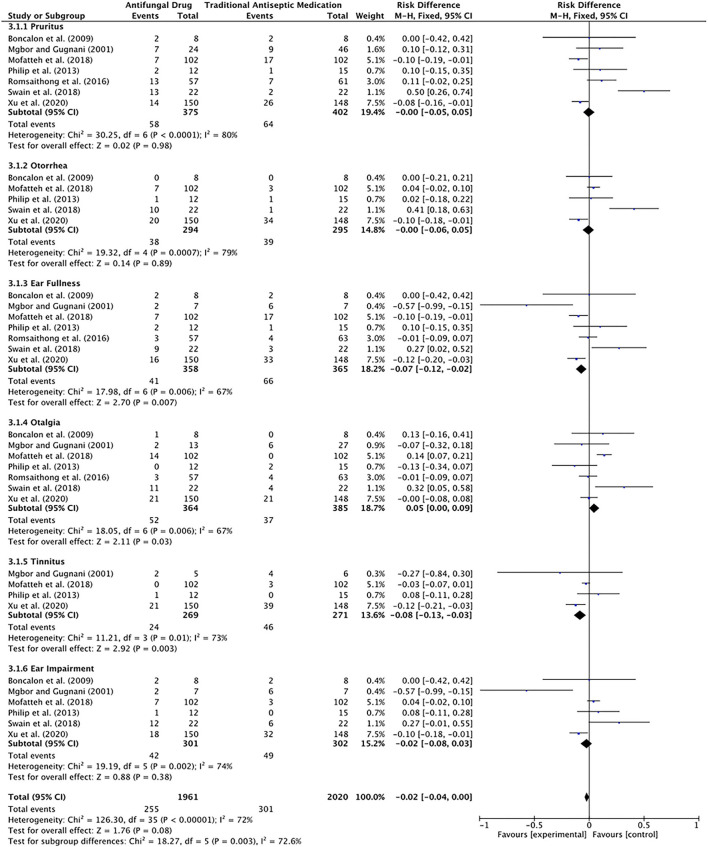
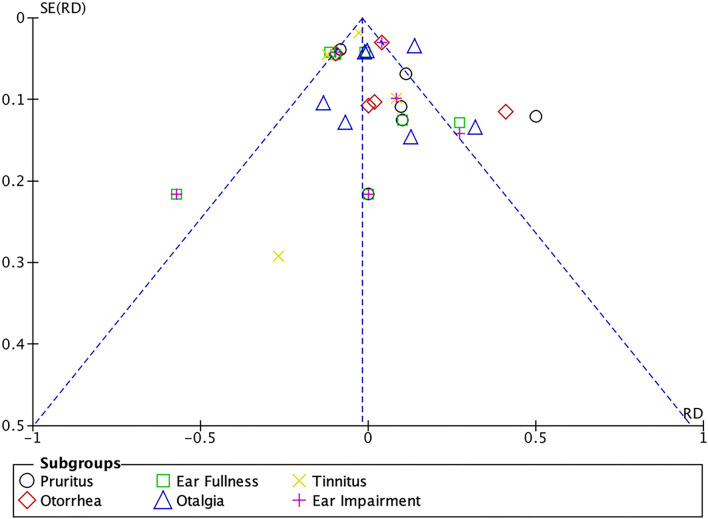
The comparison of six common complications after medication use by the fixed-effect model revealed the following: total effect Z = 1.76, P = 0.08, RD = −0.02, 95% CI [−0.04, 0.00]. The difference was not statistically significant. This result suggested that there was no significant difference in complications after the use of antifungal drugs or traditional antiseptic medication.
The authors further conducted subgroup analyses according to complications using fixed-effects models. The results indicated no significant difference in the rate of ear itching (Z = 0.02, P = 0.98), otorrhea (Z = 0.14, P = 0.89) or deafness (Z = 0.88, P = 0.38); that is, after medication use, both groups experienced complications of ear itching, otorrhea, and deafness, but the differences were not significant.
The differences in the rates of ear distension (Z = 2.70, P = 0.007), earache (Z = 2.11, P = 0.03) and tinnitus (Z = 2.92, P = 0.003) were statistically significant. Patients who received antifungal drugs had lower rates of ear swelling and tinnitus, while patients who received non-antifungal drugs had lower rates of ear pain (Figures 8, 9).
Figure 8.
Forest plot of complications associated with the two drug regimens analyzed in the meta-analysis.
Figure 9.
Funnel plot of complications associated with the two drug regimens analyzed in the meta-analysis.
Discussion
Otomycosis is a superficial fungal infection that causes subacute or chronic inflammation due to fungal replication under certain conditions (18). The fungus invades the stratum corneum of the external auditory canal, causing otalgia, itching, hearing impairment, etc. This study analyzed current literature on the treatment of otomycosis with two types of commonly used clinical drugs. The results suggested that the therapeutic effects of the two types of drugs were statistically significant. Considering the easy application process and patient acceptance, the overall therapeutic effect of topical antifungal drugs was better than that of topical antiseptic medication; however, some treatments were incomplete. Traditional antiseptic medication, which is associated with complications such as tinnitus, nausea and vomiting after treatment, causes poor treatment adherence in some patients. The type of medication should be reasonably selected according to the condition of the disease.
This meta-analysis was conducted for three main reasons. First, the anatomical structure of the external auditory canal has a physiological curvature; therefore, different methods of medication application will have an impact on their efficacy (19). Antifungal drugs are generally cream preparations that partially cover the lesions, which are prone to recurrence. Non-antifungal drugs, by comparison, are generally liquid and penetrate deep into the external auditory canal, which not only reduces local inflammation and exudation but also completely covers the lesion (20). Second, antifungal drugs contain relatively tiny amounts of hormones, alleviating local inflammation and halting the proliferation of fungi more quickly than non-antifungal drugs. Therefore, antifungal drugs have better curative effects and lead to a faster recovery. Third, the included regions were mostly tropical and subtropical regions, indicating that the incidence of otomycosis has obvious regional characteristics. In addition, there were more female patients than male patients, which may be related to a weaker immune systems (21).
Limitations of this study should be noted. First, the included studies used various evaluation criteria to define cure, and some reported data that were unable to be used in this meta-analysis, leading to publication bias. Second, there was a lack of research conducted in North America and Europe. Finally, few relevant studies have been conducted in this field, and further analyses are needed.
Otomycosis, which is diagnosed by external auditory canal secretion smears, is a common and frequently occurring clinical disease (22). Once this disease is diagnosed, remedial measures should be implemented promptly. Two classes of drugs are currently available to treat this disease. The results of this study suggest the following. Antifungal drugs, such as clotrimazole, are associated with fewer complications and have a better cure rate but are also associated with poor treatment compliance and ear pain. Traditional antiseptic medications, such as boric acid alcohol, are associated with complications that seriously affect treatment compliance and completion. In summary, although this meta-analysis has certain shortcomings, it still has certain significance in guiding clinical drug treatment.
Conclusion
This meta-analysis and literature review suggests that antifungal drugs and traditional antiseptic medication are effective in relieving symptoms in patients with otomycosis. These treatments also had a significant favorable effect on hearing. Overall, in the small number of studies evaluated, topical treatment was shown to be a safe, effective, and non-destructive alternative for patients who are refractory to initial medical therapy. Antifungal drugs had a better overall therapeutic effect with fewer complications; however, because of the obvious complications of earache, most patients found treatment unbearable. Traditional antibacterial medication is associated with a larger number of complications, although treatment is relatively thorough and inexpensive. Otolaryngologists have the option to use one medication or a combination of two drugs on the basis of the condition. However, these conclusions must be interpreted with caution due to the limitations of this analysis. Future research in this area should include RCTs with long-term follow-up to guide the development of guidelines for otomycosis to overcome some of the weaknesses noted in the literature.
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication. Shunyu Wu sorted data and wrote article. Yin Cheng provided information about literature search strategies, and assisted with the literature search. Shunzhang Lin assisted with the meta-analysis, and Huanhai Liu assisted with proofreading.
Funding
This work was financially supported by a grant (No.0907) from the Department of Otolaryngological, Shanghai Changzheng Hospital, Shanghai, China and three grants from the National Science Foundation of China (Nos. 81541038, 81670905, and 81870702).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors gratefully acknowledge the National Science Foundation of China as well as the Pyramid Talent Program number 0907 and also acknowledged for the excellent training of Navy Military Medical University.
Glossary
Abbreviations
- PRISMA
the Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCTs
Randomized controlled trials
- NOS
the Newcastle Ottawa Scale
- ORs
Odds ratios
- Cis
confidence intervals.
References
- 1.Kamali Sarwestani H, Daie Ghazvini R, Hashemi SJ, Rezaie S, Gerami Shoar M, Mahmoudi S, et al. Investigation of etiologic agents and clinical presentations of otomycosis at a tertiary referral center in Tehran, Iran. Iran J Public Health. (2019) 48:331–7. 10.18502/ijph.v48i2.832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kryukov AI, Kunelskaya NL, Kunelskaya VY, Ivoylov AY, Shadrin GB, Machulin AI. Fungal otitis externa in children: principles of diagnosis and rational therapy. Vestn Otorinolaringol. (2020) 85:60–3. 10.17116/otorino20208501160 [DOI] [PubMed] [Google Scholar]
- 3.Zakaria A, Osman M, Dabboussi F, Rafei R, Mallat H, Papon N, et al. Recent trends in the epidemiology, diagnosis, treatment, and mechanisms of resistance in clinical Aspergillus species: a general review with a special focus on the Middle Eastern and North African region. J Infect Public Health. (2020) 13:1–10. 10.1016/j.jiph.2019.08.007 [DOI] [PubMed] [Google Scholar]
- 4.Arensman K, Miller JL, Chiang A, Mai N, Levato J, LaChance E, et al. Clinical outcomes of patients treated for Candida auris infections in a multisite health system, Illinois, USA. Emerg Infect Dis. (2020) 26:876–80. 10.3201/eid2605.191588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shibuya Y, Morioka D, Nomura M, Zhang Z, Utsunomiya H. Earwax of patients with hidradenitis suppurativa: a retrospective study. Arch Plast Surg. (2019) 46:566–71. 10.5999/aps.2019.00290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arsovic N, Radivojevic N, Jesic S, Babac S, Cvorovic L, Dudvarski Z. Malignant otitis externa: causes for various treatment responses. J Int Adv Otol. (2020) 16:98–103. 10.5152/iao.2020.7709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Viswanatha B, Sumatha D, Vijayashree MS. Otomycosis in immunocompetent and immunocompromised patients: comparative study and literature review. Ear Nose Throat J. (2012) 91:114–21. 10.1177/014556131209100308 [DOI] [PubMed] [Google Scholar]
- 8.Jia X, Liang Q, Chi F, Cao W. Otomycosis in Shanghai: aetiology, clinical features and therapy. Mycoses. (2012) 55:404–9. 10.1111/j.1439-0507.2011.02132.x [DOI] [PubMed] [Google Scholar]
- 9.Fasunla J, Ibekwe T, Onakoya P. Otomycosis in Western Nigeria. Mycoses. (2008) 51:67–70. 10.1111/j.1439-0507.2007.01441.x [DOI] [PubMed] [Google Scholar]
- 10.Van Stekelenburg BCA, Aarts MCJ. Fungal otitis externa and wet ear with mucopurulent should be a influencing factors on tympanic membrane closure. Eur Arch Otorhinolaryngol. (2020) 277:2147. 10.1007/s00405-020-05917-9 [DOI] [PubMed] [Google Scholar]
- 11.Philip A, Thomas R, Job A, Sundaresan VR, Anandan S, Albert RR. Effectiveness of 7.5 percent povidone iodine in comparison to 1 percent clotrimazole with lignocaine in the treatment of otomycosis. ISRN Otolaryngol. (2013) 2013:239730. 10.1155/2013/239730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boncalon R, Arugay M, Ramos R. A preliminary study on the efficacy of Plumeria acuminata (Kalachuchi) bark extract ointment vs. clotrimazole cream in the treatment of otomycosis. Philipp J Otolaryngol Head Neck Surg. (2009) 24:5–8. 10.32412/pjohns.v24i1.701 [DOI] [Google Scholar]
- 13.Mgbor N, Gugnani HC. Otomycosis in Nigeria: treatment with mercurochrome. Mycoses. (2001) 44:395–7. 10.1046/j.0933-7407.2001.00682.x [DOI] [PubMed] [Google Scholar]
- 14.Mofatteh MR, Naseripour Yazdi Z, Yousefi M, Namaei MH. Comparison of the recovery rate of otomycosis using betadine and clotrimazole topical treatment. Braz J Otorhinolaryngol. (2018) 84:404–9. 10.1016/j.bjorl.2017.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Romsaithong S, Tomanakan K, Tangsawad W, Thanaviratananich S. Effectiveness of 3 per cent boric acid in 70 per cent alcohol vs. 1 per cent clotrimazole solution in otomycosis patients: a randomised, controlled trial. J Laryngol Otol. (2016) 130:811–5. 10.1017/S0022215116008598 [DOI] [PubMed] [Google Scholar]
- 16.Swain SK, Behera IC, Sahu MC, Das A. Povidone iodine soaked gelfoam for the treatment of recalcitrant otomycosis - Our experiences at a tertiary care teaching hospital of Eastern India. J Mycol Med. (2018) 28:122–7. 10.1016/j.mycmed.2017.11.006 [DOI] [PubMed] [Google Scholar]
- 17.Xu S, Li J, Ding L, Gao K, Xie F, Han J, et al. Efficacy and safety of terbinafine hydrochloride spray and 3% boric acid alcohol ear drops in otomycosis. Acta Otolaryngol. (2020) 140:302–6. 10.1080/00016489.2020.1712474 [DOI] [PubMed] [Google Scholar]
- 18.Nemati S, Hassanzadeh R, Khajeh Jahromi S, Delkhosh Nasrollah Abadi A. Otomycosis in the North of Iran: common pathogens and resistance to antifungal agents. Eur Arch Otorhinolaryngol. (2014) 271:953–7. 10.1007/s00405-013-2486-0 [DOI] [PubMed] [Google Scholar]
- 19.Pichon M, Joly V, Argy N, Houze S, Bretagne S, Alanio A, et al. Aspergillus flavus malignant external otitis in a diabetic patient: case report and literature review. Infection. (2020) 48:193–203. 10.1007/s15010-020-01394-8 [DOI] [PubMed] [Google Scholar]
- 20.Kiakojuri K, Rajabnia R, Mahdavi Omran S, Pournajaf A, Karami M, Taghizadeh Armaki M. Role of clotrimazole in prevention of recurrent otomycosis. Biomed Res Int. (2019) 2019:5269535. 10.1155/2019/5269535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Unadkat S, Kanzara T, Watters G. Necrotising otitis externa in the immunocompetent patient: case series. J Laryngol Otol. (2018) 132:71–4. 10.1017/S0022215117002237 [DOI] [PubMed] [Google Scholar]
- 22.Kiakojuri K, Armaki MT, Rajabnia R, Pournajaf A, Karami M, Khademian A, et al. Outer ear infections in Iran: a review. Open Access Maced J Med Sci. (2019) 7:1233–40. 10.3889/oamjms.2019.176 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.